Abstract
The calcifying odontogenic cyst (COC) accounts for 1 % of jaw cysts, found most commonly as central lesion. The COC usually manifests itself as a painless, slow growing swelling, anterior to the first molar region. Radiographically it appears as a well-defined, unilocular radiolucency, and may have a radiopaque mass in its center. Majority of the cases appear before the fourth decade of life. The COC is found rarely in patients in the first decade of life. Histopathological features include a cystic lining demonstrating characteristic “Ghost” epithelial cells with a propensity to calcify. Here we report the unusual occurrence of a case of 8 year child diagnosed with bilateral COC on right and left side of mandible.
Keywords: Calcifying odontogenic cyst, Odontogenic tumors, Epithelium, Ectomesenchyme ghost cell, Enucleation, Unerupted teeth
Introduction
The calcifying odontogenic cyst (COC) is a developmental odontogenic cyst and its occurrence constitutes about 0.3–0.8 % of all odontogenic cysts. The COC is an uncommon lesion which occurs both peripherally in the gingiva, and centrally in alveolar bone. In either location they have similar characteristic histological appearance [1]. In 1992, the World Health Organization (WHO) classified Central Ghost cell Odontogenic Cyst (CGOC) as a neoplasm rather than a cyst but confirmed that most of the cases are non neoplastic. In view of this duality, many different terminologies have been applied to cystic and solid CGOC variants, but COC is the preferred term [2].
Clinically it presents as asymptomatic, slow developing, with predilection for the anterior segment (anterior to the first permanent molar). However, the mandible and maxilla appear to be affected with the same frequency. Patient age varies widely from infancy to elderly, with no gender predilection. The mean age of patients with COC is 33 years, with most cases occurring between the second and third decades of life. The COC is found rarely in patients in the first decade of life [3–5]. In Asians it showed a higher incidence in younger age group: almost 70 % occurred in the second and third decades, whereas in whites, only about 55 % occurred in the respective decades [4, 5].
Approximately 50 per cent of cases are associated with unerupted teeth [6, 7]. The cortical bone plates are frequently thin and expanded and may become perforated by the lesion, which may occasionally lead to dental displacement and resorption of the adjacent tooth [8].
Radiographic appearance is usually a unilocular radiolucency with possible radio opacities observed within the lesion [9]. The presence of calcification ranging from tiny flecks to large masses is an important radiographic feature. Root resorption and root divergence, cortical expansion was seen. COC may be associated with impacted teeth [10]. The definitive diagnosis of COC, is made histological due to lack of characteristic clinical and radiological features as well as variable histological behavior. The histological features of a classic calcifying ghost cell odontogenic cyst are characteristic, The microscopical features of lesion showed fibrous capsule with a lining of odontogenic epithelium. The epithelial lining shows a well-defined basal layer of columnar cells and an upper layer with cell arrangement similar to that of the stellate reticulum of the dental organ and a mass of ghost cells that also may be found in the fibrous capsule. Treatment of COC involves enucleation. Recurrence is unusual and depends on the completeness of tumor removal [10, 11].
Case Report
A 8 year old child was referred to the department of Oral and Maxillofacial Surgery with a chief compliant of hard swellings present on both sides of the lower jaw, which have been progressively enlarging for the past 7 months. Not associated with pain. The patient medical history was non contributory. Physical examination showed otherwise a healthy child (Fig. 1).
Fig. 1.
Front view of the patient
Extra-oral examination revealed no obvious gross swelling noted on both sides of the lower jaw. On intra oral examination a bilateral expansion of mandibular buccal and lingual cortical plates extending from deciduous second molar on left side and deciduous first molar on right side to anterior border of ramus respectively was seen. Patient had mixed dentition with missing permanent first molars in all quadrants except for upper left quadrant. Lower permanent central incisors were erupted. The swelling was more prominent on buccal side with clinically healthy overlying mucosa. On palpation bony hard swelling was noted on both sides with no evidence of perforation, crepitation or crackling sensation.
Panoramic radiograph showed bilateral unilocular radiolucency extending from distal aspect of deciduous canine to second permanent molar tooth bud in the ramus involving the tooth bud. OPG radiographs taken at different periods by different clinicians revealed progressive increase in radiolucency, root resorption of deciduous first molar and second molars and appearance of small fleck of crescent shaped calcification overlying the crowns of unerupted permanent first molars. On aspiration slight yellowish straw colored fluid was seen. Incisional biopsy report was suggestive of odontogenic cyst with chronic inflammation (Figs. 2, 3).
Fig. 2.

Intra oral site of biopsy
Fig. 3.

Bicortical plate expansion on lower left side
Differential diagnosis at this stage was possible bilateral occurrence of dentigerous cyst, lateral periodontal cyst, unicystic ameloblastoma, central giant cell granuloma or KCOT (Figs. 4, 5, 6).
Fig. 4.
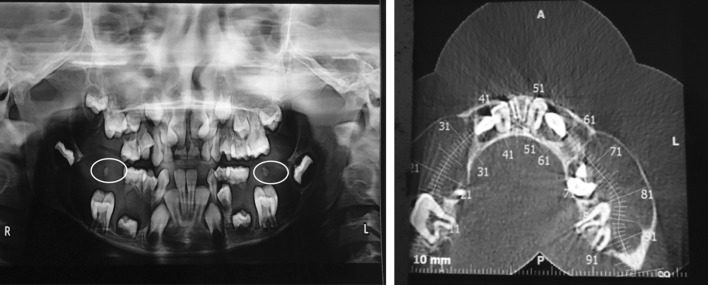
Pre-operative panoramic radiograph and CBCT scan showing radiolucent lesions on both sides with small specks of calcifications over the crowns of impacted permanent first molars seen on OPG
Figs. 5 and 6.

Exposure of the pathological lesion site on right and left side
Cystic enucleation was done under GA on both the sides. Owing to previous biopsy small amount of soft tissue mass was obtained from right side and considerable amount of tissue from left side lesion. Both specimens were sent for histopathology. Macroscopically thin soft tissue mass with embedded teeth were noted (Figs. 7, 8a, b).
Fig. 7.

Specimen from the left side lesion
Fig. 8.
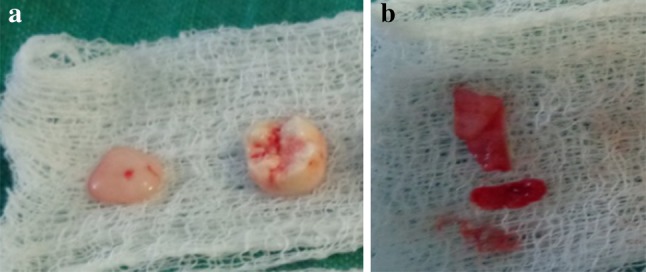
a, b Specimen from right side lesion
Microscopically it was possible to observe the presence of an epithelial lining of which the basal layer cells presented a cubic aspect, in addition to a large quantity of ghost cells and areas of stellate reticulum in both the specimens, confirming the final diagnosis as a calcifying epithelial odontogenic cyst (Fig. 9).
Fig. 9.
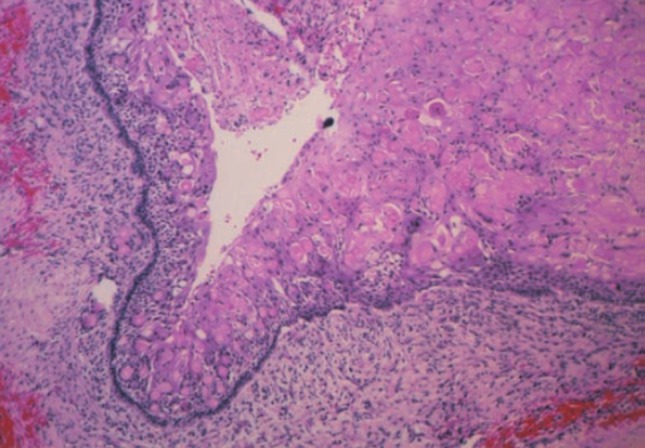
This calcifying odontogenic cyst shows the proliferation of the lining epithelium with palisades, hyperchromatic columnar nuclei, satellite reticulum-like area, and sheets of ghost cells
The patient follow-up has been satisfactory, with normal bone reshaping and without recurrence to date (7 months). Patient is under follow up for periodical post operative assessment (Figs. 10, 11).
Fig. 10.

Suturing of the lesions
Fig. 11.

Post-operative OPG after 7 months
Discussion
Gorlin et al. [12] were the first to describe this entity. They initially regarded it as the oral analogue of the cutaneous calcifying epithelioma of Malherbe but later labeled it as the COC. Prior to this, Rywkind (1932) described it as a variant of the cholesteatoma, while Maitland (1947) regarded it as a type of ameloblastoma. The COC has also been reported under a variety of other designations including: dentinogenic ghost cell odontogenic tumour, epithelial odontogenic ghost cell tumour, ghost cell cyst, calcifying ghost cell odontogenic tumour, and dentino-ameloblastoma. The WHO presently describes the COC as a non-neoplastic cyst, but classifies it as a benign tumor.
From the years of description, disagreements exist regarding the nature, terminology and classification of COC. These controversies and confusion about the lesion are due to existence of two variants of the lesion: A cyst and the neoplastic forms. Praetorious et al. framed a classification based on dualistic concept in which they divided COC (as it was called then) into two entities: A cyst and a neoplasm and proposed the term dentinogenic ghost cell tumor (DGCT) for the neoplastic variant [1]. In 1991, Buchner classified COC majorly on clinical grounds—peripheral COC and Central COC, further sub classifying each of them into cystic or neoplastic variants and included rare malignant variant of COC in the classification [1].
The COC comprises between 0.37 ± 2.1 % of all odontogenic tumours. Praetorius et al. suggested that it develops in the dental follicle, gingival tissue or bone from remnants of either odontogenic epithelium or reduced enamel epithelium [13]. The general clinical aspects (e.g. age, lesion localization and symptoms) of this case are in consonance with those previously described in the literature for COC [4, 14]. Although the incidence of COC is mostly in the second decade of life, this lesion may occur at any age. The occurrence of COC in the first decade of life is very uncommon (about 10 % of reported cases) (Table 1) [15]. In this case, it occurs in the first decade of life. The youngest patient recorded was 2 days old. Buchner found an almost equal gender distribution.
Table 1.
Frequency of COC in first decade of life
| Author | No of cases | First | % |
|---|---|---|---|
| Gorlin et al. | 15 | 1 | 6.6 |
| Fejerskov and Krough | 52 | 5 | 9.6 |
| Freedman et al. [1] | 70 | 3 | 4.3 |
| Altini and Farman | 70 | 4 | 5.7 |
| Pretorious et al. | 16 | 1 | 6.3 |
| Shear | 80 | 5 | 6.3 |
| Shamaskin et al. | 20 | 2 | 10.0 |
| Buchner | 215 | 8 | 3.7 |
Oliveira et al. [15]
The lesion appeared in the anterior portion of the mandible and the literature indicates the anterior portion of the jaws as the most common site for COC [4, 16, 17]. In the present case, the COC presented as a slow growing and painless swelling that caused expansion of the buccal and lingual cortical plates, common features of several benign intra-osseous lesions. The radiographic examination demonstrated solitary, well circumscribed radiolucent areas bilaterally in the same location anterior to permanent first molar region. Progressive root resorption was noted on successive OPG radiographs. Small fleck of calcifications was noted over the crowns of unerupted permanent first molars exactly in the same location on both sides. The COC often occurs in association with an unerupted tooth and/or an odontogenic tumor. In Buchner’s extensive review, 50 per cent of the lesions diagnosed in the first decade of life showed unerupted teeth associated with an odontoma, usually in the mandible. Moreover isolated cases have shown an association of 100 % between COC and unerupted teeth. In this case permanent first molars on either side are unerupted, which are supposed to erupt by the age of 6 years.
Due to the rarity of COC, the preoperative diagnosis is difficult to be done based only on clinical and radiographic features of the lesion. From a clinical and radiographic point of view, differential diagnosis included benign radiolucent lesions such as Dentigerous cyst, Central giant cell granuloma (CGCG), Keratocystic odontogenic tumor (KCOT), and ameloblastoma [18, 19]. Based on the fact that these lesions require different treatments, incisional biopsy and histopathological analysis are necessary for the final diagnosis. In this case incisional biopsy was planned under local anesthesia. Histopathological report was in favour of odontogenic cyst with chronic inflammation.
The CGCG (central giant cell granuloma) is one of the most important lesions to be discussed in the differential diagnosis, because, it occurs before the age of 30 years, affects anterior part of the jaws and 70 % of the cases involve mandible. Usually this lesion may present as a unilocular or multilocular radiolucency, often with poorly distinguished borders.
Other important lesion to be considered in the differential diagnosis is the KCOT that occurs over a wide age range, most commonly in the second and third decades, more frequently in men. Furthermore, the lesion affects mandible twice as often as maxilla. Ameloblastoma, specifically the unicystic type, is seen in the second or third decade of life, and must be included in the differential diagnosis. The KCOT, Ameloblastoma show slow growth; however present local invasive behaviour and high rate of recurrence if not treated with more aggressive procedures. On the other hand, the COC and CGCG exhibit slow growing but they are not invasive, generally involves only enucleation of the lesion.
The unilocular radiolucent aspect may simulate radicular cysts, lateral periodontal cysts, and if associated with the crown of an unerupted tooth, may resemble dentigerous cysts. The presence of radiopaque masses associated with a retained tooth and radiolucent areas suggest, however, that other lesions must be considered: Ameloblastic fibrodontoma, odontoameloblastoma and adenomatoid odontogenic tumor [20]. In present case unilocular radiolucencies, with presence of impacted permanent first molars, progressing root resorption, small fleck of calcifications point out that lesions could be a bilateral occurrence of calcifying epithelial odontogenic cyst.
The definitive diagnosis of COC is made histologically; COC shows normally cystic lining with tall columnar basal cells over which stellate reticulum like cells are seen. Intraepithelial ghost cells are evident. Surrounding connective tissue capsule consists of odontogenic islands, dentinoid and dystrophic calcification. In current case evidence of abundance of ghost cells and stellate reticulum like cells, in addition to clinic-radiological findings confirms the diagnosis of calcifying epithelial odontogenic cyst.
Although lesion can exhibit continuous growth due its neoplastic characteristics, simple enucleation and curettage is the treatment of choice. Periodic radiographic evaluation is recommended with more solid neoplastic variants. Although uncommon, recurrences of both cystic and solid lesions of COCs have been reported after 1–8 years. Recurrences, including patients in the first decade of life, have been observed 5 years or more after initial surgical therapy [20–23]. After the surgical treatment and follow up period of 7 months, the healing was normal with no signs of recurrence. COC has good prognosis; however we intend and continue to follow up the patient for further monitoring and documentation.
Conclusion
It is very important for the oral and maxillofacial surgeon to know how to recognize cystic lesions of oral cavity, as detailed examinations as well as the use of biopsy are necessary for an early diagnosis. As the occurrence of COC in first decade of life is not frequent and bilateral presentation is very rare, these lesions present with distinct behaviours, prognosis, and treatment planning depends upon their histological appearance.
Conflict of interest
None.
References
- 1.Freedman PD, Lumerman H, Gee JK. Calcifying odontogenic cyst: a review and analysis of seventy cases. Oral Surg Oral Med Oral Pathol. 1975;40:93–106. doi: 10.1016/0030-4220(75)90351-5. [DOI] [PubMed] [Google Scholar]
- 2.Toida M. So called calcifying odontogenic cyst: review and discussion on the terminology and classification. J Oral Pathol Med. 1998;27(2):49–52. doi: 10.1111/j.1600-0714.1998.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 3.Shear M. Cysts of the oral regions. Bristol: Wright PSG; 1983. pp. 79–86. [Google Scholar]
- 4.Buchner A. The Central (intraosseous) calcifying odontogenic cyst: an analysis of 215 cases. J Oral Maxillofac Surg. 1991;49:330–339. doi: 10.1016/0278-2391(91)90365-S. [DOI] [PubMed] [Google Scholar]
- 5.Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med. 2006;35(8):500–507. doi: 10.1111/j.1600-0714.2006.00455.x. [DOI] [PubMed] [Google Scholar]
- 6.Fejerskov O, Krough J. The calcifying ghost cell odontogenic tumor or the calcifying odontogenic cyst. J Oral Pathol. 1972;1:273–287. doi: 10.1111/j.1600-0714.1972.tb01666.x. [DOI] [PubMed] [Google Scholar]
- 7.Nagao T, Nakajima T, Fukushima M, et al. Calcifying odontogenic cyst with complex odontoma. J Oral Maxillofac Surg. 1982;40:810–813. doi: 10.1016/0278-2391(82)90180-X. [DOI] [PubMed] [Google Scholar]
- 8.Kramer IRH, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumors: a commentary on the second edition. Cancer. 1992;70:2988–2994. doi: 10.1002/1097-0142(19921215)70:12<2988::AID-CNCR2820701242>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 9.Hong SP, Ellis GI, Hariman KS. Calcifying odontogenic cyst: a review of ninety-two cases with reevaluation of their nature as cyst or neoplasms, the nature of ghost cells and subclassification. Oral Surg Oral Med Oral Pathol. 1991;72(1):56–64. doi: 10.1016/0030-4220(91)90190-N. [DOI] [PubMed] [Google Scholar]
- 10.Erasmus JH, Thompson IO, Von Rensbug IJ, Von der Westhuijzen AJ. Central odontogenic calcifying cyst: a review of the literature and the role of advanced imaging techniques. Dentomaxillofac Radiol. 1998;27(1):30–35. doi: 10.1038/sj.dmfr.4600315. [DOI] [PubMed] [Google Scholar]
- 11.Slootweg P. Odontogenic tumors are update. Curr Diagn Pathol. 2006;12:54–65. doi: 10.1016/j.cdip.2005.10.003. [DOI] [Google Scholar]
- 12.Gorlin RJ, Pindborg JJ, Clausen FP, et al. The calcifying odontogenic cyst: a possible analogue of the cutaneous calcifying epithelioma of Malherbe. Oral Surg Oral Med Oral Pathol. 1962;15:1235–1243. doi: 10.1016/0030-4220(62)90159-7. [DOI] [PubMed] [Google Scholar]
- 13.Praetorius F, Hjorting-Hansen E, Gorlin RJ, et al. Calcifying odontogenic cyst: range, variations and neoplastic potential. Acta Odontol Scand. 1981;39:227–240. doi: 10.3109/00016358109162284. [DOI] [PubMed] [Google Scholar]
- 14.Buchner A, Merrel PW, Carpenter WM. Relative frequency of central odontogenic tumors: as study of 1,088 cases from northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg. 2006;64(9):1343–1352. doi: 10.1016/j.joms.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira JAGP, da Silva CJ, Costa IM, Mota Loyola A (1995) Calcifying odontogenic cyst in infancy. J Dent Child 70–73 [PubMed]
- 16.Fernandes AM, Duarte EC, Pimenta FJ, Souza LN, Santos VR, Mesquita RA, et al. Odontogenic tumors a study of 340 cases in a Brazilian population. J Oral Pathol Med. 2005;34(10):583–587. doi: 10.1111/j.1600-0714.2005.00357.x. [DOI] [PubMed] [Google Scholar]
- 17.Lida S, Fakuda Y, Ueda T, Aikawa T, Anzpe JE, Okura M. Calcifying odontogenic cyst–radiological findings in 11 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):356–362. doi: 10.1016/j.tripleo.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 18.Mc Gowan RH, Brown RM. The calcifying odontogenic cyst: a problem of pre-operative diagnosis. Br J Oral Surg. 1982;20:203–212. doi: 10.1016/S0007-117X(82)80040-1. [DOI] [PubMed] [Google Scholar]
- 19.Sikes JW, Jr Gali GF, Troulis MJ. Expansile intra-osseous lesion of the maxilla. J Oral Maxillofac Surg. 2000;58(2):1395–1400. doi: 10.1053/joms.2000.18274. [DOI] [PubMed] [Google Scholar]
- 20.Wright BA, Bhardwaj AK, Murphy D. Recurrent calcifying odontogenic cyst. Oral Surg Oral Med Oral Pathol. 1984;58:579. doi: 10.1016/0030-4220(84)90083-5. [DOI] [PubMed] [Google Scholar]
- 21.Shafer WG, et al. Tratado de Patologia Bucal. 3. Rio de Janeiro: Interamericana; 1979. pp. 218–219. [Google Scholar]
- 22.Saito I, Suzuki T, Yamamura J, et al. Calcifying odontogenic cyst: case reports, variations and tumorous potential. J Nihon Univ Sch Dent. 1982;24:69–78. doi: 10.2334/josnusd1959.24.69. [DOI] [PubMed] [Google Scholar]
- 23.Shamaskin RG, Svirsky JA, Kaugar GE. Intraosseous and extraosseous calcifying odontogenic cyst (Gorlin cyst) J Oral Maxillofac Surg. 1989;47:562. doi: 10.1016/S0278-2391(89)80067-9. [DOI] [PubMed] [Google Scholar]


