Abstract
Abstract
TMJ ankylosis is one of the most disruptive anomaly that affects the masticatory system. The inability to move the mandible has significant functional ramification, such as the inability to eat a normal diet. Additionally, speech is affected, making it difficult for some individuals to communicate and express themselves to others. As there are several biologic and anatomic similarities to the mandibular condyles, autogenous costochondral grafts have been considered to be the most acceptable tissue for temporomandibular joint reconstruction. In addition donor site complications are infrequent and regeneration of the rib usually occurs within a year post operatively in children.
Aim
The aim of this study was to evaluate the function of costochondral grafts to replace the mandibular condyles and to assess the position, growth, overgrowth, function, success, failure and resorption of costochondral grafts.
Materials and Methods
Ten TMJ ankylosis patients were operated in the Department of Oral and Maxillofacial Surgery at Institute of Dental Sciences, Bareilly. Out of the 10 cases 6 were male patients and 4 female patients in age group of ≤14 years; of which 8 patients were of unilateral TMJ ankylosis and 2 were of bilateral TMJ ankylosis. All ten patients underwent interpositional gap arthroplasty with reconstruction of the condyle by costochondral graft.
Results
All patients with costochondral grafts had improved mandibular symmetry and growth with adequate mouth opening.
Conclusion
This study indicates that using costochondral grafts to reconstruct TMJ ankylosis in children provides a good result.
Keywords: Costochondral graft, Ankylosis, Temporomandibular joint, Temporomandibular joint reconstruction, Condyle
Introduction
The term ankylosis is derived from the Greek word meaning stiffening of a joint due to disease process, with fibrous or bony fusion. When the affliction occurs in the TMJ, the condylar head of the mandible fuses with glenoid fossa, obliterating the normal articulation and immobilizing the mandible [1–3].
TMJ ankylosis is one of the disruptive maladies that can afflict the masticatory system. The inability to move the mandible has significant functional ramification, such as the inability to eat a normal diet and difficulty in speaking, verbal expression and communication. When present in the young, growth disturbances of the mandible specifically creates facial asymmetries or severe mandibular deficiencies. Dental care becomes impossible and the patient often suffers from dental caries, periodontitis, premature loss of the teeth and inability for prosthetic replacement.
Ankylosis is most commonly associated with trauma, local or systemic infection or disease. In the case of trauma, it was hypothesized that intra-articular haematoma, with scarring and excessive bone formation, leads to hypo mobility. Infection of the TMJ is most commonly secondary to the contiguous spread from otitis media or mastoiditis but may also result from haematogenous spread, including tuberculosis, gonorrhea and scarlet fever. Systemic causes of TMJ ankylosis include ankylosing spondylitis, rheumatoid arthritis and psoriasis [4–6].
As the condyle is considered a primary mandibular growth centre, ankylosis causes interference with the development of the bone, and asymmetry will increase progressively until maturity is reached. In bilateral ankylosis, “bird-face” appearance may result and treatment of ankylosis is preferred as soon as the condition is established [7].
Regarding the treatment, surgical removal of the ankylotic mass as well as reconstruction of the TMJ with different types of materials is a most common method used for the TMJ ankylosis patient. Reconstruction of the TMJ with autogenous element represents one of the most intriguing and challenging operations in all of bone grafting.
The purpose of this study was to (i) evaluate the function of costochondral grafts used to replace the mandibular condyles (ii) evaluate radiographically the position, growth, overgrowth, function and resorption of the costochondral grafts (iii) assess the success and causes of failure of costochondral grafts.
Materials and Methods
Ten TMJ ankylosis patients were operated after informed consent and ethical committee clearance from the department of Oral and Maxillofacial Surgery, Institute of Dental Sciences, Bareilly. Six male patients and four female patients of age group ≤14 years were included in the study out of which eight patients were of unilateral TMJ ankylosis and two were of bilateral ankylosis. All patients underwent interpositional gap arthroplasty with reconstruction of the condyle with costochondral graft. The patients, TMJ were evaluated by orthopantomogram, transpharyngeal view of TMJ and CT scan. Each patient was subjected to complete hematological investigation. Clinically patients were evaluated pre and post operatively for facial asymmetry, joint movement, pain and inter-incisal distance.
Preoperatively the patients were evaluated radiographically for ankylosed mass, height of ramus. Postoperatively along with these parameters, the position, growth, overgrowth, calcification and resorption of the costochondral graft were evaluated.
Clinically and radiographically, patients were evaluated at intervals of 7 days, 3, 6 and 12 months post-operatively. Transpharyngeal view of TMJ was also used for seeing the position, growth and resorption of the costochondral graft. CT scan was used for the correct evaluation of ankylosed mass of TMJ preoperatively. The surgical methods used were pre auricular incision with Alkayat Bramley modification along with Gap Arthroplasty. The costochondral graft was taken from the 5th or 6th rib. Usually 2.5–3 cm of bone was harvested with a cap of 6–8 mm of cartilage. In bilateral cases two grafts were harvested from alternative ribs from the same side. Care was taken to preserve the perichondrium and periosteum at the bone cartilage junction to maintain adequate strength in this potentially fragile area. The graft was trimmed to the required length with a cartilaginous cap of about 5 mm. The costal cartilage and the bone were then trimmed and carved to resemble the condylar form. The overall size of the graft after reshaping was about 1.5–2.0 cm and of the cartilaginous cap was about 4–5 mm. Through the same exposure, the graft was inserted and oriented between glenoid fossa and mandibular ramus stump and fixed with stainless steel bone plate and screws.
Post operative panoramic radiographs were used to measure ramus height and to calculate mandibular ratio. The right and left ramus height were measured from the most superior point on the condyle to an intersection point between two tangents, one to the vertical ramus and other to the body of the mandible. The mandibular ratio was calculated by dividing the constructed ramus height by contralateral ramus height. Values were used to eliminate the variability factor between radiographs. If the value was less or more than 1, it denotes asymmetry of face, improvement in the value towards 1 denotes the improvement in the facial symmetry.
The following parameters were strictly followed in our patients:
The joint exposure, most commonly, was done by using the pre-auricular incision with Alkayat Bramley modification.
The ankylotic mass resection was followed by temporalis muscle and autogenous costochondral graft interposition and coronoidectomy if needed.
An intra operative mouth opening of more than 25 mm was achieved.
TMJ reconstruction was done using autogenous costochondral grafts.
Aggressive physiotherapy was started in the first post operative day itself using wooden spatulas. Great care was taken to educate the patients and their parents regarding the importance of physiotherapy.
Adequate motivation was given to patient for regular follow up.
Results
There were six male and four female patients of age ≤14 years with eight unilateral and two bilateral TMJ ankylosis. In all patients, the mean MIO was 4.10 mm with facial asymmetry (Fig. 1). Main etiological factor for ankylosis was trauma in eight patients and infection in two patients. Pre operative orthopantomogram (Fig. 2) and TMJ view (Fig. 3) showed ankylotic mass in right TMJ.
Fig. 1.

Pre-operative photograph
Fig. 2.

Pre-operative OPG
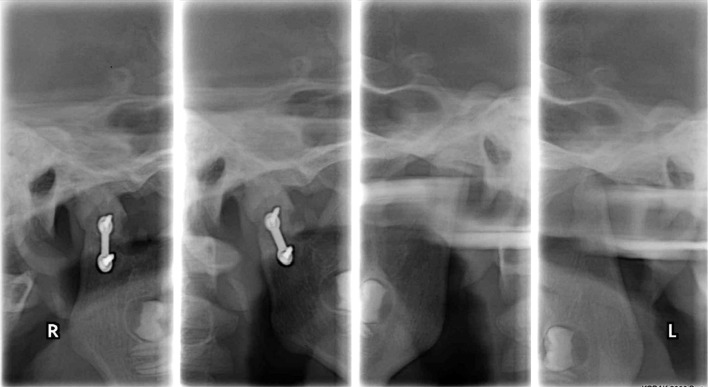
Fig. 3.
Pre-operative TMJ view
Satisfactory results was achieved in 8 out of 10 cases using costochondral grafts for the reconstruction of the joint after resection of the ankylosed mass, with adequate mouth opening of more than 25 mm in 8 patients (mean maximum interincisal opening (MIO) 35 mm in 8 out of 10 patients whereas overall MIO 28 mm), and reankylosis was seen in two cases because of lack of adequate physiotherapy and the patients were lost to proper follow-up (Table 1).
Table 1.
Maximum interincisal mouth opening in different time period
| Patient | Maximum interincisal mouth opening(in mm) | ||||
|---|---|---|---|---|---|
| Pre-op (mm) | 7th day (mm) | 3rd month (mm) | 6th month (mm) | 1 year (mm) | |
| 1. | 6 | 20 | 30 | 32 | 36 |
| 2. | 0 | 15 | 28 | 30 | 32 |
| 3. | 2 | 15 | 18 | 25 | 28 |
| 4. | 0 | 20 | 0 | 0 | 0 |
| 5. | 0 | 20 | 22 | 28 | 38 |
| 6. | 4 | 25 | 0 | 0 | 0 |
| 7. | 10 | 28 | 30 | 32 | 36 |
| 8. | 8 | 27 | 32 | 34 | 35 |
| 9. | 5 | 29 | 33 | 35 | 37 |
| 10. | 8 | 27 | 30 | 33 | 38 |
In 12 months follow up period, all patients who had ankylosis, reconstruction with costochondral grafts improved mandibular symmetry and growth with adequate mouth opening. Ratio of ramal height of both the sides was reduced which indicated the improvement in facial symmetry of the patient (Figs. 4, 5). Normal growth occurred in eight cases where grafts became completely mineralized, there was no over growth and resorption seen in any costochondral grafts, dislocation of the grafts from the glenoid fossa also occurred in one case where the screw was loose.
Fig. 4.

Post-operative OPG after 1 year
Fig. 5.
Post-operative TMJ view after 1 year
Some complications occurred intra operatively and post operatively. Pneumothorax occurred at the time of harvesting the costochondral grafts in one case which recovered within 2 days after the placement of inter-costal drain. Postoperatively perichondritis of ear occurred in one case which was resolved within 20 days. Facial nerve weakness also occurred in two cases which resolved within 6 months.
Paired t test was used to test the significant difference in radiographic measurement of the ratio of bilateral ramus height preoperatively, 7th day postoperative and consecutive 3, 6, 12 months started from 7th day postoperative. Significant difference of radiographic measurement in bilateral ramus height was observed between preoperative and 7th day postoperative, 3, 6, 12 months consecutively starting 7th postoperative day. The differences were at level of significance i.e. P < 0.01 (Table 2). However the maximum improvement of mouth opening was observed 7th day postoperative (425.58 %), and it was least between 7th day postoperative and 3rd month (1.32 %). Further the maximum improvement in radiographic measurement was observed from 7th day to 3rd month (22.97 %) and it was least between 6th month to 1 year (0.006 %) (Table 3). The MIO varied from 36 to 38 mm (Fig. 6). Repeated measure ANOVA revealed that there was statistically significant change in MIO over the group and time (P < 0.001) (Tables 4, 5).
Table 2.
Difference at different time periods of bilateral ramus height
| Time period | Mean difference ± SD | ‘t’ value | P value | Significance |
|---|---|---|---|---|
| Pre-op to 7th day | 0.207 ± 0.119 | 5.510 | <0.001 | Significant |
| Pre-op to 3 month | 0.467 ± 0.455 | 3.246 | 0.010 | Significant |
| Pre-op to 6 month | 0.476 ± 0.447 | 3.367 | 0.008 | Significant |
| Pre-op to 1 year | 0.482 ± 0.444 | 3.432 | 0.007 | Significant |
Table 3.
% Improvement in radiographic measurement and MIO
| Time period | Radiographic % | Mouth opening % |
|---|---|---|
| Pre-operative–7th day | 15.46 | 425.58 |
| 7th day–3rd month | 22.97 | 1.32 |
| 3rd month–6th month | 1.03 | 11.66 |
| 6th month–1 year | 0.006 | 12.44 |
Fig. 6.

Post-operative mouth opening
Table 4.
Repeated measure ANOVA (test of within-subjects effect)
| Source | Type III sum of squares | df | Mean square | F value | P value |
|---|---|---|---|---|---|
| Time | 3,456.68 | 4 | 864.170 | 15.933 | <0.001* |
| Error | 1,952.52 | 36 | 54.237 |
Repeated measure ANOVA revealed that there was statistically significant change in MIO over the time (P < 0.001)
* P < 0.001; Statistically significant at 1 %
Table 5.
Repeated measure ANOVA (test of between-subjects effect)
| Source | Type III sum of squares | df | Mean square | F value | P value |
|---|---|---|---|---|---|
| Group | 20,848.820 | 1 | 20,848.820 | 53.262 | <0.001* |
| Error | 3,522.980 | 9 | 391.442 |
Repeated measure ANOVA revealed that there was statistically significant change in MIO between the groups (P < 0.001)
* P < 0.001; Statistically significant at 1 %
Discussion
Ankylosis of the temporomandibular joint is a serious and disabling condition. Impairment of speech, difficulty with mastication, rampant caries poor oral hygiene, disturbances of facial and mandibular growth, and acute compromise of the airway invariably results in physical and psychological disability. This is particularly true of young children who are completely unable to open their mouth [4, 8, 9]. So, the treatment of TMJ ankylosis should start as soon as the condition is recognized in order to minimize the restriction of facial growth [10] discomfort and other complications associated with TMJ ankylosis.
The aim of surgical treatment of temporomandibular joint with using costochondral graft was to release the ankylosed mass and creation of gap to mobilize the joint and creation of a functional joint which improves patient’s nutrition, oral hygiene, and carry out necessary dental treatment along with reconstruction of the joint and restore the vertical height of the ramus, prevent recurrence, restore normal facial growth pattern(based on functional matrix theory) and to improve esthetics and rehabilitate the patient(cosmetic surgery may be carried out at a later date or at second stage by orthognathic surgery or distraction osteogenesis).
TMJ ankylosis presents a serious anesthetic challenge as rigid laryngoscopy is not possible. The report of the confidential enquiry into peri-operative deaths for England and Wales, 1986, revealed that difficult or failed intubations contributed to six of the 4,034 deaths [11]. Administration of anesthesia to patients with TMJ ankylosis ideally requires the availability of flexible fibreoptic bronchoscope, trained personnel who use the equipment and monitoring facilities. These facilities however, are lacking in many developing countries.
Blind intubation has its disadvantages which include high failure rate even in the hands of an expert, bleeding due to local trauma, secretions in the airway and distorted tissue anatomy which made it even more difficult especially in children [12]. Naveed and Sayeed [13] have described a technique of facilitating intubation by prior placement of an endotracheal tube into the oesophaghus followed by blind insertion of another endotracheal tube into the trachea. This technique of blind intubation may be helpful in reducing the psychological trauma and complications of elective tracheostomy.
Administration of general anesthesia has been a major problem in the above study because of small mandible and altered position of larynx, which make intubation more difficult. Blind nasal intubation and retrograde intubation when indicated always requires patient co-operation, which was very difficult to obtain from younger group of patients. Fibreoptic intubation technique was successfully used in these patients. Requirement of tracheostomy was also only in those cases where other intubation techniques failed.
Most authorities agree that recurrence of ankylosis is less likely when something is interposed between the two cut bony surfaces. Topazian compared gap and interpositional arthroplasties and reported 53 % incidence of recurrence, when the gap arthroplasty method was used without interposition.
So, interpositional arthroplasty involves creation of a gap, but in addition a barrier (autogenous or alloplastic) was inserted between the cut bony surface to minimize the risk of recurrence and to maintain the vertical height of the ramus.
The most widely accepted autogenous technique was costochondral graft, and as stated by Macintosh the advantages of this graft were its biological compatibility, workability, functional adaptability, and minimal additional detriment to the patient. The growth potential of the costochondral graft makes it an ideal choice in children [14].
Potential problems with the use of costochondral graft include fracture, further ankylosis, increased operating time, additional surgical site, donor site morbidity, and the variable growth behavior of the graft [15].
Some alloplastic materials and system have been developed for use in reconstruction of the TMJ. Alloplastic joints are said to allow a closer reproduction of the normal anatomy of the joint (with restoration of vertical dimension), avoidance of donor site morbidity, and reduction in operation time and reduction in the chance of recurrent ankylosis. All these factors allow immediate physiotherapy and rehabilitation with consequent increased benefit to the patient but there are potential disadvantages of alloplastic reconstruction relating mainly to wear or failure of the material. Wear particles can generate a giant cell foreign body reaction with potential loosening of the implant, resulting in occlusal change or displacement or fracture. Other problems relate to long-term stability, cost, dystrophic bone formation, and lack of growth which precludes the use of such joints in children [16].
The use of autogenous costochondral graft for TMJ reconstruction was first described by Gillies in 1920 [17]. It became popular for replacement of defective or missing mandibular condyles after many successful treatments had been reported. Clinically the graft provides the mandible with an active growth centre in children while in adults it prevents jaw deviation or production of an open bite in bilateral cases [18, 19].Costochondral grafting decreases the incidence of reankylosis after gap arthroplasty [20]. Recently, distraction osteogenesis has been used extensively to correct mandibular deformities after ankylosis but reconstruction of the joint with costochondral grafts is still indicated with, before or after distraction to reconstruct the joint and to keep the proper ramus height [21, 22].
Management of TMJ ankylosis is difficult. Several procedures can be used. Arthroplasty without interposition requires a gap of 10–20 mm [23–25] and often results in mouth deviation. For this reason it seems to be better to create a minimal gap (over 5 mm) and then perform interposition to prevent recurrence due to osteoblastic growth between the abraded bone surfaces [26, 27].
As with any grafting procedure, complications can be expected in rare instances from the recipient and donor sites. Early complications are seen as in other grafting procedures and include wound infection, loss of fixation, and exposure or fracture of the graft. Late complications at the recipient site may include unpredictable growth of the composite graft, nonunion, ankylosis or limited opening, and malocclusion. Late complications at the donor site include chronic pain, scarring, chest wall instability, and breast deformity.
Laurie and colleagues demonstrated that early morbidity (i.e., blood loss, pain, and wound healing problems) is more significant for the chest than for iliac donor site. Chest donor site morbidity is well described in the literature of greatest concerns in the early morbidity group are pleural laceration and pneumothorax. These complications have been reported as occurring anywhere from 4 to 30 % of the time. Occasionally a delayed pneumothorax occurs when the cut rib lacerates the pleura during respiration [28].
Superficial and deep wound infections rarely occur. Atelectasis is common and is caused by pain and attenuated respiratory effort. Pulmonary physical therapy and appropriate pain management can help to minimize these problems. Skouteris and colleagues reported no postoperative pulmonary complications in their subset of patients for whom bupivicaine subcostal blocks were administered. Lack of complications improved patient compliance with incentive spirometry and deep breathing and coughing exercises.
Laurie and colleagues also reported unaesthetic scarring and long-term pleuritic chest pain as being their most significant but rare chronic morbidities associated with costochondral graft harvest. More importantly, it has been stated that these chronic issues are not easily obviated by changes in surgical technique, as may be possible for iliac harvest.
Despite many reports that harvested ribs regenerate completely in children and partially in adults, Taggard et al. [29] reported significant chest wall deformities and thoracic scoliosis in their group of 18 patients who had microtia. The average follow-up was 8 years, and greater frequency of deformities have been noted when procurement was accomplished before age 10.
To avoid deforming the thorax, Brent [30] recommended certain modifications to the cartilage procurement procedure to obtain the ideal sculpting material. Harvesting has been emphasized only to create the framework, thus preserving maximum integrity of the chest wall. Chest deformities can be decreased considerably by preserving even a minimal rim of the upper margin of the sixth rib cartilage to obtain the basic ear shape of the framework. This precautionary measure retains a tether to the sternum so that the rib does not flare outward and potentially distort the chest as a child grows.
David et al. [31] reviewed 41 patients where rib graft was used and it was found to be relatively simple, reliable and safe procedure for obtaining autogenous bone and the incidence of pneumothorax was significantly lower. In this study, pneumothorax occurred in one case.
Many reports have documented the rationale for the use of costochondral graft in reconstruction of the TMJ. The costochondral graft adapts to function. Initially, its morphologic character does not resemble that of native condylar cartilage; however, it remodels over a period of time and eventually becomes similar to native condylar cartilage.
Whether the condyle acts by itself in producing change in mandibular dimension or incites a chondro-osseous proliferative response in its surrounding perichondrium and periosteum that evokes the same results was probably irrelevant in the clinical sense as long as the clinician understands that the condyle’s response is different from bones, and the ongoing adaptive capacity that is simulated by the cartilage at the costochondral junction [32].
There are three basic surgical objectives in the treatment of TMJ ankylosis. These are to establish joint movement, to prevent relapse and to achieve normal growth and development. Various autogenous grafts have been used in the reconstruction of the TMJ. These include the fibula, clavicle, sternoclavicular joint, iliac bone, metatarsal bone and metatarsal-phalangeal joint. The costochondral graft has gained popularity over the others in recent times. It offers several advantages which include biological and anatomic similarity to the mandibular condyle, low morbidity of the donor site, ease of obtaining and adapting the graft and the regenerative potential in the growing child [34]. It has almost similar primary and secondary cartilage to those of the mandibular condyle and therefore it was thought that its growth potential is similar to that of the condyle. It acts as an adaptive centre to promote symmetrical growth of the mandible and function as well as correction of mandibular retrognathia and laterognathia which overall improves the psychological outlook for both the patient and parent.
Conclusion
In the above study, recurrence was seen in two cases who were lost to follow-up and physiotherapy. Physiotherapy and regular follow up along with patient’s motivation and education is very much necessary for obtaining good result and for avoiding recurrence or reankylosis.
The result of this study indicates that using costochondral grafts to reconstruct TMJ ankylosis in children provides a good result. It provides autogenous material without the possibility of foreign body reaction, a cartilaginous articulating surface, the possibility of permanent bony union with ramus and provides biologic remodeling in response to function and growth potential.
Acknowledgments
Conflict of interest
None.
References
- 1.Kim YH, OH SH, JS Kim, et al. Total hip arthroplasty for treatment of osseous ankylosed hip. Clin Orthop Res. 2003;414:48–136. doi: 10.1097/01.blo.0000081935.75404.7f. [DOI] [PubMed] [Google Scholar]
- 2.Prodhomme G, Devoss S, Schuind F. Semi constrained total elbow: a case report. Chir Main. 2004;23:201–204. doi: 10.1016/j.main.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Hossain MA, Fraser MH. Outcome of Halo immobilization of cervical spine injury. Scott Med J. 2004;49:90–92. doi: 10.1177/003693300404900306. [DOI] [PubMed] [Google Scholar]
- 4.Adekeye EO. Ankylosis of the mandible: analysis of 76 cases. J Oral Maxillofac Surg. 1983;41:442–449. doi: 10.1016/0278-2391(83)90129-5. [DOI] [PubMed] [Google Scholar]
- 5.Ko EW, Huang CS, Chen YR (1999) Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac Surg 57:789–798 [DOI] [PubMed]
- 6.Guven O. Treatment of temporomandibular joint ankylosis by modified fossa prosthesis. J Craniomaxillofac Surg. 2004;32(4):236–242. doi: 10.1016/j.jcms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Rowe NL. Surgery of the TMJ. Proc R Soc Med. 1972;65:383–388. [PMC free article] [PubMed] [Google Scholar]
- 8.Posnick JC, Goldstein JA, et al. Surgical management of temporomandibular joint ankylosis in the pediatric population. Plast Reconstr Surg. 1993;91:791–798. doi: 10.1097/00006534-199304001-00006. [DOI] [PubMed] [Google Scholar]
- 9.Steinhauser EW. The treatment of ankylosis in children. Int J Oral Surg. 1973;2:129–135. doi: 10.1016/S0300-9785(73)80029-8. [DOI] [PubMed] [Google Scholar]
- 10.Manganella LC. Teporomandibular joint ankylosis: report of 14 cases. Int J Oral Maxillofac Surg. 2003;32:24–29. doi: 10.1054/ijom.2002.0308. [DOI] [PubMed] [Google Scholar]
- 11.American Society of Anaesthesiologists, Committee on Professional Liability (1988) Preliminary study of closed claims. ASA News letter 52: 8–10
- 12.Thompson AE. Issues in airway management in infants and children. Respir Care. 1999;44:650. [Google Scholar]
- 13.Naveed M, Sayeed A. Facilitated blind nasotracheal intubation in paralysed patients with temporomandibular joint ankylosis. JCPSP. 2005;15:4–6. [PubMed] [Google Scholar]
- 14.Macintosh RB. The use of autogenous tissues for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:63–69. doi: 10.1016/S0278-2391(00)80019-1. [DOI] [PubMed] [Google Scholar]
- 15.Link JO, Hoffman DC, Laskin DM. Hyperplasia of a costochondral graft in an adult. J Oral Maxillofac Surg. 1993;51:1392–1394. doi: 10.1016/S0278-2391(10)80148-X. [DOI] [PubMed] [Google Scholar]
- 16.Saeed NR, Hensher R. Reconstruction of the temporomandibular joint: autogenous compared with alloplastic. Br J Oral Maxillofac Surg. 2002;40:296–299. doi: 10.1016/S0266-4356(02)00139-0. [DOI] [PubMed] [Google Scholar]
- 17.Gillies HD. Plastic surgery of the face. London: Oxford University Press; 1920. pp. 177–189. [Google Scholar]
- 18.Ellen W, Ching KO, et al. Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac Surg. 1999;57:789–798. doi: 10.1016/S0278-2391(99)90816-9. [DOI] [PubMed] [Google Scholar]
- 19.Chen C, Lal J, Chen Y. Costochondral graft in acute mandibular condylar fracture. Plast Reconstr Surg. 1997;100:1234–1239. doi: 10.1097/00006534-199710000-00024. [DOI] [PubMed] [Google Scholar]
- 20.Qudah MA, Qudeimat MA, Almaaita J. Treatment of TMJ ankylosis in jordian children–a comparison of two surgical techniques. J Craniomaxillofac Surg. 2005;33:30–36. doi: 10.1016/j.jcms.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Jaquinet AR, Goudot P, Richter M. Costochondral grafting combined with mandibular distraction osteogenesis. A new approach to the correction of the temporomandibular joint ankylosis in an adult. A report of case. Ann Chir Plast Esthet. 2001;46:341–347. doi: 10.1016/S0294-1260(01)00039-5. [DOI] [PubMed] [Google Scholar]
- 22.Stelnicki EJ, Hollier L, Lee C, Lin WY, Grayson B, Mccarthy JG. Distraction osteogenesis of costochondral bone grafts in the mandible. Plast Recontr Surg. 2002;109:925–933. doi: 10.1097/00006534-200203000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Topazian RG. Etiology of ankylosis of the temporomandibular joint: analysis of 44 cases. J Oral Surg Anesth Hosp. 1964;22:227–233. [PubMed] [Google Scholar]
- 24.Lello GE. Surgical correction of temporomandibular joint ankylosis. J Craniomaxillofac Surg. 1990;18:19–26. doi: 10.1016/S1010-5182(05)80599-2. [DOI] [PubMed] [Google Scholar]
- 25.Rowe NL (1982) Ankylosis of the temporomandibular joint. Parts 1, 2 and 3. J R Coll Surg Edinb 27: 67–79,167–73,209–218 [PubMed]
- 26.Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966;4:405–409. [PubMed] [Google Scholar]
- 27.Deffez JP, Ferkadjki L, Allain P, et al. Treatment of ankylosed temporomandibular joint in post traumatic patient (temporomandibular joint ankylosis building) Rev Stomatol Chir Maxillofac. 1992;93:231–235. [Google Scholar]
- 28.Skouteris CA, Sotereanos GC, et al. Donor site morbidity following harvesting of autogenous rib grafts. J Oral Maxillofac Surg. 1989;47:808–812. doi: 10.1016/S0278-2391(89)80038-2. [DOI] [PubMed] [Google Scholar]
- 29.Taggard DA, Menezes AH, et al. Successful use of rib grafts for cranioplasty in children. Pediatr Neurosurg. 2001;34:149–155. doi: 10.1159/000056010. [DOI] [PubMed] [Google Scholar]
- 30.Brent B. Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg. 1999;104:319–334. doi: 10.1097/00006534-199908000-00001. [DOI] [PubMed] [Google Scholar]
- 31.David RJ, et al. Autogenous rib grafts in maxillofacial surgery. J Maxillofac Surg. 1983;11:201–203. doi: 10.1016/S0301-0503(83)80048-4. [DOI] [PubMed] [Google Scholar]
- 32.MacIntosh RB (1985) Current spectrum of costochondral grafting. In: Bell WH (ed) Surgical correction of dentofacial deformities: new concepts, Vol 3. Philadelphia, WB Saunders, pp 355–410