Summary
The Guatemalan NGO (Non-Governmental Organization) TulaSalud has implemented an m-health project in the Department of Alta Verapaz. This Department has 1.2 million inhabitants (78% living in rural areas and 89% from indigenous communities) and in 2012, had a maternal mortality rate of 273 for every 100,000 live births. This m-health initiative is based on the provision of a cell phone to community facilitators (CFs). The CFs are volunteers in rural communities who perform health prevention, promotion and care. Thanks to the cell phone, the CFs have become tele-CFs who able to carry out consultations when they have questions; send full epidemiological and clinical information related to the cases they attend to; receive continuous training; and perform activities for the prevention and promotion of community health through distance learning sessions in the Q’eqchí and/or Poqomchi’ languages. In this study, rural populations served by tele-CFs were selected as the intervention group while the control group was composed of the rural population served by CFs without Information and Communication Technology (ICT) tools. As well as the achievement of important process results (116,275 medical consultations, monitoring of 6,783 pregnant women, and coordination of 2,014 emergency transfers), the project has demonstrated a statistically significant decrease in maternal mortality (p < 0.05) and in child mortality (p = 0.054) in the intervention group compared with rates in the control group. As a result of the telemedicine initiative, the intervention areas, which were selected for their high maternal and infant mortality rates, currently show maternal and child mortality indicators that are not only lower than the indicators in the control area, but also lower than the provincial average (which includes urban areas).
Introduction
With a Human Development Index (HDI) of 0.581, Guatemala is considered one of the least developed countries in Latin America (only Haiti has a lower HDI) and ranked 133rd in the list of 161 countries included by UNDP (United Nations Development Programme) in the Human Development Report 2013.1 The Department of Alta Verapaz, one of 22 departments in the country (a department is a division of the country for administrative purposes), was chosen by the NGO TulaSalud for the development of their rural telemedicine pilot project. Alta Verapaz has nearly 1.2 million inhabitants of whom 78% live in rural areas and 89% are from indigenous communities,2 48% of whose population lives in extreme poverty. In this Department, 74 maternal deaths and 27,052 live births were registered in 2012, denoting a Maternal Mortality Ratio (MMR) of 273 deaths per 100,000 live births. With 389 deaths registered in the same year, the infant mortality rate (IMR) for children under one year of age was 14.38 deaths per 1,000 live births.
The main causes of maternal mortality in Latin America and the Caribbean are hypertensive disease (25% of total deaths), postpartum haemorrhage (21%), obstructed labour (13%), abortions (12%) and sepsis/infections (8%).3 Meanwhile, the main causes of infant mortality in developing countries are pneumonia (19%), diarrhoea (18%) and malaria (8%), followed by episodes related to pregnancy and childbirth, such as prematurity (10%), neonatal sepsis (10%) and asphyxia at birth (8%).4
TulaSalud was established in 2007 to combat high maternal and child mortality rates, and address the serious problems of access to health services in rural areas of Guatemala with indigenous communities. Inspired by the work of the EHAS Foundation (in Spanish “Enlace Hispano Americano de Salud”, in English “Hispanic American Health Link”) among rural indigenous communities,5,6 TulaSalud embarked upon a program for strengthening health care in Alta Verapaz using Information and Communication Technologies (ICT).
To support the work of community health workers is an extended strategy to curb maternal and child mortality in developing countries,7 and TulaSalud’s telemedicine work follows this action line by providing remote support to community facilitators (CFs). The CF is a volunteer from a rural community who, having received basic training and a small stipend from the Ministry of Health and Social Welfare (MSPAS), performs prevention, promotion and health care (with a kit of essential drugs) to a population of around 1,500 inhabitants. The CFs are visited by a team of health professionals (qualified nurses) approximately once a month.
The innovation introduced by TulaSalud to a sample of 125 CFs in Alta Verapaz was the provision of a cell phone which enabled them to become tele-CFs. The cell phone allows the CF to make consultations regarding issues about which they are unsure; send full epidemiological and clinical information related to the cases they attend; receive continuous training, and perform community health promotion and prevention activities through distance learning sessions in the Q ‘eqchí and/or Poqomchi’ languages.
TulaSalud also conducts other activities such as the distance training of nursing technicians (through a 3 year course) and nursing assistants (through a 1 year course) using a multi-video-conference system. This training is carried out in collaboration with the Coban School of Nursing and has involved more than 1,100 students in 29 remote locations across the country. The impact of this part of TulaSalud’s work has, however, not been included in the study presented in this paper.
The use of m-health solutions to support the primary health care system in rural areas of developing countries is a very promising trend that has been explored in several projects. In Uganda the RapidSMS system was used to manage the roll out of malaria’s rapid diagnostic test8; in Zambia a SMS system was employed to reduce delay in sending infant HIV testing results from a centralized laboratory to remote rural health facilities;9 in Malawi a SMS system was designed to improve communication among health workers for family planning and reproductive health in rural areas10 and to improve influenza surveillance;11 in Botswana m-health is used for improving clinical education, decision making, and patient adherences;12,13 and in India a m-health systems was used to build a health information system14. These studies were mostly focused on improving health processes and only a few of them analysed the impact on health indicators, such as HIV virological failure.15 Moreover, only two projects were found working to improve maternal and infant health care. In Rwanda a mobile phone-based communication system was deployed to monitoring pregnancy and reducing bottlenecks in communication associated with maternal and newborn deaths.16 However this project did not analyse the impact on maternal or infant mortality. The solution proposed in17 managed to reduce perinatal mortality, but it was different from the one here presented because it was not designed to remotely support the CFs, but to communicate with the pregnant women and allow them to follow-up pregnancies through a SMS system. Given that is hard to find significant evidence on the impact of m-health projects in developing countries,18,19 the objective of this research was to evaluate the impact of the previously explained m-health project on maternal and child mortality in the selected rural area of Guatemala.
Materials and Methods
The project has worked with 125 tele-CFs, who in 2012 were providing services to 466 rural communities or closer than a quarter million inhabitants. This number has been achieved gradually with 20 tele-CFs in 2008 (serving 45,979 inhabitants), 40 in 2009 (serving 84,215 inhabitants), 60 in 2010 (serving 141,351 inhabitants), 125 in 2011 (serving 227,662 inhabitants) and 125 in 2012 (serving 233,445 inhabitants). The selection of the CFs who became tele-CFs was carried out in collaboration with the Health Directorate of Alta Verapaz by prioritizing areas with high maternal and infant mortality. Therefore, the findings here presented are the result of an observational study. Data, for both child and maternal mortality, was obtained from official information published by the MSPAS for the whole Department of Alta Verapaz. The intervention group was composed of the population served by the tele-CFs, while the control group was composed of the population served by CFs without ICT tools, living both population groups in rural areas of the districts of Cahabon, Lanquin, Fray Bartolome Chisec, San Cristobal, Campur, Raxruha and Senahu. Therefore, both groups are completely similar in relation with hospital access, racial/ethnic makeup, age, education, etc.
A maternal death was allocated to the intervention or to the control group if it met the following criteria:
Death occurred while the woman was pregnant or within 42 days of the termination of pregnancy, irrespective of cause and without separation of deaths due to obstetric causes (direct) or non-obstetric causes (indirect).
Deaths occurred in one of the locations assigned to a tele-CF and took place after the tele-CF had received training and equipment from TulaSalud (for care during birth, cell phone for voice communication and data exchange, and a solar panel and battery for power supply) were allocated to the intervention group.
Deaths occurred in any of the locations assigned to a regular-CF (without technology) were allocated to the control group.
The allocation of the death of a child to the intervention or to the control group was based on meeting the following criteria:
Death from any cause in children under one year of age.
Deaths in any of the locations assigned to a tele-CF after training and the provision of equipment were allocated to the intervention group.
Deaths occurred in any of the locations assigned to a regular-CF (without technology) were allocated to the control group.
Due to concerns around inconsistencies in information, the calculation of the MMR in the zones of intervention and control was performed by considering expected pregnancies (total population·birth rate/1,000) rather than the number of live births. The total population (in communities served either by tele-CFs or by regular-CFs) for the years 2008, 2009, 2010, 2011 and 2012 was calculated using the census carried out in 20131 by health service providers2 from the Coverage Extension Program, subtracting the natural growth rate each year. The birth rates and the natural growth rates used were the average for all the Department of Alta Verapaz and are available at Table 1.
Table 1.
Birth rate and natural growth rate between the years 2008 and 2012 in Alta Verapaz.
| Year | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|
| Birth rate | 28.17 | 25.33 | 25.5 | 24.66 | 23.57 |
| Natural growth rate | 2.48 | 2.24 | 2.26 | 2.22 | 2.1 |
The statistical treatment of the data was performed with “IBM SPSS Statistics 20” using a generalized linear regression (log-linear Poisson) with deaths as the dependent variable, the existence or not of tele-CF as factor, year as a covariate and the Napierian logarithm of expected pregnancies as the offset variable.20 A confidence interval of 95% was used in all cases and the model’s goodness of fit was verified first with an Omnibus contrast (in order to identify the most significant variables) and later by calculating the Wald Chi-square.
The intervention carried out by TulaSalud comprises the following key activities:
Selection and initial training of a tele-CF. The decision as to which CF becomes a tele-CF is made jointly by the Health Directorate of Alta Verapaz and TulaSalud, and prioritizes areas with high maternal and infant morbidity and mortality. The tele-CF receives equipment (cell phone, solar panel and battery, external microphone and speaker) and initial training in voice communication and data, as well as the use of an audio-conferencing system (a corporate number to which all tele-FC call, at the same time, to receive distance training in their language). They are also provided with basic initial training in vital signs monitoring, and in identification of signs of distress in children and pregnant women.
Consultation and logistical support in emergencies. The tele-CF can make free telephone calls3 regarding clinical and administrative questions to specialists at TulaSalud as well as medical staff (gynaecologists, paediatricians, internists and surgeons) in MSPAS health centres and hospitals. They can also call for the emergency transfer of a patient by ambulance or, where this is not possible, activate a local emergency plan for the transfer of the patient with support from the community (by foot, private car, boat, etc.). Coban Hospital also has a telemedicine office that facilitates communication between the rural indigenous community and hospital staff in the case of linguistic or cultural problems.
Epidemiological surveillance and registration of patient care. TulaSalud has developed the Kawok system < www.kawok.net > which allows real-time capture (the phones4 have an application, a health information management software, that allows to register the demographic and clinical data of the patient and the care provided through the phone keyboard), transfer, processing and visualization of all clinical and epidemiological information obtained by the tele-CF. This platform also enables monitoring of epidemiological information, especially of pregnant and postpartum women, to identify danger signs or risk factors in order to prevent and treat health problems before they become serious complications.
Continuous training of the tele-CFs and promotion of community health. TulaSalud performs periodic (quarterly) face-to-face sessions for training tele-CFs in clinical issues. This training is reinforced by teleconferences taught in the Q’eqchí and/or Poqomchi’ languages (bimonthly). Periodic distance training to improve the promotion and prevention of health in rural areas is also offered to the community.
Results
Process results
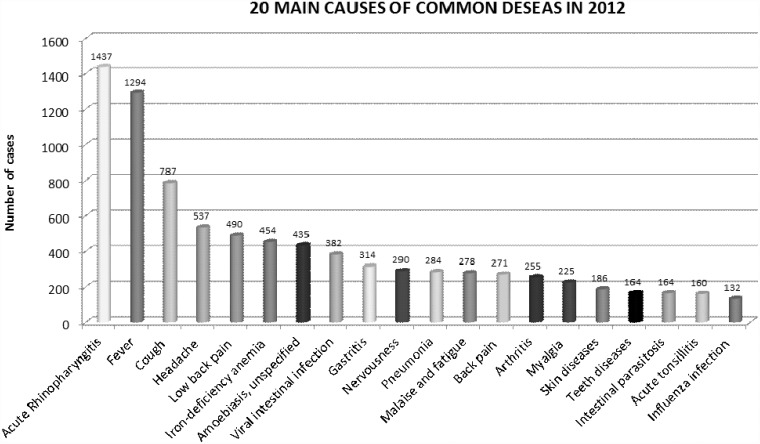
In the 5 years between 2008 and 2012, TulaSalud’s tele-CFs have carried out 116,275 general consultations (mean of 214 by tele-FC and year, with standard deviation of 157), monitored 6,783 pregnant women and coordinated 2,014 emergency transfers, 298 of which were high risk pregnancies and 235 for children under the age of 5. Only in 2012, the tele-CFs of TulaSalud made 12,950 phone calls (mean of 220 with standard deviation of 172), mainly to the headquarters of health services providers, nearby health centres and posts, the Departmental hospital and TulaSalud medical staff. According to records obtained through the Kawok system, the diseases prevalent in the area are respiratory and diarrheal infections. There is also a high incidence of anaemia among the population.
In 2012, the MSPAS described 80 cases of pregnant woman (associated with 57 paediatric cases) as “lives saved5” as a result of using TulaSalud’s communication systems to improve health care.
A 37.5% of those 80 cases were related to foetal malposition (transverse), 16.5% to placental retention, 10% were incomplete abortions, and 6.5% eclampsia and pre-eclampsia cases. The 57 paediatric cases are considered life saved because all required segmental transperitoneal caesarean (CSTP) for birth. All these cases were transferred to the Hospital of Coban, and the transfer was coordinated using the telecommunication systems.
Impact results
Although the TulaSalud project affects the general population, it has been assessed mainly in relation to the two most vulnerable groups in Alta Verapaz: pregnant women and children less than 1 year of age.
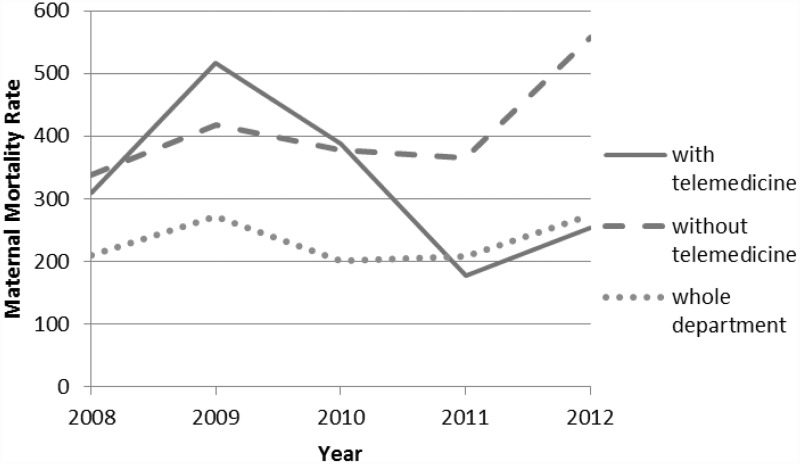
In 2008, 20 tele-CFs from TulaSalud attended to 113 rural communities in Alta Verapaz, representing a total of 45,979 inhabitants. In the same year there were 4 maternal deaths (meeting the criteria for allocation outlined above) in populations served by these tele-CFs. The expected number of pregnancies that year was 1,295, giving a MMR in the intervention area of 309 deaths for every 100,000 births. This is a much higher rate than the Departmental average which stood at 210 in 2008. The MMR in the control group was 338 (similar to the intervention group). Both values contrast with the MMR in the areas covered by health centres and health posts in the same districts which was 96 deaths for every 100,000 births that year.
If we compare the data from the intervention group in 2008 with the data from 2012, we see a significant change in trend with 14 maternal deaths (meeting our criteria) in populations served by the 125 tele-CFs (233.445 inhabitants), giving a MMR of 254. This is lower than the departmental average of 274 for that year. The drop contrasts with a significant increase in the control group (558) as well as an increase in the area attended by health posts and centres (150).
Table 2 shows the MMR data of the time series between 2008 and 2012 (5 years) for both intervention and control groups. The data is presented graphically in Figure 4 so that the change in trend produced by the intervention can be fully appreciated, specifically in areas of high maternal mortality.
Figure 1.
Community Facilitator querying a doubt.
Figure 2.
Community Facilitator sending epidemiological information.
Figure 3.
The 20 main causes of illness in Alta Verapaz in 2012.
Table 2.
Maternal Mortality Rate in intervention and control groups.
| Year | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|
| Intervention group | Cases of maternal death in communities with tele-CF | 4 | 11 | 14 | 10 | 14 |
| Population served by tele-CFs | 45,979 | 84,215 | 141,351 | 227,662 | 233,445 | |
| Expected pregnancies in areas served by tele-CFs | 1,295 | 2,133 | 3,612 | 5,614 | 5,502 | |
| MMR in communities with tele-CF (intervention group) | 309 | 516 | 388 | 178 | 254 | |
| Control group | Cases of maternal death in communities with CF (without ICT tools) | 15 | 22 | 15 | 8 | 12 |
| Population served by CFs (without ICT tools) | 157,514 | 207,697 | 155,282 | 88,535 | 91,236 | |
| Expected pregnancies in areas served by CFs (without ICT tools) | 4,437 | 5,261 | 3,967 | 2,183 | 2,150 | |
| MMR in communities with CF (without ICT tools) (control group) | 338 | 418 | 378 | 366 | 558 |
Figure 4.
Evolution of maternal mortality between 2008 and 2012.
The information in Table 2 and graph above (Figure 4) is clear: the MMR shows a notable downward trend in the intervention group (this is very sharp if we focus on the last 4 years), while the opposite is the case for the control group. The official figures for maternal mortality for the whole Department of Alta Verapaz (1.2 million inhabitants, including both urban and rural areas) were added in order to check that the behaviour in the control group was consistent with the entire Department. The group with tele-CFs shows a different pattern because of the intervention. The change in pattern of the MMR between intervention and control groups over the years was verified by conducting a log-lineal Poisson regression which obtained statistical significance (p < 0,05) for the interaction between the variables of telemedicine and years.
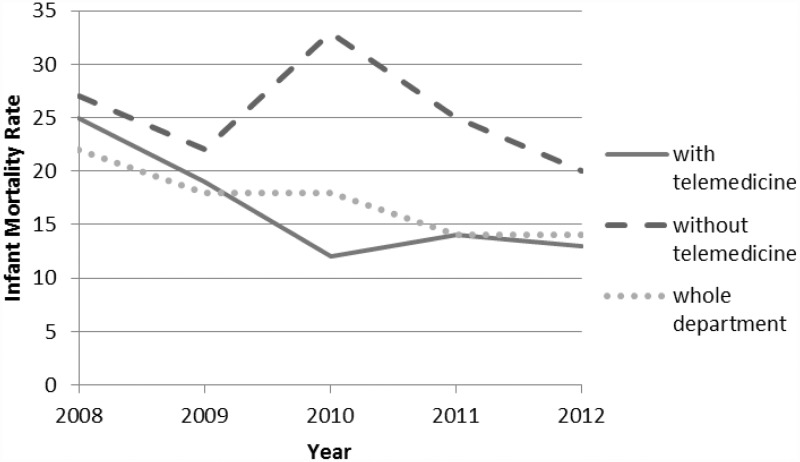
If we perform the same analysis for the infant mortality rate (Table 3), we are unable to reach conclusions as definitive as those shown in the case of maternal mortality. While an important reduction in the rate of infant mortality in the intervention group is shown (Figure 5), the change in trend in the control group is also decreasing. It must be appreciated, however, that on the basis of similar rates in the year 2008 (25 and 27 deaths for every 1,000 births in the intervention and control groups respectively), the rate in 2012 is clearly lower in the intervention group (13) than in the control group (20). In this case the p-value retrieved is 0.054, slightly higher than the limit necessary to demonstrate clear statistical significance.
Table 3.
Infant Mortality Rate in intervention and control groups.
| Year | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|
| Intervention group | Cases of infant death in communities with tele-CF | 32 | 40 | 45 | 79 | 72 |
| Population served by tele-CFs | 45,979 | 84,215 | 141,351 | 227,662 | 233,445 | |
| Expected pregnancies in areas served by tele-CFs | 1,295 | 2,133 | 3,612 | 5,614 | 5,502 | |
| IMR in populations with tele-CF (intervention group) | 25 | 19 | 12 | 14 | 13 | |
| Control group | Cases of infant death in communities with CF (without ICT tools) | 119 | 114 | 130 | 55 | 43 |
| Population served by CFs (without ICT tools) | 157,514 | 207,697 | 155,282 | 88,535 | 91,236 | |
| Expected pregnancies in areas served by CFs (without ICT tools) | 4,437 | 5,261 | 3,967 | 2,183 | 2,150 | |
| IMR in communities with CF (without ICT tools) (control group) | 27 | 22 | 33 | 25 | 20 |
Figure 5.
Evolution of infant mortality between 2008 and 2012.
Discussion
The first aspect to be explained is the procedure employed to calculate the population served by each CF (that was used to calculate the number of expected pregnancies) for each year of intervention. We had two options: 1) use information from the last official census in Guatemala (done in 2002) and projecting forward (years 2008/2009/2010/2011/2012) using the natural average growth rates; 2) use the information about population gathered by the Coverage Extension Program of the MSPAS in 2013 and projecting backwards. The second option was selected because it is based on the most updated information that is available nowadays.
The second aspect that needs to be explained is why we have not used the official data on “live births” in the denominators of the mortality rates. There are significant inconsistencies in the information of “live births” and the clearest proof of this can be seen in the data of the control group between 2009 and 2010 (Table 4). While the population served by the CFs falls in 2010 on more than 50,000 inhabitants (because they are attended by 20 new tele-CFs) the number of “live births” in these communities is almost constant. This incongruence has made us wary of official records (in these rural indigenous areas there is an underreporting problem) and we preferred to use the data of “expected pregnancies” (that followed a more reasonable trend) instead of “live births”. This change may affect the absolute value of the mortality ratios, but not the comparison between the intervention group and the control group (which is the aim of the study) because its effect is similar in both groups.
Table 4.
Live births according to the Health Directorate of Alta Verapaz.
| Year | 2008 | 2009 | 2010 | 2011 | 2012 | |
|---|---|---|---|---|---|---|
| Intervention group | Live births | 1,485 | 2,268 | 3,163 | 4,734 | 4,396 |
| Population | 45,979 | 84,215 | 141,351 | 227,662 | 233,445 | |
| Control group | Live births | 5,411 | 5,846 | 5,879 | 2,709 | 2,951 |
| Population | 157,514 | 207,697 | 155,282 | 88,535 | 91,236 |
Although the results of impact on maternal and neonatal mortality presented in this study justify the use of m-health to support the work of community health workers, we want to highlight the difficulty to adjust the statistical model, given the scarcity of data (we met the requirement of having at least 5 samples for each variable but the overall number of samples did not reach the minimum of 30). Further work is needed to extend the analysis to more years, in order to confirm the trends found in the impact on neonatal mortality.
Conclusions
The study enables us to conclude that the m-health system introduced by the Guatemalan NGO TulaSalud has significantly reduced maternal mortality (p < 0.05) and child mortality (p = 0.054) in the Department of Alta Verapaz. A detailed analysis of the information shows that impact becomes noticeable two years after the start of the intervention, leading us to reflect on the difficulty of obtaining significant short-term impact results in telemedicine projects. While this study has focused on evaluating results among the most vulnerable groups in Alta Verapaz (pregnant women and children under 1 year of age), we believe it would be interesting to conduct the same study with morbidity and mortality data in general.
Funding Acknowledgements
The project here evaluated was supported by the Tula Foundation (http://tula.org/) and carried out by Tulasalud Association (http://www.tulasalud.org), however the evaluation was conducted by researchers from the Rey Juan Carlos University and EHAS Foundation without external funding, who didn’t have previous relation with the project or the organizations previously mentioned; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work. After this research, Rey Juan Carlos University and EHAS Foundation have carried out other works with Tulasalud Association, but none of this works have relation with this research.
Notes
The last official census carried out by the Central Government took place in 2002.
The Health Service Providers are NGOs that sign an annual memo of understanding with the Ministry of Health and Social Welfare (MSPAS) in order to offer health care in rural areas that are not covered by MSPAS health centres and health posts. This service is coordinated by the Coverage Extension Program.
TulaSalud has a contract that includes 235 cell phones and 12 data modems for computers (in remote training centers and in health centers and hospitals), and allows unlimited internal calls, 300 minutes of external calls and 250 megabytes of internet access in each terminal.
Two different mobile phone models have been used in the intervention: the Sony Ericsson K550i and the Nokia Express Music 5130. Both terminals have an integrated digital camera (3MP and 2 MP respectively), they work with the Symbian operating system and have installed the application Kawok, which is a health management software based on the Commcare platform of the company Dimagi Inc. Currently the project terminals have been migrated to Huawei G510 with 4.5 inch screen, 5MP camera, and Android operating system, which allows tele-FC to also use WhatsApp, Gmail, Skype, etc.
A case is considered as “Live saved” when the patients suffers a high death risk if it is not transferred to a health facility with the proper resolution level.
Declaration of Conflicting Interests
The Authors declare that there is no conflict of interest.
Guarantor and statement of contributorship
Andrés Martínez-Fernández affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Contributors: AM designed data collection tools, monitored data collection for the whole research, wrote the statistical analysis plan, analysed the data, and drafted and revised the paper. He is guarantor. IL initiated the collaborative project, provided access to the data of the Tulasalud Association, and contributed to analyse the data and to draft the paper. CD designed data collection tools, provided access to health information of the Health Directorate of Alta Verapaz, monitored data collection for the whole trial, cleaned and analysed the data and drafted the paper. MC wrote the statistical analysis plan, collected statistical results and revised the draft paper. IP designed data collection tools and revised the draft paper.
References
- 1.Khalid Malik et al. The Rise of the South: Human Progress in a Diverse World. United Nations Development Program (2013). ISBN 978-92-1-126340-4. See [http://www.undp.org/content/dam/undp/library/corporate/HDR/2013GlobalHDR/English/HDR2013 Report English.pdf] (last checked 5 September 2013).
- 2.Cifras para el Desarrollo Humano en Guatemala. United Nations Development Program of Guatemala. See [http://www.desarrollohumano.org.gt/fasciculos/cifras_v4.html] (last checked 5 September 2013).
- 3.Khalid S Khan, Daniel Wojdyla, Lale Say, A. Metin Gülmezoglu, Paul FA Van Look. “WHO analysis of causes of maternal death: a systematic review”. The Lancet. Volume 367, Issue 9516, 1–7 April 2006, Pages 1066–1074. DOI: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed]
- 4.Jennifer Bryce, Cynthia Boschi-Pinto, Kenji Shibuya, Robert E. Black. “WHO estimates of the causes of death in children”. The Lancet. Volume 365, Issue 9465, 26 March–1 April 2005, Pages 1147–1152. DOI: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed]
- 5.Martínez A, Villarroel V, Seoane J, del Pozo F. “Analysis of information and communication needs in rural primary health care in developing countries”. IEEE Transactions on Information Technology in Biomedicine. Volume 9; Number 1; March 2005. pp 66–72. ISSN: 1089-7771. [DOI] [PubMed]
- 6.Martínez A, Villarroel V, Seoane J, del Pozo F. A study of a rural telemedicine system in the Amazon region of Peru. Journal of Telemedicine and Telecare. Volume 10; Number 4; 2004. pp 219 - 226. ISSN: 1357-633X. [DOI] [PubMed]
- 7.United Nations Development Program. Mobile technologies and empowerment: enhancing human development through participation and innovation. 2012. URL: http://www.undpegov.org/sites/undpegov.org/files/undp_mobile_technology_primer.pdf.
- 8.Asiimwe C, Gelvin D, Lee E, et al. Use of an Innovative, Affordable, and Open-Source Short Message Service–Based Tool to Monitor Malaria in Remote Areas of Uganda. Am J Trop Med Hyg 2011 Jul; 85(1): 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seidenberg P, Nicholson S, Schaefer M, et al. Early infant diagnosis of HIV infection in Zambia through mobile phone texting of blood test results. Bull World Health Organ 2012 May 1; 90(5): 348–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lemay NV, Sullivan T, Jumbe B, Perry CP. Reaching remote health workers in Malawi: baseline assessment of a pilot mHealth intervention. J Health Commun 2012; 17(Suppl 1): 105–17. [DOI] [PubMed] [Google Scholar]
- 11.Bakshi A, Narasimhan P, Junhua Li, et al. mHealth for the control of TB/HIV in developing countries. In: 13th IEEE International Conference on, e-Health Networking Applications and Services (Healthcom), 2011, pp.9,14, 13–15 June 2011. doi: 10.1109/HEALTH.2011.6026797.
- 12.Littman-Quinn R, Chandra A, Schwartz A, et al., mHealth applications for telemedicine and public health intervention in Botswana. In: IST-Africa Conference Proceedings, 2011, pp.1,11, 11–13 May 2011.
- 13.Littman-Quinn R, Chandra A, Schwartz, A, et al. mHealth applications for clinical education, decision making, and patient adherence in Botswana. In: IST-Africa Conference Proceedings, 2011, pp.1, 8, 11–13 May 2011.
- 14.Bondale N, Kimbahune S, Pande, A, “mHEALTH-PHC: A community informatic tool for primary healthcare in India,” In: IEEE Conference on Technology and Society in Asia (T&SA), 2012, pp.1, 6, 27–29 Oct. 2012. doi: 10.1109/TSAsia.2012.6397994.
- 15.Chang LW, Kagaayi J, Arem H, et al. Impact of a mHealth Intervention for Peer Health Workers on AIDS Care in Rural Uganda: A Mixed Methods Evaluation of a Cluster-Randomized Trial. AIDS and Behavior 2011; 15(8): 1776–1784. doi:10.1007/s10461-011-9995-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ngabo F, Nguimfack J, Nwaigwe F, et al. Designing and Implementing an Innovative SMS-based alert system (RapidSMS-MCH) to monitor pregnancy and reduce maternal and child deaths in Rwanda. The Pan African Medical Journal 2012; 13: 31–31. [PMC free article] [PubMed] [Google Scholar]
- 17.Lund S, Rasch V, Hemed M, et al. Mobile Phone Intervention Reduces Perinatal Mortality in Zanzibar: Secondary Outcomes of a Cluster Randomized Controlled Trial. Eysenbach G, ed. JMIR mHealth and uHealth 2014;2(1): e15. doi:10.2196/mhealth.2941. [DOI] [PMC free article] [PubMed]
- 18.Gurman TA, Rubin SE, Roess AA. Effectiveness of mHealth behavior change communication interventions in developing countries: a systematic review of the literature. J Health Commun 2012; 17(Suppl 1): 82–104. doi: 10.1080/10810730.2011.649160. [DOI] [PubMed] [Google Scholar]
- 19.Källander K, et al. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: a review. J Med Internet Res 2013 Jan 25; 15(1): e17–e17. . doi: 10.2196/jmir.2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frome EL. The analysis of rates using Poisson regression models. Biometrics 1983 Sep; 39(3): 665–74. [PubMed] [Google Scholar]