Abstract
Objectives
Among 11–12 year-old girls who received the human papillomavirus (HPV) vaccine, we explored, over the subsequent 30 months: 1) trajectories of knowledge about HPV/HPV vaccines and vaccine-related risk perceptions; 2) whether knowledge and risk perceptions impacted sexual attitudes and sexual experience; and 3) whether mothers, clinicians, and media influenced girls’ risk perceptions, attitudes, and behavior.
Methods
Girls and mothers (n=25 dyads) completed separate, semi-structured interviews within 2 days of, and 6, 18, and 30 months after, their first HPV vaccine dose. Knowledge, risk perceptions related to HPV and other sexually transmitted infections (STIs), and attitudes about sexual behaviors were assessed. Sexual experience was assessed at girls’ 30 month interviews. Clinicians completed interviews at baseline. Transcribed interviews were analyzed using framework analysis.
Results
Girls’ baseline knowledge was poor but often improved with time. Most girls (n=18) developed accurate risk perceptions about HPV but only half (n=12) developed accurate risk perceptions about other STIs by 30 months. The vast majority of girls thought that safer sex was still important, regardless of knowledge, risk perceptions, or sexual experience. Girls whose HPV knowledge was high at baseline or increased over time tended to articulate accurate risk perceptions; those who were able to articulate accurate risk perceptions tended to report not having initiated sexual activity. Girls whose mothers demonstrated higher knowledge and/or communication about HPV vaccination tended to articulate accurate risk perceptions, whereas clinicians and media exposure did not appear to influence risk perceptions.
Conclusions
Higher knowledge about HPV vaccines among mothers and girls was linked with more accurate risk perceptions among girls. Clinicians may play an important role in providing education about HPV vaccines to mothers and girls.
Keywords: Adolescents, Human papillomavirus (HPV) vaccine, Knowledge, Sexual attitudes, Mothers, Clinicians
Introduction
Human papillomavirus (HPV) vaccines are a highly effective strategy for decreasing rates of HPV-associated disease.1–4 Despite recommendations for routine HPV vaccination,5,6 recent studies demonstrate suboptimal vaccination rates among girls,7 which may be due to parents not accepting or clinicians not recommending HPV vaccines.8 Low vaccine acceptance and recommendation may be due to concerns held by some parents9,10 and physicians11,12 that vaccination may lead to inaccurate risk perceptions (such as girls believing themselves to be at lower risk for sexually transmitted infections [STIs] other than HPV after vaccination) and subsequent riskier sexual behaviors.
Although studies suggest that HPV vaccination does not lead to riskier sexual behaviors,13–16 little is known about the development of girls’ HPV vaccine-related risk perceptions and the association of risk perceptions with sexual attitudes and behaviors following vaccination. Few studies have examined girls in the target age group for vaccination or included data from their mothers and clinicians. Because risk perceptions about STIs may predict sexual behaviors,17 understanding how risk perceptions develop and change after vaccination may provide insight into how clinicians can help girls to develop or maintain accurate risk perceptions. Additionally, if risk perceptions do not change or are not related to changes in sexual attitudes and behaviors after vaccination, this information may provide reassurance to parents and clinicians, leading to increased vaccine recommendation and uptake. Other factors that may influence risk perceptions and sexual attitudes after vaccination include girls’ knowledge about HPV and HPV vaccines; parent and clinician knowledge, attitudes, and communication with girls about HPV vaccines; and girls’ exposure to media coverage about HPV vaccines. Little is known about post-vaccination attitudes among girls in the target age range for HPV vaccination; such data are essential to provide the evidence base for large-scale survey studies to determine whether vaccination affects sexual behaviors.18 Therefore, the aims of this 30-month study were to use qualitative methods to describe the following, among a sample of 11–12 year-old girls receiving the HPV vaccine, their mothers and clinicians: 1) trajectories of girls’ knowledge about HPV and HPV vaccines and risk perceptions after vaccination; 2) the relationship between girls’ knowledge and risk perceptions; 3) the relationship between girls’ knowledge, risk perceptions, and subsequent sexual attitudes and experience; and 4) the relationship between maternal knowledge and communication about HPV vaccines, clinician communication about HPV vaccines, and media messages about HPV vaccines and girls’ risk perceptions, sexual attitudes, and behavior.
Methods
This qualitative study was conducted between 6/2008 and 11/2012. Using an interview guide consisting of open- and close-ended questions, a trained interviewer conducted individual, face-to-face, semi-structured interviews with 11–12 year-old girls, their mothers, and their clinicians. In accordance with recommendations for sampling in qualitative research, recruitment was terminated when thematic saturation was achieved.19,20 Thirty-three girls, 32 mothers, and 19 clinicians were recruited from two suburban, private, pediatric practices and one urban, academic pediatric primary care practice. Girls and mothers completed interviews within 2 days of girls’ receiving their first HPV vaccine dose and 6, 18, and 30 months after the first dose. Included in this analysis are interviews with the 25 girls who attended the 30 month visit and at least 3 of the 4 total visits. Of these, 21 girls completed all visits; 1 girl completed the baseline, 6 month, and 30 month visits; and 3 girls completed the baseline, 18 month, and 30 month visits. Each girl’s clinician completed one interview at baseline. Each interview with girls assessed knowledge about HPV and HPV vaccines, risk perceptions related to HPV and other STIs, attitudes about sexual behaviors, and perceived influence of mothers, clinicians, and media on risk perceptions. Risk perceptions were assessed by asking the girl whether she perceived that the vaccine decreased her risk of HPV and other STIs. Sexual attitudes were assessed by asking the girl whether her risk perceptions about HPV and other STIs would influence her decisions about sexual behaviors. Girls were asked about the content of maternal and clinician communication about HPV vaccines, the content of any consumed media related to HPV vaccines, and the perceived influence of these factors on the girls’ vaccine-related risk perceptions. During the 30 month interview, sexual experience was assessed by asking the girl if she had ever had sex. Interviews of mothers assessed knowledge about HPV/HPV vaccines, communication with the daughter about HPV vaccines, and perception of the daughter’s vaccine-related risk perceptions. Interviews of clinicians assessed HPV vaccine-related knowledge, attitudes, and communication with the girl and mother. The hospital institutional review board approved this research.
Recordings were transcribed by an independent transcriptionist. The interviewer’s field notes were added to transcripts before analysis. The qualitative data was systematically analyzed using Framework Analysis approach.21,22 Each investigator (TKM, LEW, JAK) read and coded the transcripts independently. The investigators met to develop consensus on coding and data interpretation. First, we assessed knowledge (number of vaccine doses required, what diseases vaccination may prevent), vaccine-related risk perceptions with respect to HPV and other STIs (i.e. beliefs about whether the vaccine protects against HPV and/or other STIs), and attitudes toward sexual behaviors for each girl at each visit. Accurate risk perceptions were defined as a girl reporting that she was more protected against HPV and not protected from other STIs after vaccination. Based on these analyses, we described three trajectories over the 30-month study period: adolescent knowledge (i.e. did knowledge increase, decrease, remain unchanged), vaccine-related risk perceptions with respect to HPV and STIs (i.e. did the accurateness of HPV-related and STI-related risk perceptions change), and sexual attitudes (i.e. perceived need to practice safer sexual behaviors). For each girl, we first categorized trajectories of knowledge into: i) high knowledge throughout; ii) knowledge improving over time; iii) low knowledge throughout; and iv) inconsistent knowledge (knowledge varied over time). HPV and STI risk perceptions were categorized into: i) inaccurate/inability to articulate risk perceptions; ii) consistently accurate over time; iii) increasingly accurate over time; and iv) inconsistent. Second, we assessed the relationship between adolescent knowledge and risk perceptions over time. Third, we assessed the relationship between knowledge, risk perceptions, and sexual attitudes and experience over time. Fourth, we explored whether maternal and clinician knowledge and attitudes, communication between girls, mothers, and clinicians (as reported by all three), and media exposure (as reported by girls) were related to girls’ knowledge, risk perceptions, and sexual attitudes. Mothers and clinicians were considered influential if similar themes were reported by the girl/mother or clinician/girl dyad, respectively. A conceptual model depicting the study findings was developed.
Results
Thirteen girls were recruited at suburban practices; 12 were recruited from the urban practice. All girls recruited from the suburban practices were white; all girls recruited from the urban practice were black. Findings related to 1) trajectories of knowledge and risk perceptions, 2) influence of knowledge on risk perceptions, 3) influence of knowledge and risk perceptions on sexual attitudes and experience, and 4) influence of mothers, clinicians, and media on girls’ knowledge, risk perceptions, and sexual attitudes are described below.
Trajectories of Knowledge and Risk Perceptions
Trajectories of HPV and HPV Vaccine Knowledge
Baseline knowledge was generally low, although some girls gained knowledge over time. Half of girls (12/25) demonstrated good or improving knowledge; half (13/25) demonstrated low or inconsistent knowledge. Nine of 13 suburban girls demonstrated good or improving knowledge as compared to only 3 of 12 urban girls. Improvement in knowledge appeared to be related to education that the girl received outside of the clinical setting, such as education received from a parent or in school, as evidenced by the reports of many girls of little clinician communication about the vaccine. Key knowledge points that girls identified included: a) HPV is an STI, b) HPV is sexually transmitted, and c) the vaccine prevents cancer/cervical cancer. Several misperceptions about HPV and the vaccine were noted, including: a) the type of cancer that the vaccine prevents (e.g., erroneously reported as breast cancer); b) what STI the vaccine prevents (e.g., erroneously reported as HIV/AIDS); c) the vaccine is therapeutic; and d) how HPV is transmitted (e.g., erroneously reported to be through smoking).
Trajectories of Risk Perceptions
Most girls (18/25) had accurate or increasingly accurate HPV-related risk perceptions, while 7/25 girls had inconsistent or inaccurate risk perceptions or were unable to articulate risk perceptions. Eleven of 13 suburban girls had accurate HPV risk perceptions by the end of the study as compared to 7 of 12 urban girls. In contrast, half of girls (13/25) had inaccurate or inconsistent STI-related risk perceptions by the 30 month visit (“I think if you prevent HPV, you can prevent lesser diseases [STIs].”), and half of girls (12/25) had accurate STI-related risk perceptions (“I don’t think that it [HPV vaccine] stops the others [STIs] because… it only stops this [HPV]. It doesn’t stop the other ones.”) These proportions were similar in suburban and urban girls.
Influence of Knowledge on Risk Perceptions
Girls who demonstrated consistently high or improving knowledge tended to articulate accurate HPV-related risk perceptions. Girls with high knowledge tended to articulate accurate STI-related risk perceptions; in contrast, those with low knowledge tended to articulate inaccurate risk perceptions. As knowledge increased over time, risk perceptions often became more accurate.
Influence of Knowledge and Risk Perceptions on Sexual Attitudes and Behavior
Seven girls specifically linked knowledge about HPV and the vaccine with safer sexual behavior: “I also believe that STDs, not all you can get rid of. And this [HPV vaccine] is meant to prevent some. So I still think it’s [having sex is] a bad decision.” Many girls and mothers believed that vaccination and vaccine-related risk perceptions would not influence girls’ sexual behaviors; one girl reported, “I wouldn’t not use protection just because I got the shot.” Although 20 girls endorsed feeling safer having sex following vaccination, the vast majority of these girls (18/20) felt unsafe having unprotected sex (i.e. without a condom). Even girls with poor knowledge and inaccurate risk perceptions reported that safer sex was important. By the conclusion of the study, 6/25 girls had initiated sexual activity; all six of them endorsed a belief in safer sex. None of the sexually experienced girls demonstrated high/increasing knowledge and accurate/improving risk perceptions. In contrast, over 1/3 of sexually inexperienced girls demonstrated high/increasing knowledge and accurate/improving risk perceptions. Only two girls maintained high knowledge throughout the study; both girls had accurate risk perceptions, expressed the importance of safer sex, and were not sexually experienced.
Influence of Mothers, Clinicians, and Media on Girls’ Knowledge, Risk Perceptions, and Sexual Attitudes
Influence of Mothers
Good maternal knowledge and/or communication, as reported by girls and mothers, were related to accurate risk perceptions among girls (14/25), while poor maternal knowledge and/or communication were related to inaccurate or poor articulation of risk perceptions (7/25). Vaccination was described as protective, not just because vaccination prevented HPV but also because of the educational opportunity provided by the vaccination visit: “It [Getting the vaccine] made her smarter about it [delaying sex]. And just in case she doesn’t wait, then she needs to do something to protect herself from things.” Vaccination was seen as an opportunity to provide sexual health education to the girl (n=3): “We had the sex talk… So it definitely gave me an opportunity whereas before I’m not sure I would have… I would’ve had the conversation with her, but it gave me an excuse to have it.” Only half of the sexually experienced girls (3/6) reported that their mothers influenced their risk perceptions; in contrast, all of the sexually inexperienced girls noted that communication with their mothers was influential to their risk perceptions.
Influence of Clinicians
In half of girls (12/25), poor clinician communication, as evidenced by both clinicians and girls reporting little clinician communication about the vaccine, appeared to influence the girl’s inability to articulate risk perceptions. Although 12 girls reported that their clinician was influential in the formation of their risk perceptions, only 3 girls demonstrated evidence of this influence (i.e., girl recalled information imparted by the clinician and discussed this information when describing her risk perceptions).
Influence of Media
Only one girl reported that the media was influential. However, her media exposure consisted of information that was obtained from the clinician’s office and an online group of which the girl was a member. Another girl reported using the internet with her mother in order to learn more about the vaccine. No girl reported that television or commercial print media was influential in the formation of her risk perceptions.
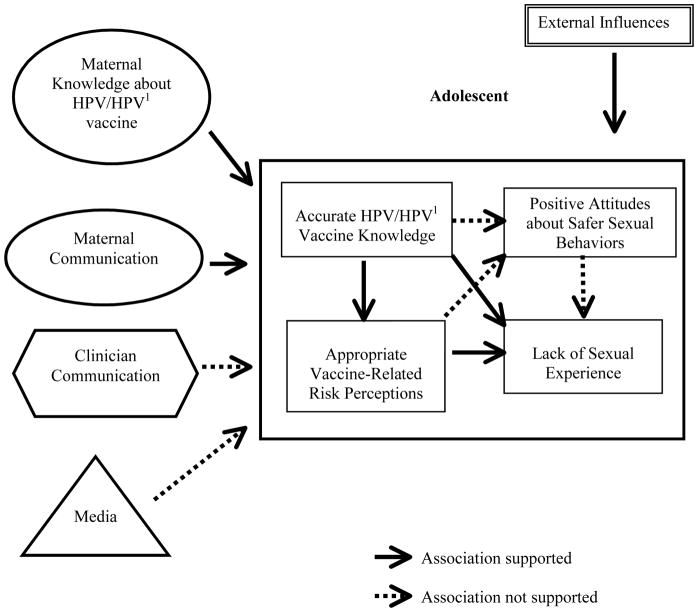
The conceptual model is shown in the Figure, demonstrating the key relationships betweenthemes as described above.
Figure 1.
Conceptual Model: Relationships between Key Themes
1. HPV: Human papillomavirus
Accurate adolescent knowledge about HPV and the HPV vaccine is linked to appropriate vaccine-related risk perceptions. Both accurate knowledge about HPV and the HPV vaccine and appropriate vaccine-related risk perceptions were linked to lack of sexual experience. Maternal knowledge about HPV and the HPV vaccine, maternal communication, and other external influences (such as school) also influenced adolescent HPV and HPV vaccine knowledge and vaccine-related risk perceptions.
Discussion
We examined trajectories of knowledge and risk perceptions, the impact of knowledge and risk perceptions on sexual attitudes and sexual experience, and the influence of mothers, clinicians, and media on risk perceptions and sexual attitudes among 11–12 year old girls who received the HPV vaccine. This is the first study, to our knowledge, to examine longitudinal changes in risk perceptions, sexual attitudes, and sexual experience among girls who are in the target age group for HPV vaccination, and one of the first to include data collected from mothers and clinicians. Overall, we did not find evidence that HPV vaccination led to changes in girls’ sexual attitudes or riskier sexual behaviors. On the contrary, we found that mothers and girls generally believed that vaccination would lead to safer sexual behaviors because of the education provided during the vaccination visit.
Girls generally had poor knowledge and inaccurate risk perceptions at baseline, particularly with respect to perceived risk of STIs other than HPV. We found that girls with high knowledge tended to be able to articulate accurate risk perceptions, whereas girls with poor knowledge were unable to articulate accurate risk perceptions, implying that sufficient knowledge was important in the formation of accurate risk perceptions. We observed differences in knowledge and risk perceptions between suburban and urban girls, which may be due to differences in health literacy23,24 or girls not seeing a consistent provider at the urban practice.25,26 Our data suggest that high knowledge may be related to both accurate risk perceptions and not initiating sexual activity. However, the vast majority of girls, regardless of knowledge, risk perceptions, or sexual experience, reported that condom use during sex was important. Our findings are consistent with prior studies demonstrating poor HPV knowledge among girls27–31 and women.27,32–34 This poor knowledge, combined with our findings that better knowledge about HPV and HPV vaccines was linked with more accurate risk perceptions and sexual inexperience, suggests that clinicians, parents, and others are missing opportunities to educate girls and ensure the development of accurate risk perceptions and safer sexual behaviors.
Our findings suggest that receiving HPV vaccination is unlikely to change girls’ sexual attitudes. Almost all of the girls reported plans to practice safer sexual behaviors and reported feeling unsafe having unprotected sex after vaccination. Furthermore, in contrast to reports of parental concerns that vaccination may lead to changes in risk perceptions and riskier sexual behaviors, we found that most mothers believed that vaccinated girls would be less likely to practice riskier behaviors due to the education that girls received with vaccination. Some mothers even noted that they used the vaccination visit as an opportunity to talk about their family’s values related to sex and provide sexual health education to their daughter. In a prior study, nearly half of mothers who had talked to their daughters about the HPV vaccine reported that the vaccine discussion led to a discussion about sex.35 The results of this study, combined with those of previous studies,13–16,36 suggest that clinicians can reassure parents that HPV vaccination does not lead to riskier sexual attitudes and that in fact the vaccination visit can be utilized by clinicians to promote healthier sexual behaviors.
Most mothers seemed to be influential in the development of girls’ knowledge and risk perceptions. Girls whose mothers had higher knowledge about HPV and communicated with their daughters about HPV vaccines demonstrated higher knowledge and more accurate risk perceptions. The influence of mothers is likely in part due to the sustained exposure that girls have to their mothers’ communication about sexual health and values.37 Because parents influence their children’s sexual attitudes and behaviors, clinicians should provide accurate information and resources to parents about sexual health38 so that parents can educate their children. Encouraging mothers to discuss safer sexual behaviors and convey their values to their daughters may lead to increased knowledge and development of accurate risk perceptions among girls.
In this study clinicians did not appear to be very influential in shaping girls’ knowledge, risk perceptions, or sexual attitudes. Girls reported that little vaccine-related information was communicated to them at the vaccination visit, which may not differ from their experiences with other routine vaccines. Most girls gained knowledge about HPV and the vaccine over time, but this appeared to be related to education received outside of the clinician’s office. Clinicians may have more impact on girls’ knowledge and risk perceptions by discussing HPV, the vaccine, and sexual health with girls, and repeating this information at multiple visits. These topics can be incorporated into clinicians’ ongoing discussions of sexuality and reproductive health with children, adolescents, and parents, as recommended by clinical guidelines.38
Girls reported that print and television media did not influence their knowledge or risk perceptions. Among girls who were shown a television advertisement for the HPV vaccine, very few recalled any key messages about HPV or the vaccine.29 However, one girl in our study reported that her participation in an online, interactive group was influential. Future studies should examine whether media other than print or television, such as the internet, could be tools to facilitate education of, and communication between, parents and adolescents.
This study is subject to several limitations. Apparent low baseline knowledge or inability to articulate risk perceptions among girls may have been related to discomfort or inexperience talking about these topics. Second, girls’ knowledge may have been inconsistent because girls may retain information immediately after the clinic visit; this knowledge may diminish over time.39 Third, some girls may have reported perceived need for safer sexual behaviors because safer sex is socially desirable. We attempted to minimize this by using open-ended questions and a non-judgmental approach. Finally, girls were asked directly about whether they perceived an influence of the media on their risk perceptions. Because girls may not be aware that they had been influenced by media, this may result in an underestimation of the impact of media on the development of risk perceptions among girls. A concern sometimes raised regarding qualitative studies is that the findings are not generalizable. However, the goal of qualitative research is not to generate generalizable results but instead to gain an in-depth understanding of a phenomenon or an experience - in this study, risk perceptions, sexual attitudes, and sexual behaviors after HPV vaccination.
Conclusions
Among 11–12 year-old girls who received the HPV vaccine, the vast majority thought that safer sex was still important, regardless of knowledge, risk perceptions, or sexual experience. Because better knowledge among girls and mothers was linked with girls having accurate risk perceptions, clinicians should provide education to girls and their mothers about HPV and the vaccine, which may lead to the development of accurate long-term risk perceptions among girls and reinforcement of girls’ decisions to practice safer sexual behaviors.
Highlights.
Girls with higher HPV and HPV vaccine knowledge had more accurate risk perceptions.
Girls with accurate risk perceptions had healthier sexual attitudes/behaviors.
Mothers’ knowledge and communication affected girls’ knowledge and risk perceptions.
The majority of girls reported that safer sex was still important.
Acknowledgments
The authors thank Susan Glynn, B.A., for her recruitment, interviews, and transcript review. We also thank the girls, their mothers, and the clinicians who participated in the study. This study was funded by National Institutes of Health (NIAID) grant R01073713 (Kahn); Cincinnati Children’s Research Foundation Procter Scholar Award (Mullins); National Institutes of Health (NICHD) grant K23HD072807 (Mullins).
Abbreviations
- HPV
human papillomavirus
- STI
sexually transmitted infections
- GU
genitourinary
Footnotes
Contributors’ Statement Page
Tanya L. K. Mullins: Dr. Mullins carried out analyses, drafted the initial manuscript, made revisions, and approved the final manuscript as submitted.
Lea E. Widdice: Dr. Widdice carried out analyses, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Susan L. Rosenthal: Dr. Rosenthal conceptualized and designed the study, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Gregory D. Zimet: Dr. Zimet conceptualized and designed the study, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Jessica A. Kahn: Dr. Kahn conceptualized and designed the study, supervised data collection, analyzed the data, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
All of the authors have approved the final article.
Conflict of Interest Statement: Dr. Mullins and Dr. Widdice have no financial disclosures relevant to this research to report. Dr. Rosenthal serves as an unfunded co-investigator on an investigator-initiated grant from Pfizer. Dr. Zimet has been an investigator on investigator-initiated HPV vaccination grants funded by Merck and received an unrestricted cervical cancer prevention program development grant from GSK. Dr. Kahn served as the chair of a grant review committee for a grant program sponsored by the Society for Adolescent Health and Medicine, which provided funding for public health demonstration projects to improve adolescent vaccination. Funding for the grant program was provided by Merck. Dr. Kahn has also served as co-chair of two clinical trials of an HPV vaccine in HIV-infected individuals; these studies were funded primarily by the NIH, but Merck provided vaccines and immunogenicity testing.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Garland SM, Hernandez-Avila M, Wheeler CM, et al. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356(19):1928–1943. doi: 10.1056/NEJMoa061760. [DOI] [PubMed] [Google Scholar]
- 2.Group FIS. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356(19):1915–1927. doi: 10.1056/NEJMoa061741. [DOI] [PubMed] [Google Scholar]
- 3.Joura EA, Leodolter S, Hernandez-Avila M, et al. Efficacy of a quadrivalent prophylactic human papillomavirus (types 6, 11, 16, and 18) L1 virus-like-particle vaccine against high-grade vulval and vaginal lesions: a combined analysis of three randomised clinical trials. Lancet. 2007;369(9574):1693–1702. doi: 10.1016/S0140-6736(07)60777-6. [DOI] [PubMed] [Google Scholar]
- 4.Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365(17):1576–1585. doi: 10.1056/NEJMoa1010971. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease C and Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2010;59(20):626–629. [PubMed] [Google Scholar]
- 6.Markowitz LE, Dunne EF, Saraiya M, et al. Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56(RR-2):1–24. [PubMed] [Google Scholar]
- 7.Stokley S, Jeyarajah J, Yankey D, et al. Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014 -United States. MMWR Morb Mortal Wkly Rep. 2014;63(29):620–624. [PMC free article] [PubMed] [Google Scholar]
- 8.Vadaparampil ST, Malo TL, Kahn JA, et al. Physicians’ human papillomavirus vaccine recommendations, 2009 and 2011. Am J Prev Med. 2014;46(1):80–84. doi: 10.1016/j.amepre.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahn JA, Cooper HP, Vadaparampil ST, et al. Human papillomavirus vaccine recommendations and agreement with mandated human papillomavirus vaccination for 11-to-12-year-old girls: a statewide survey of Texas physicians. Cancer Epidemiol Biomarkers Prev. 2009;18(8):2325–2332. doi: 10.1158/1055-9965.EPI-09-0184. [DOI] [PubMed] [Google Scholar]
- 11.Quinn GP, Murphy D, Malo TL, Christie J, Vadaparampil ST. A national survey about human papillomavirus vaccination: what we didn’t ask, but physicians wanted us to know. J Pediatr Adolesc Gynecol. 2012;25(4):254–258. doi: 10.1016/j.jpag.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sussman AL, Helitzer D, Sanders M, Urquieta B, Salvador M, Ndiaye K. HPV and cervical cancer prevention counseling with younger adolescents: implications for primary care. Ann Fam Med. 2007;5(4):298–304. doi: 10.1370/afm.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bednarczyk RA, Davis R, Ault K, Orenstein W, Omer SB. Sexual activity-related outcomes after human papillomavirus vaccination of 11- to 12-year-olds. Pediatrics. 2012;130(5):798–805. doi: 10.1542/peds.2012-1516. [DOI] [PubMed] [Google Scholar]
- 14.Liddon NC, Leichliter JS, Markowitz LE. Human papillomavirus vaccine and sexual behavior among adolescent and young women. Am J Prev Med. 2012;42(1):44–52. doi: 10.1016/j.amepre.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Mayhew A, Mullins TL, Ding L, et al. Risk perceptions and subsequent sexual behaviors after HPV vaccination in adolescents. Pediatrics. 2014;133(3):404–411. doi: 10.1542/peds.2013-2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rysavy MB, Kresowik JD, Liu D, Mains L, Lessard M, Ryan GL. Human papillomavirus vaccination and sexual behavior in young women. J Pediatr Adolesc Gynecol. 2014;27(2):67–71. doi: 10.1016/j.jpag.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Champion VL, Skinner CS. The Health Belief Model. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4. San Francisco: Jossey-Bass; 2008. pp. 45–65. [Google Scholar]
- 18.Allen JD, Coronado GD, Williams RS, et al. A systematic review of measures used in studies of human papillomavirus (HPV) vaccine acceptability. Vaccine. 2010;28(24):4027–4037. doi: 10.1016/j.vaccine.2010.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuzel AJ. Sampling in Qualitative Inquiry. In: Crabtree B, Miller WL, editors. Doing Qualitative Research. Sage; 1999. pp. 33–45. [Google Scholar]
- 20.Kvale S, Brinkmann S. Interviews. 2. Los Angeles: Sage; 2009. [Google Scholar]
- 21.Kahn JA, Slap GB, Bernstein DI, et al. Personal meaning of human papillomavirus and Pap test results in adolescent and young adult women. Health Psychol. 2007;26(2):192–200. doi: 10.1037/0278-6133.26.2.192. [DOI] [PubMed] [Google Scholar]
- 22.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Brugess R, editors. Analyzing Qualitative Data. Routledge; 1994. pp. 173–194. [Google Scholar]
- 23.Bailey SC, Pandit AU, Yin S, et al. Predictors of misunderstanding pediatric liquid medication instructions. Fam Med. 2009;41(10):715–721. [PubMed] [Google Scholar]
- 24.Weekes CV. African Americans and health literacy: a systematic review. ABNF J. 2012;23(4):76–80. [PubMed] [Google Scholar]
- 25.Darden PM, Ector W, Moran C, Quattlebaum TG. Comparison of continuity in a resident versus private practice. Pediatrics. 2001;108(6):1263–1268. doi: 10.1542/peds.108.6.1263. [DOI] [PubMed] [Google Scholar]
- 26.McBurney PG, Gustafson KK, Darden PM. Effect of 80-hour workweek on continuity of care. Clin Pediatr (Phila) 2008;47(8):803–808. doi: 10.1177/0009922808318341. [DOI] [PubMed] [Google Scholar]
- 27.Cooper Robbins SC, Bernard D, McCaffery K, Brotherton J, Garland S, Skinner SR. “Is cancer contagious?”: Australian adolescent girls and their parents: making the most of limited information about HPV and HPV vaccination. Vaccine. 2010;28(19):3398–3408. doi: 10.1016/j.vaccine.2010.02.078. [DOI] [PubMed] [Google Scholar]
- 28.Hilton S, Smith E. I thought cancer was one of those random things. I didn’t know cancer could be caught…”: adolescent girls’ understandings and experiences of the HPV programme in the UK. Vaccine. 2011;29(26):4409–4415. doi: 10.1016/j.vaccine.2011.03.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leader AE, Cashman R, Voytek CD, Baker JL, Brawner BM, Frank I. An exploratory study of adolescent female reactions to direct-to-consumer advertising: the case of the Human Papillomavirus (HPV) Vaccine. Health Mark Q. 2011;28(4):372–385. doi: 10.1080/07359683.2011.630289. [DOI] [PubMed] [Google Scholar]
- 30.Marlow LA, Forster AS, Wardle J, Waller J. Mothers’ and adolescents’ beliefs about risk compensation following HPV vaccination. J Adolesc Health. 2009;44(5):446–451. doi: 10.1016/j.jadohealth.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 31.Miller MK, Wickliffe J, Jahnke S, Linebarger J, Humiston SG. Views on Human Papillomavirus Vaccination: A Mixed-Methods Study of Urban Youth. J Community Health. 2014 doi: 10.1007/s10900-014-9858-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friedman AL, Shepeard H. Exploring the knowledge, attitudes, beliefs, and communication preferences of the general public regarding HPV: findings from CDC focus group research and implications for practice. Health Educ Behav. 2007;34(3):471–485. doi: 10.1177/1090198106292022. [DOI] [PubMed] [Google Scholar]
- 33.Grabiel M, Reutzel TJ, Wang S, et al. HPV and HPV vaccines: the knowledge levels, opinions, and behavior of parents. J Community Health. 2013;38(6):1015–1021. doi: 10.1007/s10900-013-9725-6. [DOI] [PubMed] [Google Scholar]
- 34.Strohl AE, Mendoza G, Ghant MS, et al. Barriers to prevention: knowledge of HPV, cervical cancer, and HPV vaccinations among African American women. Am J Obstet Gynecol. 2015;212(1):65.e1–5. doi: 10.1016/j.ajog.2014.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McRee AL, Reiter PL, Gottlieb SL, Brewer NT. Mother-daughter communication about HPV vaccine. J Adolesc Health. 2011;48(3):314–317. doi: 10.1016/j.jadohealth.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hansen BT, Kjaer SK, Arnheim-Dahlstrom L, et al. Human papillomavirus (HPV) vaccination and subsequent sexual behaviour: Evidence from a large survey of Nordic women. Vaccine. 2014;32(39):4945–4953. doi: 10.1016/j.vaccine.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 37.Martino SC, Elliott MN, Corona R, Kanouse DE, Schuster MA. Beyond the “big talk”: the roles of breadth and repetition in parent-adolescent communication about sexual topics. Pediatrics. 2008;121(3):e612–618. doi: 10.1542/peds.2007-2156. [DOI] [PubMed] [Google Scholar]
- 38.American Academy of Pediatrics. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3. American Academy of Pediatrics; 2007. [Google Scholar]
- 39.Brabin L, Stretch R, Roberts SA, Elton P, Baxter D, McCann R. Survey of girls’ recall of a film providing information on human papillomavirus and cervical cancer 6 months after an offer of vaccination. Vaccine. 2010;28(25):4210–4214. doi: 10.1016/j.vaccine.2010.03.077. [DOI] [PubMed] [Google Scholar]