Abstract
Objective(s):
We investigated the contribution of gyrA and parC mutational mechanism in decreased ciprofloxacin susceptibility of Acinetobacter baumannii isolated from burn wound infections.
Materials and Methods:
Ciprofloxacin susceptibility of 50 A. baumannii isolates was evaluated by disk diffusion and agar dilution methods. PCR and sequencing were performed for detection of mutation in gyrA and parC genes.
Results:
The 44 and 4 isolates of A. baumannii exhibited full and intermediate-resistant to ciprofloxacin, respectively. Overall, the 42 isolates with double mutations of gyrA and parC genes showed a higher level of ciprofloxacin resistance than the 3 isolates with single mutations of gyrA or parC.
Conclusion:
Simultaneous mutations in gyrA and parC genes are expected to play a major role in high-level fluoroquinolone resistance in A. baumannii; albeit a single mutation in DNA topoisomerase IV could occasionally be associated with intermediate-resistance to these antimicrobials.
Keywords: Acinetobacter baumannii, Burn, Ciprofloxacin resistance, gyrA, parC
Introduction
A list of organisms has been identified by the Infectious Disease Society of America as being responsible for the majority of healthcare associated drug resistant infections. These organisms are the members of the notorious “ESKAPE” (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) (1). Among these problematic organisms, A. baumannii has nowadays emerged as a particular concern worldwide; because it is responsible for a variety of infections, such as blood infection, meningitis, ventilator associated pneumoniae (VAP), and wound infections, especially among patients admitted in burn and intensive care units (2, 3). In addition, this organism is a successful pathogen to escape the effects of several classes of antimicrobials, including fluoroquinolones and represents a significant challenge to infectious disease specialists (4).
The antimicrobial activity of fluoroquinolones is to form ternary complexes, including enzymes, such as DNA gyrase or topoisomerase IV, drug, and DNA which can block DNA replication and transcription, probably before DNA cleavage occurs (5). There is remarkable conservation of protein sequences between the DNA gyrase subunit A (GyrA) and topoisomerase IV subunit C (ParC) in the quinolone resistance determining region (QRDR). Resistance to fluoroquinolone in bacteria is mediated mainly by spontaneous mutations in the QRDR of gyrA and parC genes (8). In Escherichia coli, the most important mutations leading to a quinolone-resistant phenotype are Ser83Leu and Asp87Asn in the gyrA gene, and Ser80Arg and Glu84Val in the parC gene (6, 7).
Many fluoroquinolone-resistant A. baumannii clinical isolates have been reported in Iran (8-9). There are, however, few studies about the prevalence of mutations in the genes for DNA gyrase and topoisomerase IV in this organism. So, the present study aimed to specifically assess the presence of mutations in the gyrA and parC genes and their effects on resistance to fluoroquinolones in A. baumannii isolates from patients at a teaching hospital in Tehran.
Materials and Methods
Bacterial isolates
Motahari Hospital is a 120-bed university affiliated Burn and Reconstruction Center located in Tehran, Iran. A total of 50 non-repetitive A. baumannii isolates were recovered between April 2012 and March 2013 from burn wounds of patients admitted in this hospital. All isolates were assigned to A. baumannii by bacteriologic and traditional phenotypic methods, including gram’s staining, oxidase and catalase tests, motility, oxidative-fermentative (OF) test, and growth at 37 °C and 44 °C. The PCR of the intrinsic blaOxa-51-like gene was done to confirm A. baumannii species (10).
Antimicrobial susceptibility testing
The susceptibility of A. baumannii isolates to ciprofloxacin disk (5 µg) (Mast, Merseyside, U.K) was assessed by the standard disk agar diffusion method on Mueller Hinton agar plates. The MIC for ciprofloxacin was determined by the broth macrodilution method in accordance to the Clinical and Laboratory Standards Institute (CLSI) criteria (11). Briefly, a serial dilutions of ciprofloxacin was prepared in Mueller Hinton broth tubes with the bacteria at a density of 5×106 CFU/ml. Microbial tubes were incubated at 37 °C for 18 hr and finally, the lowest concentration of antibiotic with no visible bacterial growth was defined as the MIC. Quality control was done using Pseudomonas aeruginosa ATCC 27853 strain, and results were compared to MIC ranges of CLSI. A. baumannii isolates were considered as intermediate-resistant and full-resistant to ciprofloxacin when the MIC was 2 µg/ml and ≥4 µg/ml, respectively.
PCR amplification and sequencing
The QRDRs of the gyrA and parC genes in A. baumannii clinical isolates were amplified by PCR assay. Two pairs of oligonucleotide primers used for the PCR reactions were gyrA primer: forward, 5’-AAATCTGCTCGTGTCGTTGG-3’; reverse, 5’-GCCATACCTACAGCAATACC-3’, and parC primer: forward, 5’-AAGCCCGTACAGCGCCGTATT-3’; reverse, 5’-AAAGTTATCTTGCCATTCGCT-3’. Extraction of genomic DNA from A. baumannii colonies was performed using genomic DNA purification kit (Fermentas, Germany), based on the manufacturer’s instructions. For all amplification reactions, a PCR mixture was used that contained 12.5 µl of 2× Master Mix (Ampliqon, Denmark), including 1× PCR buffer, 1.5 mmol/l MgCl2, dNTPs at a concentration of 0.15 mmol/l each dNTP, 1.25 U of Taq DNA polymerase, 0.5 µl of 0.8 µM of each primer, 1 µl of template DNA (0.5 µg), and sterile distilled water up to 25 µl. DNA amplification was performed in the Mastercycler gradient instrument (Eppendorf, Germany). For gyrA, PCR conditions consisted of an initial denaturation at 95 °C for 1 min; 35 cycles of denaturation at 95 °C for of 30 sec, 30 sec of annealing at 52 °C, and 2 min of extension at 72 °C; ending with a final extension at 72 °C for 10 min. The temperature profile for parC gene was comprised of 95 °C for 2 min, followed by 35 cycles of 1 min at 95 °C, 1 min at 60 °C and 2 min at 72 °C, with 10 min at 72 °C for final extension step. DNA fragments were analyzed by electrophoresis on agarose gel (2%, wt/vol) containing 0.5 mg of ethidium bromide per liter and photographed with ultraviolet illumination. Direct sequencing of the PCR products in both directions was performed by using an ABI3730XL DNA analyzer (Applied Biosystems, Forster, USA). Nucleotide sequences data were analyzed at the National Center for Biotechnology Information (NCBI), available at the website (http:/www.ncbi.nlm.nih.gov/BLAST/).
Statistical data analysis
SPSS version 11.5 (SPSS, Inc., Chicago, IL, USA) was employed for statistical analysis. Descriptive statistics and Pearson’s chi-square tests were used to evaluate correlation between mutation and ciprofloxacin resistance. Statistical significance was defined as P-value less than 0.05.
Results
Ciprofloxacin susceptibility and amino acid substitutions
The susceptibility testing by disk diffusion method determined that 4%, 8%, and 88% of A. baumannii clinical isolates were susceptible, intermediate-resistant and full-resistant to cipro-floxacin, respectively. The MIC range of ciprofloxacin in 44 full-resistant isolates was 4 to ≥128 µg/ml. To determine the changes in the structure of DNA gyrase and topoisomerase IV enzymes, the QRDRs of corresponding genes, gyrA and parC, were analyzed by PCR sequencing technique in all 50 clinical isolates with intermediate-resistant and full-resistant to ciprofloxacin. Amplification of gyrA and parC genes yielded PCR products of 349 and 327 bp, respectively (Figure 1). The nucleotide sequencing results revealed that 45 (90%) of the 50 isolates had amino acid alteration in gyrA and parC, as follow: 1 (2.2%) isolate in gyrA only, 2 (4.4%) isolates in parC only, and 42 (93.3%) isolates in gyrA and parC, concurrently. The A. baumannii isolates were divided into five groups based on the amino acid substitutions associated with resistance to fluoroquinolone (Table 1). Single mutations encoding Ser83Leu and Gly81Asp were found in the QRDR of gyrA in 37 (82.2%) and 6 (13.3%) of the 45 mutated isolates, respectively. Forty four of the 45 Acinetobacter isolates (95.5%) had a single mutation in parC encoding Ser80Leu (23; 51.1%), Glu84Lys (19; 42.2%), and Gly78Cys (2; 4.4%).
Figure 1.
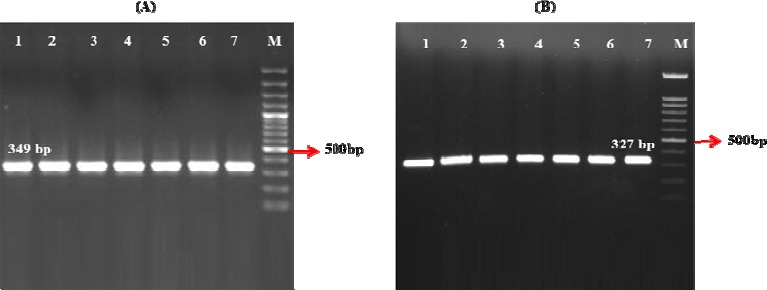
PCR amplification of the QRDRs of the gyrA (A) and parC (B) genes in Acinetobacter baumannii isolates. Lanes: 1- 7, PCR products of the corresponding genes; M, 100 bp Plus DNA Ladder
Table 1.
Point mutations in the QRDRs of the gyrA and parC genes of Acinetobacter baumannii isolates, and the ciprofloxacin MIC in the isolates of mutation groups
| Mutation group | No. (%) of isolates | No. (%) of isolates with MIC (µg/ml) to ciprofloxacin | gyrA mutations | parC mutations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 4 | 8 | 16 | 32 | 64 | 128 | >128 | S83(tca) | G81(ggt) | S80(tcg) | E84(gaa) | G78(ggt) | ||
| I | 1(2.2) | 1(2.2) | L(tta) | |||||||||||
| II | 2(4.4) | 2(4.4) | C(tgt) | |||||||||||
| III | 17(37.8) | 2(4.4) | 4(8.9) | 7(15.6) | 2(4.4) | 2(4.4) | L(tta) | L(ttg) | ||||||
| IV | 6(13.3) | 1(2.2) | 1(2.2) | 1(2.2) | 2(4.4) | 1(2.2) | D(gat) | L(ttg) | ||||||
| V | 19(42.2) | 3(6.7) | 10(22.1) | 3(6.7) | 3(6.7) | L(tta) | K(aaa) | |||||||
MIC for ciprofloxacin in the QRDR mutants
Groups I and II mutants had a single mutation in gyrA and parC, respectively; but their ciprofloxacin MIC ranged from 2 to 4 µg/ml. Acinetobacter isolates present in the mutation groups III, IV, and V showed double mutations in gyrA and parC and were resistant to ciprofloxacin with a MIC range of 8 to ≥128 µg/ml. Overall, isolates with double mutations of gyrA and parC genes showed a higher level of ciprofloxacin resistance than isolates with single mutations of gyrA or parC (P< 0.05).
Nucleotide sequence accession number
The nucleotide sequences data reported in the present study have been deposited in the Pubmed/NCBI/GenBank nucleotide sequence database under accession numbers for gyrA (KJ195830.1 and KJ195831.1) and parC (KJ756512, KJ756513 and KJ756514) genes.
Discussion
Previous studies have shown that fluoroquino-lones are one of the first line therapies for A. baumannii infections (12, 13). However, our results in agreement with other studies revealed a considerable increase in ciprofloxacin resistance in Iran (8, 9). Resistance to ciprofloxacin in Acinetobacter isolates is alarming; since many of such strains are usually multi-drug resistant (MDR), and at these circumstances, the remaining therapeutic options are colistin (a relatively toxic drug), tigecycline (a bacteriostatic agent, i.e. a disadvantage when using in immunocompromised patients), and sulbactam (with a limited antibacterial spectrum only) (14).
It is accepted that changes in the structure of the antibiotic targets DNA gyrase and DNA topoisomerase IV are one of the most significant mechanisms in conferring a resistance to fluoroquinolone in gram negative bacilli (7). In E. coli, three or four mutations in both gyrA and parC genes are necessary to obtain high-level resistance to ciprofloxacin, even as double mutations at positions 83 (Ser83) of gyrA and 80 (Ser80) of parC cause only moderate-level resistance (6, 7). Nevertheless, the situation in A. baumannii is rather different from that in E. coli, since we found in the present study that only a double mutation could lead to high-level resistant phenotype. So that, among 44 ciprofloxacin-resistant isolates, 11 (25%) had MIC range of 8-32 µg/ml and the majority (31; 70.4%) of isolates had MICs of 128 µg/ml or higher, that indicate these isolates are highly resistant to fluoroquinolones.
Our sequencing results revealed serine to leucine mutation at position 83 of gyrA subunit in 38 of 44 ciprofloxacin-resistant Acinetobacter isolates. Similar to study by Park et al (15), this is indicative of the fact that Ser83Leu substitution is the principal mutation in A. baumannii for resistance to fluoroquinolones. Other mutations in the gyrA gene resulting in Ala84Pro or Gly81Val reported in ciprofloxacin resistant isolates of previous study (16) were not observed in our included isolates. Instead, we found a novel mutation in the gyrA gene, leading to Gly81Asp substitution DNA gyrase, in six resistant isolates with a MIC range at 8 to ≥128 µg/ml.
In A. baumannii, topoisomerase IV is a target of quinolones and mutations at residues Ser80 and Glu84 of parC contribute to decreased fluoroquino-lone susceptibility (16). Although parC mutations always along with mutations in gyrA are needed to acquire a high-level resistance to quinolones (4), two clinical isolates in our study had mutations in parC without gyrA, suggesting that parC might not only be a secondary target for quinolones but is really as important as gyrA to cause a decreased susceptibility to fluoroquinolones in A. baumannii. On the other hand, QRDRs of the three isolates with intermediate-resistance to ciprofloxacin in the current study did not possess alterations associated with fluoroquino-lones resistance in the sequence of either genes, indicating other resistance mechanisms, such as efflux systems should be considered in these isolates (17).
Conclusion
Although a single point mutation in DNA gyrase is enough for resistance to fluoroquinolone in A. baumannii, the concurrent mutations within QRDR regions of the gyrA and parC genes are expected to significantly contribute to high-level fluoroquinolone resistance. Further studies are required to elucidate mechanisms, other than alterations in gyrA and parC, leading to decreased susceptibility to quinolones in A. baumannii isolates.
Acknowledgment
The results described in this paper were part of PhD thesis. The authors would like to acknowledge the financial support of Iran University of Medical Science (grant number 1067). We gratefully acknowledge for partially conducting this study in microbiology department of Golestan University of Medical Science, Golestan, Iran.
Footnotes
Conflicts of interest
No declarations were made by the authors of this paper.
References
- 1.Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 2.Towner KJ, Levi K, Vlassiadi M. Genetic diversity of carbapenem-resistant isolates of Acinetobacter baumannii in Europe. Clin Microbiol Infect. 2008;14:161–167. doi: 10.1111/j.1469-0691.2007.01911.x. [DOI] [PubMed] [Google Scholar]
- 3.Ardebili A, Talebi M, Azimi L, Lari AR. Effect of efflux pump inhibitor CCCP on the MIC of ciprofloxacin in Acinetobacter baumannii clinical isolates. Jundishapur J Microbiol. 2014;7 doi: 10.5812/jjm.8691. doi:10.5812/jjm.8691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valentine SC, Contreras D, Tan S, Real LJ, Chu S, Xu HH. Phenotypic and molecular characterization of Acinetobacter baumannii clinical isolates from nosocomial outbreaks in Los Angeles County, California. J Clin Microbiol. 2008;46:2499–2507. doi: 10.1128/JCM.00367-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacoby GA. Mechanisms of resistance to quinolones. Clin Infect Dis. 2005;41:120–126. doi: 10.1086/428052. [DOI] [PubMed] [Google Scholar]
- 6.Fàbrega A, Madurga S, Giralt E, Vila J. Mechanism of action of and resistance to quinolones. Microbial Biotech. 2009;2:40–61. doi: 10.1111/j.1751-7915.2008.00063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JK, Lee YS, Park YK, Kim BS. Mutations in the gyrA and parC genes in ciprofloxacin-resistant clinical isolates of Acinetobacter baumannii in Korea. MicrobiolImmunol. 2005;49:647–653. doi: 10.1111/j.1348-0421.2005.tb03643.x. [DOI] [PubMed] [Google Scholar]
- 8.Mostofi S, Mirnejad R, Masjedian F. Multi-drug resistance in Acinetobacter baumannii strains isolated from clinical specimens from three hospitals in Tehran, Iran. Afr J Microbiol Res. 2011;5:3579–3582. [Google Scholar]
- 9.Rahbar M, Mehrgan H, Negar HA. Prevalence of antibiotic-resistant Acinetobacter baumannii in a 1000-bed tertiary care hospital in Tehran, Iran. Ind J Pathol Microbiol. 2010;53:290–293. doi: 10.4103/0377-4929.64333. [DOI] [PubMed] [Google Scholar]
- 10.Turton JF, Woodford N, Glover J, Yarde S, Kaufmann ME, Pitt TL. Identification of Acinetobacter baumannii by detection of the blaOXA -51-like carbapenemase gene intrinsic to this species. J Clin Microbiol. 2006;44:2974–2976. doi: 10.1128/JCM.01021-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.PA: Clinical Laboratory Standards Institute, Wayne; 2013. CLSI Performance standards for antimicrobial susceptibility testing: twentieth informational supplement; pp. M100–S20. CLSI document. [Google Scholar]
- 12.Leonov Y, Schlaeffer F, Karpuch J, Bourvin A, Shemesh Y, Lewinson G. Ciprofloxacin in the treatment of nosocomial multiply resistant Acinetobacter calcoaceticus bacteremia. Infection. 1990;18:234–236. doi: 10.1007/BF01643395. [DOI] [PubMed] [Google Scholar]
- 13.Prashanth K, Badrinath S. In vitro susceptibility pattern of Acinetobacter species to commonly used cephalosporins, quinolones, and aminoglycosides. Indian J Med Microbiol. 2004;22:97–103. [PubMed] [Google Scholar]
- 14.Pachon J, Vila J. Treatment of multiresistant Acinetobacter baumannii infections. Curr Opin Investig Drugs. 2009;10:150–156. [PubMed] [Google Scholar]
- 15.Park S, Lee KM, Yoo YS, Yoo JS, Yoo J, Kim HS, et al. Alterations of gyrA gyrB and parC and activity of efflux pump in fluoroquinolone-resistant Acinetobacter baumannii. Public Health Res Perspect. 2011;2:164–170. doi: 10.1016/j.phrp.2011.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vila J, Ruiz J, Goni P, Marcos A, de Jimenez Anta T. Mutation in the gyrA gene of quinolone-resistant clinical isolates of Acinetobacter baumannii. Antimicrob Agents Chemother. 1995;39:1201–1203. doi: 10.1128/aac.39.5.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ardebili A, Rastegar Lari A, Talebi M. Correlation of ciprofloxacin resistance with the AdeABC efflux system in Acinetobacter baumannii clinical isolates. Ann Lab Med. 2014;34:433–438. doi: 10.3343/alm.2014.34.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]


