Abstract
Objective
Rapid plasma reagin (RPR) is frequently used to test women for maternal syphilis. Rapid syphilis immunochromatographic strip tests detecting only Treponema pallidum antibodies (single RSTs) or both treponemal and non-treponemal antibodies (dual RSTs) are now available. This study assessed the cost-effectiveness of algorithms using these tests to screen pregnant women.
Methods
Observed costs of maternal syphilis screening and treatment using clinic-based RPR and single RSTs in 20 clinics across Peru, Tanzania, and Zambia were used to model the cost-effectiveness of algorithms using combinations of RPR, single, and dual RSTs, and no and mass treatment. Sensitivity analyses determined drivers of key results.
Results
Although this analysis found screening using RPR to be relatively cheap, most (> 70%) true cases went untreated. Algorithms using single RSTs were the most cost-effective in all observed settings, followed by dual RSTs, which became the most cost-effective if dual RST costs were halved. Single test algorithms dominated most sequential testing algorithms, although sequential algorithms reduced overtreatment. Mass treatment was relatively cheap and effective in the absence of screening supplies, though treated many uninfected women.
Conclusion
This analysis highlights the advantages of introducing RSTs in three diverse settings. The results should be applicable to other similar settings.
Keywords: Africa, Cost-effectiveness analysis, Diagnostic algorithms, Latin America, Syphilis screening and treatment
1. Background
Antenatal syphilis causes a high burden of disease worldwide, with over half of pregnancies in women with untreated syphilis leading to adverse effects, including stillbirth, neonatal deaths, prematurity, and low birth weight [1]. Despite syphilis treatment being effective and inexpensive [2–4], many pregnant women remain undiagnosed owing to lack of symptoms and the unavailability of laboratories equipped to offer syphilis screening using traditional tests, such as rapid plasma reagin (RPR), in most antenatal care (ANC) clinics [5–7]. Recent improvements in syphilis screening have been made possible by the introduction of rapid syphilis tests (RSTs), which hold several advantages over the traditional RPR [8], including not requiring laboratory infrastructure (e.g. electricity and equipment) and their ability to be used correctly by different health professionals [9]. As such, they can be performed at the point of care, allowing for immediate treatment, and have been shown to be acceptable to patients [10,11]. However, most current RSTs are treponemal tests and are therefore reactive to both current and past syphilis infections [9]. In contrast, RPR is a non-treponemal test used to diagnose active infection despite its low sensitivity [12,13]. New dual RSTs with both treponemal and non-treponemal components have been recently developed [14,15], but currently cost US $2.50 per test, which is two to five times more than single treponemal tests.
Numerous studies have reported on the cost or cost-effectiveness of antenatal syphilis screening interventions [2,16–20,35], while others have modeled the cost-effectiveness of different screening approaches [21–25] or the burden and cost-effectiveness of national or regional screening programs [3,26]. All of these studies show that antenatal syphilis screening and treatment is highly cost-effective, but none has compared a broad range of possible screening and treatment approaches, nor have they accessed a detailed dataset for multiple countries to parameterize their models.
Using cost and outcome data from evaluations of the RPR and single RST in three countries, this study models the cost-effectiveness of maternal syphilis screening and treatment approaches in Peru, Tanzania, and Zambia.
2. Materials and methods
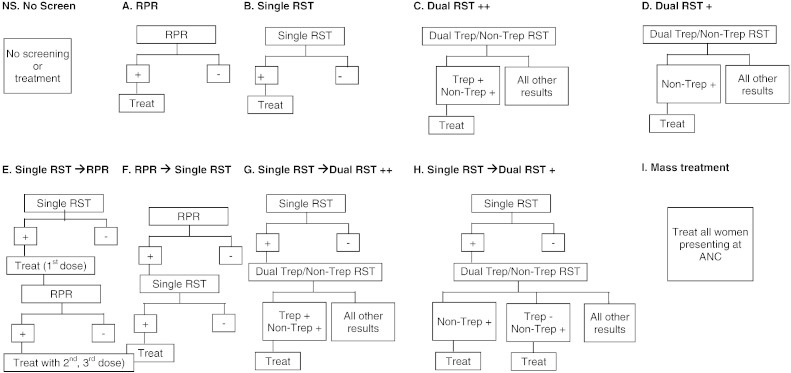
The present analysis considers 10 screening and treatment approaches (Fig. 1). Four approaches involve single tests (Fig. 1A–D), four entail a sequence of tests (Fig. 1E–H), and additional scenarios consider no screening or treatment (Fig. 1NS) and mass treatment without screening (Fig. 1I). Standardized facility-based data were used to model the cost-effectiveness of each approach.
Fig. 1.
Screening and treatment approaches. +, Only non-treponemal antibody test results used; ++, Dual RST – both treponemal and non-treponemal antibody test results used to determine a positive case; Trep, Treponemal antibody test result; non-Trep, Non-treponemal antibody test result; RPR, Rapid plasma reagin; RST, Rapid syphilis test.
2.1. Setting and primary data
Between 2009 and 2010, study clinics in Peru, Tanzania, and Zambia undertook operational research to estimate the cost-effectiveness of introducing treponemal-based RSTs for the screening of maternal syphilis in ANC and prevention of mother-to-child transmission of HIV programs [8,27]. Prior to introducing RSTs, a baseline assessment of current syphilis screening using the RPR test was undertaken, including collection of the numbers of women screened and treated, and the associated costs (Supplementary Material S1). Data from these studies [18,28; unpublished data] were used to parameterize the models.
Between 2009 and 2010, study clinics in Peru, Tanzania, and Zambia undertook operational research to estimate the cost-effectiveness of introducing treponemal-based RSTs for the screening of maternal syphilis in ANC and prevention of mother-to-child transmission of HIV programs [8,27]. Prior to introducing RSTs, a baseline assessment of current syphilis screening using the RPR test was undertaken, including collection of the numbers of women screened and treated, and the associated costs (Supplementary Material S1). Data from these studies [18,28; unpublished data] were used to parameterize the models.
Table 1 presents characteristics of the clinics in Peru, Tanzania, and Zambia. These three settings represent a range of maternal syphilis prevalence: 1.2% in Peru, 10.0% in Tanzania, and 12.4% in Zambia. Although all three countries had a national policy of universal antenatal syphilis screening, in the period prior to RST introduction, only about 60% of the studied facilities in these countries performed any syphilis screening using RPR. Average country screening rates during the baseline RPR period ranged from between 17.8% and 91.1%, improving to between 86.1% and 97.3% during the RST pilot. Average treatment rates also improved from between 56.7% and 76.8% at baseline to between 77.4% and 93.9% during the RST pilot. These improvements can be attributed to both the point-of-care nature of the RST test and the increased supervision given to clinics [8]. More details on each setting can be found elsewhere [18].
Table 1.
Overview of clinical screening by country.
| Inputs | RPR |
RST |
||||
|---|---|---|---|---|---|---|
| Peru | Tanzania | Zambia | Peru | Tanzania | Zambia | |
| Overview | ||||||
| Number of clinics | 6 | 9 | 5 | 6 | 9 | 5 |
| True prevalence | 1.25% | 5.14% | 9.04% | 1.25% | 5.14% | 9.04% |
| Time period for RPR costing | Mar–Nov 2009 | Sep 2008–Jun 2009 | Mar–Jul 2010 | Feb–Nov 2010 | Sep 2009–Jun 2010 | Mar–Jul 2010 |
| Program inputs | ||||||
| Percentage of ANC attendees screened | 91.13% | 17.79% a | 79.91% | 96.28% | 86.14% | 97.33% |
| (39.86–98.86) | (0–83.40) | (87.31–97.25) | (68.09 – 100) | (87.60–99.01) | ||
| Treatment rate | 76.77% | 74.07% | 56.70% | 88.57% | 93.89% | 77.36% |
| (33.33–100) | (46.00–90.49) | (0–95.00) | (75.00–100) | (83.81 – 100) | (66.67–100) | |
| Loss to follow-up | 76.77% | 74.07% | 56.70% | 88.57% | 93.89% | 77.36% |
| Number of attendees | 1482.4 | 449.2 | 286.6 | 1482.4 | 1,190.1 | 989.8 |
| (214–7002) | (85.0–1464) | (60.0–766) | (214–7002) | (196–1667) | (162–2379) | |
| Numbers testedb | 1351 | 79.9 | 229 | 1427.3 | 1025.1 | 963.4 |
| (119–6922) | (0.0–217) | (0.0–639) | (205–6810) | (196–3334) | (142–2348) | |
| Reactivity rates | 0.39% | 39.43% | 4.69% | 1.07% | 9.89% | 12.38% |
| (0.30–0.40) | (9.09–58.82) | (2.80–7.28) | (0.68–2.33) | (7.44–15.77) | (7.14–23.58) | |
| Numbers reactivec | 5.2 | 31.5 | 10.8 | 15.2 | 101.3 | 119.3 |
| (0.4–27.7) | (10.0–95.0) | (4.0–20.0) | (1.4–67.1) | (23.0–268) | (21.0–180) |
In Tanzania, antenatal attendance was not collected within the cost study, therefor an average screening rate during the RPR period across all pilot clinics was used.
Product of the Number of attendees and Percentage of ANC attendees screened.
Product of the Reactivity rate and Numbers tested.
2.2. Modeling
Outcomes and costs were modeled initially at the average observed scale of screening per country, converted to a common denominator of 1000 ANC attendees.
Data from each setting were collected on the number of women attending the clinic, number screened, proportion reactive for the RPR and single RST, number of women treated, and loss to follow-up (Table 1). An active syphilis case is traditionally defined as RPR positive, confirmed by a laboratory-based treponemal assay such as the Treponema pallidum particle agglutination (TPPA) or Treponema pallidum hemagglutination assay (TPHA). Field performance data (sensitivity and specificity) of the single RST and clinic-based RPR test against a laboratory-based RPR and TPPA test (Table 2) were used to estimate the proportion of reactive tests that were likely true syphilis cases. For Peru, detailed data were available to assess field performance. For Zambia and Tanzania, data from a field performance evaluation in South Africa were used [29]. The sensitivity of the dual RST was obtained from the literature [14,30]. The percentage of women with a single positive or negative RST result with different laboratory RPR and/or TPHA results is presented in Supplementary Table S1.
Table 2.
Test sensitivity and specificity characteristics and distributions assumed in probabilistic sensitivity analysis.
| Test characteristic | Peru | Tanzania and Zambia | Distribution | Source |
|---|---|---|---|---|
| Sensitivity of single RSTa | 77.2% (70.6%–83.0%) | 70.5% (54.8%–83.2%) | Binomial assumed on original sample size and probability of success, then divided by sample size to get proportion | Peru data and Bronzan et al. 2007 [29] |
| Specificity of single RSTa | 99.9% (99.9%–100%) | 92.9% (90.7%–94.8%) | ||
| Sensitivity of clinic RPRa | 55.7% (42.4%–68.5%) | 45.7% (28.8%–63.4%) | ||
| Specificity of clinic RPRa | 98.6% (97.1%–99.4%) | 96.6% (95.1%–98.2%) | ||
| Sensitivity of dual RST against lab TPHA | 96.4% (95.2%–97.6%) | 96.4% (95.2%–97.6%) | Normal distribution | Castro et al. 2010 [15] |
| Specificity of dual RST against lab TPHA | 99.1% (93.5%–97.0%) | 99.1% (93.5%–97.0%) | ||
| Sensitivity of dual RST against lab RPR | 88.6% (86.3%–90.7%) | 88.6% (86.3%–90.7%) | ||
| Specificity of dual RST against lab RPR | 98.6% (97.4%–99.3%) | 98.6% (97.4%–99.3%) |
Abbreviations: RPR, rapid plasma reagin; RST, rapid syphilis test; TPHA, Treponema pallidum hemagglutination assay.
Compared against laboratory based RPR and TPHA test.
Data from each setting were collected on the number of women attending the clinic, number screened, proportion reactive for the RPR and single RST, number of women treated, and loss to follow-up (Table 1). An active syphilis case is traditionally defined as RPR positive, confirmed by a laboratory-based treponemal assay such as the Treponema pallidum particle agglutination (TPPA) or Treponema pallidum hemagglutination assay (TPHA). Field performance data (sensitivity and specificity) of the single RST and clinic-based RPR test against a laboratory-based RPR and TPPA test (Table 2) were used to estimate the proportion of reactive tests that were likely true syphilis cases. For Peru, detailed data were available to assess field performance. For Zambia and Tanzania, data from a field performance evaluation in South Africa were used [29]. The sensitivity of the dual RST was obtained from the literature [14,30]. The percentage of women with a single positive or negative RST result with different laboratory RPR and/or TPHA results is presented in Supplementary Table S1.
The impact model estimated both the intermediate outcomes as well as final outcome measures: true cases treated, cases missed, and overtreatment. Further details of how specific outputs for each algorithm were calculated are given in Supplementary Material S2.
The impact model estimated both the intermediate outcomes as well as final outcome measures: true cases treated, cases missed, and overtreatment. Further details of how specific outputs for each algorithm were calculated are given in Supplementary Material S2.
Standard approaches were used to estimate disability-adjusted life years (DALYs) averted from treating pregnant women with syphilis [17,19,26]. Adverse outcomes averted were obtained from Gomez et al. [1]. Disability weights for congenital syphilis and low birth weight were 0.315 and 0.291, respectively. Stillbirth was treated as a full life lost and attributable adverse outcomes were captured through to end of life; country-specific life expectancies and a 3% discount rate were applied. Ranges applied in the sensitivity analysis were taken from the literature [3,31,32]. All DALY inputs are shown in Supplementary Table S2.
Standard approaches were used to estimate disability-adjusted life years (DALYs) averted from treating pregnant women with syphilis [17,19,26]. Adverse outcomes averted were obtained from Gomez et al. [1]. Disability weights for congenital syphilis and low birth weight were 0.315 and 0.291, respectively. Stillbirth was treated as a full life lost and attributable adverse outcomes were captured through to end of life; country-specific life expectancies and a 3% discount rate were applied. Ranges applied in the sensitivity analysis were taken from the literature [3,31,32]. All DALY inputs are shown in Supplementary Table S2.
Total and unit costs were estimated. Total costs allowed for basic comparisons of budget impact, while unit costs allowed for comparison of the efficiency of service delivery. The cost model applied a health systems approach (i.e. did not include patient costs). The model included average clinic level costs for health systems inputs, fixed clinic costs, and variable costs at the patient level to estimate total clinic costs per screening and treatment approach (Table 3). The model assumed that acceptability/uptake of treatment for all approaches would be the same as the single RST, including treating healthy mothers in the case of mass treatment, with the exception of the RPR test, for which the observed uptake was used. The model did not capture any averted treatment costs attributable to treating infants born alive to an infected mother or the costs of partner treatment. All costs are presented in 2012 US dollars.
Table 3.
Clinic cost inputs and distributions (costs are presented in 2012 US dollars).a
| Cost inputs | RPR |
RST |
||||
|---|---|---|---|---|---|---|
| Peru | Tanzania | Zambia | Peru | Tanzania | Zambia | |
| Fixed systems costs | 494.15 | 760.04 | 1,840.54 | |||
| (380–619) | (684–893) | (1502–2046) | ||||
| Fixed clinic costs | 1563.12 | 60.04 | 399.37 | 772.17 | 135.48 | 311.66 |
| (24.64–7150) | (45.61–76.89) | (185–645) | (320–2879) | (93.06–253) | (155–525) | |
| RPR equipment | 176.47 | 26.83 | 96.02 | |||
| (10.61–724) | (26.83–26.83) | (23.14–136) | ||||
| Screening costs | ||||||
| Personnel | 1.66 | 0.36 | 1.74 | 0.21 | 0.17 | 0.45 |
| (1.17–2.88) | (0.24–0.47) | (0.99–2.63) | (0.05–0.36) | (0.05–0.36) | (0.05–0.36) | |
| Test kits | 0.11 | 0.07 | 0.02 | 0.94 | 1.29 | 0.72 |
| Supplies and others | 0.99 | 0.79 | 0.2 | 0.38 | 0.18 | 0.09 |
| (0.78–1.28) | (0.67–0.91) | (0.11–0.3) | (0.33–0.66) | (0.04–0.42) | (0.02–0.16) | |
| Counselling costs | Counseling and treatment costs applied from RST observed costs |
|||||
| Negative | 0.19 | 0.03 | 0.15 | |||
| (0.11–0.55) | (0.02–0.08) | (0.07–0.35) | ||||
| Positive | 1.13 | 0.14 | 0.33 | |||
| (0.66–2.59) | (0.05–0.25) | (0.17–0.75) | ||||
| Treatment costs | ||||||
| Personnel first treatment | 1.08 | 0.29 | 0.3 | |||
| (0.783–1.94) | (0.15–0.51) | (0.23–0.36) | ||||
| Supplies (incl. drugs) | 0.63 | 0.74 | 0.69 | |||
| (0.58–0.78) | (0.61–0.95) | (0.63–0.82) | ||||
| Personnel second and third treatments | 0.32 | 0.29 | 0.3 | |||
| (0.23–0.77) | (0.15–0.51) | (0.23–0.36) | ||||
Abbreviations: RPR, rapid plasma reagin; RST, rapid syphilis test.
Point estimates are averages across facilities in each country, and ranges are lowest and highest values observed across the clinics.
Incremental cost-effectiveness ratios (ICERs; ratio of incremental costs over incremental benefits) are presented assuming a baseline of no screening (approach NS), though ICERs were also estimated for transitions from RPR to RST screening approaches. ICERs allow for comparisons of the efficiency of resource allocations for competing interventions.
2.3. Sensitivity analysis
A sensitivity analysis was undertaken to assess how robust the conclusions were to variations in the model parameters. The present study was unique in using data from different clinic settings in each country. This allowed incorporation of the observed variation in different model inputs as ranges in a probabilistic sensitivity analysis (PSA) considering the cost-effectiveness of each algorithm in each country. Model parameters not obtained from the clinics were obtained from the literature and uncertainty bounds were based on their 95% confidence intervals (CIs). All program and cost inputs were given a triangular distribution. Further details on the ranges and distributions used for all parameters are given in Tables 1–3, Supplementary Material S3, and Supplementary Table S2.
A sensitivity analysis was undertaken to assess how robust the conclusions were to variations in the model parameters. The present study was unique in using data from different clinic settings in each country. This allowed incorporation of the observed variation in different model inputs as ranges in a probabilistic sensitivity analysis (PSA) considering the cost-effectiveness of each algorithm in each country. Model parameters not obtained from the clinics were obtained from the literature and uncertainty bounds were based on their 95% confidence intervals (CIs). All program and cost inputs were given a triangular distribution. Further details on the ranges and distributions used for all parameters are given in Tables 1–3, Supplementary Material S3, and Supplementary Table S2.
For the PSA, sets of parameters were randomly sampled 1000 times from their uncertainty distributions for each algorithm and country. For each sampled parameter set, the impact and cost-effectiveness of each algorithm were estimated to determine the uncertainty in each model output. The point estimates for each output were used to rank the algorithms, whereas individual paired runs were used to assess the probability that one algorithm was more cost-effective than another in terms of cost per DALY averted. The runs were also used to assess to which model parameters the estimated cost and impact (DALYs averted) of the best performing algorithm were most sensitive.
Univariate sensitivity analyses also explored how sensitive the cost-effectiveness of algorithms A, B, and C (single RPR, RST, and dual test algorithms) was to changes in the cost of the dual test, prevalence of syphilis (0.5%, 1%, 5%, 10%), and increases in screening and treatment rates up to WHO targets for elimination of mother-to-child transmission of syphilis (95% for both) [33].
3. Results
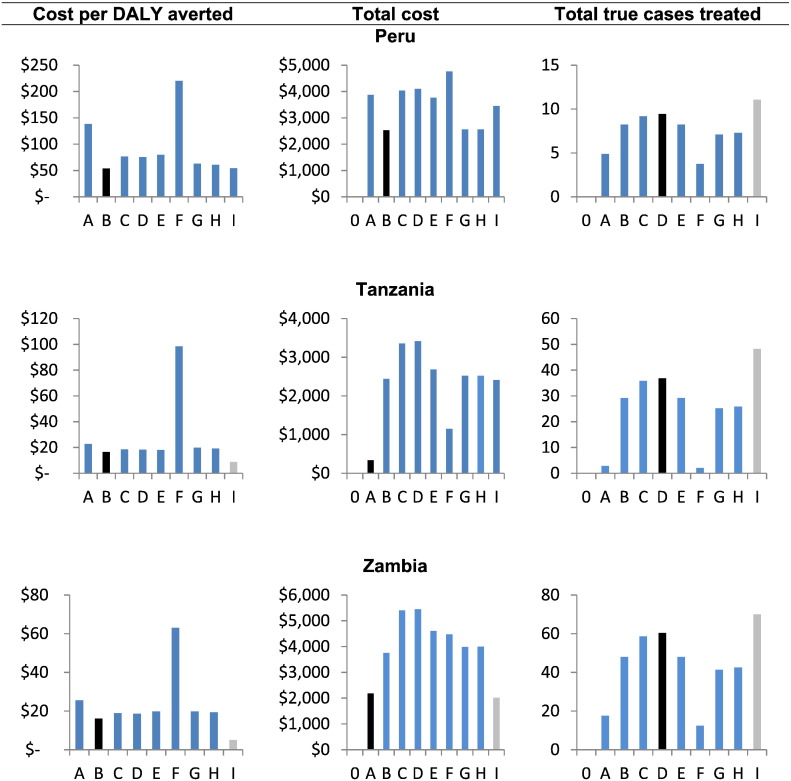
It is estimated that there would be 13, 51, and 90 true cases of maternal syphilis per 1000 ANC attendees in Peru, Tanzania, and Zambia, respectively (Table 4). In the absense of an ANC syphilis screenng programme (approach NS) no cases woudl be treated, whereas mass treatment (Approach I) would treat 11, 48, and 70 cases, assuming no treatment supply shortages (Fig. 2). Screening algorithms that used the clinic-based RPR test performed worse than algorithms using the RST, partly because of the poor sensitivity (43% to 55% when compared with laboratory-based RPR and TPHA) of the RPR test, as well as low screening rates for the RPR in these settings. This was particularly the case in Tanzania, where RPR screening rates were just 18%.
Table 4.
Impact and cost-effectiveness of the 10 screening and treatment approaches (costs are presented in 2012 US dollars).a
| NS. No Screen | A. Clinic RPR | B. Single RST | C. Dual treat ++ | D. Dual treat + | E. Single RST → RPR | F. Clinic RPR → Single RST | G. Single RST → Dual treat ++ | H. Single RST → Dual treat + | I. Mass treatment | |
|---|---|---|---|---|---|---|---|---|---|---|
| Peru | ||||||||||
| True cases treated | 0 | 4.9 | 8.2 | 9.2 | 9.5 | 8.2 | 3.8 | 7.1 | 7.3 | 11.1 |
| (2.0–9.4) | (5.8–16.5) | (6.4–18.3) | (6.7–18.9) | (5.8–16.5) | (1.6–7.3) | (5.0–14.2) | (5.2–14.7) | (8.0–22.9) | ||
| Missed cases | 12.5 | 7.6 | 4.3 | 3.3 | 3.1 | 4.3 | 8.7 | 5.4 | 5.2 | 1.4 |
| (9.2–25.6) | (6.1–18.9) | (3.1–10.0) | (2.5–8.2) | (2.2–7.6) | (3.1–10.0) | (6.9–20.4) | (4.1–12.3) | (3.8–11.8) | (0.4–4.2) | |
| Over-treated | 0 | 9.8 | 0.8 | 0.8 | 16.3 | 0.0 | 0.0 | 0.0 | 0.0 | 841.7 |
| (2.0–15.6) | (0.7–0.9) | (0.1–0.4) | (9.2–22.5) | (0.0–0.0) | (0.0–0.0) | (0.0–0.0) | 0.00.0 | (705–900) | ||
| Total $ | n.a. | 3873.8 | 2535.5 | 4036.6 | 4103.7 | 3762.8 | 4761.9 | 2558.8 | 2559.6 | 3454.8 |
| (2220–7549) | (1973–4404) | (3417–5874) | (3485–5952) | (2507–8918) | (2777–9923) | (2009–4424) | (2010–4425) | (2989–4810) | ||
| $/woman screened | n.a. | 4.25 | 2.63 | 4.19 | 4.26 | 3.91 | 4.95 | 2.66 | 2.66 | n.a. |
| (2.40–8.1) | (2.13–4.8) | (3.7–6.3) | (3.8–6.4) | (2.7–9.5) | (3.0–10.6) | (2.2–4.8) | (2.2–4.8) | |||
| $/woman treated | n.a. | 263.40 | 279.14 | 404.83 | 159.08 | 456.59 | 1,260.42 | 360.04 | 349.95 | 4.05 |
| (160–820) | (133–505) | (205–679) | (104–255) | (191–1,061) | (571–3,684) | (166–659) | (161–639) | (4.0–5.6) | ||
| $/DALY averted | n.a. | 138.58 | 53.69 | 76.66 | 75.75 | 79.68 | 220.52 | 62.91 | 61.17 | 54.41 |
| (56.9–544) | (19.8–135) | (27.6–182) | (27.2–179) | (27.9–252) | (86.2–891) | (24.0–158) | (22.9–153) | (21.2–130) | ||
| Tanzania | ||||||||||
| True cases treated | 0 | 2.90 | 29.3 | 35.8 | 36.8 | 29.3 | 2.0 | 25.2 | 26.0 | 48.2 |
| (0.4–23.0) | (5.5–74.9) | (6.4–94.6) | (6.6–98.4) | (5.5–74.9) | (0.3–15.3) | (4.8–64.4) | (5.0–66.8) | (8.9–130) | ||
| Missed cases | 51.4 | 48.5 | 22.1 | 15.6 | 14.6 | 22.1 | 49.3 | 26.2 | 25.4 | 3.1 |
| (9.3–142) | (8.2–129) | (3.8–74.1) | (2.9–50.4) | (2.6–47.4) | (3.8–74.1) | (8.5–13) | (4.8–82.5) | (4.6–81.1) | (0.4–13.4) | |
| Over-treated | 0 | 3.9 | 50.7 | 1.7 | 20.3 | 1.2 | 0.3 | 0.6 | 1.8 | 760.5 |
| (1.0–18.7) | (31.6–67.0) | (0.4–1.5) | (12.5–26.9) | (0.7–1.6) | (0.1–1.3) | (0.2–1.0) | (1.0–2.5) | (579–857) | ||
| Total $ | 0 | 334.6 | 2438.3 | 3354.0 | 3412.7 | 2682.6 | 1152.6 | 2519.5 | 2525.1 | 2413.6 |
| (202–1045) | (2186–4253) | (3000–5178) | (3049–5239) | (2417–4646) | (975–3264) | (2254–4339) | (2260–4344) | (1904–3118) | ||
| $/woman screened | n.a. | 1.9 | 2.8 | 3.9 | 4.0 | 3.1 | 6.5 | 2.9 | 2.9 | n.a. |
| (1.4–3.5) | (2.7–4.9) | (3.7–6.0) | (3.8–6.1) | (2.9–5.5) | (2.7–22.4) | (2.7–5.1) | (2.7–5.1) | |||
| $/woman treated | n.a. | 49.6 | 30.5 | 89.6 | 59.8 | 88.1 | 501.7 | 97.5 | 91.2 | 3.0 |
| (23.1–103) | (22.3–53.5) | (38.9–432) | (32.2–145) | (39.8–389) | (109–2,152) | (44.3–468) | (42.0–374) | (2.6–3.7) | ||
| $/DALY averted | n.a. | 22.8 | 16.5 | 18.6 | 18.4 | 18.1 | 98.4 | 19.8 | 19.3 | 8.7 |
| (5.7–155) | (5.7–109) | (6.0–124) | (5.9–121) | (6.4–116) | (17.8–770) | (7.0–130) | (6.8–125) | (2.2–56.2) | ||
| Zambia | ||||||||||
| True cases treated | 0 | 17.6 | 48.0 | 58.7 | 60.3 | 48.0 | 12.4 | 41.3 | 42.5 | 70.0 |
| (1.0–44.1) | (13.5–126) | (16.1–156) | (16.4–161) | (13.5–126) | (0.7–29.9) | (11.4–108) | (11.8–112) | (19.8–193) | ||
| Missed cases | 90.4 | 72.9 | 42.5 | 31.8 | 30.1 | 42.5 | 78.1 | 49.1 | 47.9 | 20.5 |
| (26.3–250) | (22.7–218.8) | (11.6–134) | (9.5–98.7) | (8.9–93.5) | (11.6–133) | (24.5–228) | (14.2–150) | (13.7–147) | (4.6–66.3) | |
| Over-treated | 0 | 12.7 | 45.2 | 1.5 | 18.1 | 1.1 | 0.8 | 0.6 | 1.6 | 683.0 |
| (1.2–19.7) | (28.1–59.2) | (0.3–1.3) | (11.2–22.9) | (0.6–1.4) | (0.1–1.4) | (0.2–0.8) | (0.9–2.1) | (499–768) | ||
| Total $ | 0 | 2,180.3 | 3,754.7 | 5,400.8 | 5,447.4 | 4,606.8 | 4,476.4 | 3,990.5 | 3,996.1 | 2,012.8 |
| (708–2843) | (2558–7039) | (4139–8729) | (4188–8771) | (3132–8931) | (2186–8304) | (2768–7426) | (2774–7432) | (1581–2522) | ||
| $/woman screened | n.a. | 2.2 | 3.9 | 5.6 | 5.6 | 4.7 | 4.6 | 4.1 | 4.1 | n.a. |
| (0.7–3.0) | (2.7–7.3) | (4.4–9.1) | (4.4–9.1) | (3.3–9.6) | (2.3–8.8) | (2.9–7.6) | (2.9–7.7) | |||
| $/woman treated | n.a. | 72.1 | 40.3 | 89.8 | 69.5 | 94.0 | 338.8 | 95.3 | 90.7 | 2.7 |
| (33.0–427) | (20.0–81.5) | (32.4–329) | (29.2–177) | (34.7–308) | (121–4,535) | (35.1–327) | (34.0–300) | (2.5–3.2) | ||
| $/DALY averted | n.a. | 25.5 | 16.1 | 18.9 | 18.6 | 19.8 | 63.1 | 19.9 | 19.3 | 5.0 |
| (8.0–254) | (4.3–76.5) | (5.0–86.9) | (4.9–84.2) | (5.7–92.6) | (19.6–1014) | (5.6–91.9) | (5.5–88) | (1.3–21.8) |
Abbreviations: + Algorithms using only non-treponemal test result; ++ Algorithms using treponemal and non-treponemal test results of the dual test; Arrow indicates second test following a positive first test; n.a., Not available; DALY, disability-adjusted life year; RPR, rapid plasma reagin; RST, rapid syphilis test.
Ranges for each outcome are 2.5 to 97.5 percentile range from probabilistic sensitivity analysis.
Fig. 2.
Comparison of approach by key indicators: health impact (total true cases averted), budget impact (total cost), and cost-effectiveness (cost per DALY averted), by country and screening and treatment approach. Costs are presented in 2012 US dollars. 0. None (No screening); A. Clinic RPR; B. Single RST; C. Dual treat ++; D. Dual treat +; E. Single RST → RPR; F. Clinic RPR → Single RST; G. Single RST → Dual treat ++; H. Single RST → Dual treat +; I. Mass treatment.
Using the dual test on its own resulted in the greatest number of true cases treated in all settings. Dual tests could trigger treatment based solely on the non-treponemal result (algorithms D and H) or based on both treponemal and non-treponemal reactivity (C and G). While the former had slight benefits in terms of fewer missed cases, it did increase overtreatment by 16- to 20-fold when used alone (D compared with C), or up to three times when used to confirm the single RST result (H compared with G). Finally, all sequenced algorithms reduced overtreatment relative to single tests, although, generally, the number of missed cases also increased owing to more false negatives.
3.1. Total costs
At the facility level (i.e. per 1000 ANC attendees screened), the RPR test was the cheapest screening and treatment approach in Tanzania (US $335) and Zambia (US $2180), while RST was the lowest cost approach in Peru (US $2535). While RPR test kits cost very little (US $0.02 to $0.11 per person screened), they are more labor intensive and labor costs were higher in Peru.
3.2. Cost-effectiveness
The cost per DALY averted provided a comparison of the screening and treatment algorithms relative to the baseline scenario of no screening. Approach B (single RST) was the most cost-effective diagnostic approach across all countries, while mass treatment was the most cost-effective treatment approach in the higher prevalence settings (Tanzania and Zambia). The dual test approaches (C, D, G, and H) performed well in terms of identifying true cases while reducing overtreatment, but at US $2.50 per test, they were not as cost-effective as approach B.
However, the single and dual RST algorithms cost much more than just using the clinic-based RPR test (algorithm A) in Tanzania and Zambia, highlighting that, in these settings, the RPR algorithm could be the best option if the budget is constrained, although limited impact is achieved (Supplementary Fig. S1). Conversely, in Zambia, mass treatment (US $5.02 per DALY averted) could also be a cheaper option for achieving greater impact albeit with considerable overtreatment. In Peru, the single RST algorithm (B) was both the cheapest and the most cost-effective option.
However, the single and dual RST algorithms cost much more than just using the clinic-based RPR test (algorithm A) in Tanzania and Zambia, highlighting that, in these settings, the RPR algorithm could be the best option if the budget is constrained, although limited impact is achieved (Supplementary Fig. S1). Conversely, in Zambia, mass treatment (US $5.02 per DALY averted) could also be a cheaper option for achieving greater impact albeit with considerable overtreatment. In Peru, the single RST algorithm (B) was both the cheapest and the most cost-effective option.
The incremental cost per facility of moving from using the clinic-based RPR (algorithm A) to single RST (algorithm B) was US $2104 and US $1574 (US $0.95 and US $1.13 per woman screened) in Tanzania and Zambia, respectively, while it would save US $1338 per facility (US $1.62 per woman screened) in Peru (Supplementary Fig. S1). This would achieve an additional 133, 148, and 19 DALYs averted in Tanzania, Zambia, and Peru, respectively, and was equivalent to an incremental cost per DALY averted of US $15.79 and US $10.64 in Tanzania and Zambia, respectively, while saving US $69 per DALY averted in Peru.
The incremental cost per facility of moving from using the clinic-based RPR (algorithm A) to single RST (algorithm B) was US $2104 and US $1574 (US $0.95 and US $1.13 per woman screened) in Tanzania and Zambia, respectively, while it would save US $1338 per facility (US $1.62 per woman screened) in Peru (Supplementary Fig. S1). This would achieve an additional 133, 148, and 19 DALYs averted in Tanzania, Zambia, and Peru, respectively, and was equivalent to an incremental cost per DALY averted of US $15.79 and US $10.64 in Tanzania and Zambia, respectively, while saving US $69 per DALY averted in Peru.
3.3. Probabilistic sensitivity analysis
The results of the PSA (Table 4 and Supplementary Fig. S2) emphasized the substantial variability/uncertainty in all model outputs. However, despite this uncertainty, the analysis suggested that the first choice algorithm (B) using the single RST had the lowest cost per DALY averted in over 74% of model simulations in all three settings. Analyses of covariance showed that the variability in the DALYs averted for this algorithm was mainly due to variability in the single RST reactivity rate (accounting for 37% to 62% of variability) across different clinics and uncertainty in the discount rate (27% to 53% of variability). Conversely, variability in the total cost was mainly driven by variability in ANC attendance (75% to 95%) across different clinics, followed by fixed clinic costs (1% to 17.7%) and screening coverage rates (0.2% to 8.2%). Despite these results highlighting that there was large between-clinic variation in the costs and impact, the uncertainty analysis suggests the results were largely robust and insensitive to this variability.
The results of the PSA (Table 4 and Supplementary Fig. S2) emphasized the substantial variability/uncertainty in all model outputs. However, despite this uncertainty, the analysis suggested that the first choice algorithm (B) using the single RST had the lowest cost per DALY averted in over 74% of model simulations in all three settings. Analyses of covariance showed that the variability in the DALYs averted for this algorithm was mainly due to variability in the single RST reactivity rate (accounting for 37% to 62% of variability) across different clinics and uncertainty in the discount rate (27% to 53% of variability). Conversely, variability in the total cost was mainly driven by variability in ANC attendance (75% to 95%) across different clinics, followed by fixed clinic costs (1% to 17.7%) and screening coverage rates (0.2% to 8.2%). Despite these results highlighting that there was large between-clinic variation in the costs and impact, the uncertainty analysis suggests the results were largely robust and insensitive to this variability.
3.4. Univariate sensitivity analysis
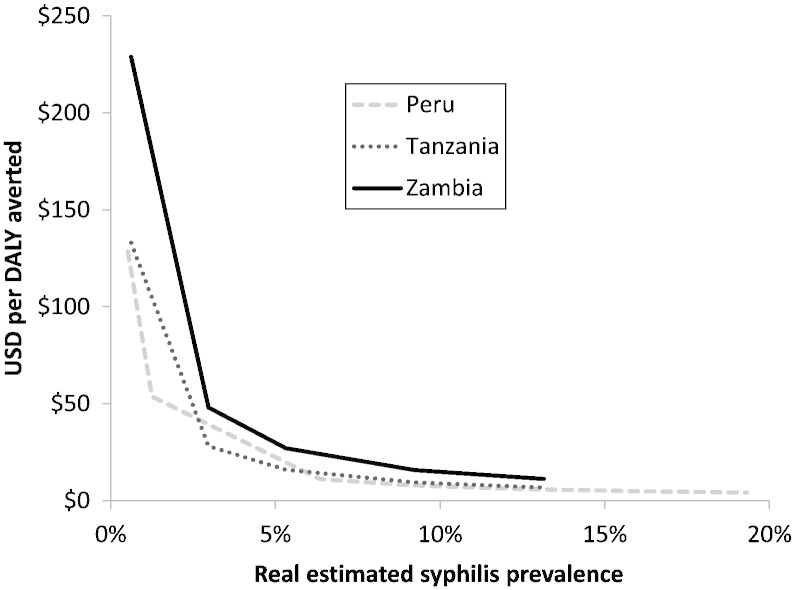
Univariate sensitivity analysis showed that, for the dual RST (C) to achieve the same cost per DALY averted as the single RST (B), the dual test price would need to drop from US $2.50 to US $2.07 in Tanzania, US $1.67 in Zambia, and US $1.24 in Peru. There was also a strong inverse relationship between the cost per DALY averted and true syphilis prevalence because greater impact was achieved at higher prevalence and the fixed costs of screening were spread between these outcomes (Fig. 3). However, this did not affect the relative ordering of the algorithms, except for mass treatment, which became relatively cheaper in higher prevalence settings.
Fig. 3.
The relationship between cost-effectiveness (US $/DALY averted) and true syphilis prevalence. Costs are presented in 2012 US dollars.
The cost-effectiveness of screening and treatment could be improved if the rates were strengthened. With the RPR, average ANC screening rates were 18% to 91% with treatment rates of 57% to 77%. Introduction of the RST improved this, with screening rates increasing to 86% to 97% and treatment rates to 77% to 94%. If countries achieve the WHO target of 95% for screening and treatment [33], the cost per DALY averted would drop marginally (3%) for RST to US $50, US $16, and US $14 in Peru, Tanzania, and Zambia, respectively. Greater improvements (42%) would occur for the RPR because of the lower testing and treatment rates, and this would become the most cost-effective approach in Tanzania.
4. Discussion
The present study used observed data from clinic-based evaluations of RPR and RST in Peru, Tanzania, and Zambia to model the cost-effectiveness of 10 screening and treatment approaches being explored by WHO and other partners. Despite being the most widely applied approach, maternal syphilis screening using the RPR test leaves many women unscreened, results in high numbers of missed cases, and considerable overtreatment.
This study shows how the introduction of a treponemal-based RST increased the access to and effectiveness of screening, identifying most (54% to 66%) true cases at the initial visit, encouraging high treatment rates, and was more cost-effective than any other screening approach considered in all settings. However, some policymakers are concerned about overtreatment owing to the failure of treponemal tests to distinguish between past and current syphilis. Sequentially combining tests or using new dual treponemal and non-treponemal RSTs could greatly improve this issue. However, this would require a budget expansion of at least 38% above what is needed for the single RST at current prices. Nevertheless, if prices halve, the dual RST would be the most cost-effective.
To our knowledge, this is the first study to estimate the cost-effectiveness of mass treatment for averting adverse birth outcomes attributable to maternal syphilis infection, showing that, in high prevalence settings, mass treatment can be the cheapest alternative with the fewest missed cases. An advantage of mass treatment is that it overcomes the problem of stockouts of syphilis testing supplies, which can occur with both RPR and RST. Mass treatment could also reduce the stigma related to a positive syphilis test if all pregnant women are treated regardless of status. However, mass treatment is a controversial approach. A core concern is adverse reaction to benzathine penicillin, which occurs in approximately 2 per 1 000 000 people treated [34]. Further concerns arise around the inability to identify infected partners, the feasibility of delivering treatment to all ANC attendees in terms of infrastructure and human resource capacity on the providers’ side, and the willingness of pregnant women to accept treatment without knowingly being infected. It would be useful for future syphilis screening and treatment guidelines to evaluate the advantages and disadvantages of mass treatment, particularly during diagnostic and supply stockouts. Ultimately, it is a decision that must be taken by country policymakers and practitioners considering the epidemiologic context and balancing the potential risks and benefits to mothers and their infants.
As with all cost-effectiveness analyses, this analysis has its strengths and limitations. While site-specific sensitivity and specificity data were available for the single RST and clinic-based RPR for Peru, clinical performance data for Tanzania and Zambia had to be obtained from South Africa [29]. It was assumed that no treatment was available for infants born to mothers infected with syphilis, which may have overestimated the benefit and costs of the interventions. Further, averted treatment costs among live-born infants affected by maternal syphilis and treatment benefits among adults were not accounted for. This renders the cost-effectiveness results conservative relative to the no treatment scenario. While there was a large variation between clinics, the sample of clinics was too small to explore key clinic level drivers of variation in cost-effectiveness such as geographical remoteness and scale. In the current approach, averages per clinic were considered, treating each clinic as an observation so as to capture variation across clinics. Ideally, this would have been weighted appropriately relative to the number and type of facilities in each country.
5. Conclusions
The present study models the cost-effectiveness of different screening and treatment approaches for maternal syphilis using detailed costing and clinical data. This strengthens the realism and generalizability of the results compared with studies drawing on inputs from published sources. The analysis suggested that the single RST should be considered the best screening option unless the price of the dual RST is significantly reduced. Because of its poor performance, the clinic-based RPR should only be considered in severely resource-restricted settings where it may be the cheapest option, but misses many cases. In contrast, sequential testing regimens were costly but could minimize overtreatment. More research is required to determine the optimal situations for mass treatment, no treat the highest number of cases at low cost but without resulting in substantial overtreatment, which would lead to ethical concerns.
The following are the supplementary data related to this article.
Primary costing methods
Specific calculations for each algorithm
Sensitivity analysis
Percentage of women with single positive or negative RST result with different laboratory RPR and TPHA results. Not sampled but adjusted based on the sampled sensitivity of the RST with range given in Table 2.
DALY inputs and range used in probabilistic sensitivity analysis (PSA).
Frontier plot of total cost (in 2012 US dollars) and total DALYs averted. Approaches are more advantageous the closer to the North-West corner they lie.
Comparison of approach by key indicators, with uncertainty bounds shown (2.5 to 97.5 percentile range from probabilistic sensitivity analysis). Costs are presented in 2012 US Dollars.
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.ijgo.2015.04.007.
Acknowledgments
The original data collection for this work was supported by the Bill and Melinda Gates Foundation (Grant 47697). The present analysis was funded by a grant from the Department of Reproductive Health and Research, WHO.
Conflict of interest
The authors declare that they have no conflicts of interest.
References
- 1.Gomez G.B., Kamb M.L., Newman L.M., Mark J., Broutet N., Hawkes S.J. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ. 2013;91(3):217–226. doi: 10.2471/BLT.12.107623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blandford J.M., Gift T.L., Vasaikar S., Mwesigwa-Kayongo D., Dlali P., Bronzan R.N. Cost-effectiveness of on-site antenatal screening to prevent congenital syphilis in rural Eastern Cape Province, Republic of South Africa. Sex Transm Dis. 2007;34(7 Suppl):S61–S66. doi: 10.1097/01.olq.0000258314.20752.5f. [DOI] [PubMed] [Google Scholar]
- 3.Kahn J.G., Jiwani A., Gomez G.B., Hawkes S.J., Chesson H.W., Broutet N. The cost and cost-effectiveness of scaling up screening and treatment of syphilis in pregnancy: a model. PLoS One. 2014;9(1):e87510. doi: 10.1371/journal.pone.0087510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hook E.W., 3rd, Marra C.M. Acquired syphilis in adults. N Engl J Med. 1992;326(16):1060–1069. doi: 10.1056/NEJM199204163261606. [DOI] [PubMed] [Google Scholar]
- 5.Trepka M.J., Bloom S.A., Zhang G., Kim S., Nobles R.E. Inadequate syphilis screening among women with prenatal care in a community with a high syphilis incidence. Sex Transm Dis. 2006;33(11):670–674. doi: 10.1097/01.olq.0000216032.52731.ea. [DOI] [PubMed] [Google Scholar]
- 6.Munkhuu B., Liabsuetrakul T., Chongsuvivatwong V., Geater A., Janchiv R. Coverage of antenatal syphilis screening and predictors for not being screened in Ulaanbaatar, Mongolia. Sex Transm Dis. 2006;33(5):284–288. doi: 10.1097/01.olq.0000194577.71693.c7. [DOI] [PubMed] [Google Scholar]
- 7.Yang L.G., Tucker J.D., Wang C., Shen S.Y., Chen X.S., Yang B. Syphilis test availability and uptake at medical facilities in southern China. Bull World Health Organ. 2011;89(11):798–805. doi: 10.2471/BLT.11.089813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mabey D.C., Sollis K.A., Kelly H.A., Benzaken A.S., Bitarakwate E., Changalucha J. Point-of-care tests to strengthen health systems and save newborn lives: the case of syphilis. PLoS Med. 2012;9(6):e1001233. doi: 10.1371/journal.pmed.1001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.TDR . WHO; Geneva: 2003. Diagnostics Evaluation Series No. 1: Laboratory-based evaluation of rapid syphilis diagnostics. http://www.who.int/tdr/publications/tdr-research-publications/sdi/en/ [Google Scholar]
- 10.Mishra S., Naik B., Venugopal B., Kudur P., Washington R., Becker M. Syphilis screening among female sex workers in Bangalore, India: comparison of point-of-care testing and traditional serological approaches. Sex Transm Infect. 2010;86(3):193–198. doi: 10.1136/sti.2009.038778. [DOI] [PubMed] [Google Scholar]
- 11.Lee D., Fairley C., Cummings R., Bush M., Read T., Chen M. Men who have sex with men prefer rapid testing for syphilis and may test more frequently using it. Sex Transm Dis. 2010;37(9):557–558. doi: 10.1097/olq.0b013e3181d707de. [DOI] [PubMed] [Google Scholar]
- 12.Dorigo-Zetsma J.W., Belewu D., Meless H., Sanders E., Coutinho R.A., Schaap A. Performance of routine syphilis serology in the Ethiopian cohort on HIV/AIDS. Sex Transm Infect. 2004;80(2):96–99. doi: 10.1136/sti.2003.005827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gwanzura L., Latif A., Bassett M., Machekano R., Katzenstein D.A., Mason P.R. Syphilis serology and HIV infection in Harare, Zimbabwe. Sex Transm Infect. 1999;75(6):426–430. doi: 10.1136/sti.75.6.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin Y.P., Chen X.S., Wei W.H., Gong K.L., Cao W.L., Yong G. A dual point-of-care test shows good performance in simultaneously detecting nontreponemal and treponemal antibodies in patients with syphilis: a multisite evaluation study in China. Clin Infect Dis. 2013;56(5):659–665. doi: 10.1093/cid/cis928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castro A.R., Esfandiari J., Kumar S., Ashton M., Kikkert S.E., Park M.M. Novel point-of-care test for simultaneous detection of nontreponemal and treponemal antibodies in patients with syphilis. J Clin Microbiol. 2010;48(12):4615–4619. doi: 10.1128/JCM.00624-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larson B.A., Lembela-Bwalya D., Bonawitz R., Hammond E.E., Thea D.M., Herlihy J. Finding a needle in the haystack: the costs and cost-effectiveness of syphilis diagnosis and treatment during pregnancy to prevent congenital syphilis in Kalomo District of Zambia. PLoS One. 2014;9(12):e113868. doi: 10.1371/journal.pone.0113868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schackman B.R., Neukermans C.P., Fontain S.N.N., Nolte C., Joseph P., Pape J.W. Cost-effectiveness of rapid syphilis screening in prenatal HIV testing programs in Haiti. PLoS Med. 2007;4(5):e183. doi: 10.1371/journal.pmed.0040183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sweeney S., Mosha J.F., Terris-Prestholt F., Sollis K.A., Kelly H., Changalucha J. The costs of accessible quality assured syphilis diagnostics: informing quality systems for rapid syphilis tests in a Tanzanian setting. Health Policy Plan. 2014;29(5):633–641. doi: 10.1093/heapol/czt049. [DOI] [PubMed] [Google Scholar]
- 19.Terris-Prestholt F., Watson-Jones D., Mugeye K., Kumaranayake L., Ndeki L., Weiss H. Is antenatal syphilis screening still cost effective in sub-Saharan Africa. Sex Transm Infect. 2003;79(5):375–381. doi: 10.1136/sti.79.5.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levin C.E., Steele M., Atherly D., Garcia S.G., Tinajeros F., Revollo R. Analysis of the operational costs of using rapid syphilis tests for the detection of maternal syphilis in Bolivia and Mozambique. Sex Transm Dis. 2007;34(7 Suppl):S47–S54. doi: 10.1097/01.olq.0000245986.62775.b6. [DOI] [PubMed] [Google Scholar]
- 21.Liu C., Ou Q., Chen H., Chen J., Lin S., Jiang L. The diagnostic value and performance evaluation of five serological tests for the detection of Treponema pallidum. J Clin Lab Anal. 2014;28(3):204–209. doi: 10.1002/jcla.21667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Owusu-Edusei K., Jr, Gift T.L., Ballard R.C. Cost-effectiveness of a dual non-treponemal/treponemal syphilis point-of-care test to prevent adverse pregnancy outcomes in sub-Saharan Africa. Sex Transm Dis. 2011;38(11):997–1003. doi: 10.1097/OLQ.0b013e3182260987. [DOI] [PubMed] [Google Scholar]
- 23.Owusu-Edusei K., Jr, Koski K.A., Ballard R.C. The tale of two serologic tests to screen for syphilis–treponemal and nontreponemal: does the order matter? Sex Transm Dis. 2011;38(5):448–456. doi: 10.1097/OLQ.0b013e3182036a0f. [DOI] [PubMed] [Google Scholar]
- 24.Vickerman P., Peeling R.W., Terris-Prestholt F., Changalucha J., Mabey D., Watson-Jones D. Modelling the cost-effectiveness of introducing rapid syphilis tests into an antenatal syphilis screening programme in Mwanza, Tanzania. Sex Transm Infect. 2006;82(Suppl. 5):v38–v43. doi: 10.1136/sti.2006.021824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rydzak C.E., Goldie S.J. Cost-effectiveness of rapid point-of-care prenatal syphilis screening in sub-Saharan Africa. Sex Transm Dis. 2008;35:775–784. doi: 10.1097/OLQ.0b013e318176196d. [DOI] [PubMed] [Google Scholar]
- 26.Kuznik A., Lamorde M., Nyabigambo A., Manabe Y.C. Antenatal syphilis screening using point-of-care testing in sub-Saharan African countries: a cost-effectiveness analysis. PLoS Med. 2013;10(11):e1001545. doi: 10.1371/journal.pmed.1001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peeling R.W., Holmes K.K., Mabey D., Ronald A. Rapid tests for sexually transmitted infections (STIs): the way forward. Sex Transm Infect. 2006;82(Suppl. 5):v1–v6. doi: 10.1136/sti.2006.024265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strasser S., Bitarakwate E., Gill M., Hoffman H., Musana O., Phiri A. Introduction of rapid syphilis testing within prevention of mother-to-child transmission of HIV programs in Uganda and Zambia: a field acceptability and feasibility study. J Acquir Immune Defic Syndr. 2012;61(3):e40–e46. doi: 10.1097/QAI.0b013e318267bc94. [DOI] [PubMed] [Google Scholar]
- 29.Bronzan R.N., Mwesigwa-Kayongo D.C., Narkunas D., Schmid G.P., Neilsen G.A., Ballard R.C. Onsite rapid antenatal syphilis screening with an immunochromatographic strip improves case detection and treatment in rural South African clinics. Sex Transm Dis. 2007;34(Suppl. 7):S55–S60. doi: 10.1097/01.olq.0000245987.78067.0c. [DOI] [PubMed] [Google Scholar]
- 30.Castro A.R., Mody H.C., Parab S.Y., Patel M.T., Kikkert S.E., Park M.M. An immunofiltration device for the simultaneous detection of non-treponemal and treponemal antibodies in patients with syphilis. Sex Transm Infect. 2010;86(7):532–536. doi: 10.1136/sti.2010.042937. [DOI] [PubMed] [Google Scholar]
- 31.Jamison D.T., Shahid-Salles S.A., Jamison J., Lawn J.E., Zupan J. Incorporating deaths near the time of birth into estimates of the global burden of disease. In: Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J.L., editors. Global Burden of Disease and Risk Factors. World Bank; Washington, DC: 2006. Chapter 6. [PubMed] [Google Scholar]
- 32.World Health Organization . Global Health Estimates Technical Paper WHO/HIS/GHE/2013.4. WHO; Geneva: 2013. WHO methods and data sources for glabal burden of disease estimates 2000–2011. [Google Scholar]
- 33.World Health Organization . WHO; Geneva: 2014. Global guidance on criteria and processes for validation: elimination of mother-to-child transmission (EMTCT) of HIV and syphilis. [Google Scholar]
- 34.Galvao T.F., Silva M.T., Serruya S.J., Newman L.M., Klausner J.D., Pereira M.G. Safety of benzathine penicillin for preventing congenital syphilis: a systematic review. PLoS One. 2013;8(2):e56463. doi: 10.1371/journal.pone.0056463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shelley Katharine D., Ansbro Éimhín M., Ncube Alexander Tshaka, Phiri Anne, Sweeney Sedona, Fleisher Colette, Mumba Grace Tembo, Gill Michelle M., Strasser Susan, Peeling Rosanna W., Terris-Prestholt Fern. Integrating point-of-care syphilis testing into antenatal care in Zambia: An economic evaluation to compare cost and quality differences between pilot and national rollout implementation. PLoS One. 2015 doi: 10.1371/journal.pone.0125675. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primary costing methods
Specific calculations for each algorithm
Sensitivity analysis
Percentage of women with single positive or negative RST result with different laboratory RPR and TPHA results. Not sampled but adjusted based on the sampled sensitivity of the RST with range given in Table 2.
DALY inputs and range used in probabilistic sensitivity analysis (PSA).
Frontier plot of total cost (in 2012 US dollars) and total DALYs averted. Approaches are more advantageous the closer to the North-West corner they lie.
Comparison of approach by key indicators, with uncertainty bounds shown (2.5 to 97.5 percentile range from probabilistic sensitivity analysis). Costs are presented in 2012 US Dollars.