Abstract
This study aims to investigate the long-term prognosis and the affecting factors towards the patients with acute pulmonary thromboembolism (APTE). The clinical data of 903 PTE patients, diagnosed by the spiral CT pulmonary angiography (CTPA) or lung ventilation perfusion scanning when hospitalized in the Second Hospital of Hebei Medical University from January 1998 to December 2013, were collected, among who 548 patients were performed the long-term follow-up, and the factors that would affect the prognosis were statistically analyzed. The univariate analysis showed that many factors would affect the prognosis of PTE. The multivariate non-conditional logistic regression analysis showed that: the relevant factors of re-embolization included the idiopathic pulmonary embolism, RVD, D-dimer positive, anticoagulation treatment < 3 months, post-treatment PASP > 40 mmHg, the relevant factors of death included the D-dimer positive, anticoagulation treatment < 3 months, cTnI positive, post-treatment PASP > 40 mmHg. RVD and post-treatment PASP > 40 mmHg would increase the risk of chronic thromboembolic pulmonary hypertension (CTEPH). The idiopathic pulmonary embolism, RVD, D-dimer positive, anticoagulation treatment < 3 months, cTnI positive and post-treatment PASP > 40 mmHg were the important factors that would affect the long-term prognosis of PTE patients.
Keywords: Pulmonary thromboembolism, prognosis, risk factors
Introduction
The pulmonary thromboembolism (PTE) referred to a series of clinical and pathophysiological syndromes that were caused by the thrombosis of pulmonary artery or other branches, as a common emergency of internal medicine, its poor prognosis included the re-embolism, death, CTEPH and so on. With the development of medical technologies, its prognosis had become the focus of many scholars. Despite adequate treatment, up to one quarter of patients with symptomatic deep vein thrombosis (DVT) and/or pulmonary embolism (PTE) will experience recurrent venous thromboembolism (VTE) within the subsequent 5 years [1-3]. Of note, 25% of the patients do not survive the first year after diagnosis, although the majority of deaths during this time are related to underlying conditions such as cancer or chronic heart disease rather than to PE itself [4,5]. Previous studies 1, 3 have reported an incidence of CTPH between 0.1% and 3.8% in patients with previous venous thromboembolism (VTE) [6-8]. Currently, many researchers had found that the re-embolism rate of idiopathic PTE patients was more than 2-fold of non-idiopathic patients, especially the patients with temporary risk factors [1,9,10]. In addition, many scholars believed that the right ventricular dysfunction was the important cause of death towards the PTE patients, Zhu et al [11] found that the 14-day mortality of PTE patients associated with right ventricular dysfunction was significantly increased than those with normal right ventricular function (2.0% vs 0.4%, P < 0.01). Furthermore, the foreign studies had shown that the incidence of CTEPH was 0.5%-3.8% [6,7,12-14], and most CTEPH patients exhibited poor quality of life and prognosis. Therefore, it would be important to make clear the long-term prognosis and related factors of PTE patients.
Here we report on the prospective long-term follow-up of a large series of patients with PTE. All of them received conventional anticoagulation and/or thrombolytic therapy, and were then followed-up for a maximum of 12 years after the PTE was diagnosed in order to document the incidence of recurrent PTE, death and CTEPH, and analysis the risk factors.
Materials and methods
Case selection
The PTE patients, diagnosed by the spiral CT pulmonary angiography (CTPA) or lung ventilation perfusion scanning when hospitalized in the Second Hospital of Hebei Medical University from January 1998 to December 2013, were selected. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Hebei Medical University. Written informed consent was obtained from all participants.
Inclusion criteria: 1. Based on the diagnostic criteria of “diagnosis and treatment guidelines of pulmonary thromboembolism”, issued by the Respiratory Branch of Chinese Society in 2001 [15]. 2. with the disease duration less than two weeks. 3. According to the ESC PTE Guidelines in 2008, the high-risk group was performed the thrombolytic therapy, the middle-risk group was performed the thrombolytic or anticoagulant therapy based on the clinical circumstances and wishes of patients, and the low-risk group was performed the anticoagulant therapy. The oral anticoagulant therapy used the low molecular weight heparin and started within 1 week, and the anticoagulant treatment should be determined according to the real situations.
Clinical data collection
Patient-related information was screened, including communication information, general situation when admission, clinical manifestations, laboratory examinations, treatment methods, complications, re-embolism and death, etc.
Diagnosis of right heart dysfunction
RVD could be diagnosed when the patient met any one of the following conditions: 1. the right ventricle enlarged (diastolic trans diameter of right ventricle/diastolic trans diameter of left ventricle > 1, or diastolic anteroposterior diameter of right ventricle/diastolic anteroposterior diameter of left ventricle > 0.5, or end-diastolic inner diameter of right ventricle > 25 mm); 2. the right ventricular wall motion weakened (amplitude of right ventricular anterior wall motion < 5 mm); 3. pressure overload (pulmonary artery systolic pressure > 30 mmHg).
Follow-up
The 3-month to 12-year follow-up was performed by telephone and patient’s hospital visiting, and such necessary relevant checks as CTPA, UCG, lower limb-venous ultrasound, D-dimer, oral anticoagulation therapy were performed, with the focus as events and related factors of re-embolism, death and CTEPH, etc.
Statistical methods
The statistical analysis was performed by SPSS13.0 software package. The measurement data were expressed as mean ± standard deviation (x ± s), the intergroup comparison used the t test. The counting data were expressed as rate or construction proportion, the intergroup comparison used the χ2 test (with P < 0.05 considered as the statistical significance). The multivariate analysis used the multivariate non-conditional logistic regression analysis to calculate the relative risk (RR) and confidence intervals (95% CI), with P < 0.1 considered as statistically significant.
Results
Patients
The clinical data of 903 PTE patients, diagnosed by the spiral CT pulmonary angiography (CTPA) or lung ventilation perfusion scanning when hospitalized in the Second Hospital of Hebei Medical University from January 1998 to December 2013, were collected. Among who 548 cases exhibited better compliance, the follow-up period was (2.34±1.20) years. Among the 548 follow-up cases, 66 cases died (12.04%), 48 cases exhibited the re-embolism (8.76%), and 20 cases exhibited the CTEPH (3.65%).
Basic features
520 cases were diagnosed by the pulmonary artery angiography (94.72%), 29 cases were diagnosed by the pulmonary ventilation perfusion scanning (5.28%), among who 270 cases were males and 278 cases were females, aged 19 to 90 years old, with the mean age as (59.87±15.26) years old. The population aged over 40 years old, when PTE onset, accounted for 88.34%, while those under 40 years old accounted for 11.66%. Among the 48 cases of re-embolism, 23 were males and 25 were females, with the mean age as (57.66±13.57) years old, among the 66 cases of death, 41 cases were males and 25 cases were females, with the mean age as (65.22±13.05) years old, among 20 cases of CTEPH, 12 cases were males and 8 cases were females, with the mean age as (55.28±13.68) years old, among the 414 cases that did not occur the poor prognosis, 223 cases were males and 197 cases were females, with the average age as (58.93±15.69) years old, there was no statistical significance in the constituent ratios of sex and age among the four groups (P > 0.05).
Underlying diseases
The hypertension was the most common, accounting for 41.06% (225 cases), followed by 148 cases of DVT and (or) varicose vein of lower limbs (26.96%), 128 cases of long-term bed laying (23.32%), 97 cases of coronary heart disease (17.67%), 64 cases of diabetes (11.66%), 65 cases of chronic lung disease (11.84%), 135 cases of idiopathic patients (24.64%), 33 cases of trauma surgery (6.01%), 42 cases of heart failure (7.66%) and 16 cases of cancer (2.91%).
Clinical symptoms
The shortness of breath and breathing difficulty were the most common, accounting for 69.03% (379 cases), followed by 137 cases of chest pain (36.07%), 115 cases of syncope (20.95%). The occurrence rate of typical triad (dyspnea, chest pain and hemoptysis) was 4.56%. The signs of faster respiratory rate (291 cases, 53.01%), lower extremity edema or varicose veins (214 cases, 38.98%) and P2 hyperthyroidism (205 cases, 37.34%) were common.
Auxiliary examinations
All the patients were performed the electrocardiography, echocardiography, venous ultrasound examination and serological examination, among who 234 cases (42.62%) exhibited the ECG changes, including newly-emerged QRS right axis bias, SIQIIITIII, complete or incomplete bundle branch block, and inversion of pulmonary P wave and T wave. 450 patients (81.97%) were performed the echocardiography examination, and 208 cases exhibited the right ventricular dilatation (46.22%), 174 cases exhibited the pulmonary hypertension (38.67%), with the mean pulmonary artery pressure as 58.72±23.10 mmHg, 42 patients exhibited the intracardiac thrombus (9.33%). 318 cases were performed the venous ultrasonography, and it was found that 201 cases had the deep vein thrombosis (63.21%). The serological examinations: 348 cases were performed the D-dimer examination, with the positive rate as 74.59%, and 237 cases were performed the clear troponin (cTnI) examination, with the positive rate as 11.45%. 489 cases were performed the arterial blood gas analysis, with the average arterial oxygen pressure as 76.49±22.81 mmHg, and the occurrence rate of hypoxemia was 19.02% (93 cases).
Prognosis
548 patients were followed up for a period of 3 months to 12 years, during the follow-up period, 48 patients occurred the re-embolism, 5 patients occurred the chronic thromboembolic pulmonary hypertension, 66 patients died, including 19 PTE-related cases, 2 cases died of the blood diseases, 2 cases of malignant tumors, 8 cases of heart failure or respiratory failure, and another 35 cases had unknown or uncertain reasons.
During the hospitalization, 95 patients were performed the thrombolytic therapy, 2 cases were implanted the inferior vena cava filter, and only 3 cases exhibited serious gastrointestinal bleeding. 11 cases (2.00%) died during the hospitalization, among who 6 patients died of PTE, among the rest 5 cases, 3 cases died of malignant cancers, and 2 cases died of chronic lung disease-caused respiratory failure.
During January 2005 and December 2013, the annual incidence rates of PTE patients’ death, re-embolism and CTEPH were decreased significantly, which were from 25.0%, 12.5% and 5.0% to 1.69%, 2.81% and 0.90%, respectively, thus it could be seen that the PTE diagnosis and treatment obtained the rapid progress in the recent years (Figure 1).
Figure 1.
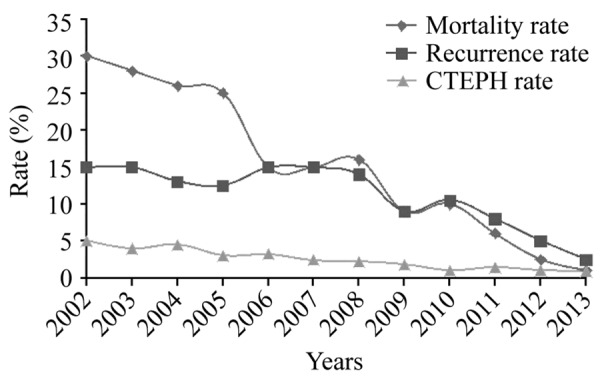
Trends of annual incidence rates of re-embolism, death and CTEPH in the acute PTE patients.
Analysis of relevant factors
The univariate analysis showed that: idiopathic PTE, DVT, heart failure, long-term bed laying, right ventricular dysfunction (RVD), D-dimer (D-dimer) positive, cTnI positive, anticoagulation treatment < 3 months, age > 65 years and post-treatment PASP > 40 mmHg were the risk factors of re-embolism; deep vein thrombosis (DVT), chronic lung disease, heart failure, history of stroke, anticoagulation treatment < 3 months, thrombolytic treatment, long-term bed laying, hyperlipidemia, RVD, D-dimer positive, cTnI positive and post-treatment PASP > 40 mmHg were the a risk factors of death; idiopathic PTE, DVT, heart failure, coronary artery disease, hyperlipidemia, thrombolytic therapy, RVD, D-dimer positive, cTnI positive, hypoxemia, pre-treatment PASP > 50 mmHg and post-treatment PASP > 40 mmHg were the risk factors of CTEPH (P < 0.05, Table 1).
Table 1.
Single factor χ2 test that would affect the long-term prognosis
| Risk factor | Better prognosis 414 cases (%) | Re-embolism 48 cases (%) | χ2 | P | Death 66 cases (%) | χ2 | P | CTEPH 20 cases (%) | χ2 | P |
|---|---|---|---|---|---|---|---|---|---|---|
| Idiopathic PTE | 94/414 | 38/48 | 67.189 | 0.000 | 17/66 | 0.298 | 0.342 | 16/20 | 33.099 | 0.000 |
| Hypertension | 190/414 | 28/48 | 3.172 | 0.052 | 25/66 | 1.479 | 0.319 | 8/20 | 0.267 | 0.390 |
| DVT | 117/396 | 21/40 | 5.700 | 0.017 | 22/59 | 7.839 | 0.005 | 12/20 | 8.254 | 0.006 |
| CPD | 53/414 | 3/48 | 1.733 | 0.137 | 17/66 | 7.670 | 0.007 | 4/20 | 0.866 | 0.261 |
| HF | 23/414 | 12/48 | 23.226 | 0.000 | 10/66 | 8.187 | 0.008 | 8/20 | 34.126 | 0.000 |
| CHD | 72/414 | 12/48 | 1.674 | 0.137 | 9/66 | 0.572 | 0.288 | 8/20 | 6.486 | 0.018 |
| DM | 52/414 | 3/48 | 1.633 | 0.147 | 10/66 | 0.340 | 0.339 | 0 | 2.854 | 0.073 |
| Stroke | 24/414 | 3/48 | 0.016 | 0.548 | 9/66 | 5.464 | 0.026 | 0 | 1.227 | 0.312 |
| Thrombolysis | 109/414 | 12/48 | 0.039 | 0.499 | 6/66 | 4.946 | 0.016 | 0 | 7.032 | 0.003 |
| Surgery/trauma | 24/414 | 3/48 | 0.016 | 0.548 | 4/66 | 0.007 | 0.554 | 0 | 1.227 | 0.312 |
| Long-term bed laying | 102/414 | 5/48 | 4.488 | 0.016 | 4/66 | 11.417 | 0.000 | 0 | 6.441 | 0.004 |
| Hyperlipidemia | 17/414 | 1/48 | 0.470 | 0.424 | 19/66 | 49.986 | 0.000 | 8/20 | 45.279 | 0.000 |
| Cancer | 10/414 | 2/48 | 0.521 | 0.360 | 2/66 | 0.088 | 0.509 | 0 | 0.494 | 0.621 |
| RVD | 99/337 | 32/45 | 33.744 | 0.000 | 24/51 | 19.721 | 0.000 | 20/20 | 42.374 | 0.000 |
| D-dimer positive | 262/346 | 45/48 | 20.097 | 0.000 | 39/46 | 21.487 | 0.000 | 4/20 | 29.564 | 0.000 |
| cTnI positive | 11/260 | 8/40 | 18.913 | 0.000 | 5/30 | 5.772 | 0.016 | 4/20 | 9.108 | 0.016 |
| Anticoagulation therapy < 3 m | 42/414 | 10/48 | 4.920 | 0.031 | 12/66 | 3.683 | 0.049 | 4/20 | 1.955 | 0.151 |
| Hypoxemia | 64/414 | 5/48 | 0.861 | 0.244 | 6/66 | 1.853 | 0.117 | 8/20 | 8.304 | 0.009 |
| Male | 221/414 | 21/48 | 1.800 | 0.133 | 30/66 | 1.434 | 0.144 | 12/20 | 0.336 | 0.365 |
| Age > 65 | 148/414 | 9/48 | 5.540 | 0.012 | 28/66 | 1.092 | 0.182 | 4/20 | 2.079 | 0.112 |
| Pre-treatment PASP > 50 | 126/330 | 14/43 | 0.513 | 0.474 | 22/59 | 0.017 | 0.896 | 20/20 | 29.639 | 0.000 |
| Post-treatment PASP > 40 | 11/58 | 13/24 | 10.161 | 0.001 | 14/42 | 36.592 | 0.000 | 16/20 | 24.995 | 0.000 |
Note: DVT: deep vein thrombosis; CPD: chronic pulmonary disease; HF: heart failure; CHD: coronary heart disease; DM: diabetes; RVD: Right ventricular dysfunction; PASP: pulmonary artery systolic pressure.
Multivariate unconditional logistic regression analysis
The multivariate unconditional logistic regression analysis revealed that the idiopathic PTE, RVD, D-dimer positive, anticoagulation treatment < 3 months and post-treatment PASP > 40 mmHg were associated with the re-embolism; D-dimer positive, anticoagulation treatment < 3 months, cTnI positive and post-treatment PASP > 40 mmHg were related with death; RVD and post-treatment PASP > 40 mmHg could increase the risk of CTEPH (P < 0.05, Table 2).
Table 2.
Multivariate unconditional logistic regression analysis that would affect the long-term prognosis
| Risk factor | RR | 95% CI | P | |
|---|---|---|---|---|
| Re-embolism | RVD | 8.05 | 2.85-22.78 | 0.000 |
| D-dimer positive | 5.89 | 1.35-25.68 | 0.018 | |
| Idiopathic PTE | 20.09 | 5.85-69.02 | 0.000 | |
| Post-treatment PASP > 40 | 10.39 | 3.49-30.90 | 0.000 | |
| Anticoagulation therapy < 3 m | 2.23 | 1.06-3.49 | 0.03 | |
| Death | D-dimer positive | 3.83 | 1.01-14.53 | 0.049 |
| Post-treatment PASP > 40 | 7.20 | 1.62-31.97 | 0.009 | |
| Anticoagulation therapy < 3 m | 5.36 | 1.14-25.23 | 0.033 | |
| cTnI positive | 7.04 | 1.39-35.66 | 0.018 | |
| CTEPH | RVD | 1.40 | 1.12-3.32 | 0.048 |
| Post-treatment PASP > 40 | 2.37 | 1.15-6.12 | 0.007 |
Discussion
The recent studies found that the incidence rate of re-embolism 3 months, 1 year, 3 years, 5 years and 10 years after the acute pulmonary embolism (APTE) were 5.7%, 11.0%, 19.6%, 29.1% and 39.9%, respectively, and the relative risk factors included idiopathic PE, aging, thrombophilia, primary DVT and too short anticoagulation treatment, etc. [16,17]. The 30-day, 1-year and 3-year mortality were 13.0%, 26.0% and 35.3%, respectively, and the main related factors were instable hemodynamics, RVD and cTnI positive, etc. [18]. The CTEPH incidence rates 6 months, 1 year and 2 years after APTE were 1.0%, 3.1% and 3.8%, and mainly related with small onset age, persistent pulmonary thromboembolism and idiopathic PTE, etc. [7]. This study performed the follow-up research towards the PTE patients within the recent 15 years, aiming to understand the prognosis-related factors of PTE, then minimize the mortality and morbidity. The results showed the idiopathic PTE, RVD, D-dimer positive, anticoagulation treatment < 3 months, cTnI positive and post-treatment PASP > 40 mmHg were the important factors that would affect the long-term prognosis of PTE patients.
Among the patients reported by Meneveau et al. [19], age > 75 years old, malignancy and post-thrombolysis persistent pulmonary obstruction > 30% were the major factors that would cause death. The short-term all-cause mortality of patients with echocardiographic RVD was 10%, while that of the patients without short-term echocardiographic RVD was 3%, the mortality of patients with RVD was significantly increased [20]. The retrospective study revealed that the right ventricular dilation in CT might be the independent predictor of all-cause mortality and adverse events of PTE patients [21]. The Meta-analysis of two retrospective studies showed that 47% PE patients exhibited the right ventricular dilation in CT, this study set the end-diastolic diameter ratio of right/left ventricle > 0.9 to 1.5 as the right ventricular dilation criteria. The short-term all-cause mortalities of the patients with or without right ventricular dilation were 14% and 6%. The risk increase of mortality of the patients with right ventricular dilation was not statistically significant (RR = 2.3, 95 CI = 0.9-6.0) [20]. This study and the above literatures all suggested the existence of continued pulmonary vascular obstruction after the PTE treatment, especially the post-treatment PASP > 40 mmHg would result in the pulmonary hypertension and RVD; the right ventricular dilation would cause the septal left shifting, left ventricular dysfunction, followed by the cardiac output declining, which would thereby cause the systemic hypotension or shock; the low intra-aortic blood pressure and high right atrial pressure would cause the gradient declining of coronary perfusion and myocardial blood flow, especially the right ventricular subendocardial cardiac muscle would be in the status of hypo-perfusion. At the same time, the nervous and humoral factors activated the sympathetic nervous system, resulting in the positive chronotropic and inotropic changes, meanwhile under the Frank-Starling mechanism, the cardiac output was increased to maintain the stability of pulmonary circulation blood volume and systemic blood pressure. The combined effects of the above situations resulted in the increase of myocardial oxygen demand and gradient descent of coronary perfusion, which would lead to the myocardial injury, create a vicious cycle and affect the prognosis [22], so that the incidence rates of such adverse outcomes as re-embolism, death and CTEPH would increase.
In addition, the idiopathic PTE was also an important factor that would affect the prognosis of patients. Due to the unknown reasons, it would often be difficult to perform the targeted prevention measures, so the majority of scholars agreed that the anticoagulant treatment of the patients with idiopathic PTE should be longer than six months, even lifelong. This study showed that the idiopathic PTE could increase patients’ thrombosis and mortality, which might be related with the repeated embolization caused by the unknown difficult-to-prevent risk factors, low level attention from the patients and no adherence to the long-term anticoagulant therapy.
D-dimer positive was also an important factor that would affect the prognosis of PTE patients. Cosmi et al [23] found that in a case-control study that compared with the sustained negative patients, the re-embolism rate of continuous D-dimer positive (HR = 9.38) or turned positive within three months and continued positive was higher (HR = 3.78). Based on the D-dimer levels (immunoturbidimetric assay), Palareti et al. [24] divided the PTE patients into three layers (D-dimer 500-2499 ng/mL, 2500-4999 ng/mL and > 5000 ng/mL), the distribution of these 3 groups’ patients were 47.8%, 26.0% and 20.4%; D-dimer 500-2499 ng/mL was set as the reference, the relative risks of death of the following two groups increased in turn (OR, 1.91 and 2.94 respectively), and the death risk of fatal pulmonary embolism in the D-dimer > 5000 ng/mL PTE patients was significantly higher than those combined with cancer, braking, renal dysfunction and other complications (OR = 4.4 vs 2.1). Through the univariate and multivariate analysis. This study also showed that the continuous D-dimer positive could increase the re-embolism and mortality rates of the PTE patients.
The inadequate anticoagulation treatment could also increase the incidence rate of adverse events in the PTE patients. Ageno et al [25] found that the standard anticoagulation intensity could reduce the risk of re-thrombosis than the low-intensity, while did not significantly increase the risk of bleeding. In addition, this study also found that the re-embolism rate towards the low international normalized ratio (INR) was higher than those with the standard intensity (1.9% vs 0.9%), and the longer the target-achieving time in the early INR treatment, the higher the re-embolism rate at the end of anticoagulation [26]. In addition, the inadequate period or intensity of anticoagulation, post-treatment persistent thrombosis and general obstruction of pulmonary vascular bed more than 40% would form CTEPH and RVD [6], thus leading to the right heart failure, even the whole heart failure, which would reduce the patients’ life quality, even increase the mortality. Furthermore, CTEPH exhibited the progressive development, and poor results towards the drug treatment, the effects of non-surgical treatment could not be entirely ensured. Through the long-term follow-up, this study found that the incidence rate of CTEPH was 3.88%, slightly higher than the above studies. Therefore, the prevention and effective treatment of CTEPH still needed the further study.
The recent studies had found that partial acute PTE patients also exhibited the elevated serum troponin levels, and significantly correlated with the short-term prognosis of patients. The Meta analysis of 20 studies showed that 31 PTE patients exhibited the elevated troponin levels. The determination of troponin and definition of abnormal value varied largely among different studies. The significantly increased troponin was also associated with the increased short-term all-cause mortality (OR = 52, 95% CI = 3.3%-84%) and PTE-related mortality (OR = 9.4, 95% CI = 4.1%-21.5%). The mortalities of PTE patients with normal and abnormal troponin levels were 3.7% and 19.7% [27]. The Meta-analysis of three PE patients with stable hemodynamics showed that the short-term mortality was significantly associated with the troponin (RR = 8.3%, 95 CI = 3.6%-19.3%), the sensitivity of mortality prediction was 81%, the negative predictive value was 73%, and the positive predictive value was 75% [20]. The long-term follow-up of this study found that the plasma troponin levels might reflect the long-term prognosis. Moreover, Stein et al. [28] and Thielmann et al [29] also found that the combination of cTnI positive and right ventricular dilation had a higher value towards the PTE prognosis. The troponin was the sensitive and specific indicator that could evaluate the ischemic myocardial injury, when this value increased, the mortality also significantly increased.
In addition, age, basic diseases (cancer, heart failure, hyperlipidemia, chronic lung disease, etc.), poor control and DVT could all affect the long-term prognosis of PTE patients [16,20]. Certain prospective study had already demonstrated that the simultaneous existence of ultrasound diagnosed deep venous thrombosis was an independent predictor of poor prognosis towards the PE patients, and compared with the patients without deep vein thrombosis, the short-term overall mortality and PE-related mortality of former PE patients were increased by 2 to 4 times [30]. The univariate analysis of this study found that the above factors could affect the occurrence of re-embolism, death and CTEPH, but the multivariate analysis revealed no statistical significance among these factors, which needed the larger clinical studies in future to further confirm its role in the PTE prognosis.
In summary, this study and a number of domestic and foreign studies all considered that the idiopathic PTe, RVD, D-dimer positive, anticoagulation treatment < 3 months, cTnI positive and post-treatment PASP > 40 mmHg were the important factors that would affect the long-term prognosis towards the PTE patients. Besides the effective anticoagulant therapy, the patients with the above factors should be performed the essential appropriate precautions and active education.
Acknowledgements
This study was supported by Hebei Province Natural Science Fund Project (H2013206403).
Disclosure of conflict of interest
None.
References
- 1.Palareti G. Recurrent venous thromboembolism: what is the risk and how to prevent it. Scientifica. 2012;2012:391734. doi: 10.6064/2012/391734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein SJ, Vedantham S. Acute deep vein thrombosis cases in the real world. Semin Intervent Radiol. 2012;29:23–28. doi: 10.1055/s-0032-1302448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farzamnia H, Rabiei K, Sadeghi M, Roghani F. The predictive factors of recurrent deep vein thrombosis. ARYA Atheroscler. 2011;7:123–128. [PMC free article] [PubMed] [Google Scholar]
- 4.Eichinger S, Weltermann A, Minar E, Stain M, Schönauer V, Schneider B, Kyrle PA. Symptomatic pulmonary embolism and the risk of recurrent venous thromboembolism. Arch Intern Med. 2004;164:92–96. doi: 10.1001/archinte.164.1.92. [DOI] [PubMed] [Google Scholar]
- 5.Bertoletti L, Quenet S, Laporte S, Sahuquillo JC, Conget F, Pedrajas JM, Martin M, Casado I, Riera-Mestre A, Monreal M RIETE Investigators. Pulmonary embolism and 3-month outcomes in 4036 patients with venous thromboembolism and chronic obstructive pulmonary disease: data from the RIETE registry. Respir Res. 2013;14:75. doi: 10.1186/1465-9921-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim NH, Delcroix M, Jenkins DP, Channick R, Dartevelle P, Jansa P, Lang I, Madani MM, Ogino H, Pengo V, Mayer E. Chronic thromboembolic pulmonary hypertension. J Am Coll Cardiol. 2013;62:D92–99. doi: 10.1016/j.jacc.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 7.Toshner M, Pepke-Zaba J. Chronic thromboembolic pulmonary hypertension: time for research in pathophysiology to catch up with developments in treatment. F1000Prime Rep. 2014;6:38. doi: 10.12703/P6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, Albanese P, Biasiolo A, Pegoraro C, Iliceto S, Prandoni P Thromboembolic Pulmonary Hypertension Study Group. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350:2257–2264. doi: 10.1056/NEJMoa032274. [DOI] [PubMed] [Google Scholar]
- 9.Tricotel A, Raguideau F, Collin C, Zureik M. Estimate of venous thromboembolism and related-deaths attributable to the use of combined oral contraceptives in france. PLoS One. 2014;9:e93792. doi: 10.1371/journal.pone.0093792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352–2361. doi: 10.1001/jama.293.19.2352. [DOI] [PubMed] [Google Scholar]
- 11.Zhu L, Yang Y, Wu Y, Zhai Z, Wang C. Value of right ventricular dysfunction for prognosis in pulmonary embolism. Int J Cardiol. 2008;127:40–45. doi: 10.1016/j.ijcard.2007.06.093. [DOI] [PubMed] [Google Scholar]
- 12.Klok FA, van Kralingen KW, van Dijk AP, Heyning FH, Vliegen HW, Huisman MV. Prospective cardiopulmonary screening program to detect chronic thromboembolic pulmonary hypertension in patients after acute pulmonary embolism. Haematologica. 2010;95:970–975. doi: 10.3324/haematol.2009.018960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta S, Helmersen D, Provencher S, Hirani N, Rubens FD, De Perrot M, Blostein M, Boutet K, Chandy G, Dennie C, Granton J, Hernandez P, Hirsch AM, Laframboise K, Levy RD, Lien D, Martel S, Shoemaker G, Swiston J, Weinkauf J Canadian Thoracic Society Pulmonary Vascular Disease-CTEPH CPG Development Committee; Canadian Thoracic Society Canadian Respiratory Guidelines Committee. Diagnostic evaluation and management of chronic thromboembolic pulmonary hypertension: a clinical practice guideline. Can Respir J. 2010;17:301–334. doi: 10.1155/2010/704258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poli D, Grifoni E, Antonucci E, Arcangeli C, Prisco D, Abbate R, Miniati M. Incidence of recurrent venous thromboembolism and of chronic thromboembolic pulmonary hypertension in patients after a first episode of pulmonary embolism. J Thromb Thrombolysis. 2010;30:294–299. doi: 10.1007/s11239-010-0452-x. [DOI] [PubMed] [Google Scholar]
- 15.Ageno W, Turpie AG, Steidl L, Ambrosini F, Cattaneo R, Codari RL, Nardo B, Venco A. Comparison of a daily fixed 2.5 mg warfarin dose with a 5 mg, international normalized ratio adjusted, warfarin dose initially following heart valve replacement. Am J Cardiol. 2001;88:40–44. doi: 10.1016/s0002-9149(01)01582-x. [DOI] [PubMed] [Google Scholar]
- 16.Marcucci M, Iorio A, Douketis J. Management of patients with unprovoked venous thromboembolism: an evidence-based and practical approach. Curr Treat Options Cardiovasc Med. 2013;15:224–239. doi: 10.1007/s11936-012-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heit JA. Predicting the risk of venous thromboembolism recurrence. Am J Hematol. 2012;87:S63–67. doi: 10.1002/ajh.23128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spencer FA, Gore JM, Lessard D, Douketis JD, Emery C, Goldberg RJ. Patient outcomes after deep vein thrombosis and pulmonary embolism: the Worcester Venous Thromboembolism Study. Arch Intern Med. 2008;168:425–430. doi: 10.1001/archinternmed.2007.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meneveau N, Ming LP, Séronde MF, Mersin N, Schiele F, Caulfield F, Bernard Y, Bassand JP. Inhospital and long term outcome after submassive and massive pulmonary embolism submitted to thrombolytic therapy. Eur Heart J. 2003;24:1447–1454. doi: 10.1016/s0195-668x(03)00307-5. [DOI] [PubMed] [Google Scholar]
- 20.Kang DK, Thilo C, Schoepf UJ, Barraza JM Jr, Nance JW Jr, Bastarrika G, Abro JA, Ravenel JG, Costello P, Goldhaber SZ. CT signs of right ventricular dysfunction: prognostic role in acute pulmonary embolism. JACC Cardiovasc Imaging. 2011;4:841–849. doi: 10.1016/j.jcmg.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Boukantar M, Lim P, Mitchell-Heggs L. Right ventricular thrombus and pulmonary embolism in patient with anterior myocardial infarction. Eur Heart J. 2010;31:2870. doi: 10.1093/eurheartj/ehq274. [DOI] [PubMed] [Google Scholar]
- 22.Grau E, Tenías JM, Soto MJ, Gutierrez MR, Lecumberri R, Pérez JL, Tiberio G RIETE Investigators. D-dimer levels correlate with mortality in patients with acute pulmonary embolism: Findings from the RIETE registry. Crit Care Med. 2007;35:1937–1941. doi: 10.1097/01.CCM.0000277044.25556.93. [DOI] [PubMed] [Google Scholar]
- 23.Cosmi B, Legnani C, Tosetto A, Pengo V, Ghirarduzzi A, Testa S, Prisco D, Poli D, Tripodi A, Marongiu F, Palareti G PROLONG Investigators (on behalf of Italian Federation of Anticoagulation Clinics) Usefulness of repeated D-dimer testing after stopping anticoagulation for a first episode of unprovoked venous thromboembolism: the PROLONG II prospective study. Blood. 2010;115:481–488. doi: 10.1182/blood-2009-08-237354. [DOI] [PubMed] [Google Scholar]
- 24.Palareti G, Cosmi B, Legnani C, Tosetto A, Brusi C, Iorio A, Pengo V, Ghirarduzzi A, Pattacini C, Testa S, Lensing AW, Tripodi A PROLONG Investigators. D-Dimer testing to determine the durationof anticoagulation therapy. N Engl J Med. 2006;355:1780–1789. doi: 10.1056/NEJMoa054444. [DOI] [PubMed] [Google Scholar]
- 25.Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G. Oral anticoagulant therapy: Antithrombotic Therapy and Prevent-ion of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e44S–88S. doi: 10.1378/chest.11-2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Becattini C, Vedovati MC, Agnelli G. Prognostic value of troponins in acute pulmonary embolism: a meta-analysis. Circulation. 2007;116:427–433. doi: 10.1161/CIRCULATIONAHA.106.680421. [DOI] [PubMed] [Google Scholar]
- 27.Sanchez O, Trinquart L, Colombet I, Durieux P, Huisman MV, Chatellier G, Meyer G. Prognostic value of right ventricular dysfunction in patients with haemodynamically stable pulmonary embolism: a systematic review. Eur Heart J. 2008;29:1569–1577. doi: 10.1093/eurheartj/ehn208. [DOI] [PubMed] [Google Scholar]
- 28.Stein PD, Janjua M, Matta F, Pathak PK, Jaweesh F, Alrifai A, Chughtai HL. Prognosis based on creatine kinase isoenzyme MB, cardiac troponin I, and right ventricular size in stable patients with acute pulmonary embolism. Am J Cardiol. 2011;107:774–777. doi: 10.1016/j.amjcard.2010.10.061. [DOI] [PubMed] [Google Scholar]
- 29.Thielmann M, Pasa S, Wendt D, Price V, Marggraf G, Neuhäuser M, Piotrowski A, Jakob H. Prognostic significance of cardiac troponin I on admission for surgical treatment of acute pulmonary embolism: a single-centre experience over more than 10 years. Eur J Cardiothorac Surg. 2012;42:951–957. doi: 10.1093/ejcts/ezs122. [DOI] [PubMed] [Google Scholar]
- 30.Nounou HA, Deif MM, Shalaby MA. Effect of flaxseed supplementation and exercise training on lipid profile, oxidative stress and inflammation in rats with myocardial ischemia. Lipids Health Dis. 2012;11:129. doi: 10.1186/1476-511X-11-129. [DOI] [PMC free article] [PubMed] [Google Scholar]


