In the second paragraph of the Results the sentence describing the number of studies receiving non-profit or no support should read “The majority of studies adopted a Bayesian framework (n = 214, 67%) and either received non-profit or no support (n = 217, 69%).”
In the final paragraph of the Results the percentage of studies with a closed loop is incorrect. The correct sentence should read “Among studies with a closed loop, i.e., three or more included treatments had been compared in head-to-head trials, 31% did not report the consistency of direct and indirect evidence.”
Under Publication Date the p value for 62% versus 79% should read (62% versus 79%, p = 0.0005).
Under Source of Financial Support the p value for 49% versus 28% in the first paragraph should read (49% versus 28%, p = 0.0003).
Under Source of Financial Support the second paragraph should read “Industry-supported studies more often used a Bayesian framework (77% versus 63%, p = 0.0191), and adjusted for study covariates (38% versus 25%, p = 0.0205); however, they less often performed a risk of bias assessment of included studies (54% versus 77%, p∠0.0001), and, for closed loop studies, less often compared the consistency of direct and indirect evidence (39% versus 79%, p∠0.0001).”
In the Discussion the third paragraph should read “An interesting finding is that industry-sponsored studies more often used a Bayesian framework”
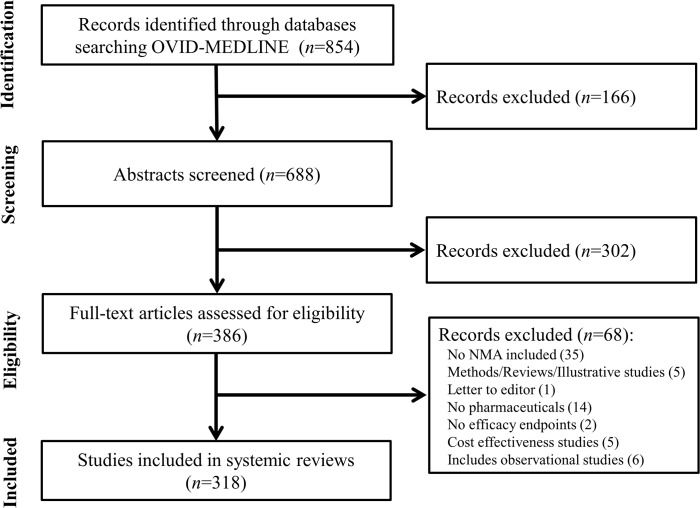
Fig 1 is incorrect in the published article. Please see the correct Fig 1 here.
Fig 1. Identification of network meta-analyses included in review.
There are errors in Table 1 and Table 2 of the published article. Please see the correct tables here.
Table 1. Frequency of network meta-analyses (n = 318) by year, indication, and country.
| Year study published† | n |
| 1997 | 1 (0.3%) |
| 2003 | 3 (0.9%) |
| 2004 | 1 (0.3%) |
| 2006 | 3 (0.9%) |
| 2007 | 3 (0.9%) |
| 2008 | 9 (2.8%) |
| 2009 | 16 (5.0%) |
| 2010 | 21 (6.9%) |
| 2011 | 44 (13.8%) |
| 2012 | 66 (20.4%) |
| 2013 | 78 (24.5%) |
| 2014 (through July 31st) | 73 (23.0%) |
| International Statistical Classification of Diseases (ICD) disease categories | n |
| Blood Disease | 3 (0.9%) |
| Circulatory System | 64 (20.1%) |
| Digestive System | 13 (4.1%) |
| Endocrine, Nutritional, Metabolic, and Immunity | 28 (8.8%) |
| Genitourinary System | 7 (2.2%) |
| Infectious and Parasite Disease | 14 (4.4%) |
| Mental and Behavioral Disorder | 13 (4.1%) |
| Musculoskeletal System and Connective Tissue | 45 (14.2%) |
| Neoplasm | 39 (12.3%) |
| Nervous System and Sensory Organs | 33 (10.4%) |
| Respiratory System | 20 (6.3%) |
| Skin and Subcutaneous Tissues | 9 (2.8%) |
| Other | 30 (9.4%) |
| Country | n |
| USA | 81 (25.5%) |
| UK | 79 (24.8%) |
| Canada | 28 (8.8%) |
| Italy | 21 (6.6%) |
| China | 16 (5.0%) |
| France | 14 (4.4%) |
| The Netherlands | 10 (3.1%) |
| Germany | 8 (2.5%) |
| Brazil | 6 (1.9%) |
| Switzerland | 6 (1.9%) |
| Taiwan | 6 (1.9%) |
| Greece | 5 (1.6%) |
| Spain | 4 (1.3%) |
| Other | 34 (10.7%) |
| Type of pharmaceutical intervention included | n |
| Multiple pharmaceuticals compared | 304 (95.6%) |
| Study included a non pharmaceutical treatment (e.g., surgery, exercise, counselling, etc) | 30 (9.4%) |
| Different strengths of the same pharmaceutical compared (e.g., simvastatin 20mg vs. 40mg) | 82 (25.8%) |
| Treatments in the same drug class grouped together as a comparator (e.g., beta-blockers, or statins) | 75 (23.6%) |
| Multiple modes of administration of a drug compared (e.g., oral, sublingual, intramuscular, etc) | 10 (3.1%) |
† We limited our literature search to studies published in the medical literature. We did not include NMAs submitted to national health technology assessment agencies unless also published in the Ovid-MEDLINE database. * ‘Other countries’ includes Greece, Ireland, Singapore, Australia, Cameroon, Denmark, Finland, Hong Kong, Korea, Norway, Poland, and Portugal.
Table 2. Assessment of network meta-analysis study characteristics.
| Assessment criteria | All studies (n = 318) | Journal quality (n = 301)* | Date of study publication (n = 318) | Source of study support (n = 315)** | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low impact factor (<3.534) (n = 147) | High impact factor (≥3.534) (n = 154) | p-value | Older studies (published prior to 2013) (n = 167) | Recent studies (2013, 2014) (n = 151) | p-value | Industry support (n = 98) | Non-Industry support/ no support (n = 217) | p-value | ||
| General study characteristics | ||||||||||
| Number of treatments compared | 6.3 (±6.4) | 6.8 (±8.5) | 6.0 (±3.9) | 0.3136 | 6.0 (±4.2) | 6.7 (±8.2) | 0.3816 | 5.9 (±3.6) | 6.5 (±7.3) | 0.446 |
| Total number of studies | 32.9 (±45.5) | 28.3 (±38.6) | 36.5 (±46.9) | 0.0992 | 30.5 (±50.2) | 35.5 (±50.2) | 0.3341 | 22.7 (±29.4) | 37.4 (±50.5) | 0.0079 |
| Total number of patients | 26875 (±65936) | 21938 (±46061) | 33292 (±82859) | 0.1549 | 23711 (±49899) | 30460 (±80375) | 0.3732 | 10945 (±13183) | 33864 (±77635) | 0.005 |
| HTA region (UK, AUS and Canada)† | 110 (35%) | 50 (34%) | 56 (36%) | 0.6709 | 68 (41%) | 42 (28%) | 0.0156 | 48 (49%) | 62 (28%) | 0.0003 |
| Journal impact factor | 5.5 (±6.2) | NA | NA | NA | 5.8 (±6.5) | 5.2 (±5.9) | 0.3791 | 3.1 (±1.7) | 6.5 (±7.1) | <0.0001 |
| Study method | ||||||||||
| Bayesian framework | 214 (67%) | 91 (62%) | 109 (71%) | 0.1038 | 106 (63%) | 108 (72%) | 0.1273 | 75 (77%) | 139 (63%) | 0.0191 |
| Risk of bias assessment of included studies | 223 (70%) | 100 (68%) | 111 (72%) | 0.4446 | 103 (62%) | 120 (79%) | 0.0005 | 53 (54%) | 170 (77%) | <0.0001 |
| Adjustment for covariates | 92 (29%) | 35 (24%) | 51 (33%) | 0.0744 | 54 (32%) | 38 (25%) | 0.1601 | 37 (38%) | 55 (25%) | 0.0205 |
| Random effects model*** | 221 (70%) | 98 (67%) | 114 (75%) | 0.1609 | 116 (69%) | 106 (71%) | 0.7453 | 67 (68%) | 155 (71%) | 0.6243 |
| Assessment of model fit | 127 (40%) | 53 (36%) | 70 (45%) | 0.0979 | 69 (41%) | 58 (38%) | 0.5985 | 46 (47%) | 81 (37%) | 0.0894 |
| Sensitivity analysis | 179 (56%) | 73 (50%) | 96 (62%) | 0.0267 | 88 (53%) | 91 (60%) | 0.1752 | 57 (58%) | 122 (58%) | 0.6542 |
| Consistency of direct and indirect evidence reported**** (closed loop studies only, n = 167) | 116 (69%) | 39 (57%) | 73 (79%) | 0.0017 | 57 (66%) | 59 (73%) | 0.3606 | 16 (39%) | 100 (79%) | <0.0001 |
| Study transparency and reproducibility | ||||||||||
| Search terms reported | 254 (80%) | 112 (76%) | 129 (84%) | 0.1007 | 129 (77%) | 125 (83%) | 0.2201 | 61 (62%) | 193 (88%) | <0.0001 |
| Network diagram | 194 (61%) | 85 (58%) | 101 (66%) | 0.1671 | 103 (62%) | 91 (60%) | 0.7974 | 62 (63%) | 132 (60%) | 0.5829 |
| Extracted data from contributing clinical studies | 206 (65%) | 87 (60%) | 106 (69%) | 0.0955 | 116 (69%) | 91 (60%) | 0.1011 | 58 (60%) | 149 (68%) | 0.1726 |
| Table of key clinical study characteristics | 286 (90%) | 128 (87%) | 141 (92%) | 0.2084 | 145 (87%) | 141 (93%) | 0.0527 | 89 (91%) | 197 (90%) | 0.729 |
| Model code (Bayesian framework only, n = 214) | 35 (16%) | 9 (6%) | 24 (16%) | 0.0085 | 24 (14%) | 11 (7%) | 0.0439 | 8 (8%) | 27 (12%) | 0.2811 |
| Presentation of study findings | ||||||||||
| Full matrix of head-to-head comparisons | 203 (64%) | 84 (57%) | 108 (70%) | 0.0191 | 110 (66%) | 93 (62%) | 0.4294 | 44 (45%) | 159 (73%) | <0.0001 |
| Reported probability of being best (Bayesian framework only, n = 214) | 87 (41%) | 32 (22%) | 51 (33%) | 0.0277 | 41 (25%) | 46 (30%) | 0.2389 | 25 (26%) | 62 (28%) | 0.623 |
| Ranking of included treatments (Bayesian framework only, n = 214) | 67 (31%) | 26 (18%) | 40 (26%) | 0.0829 | 29 (17%) | 39 (26%) | 0.0664 | 11 (11%) | 56 (26%) | 0.0031 |
† Regions in which submissions to HTA agencies generally require a NMA
* 17 studies published in journals with no associated impact factor
** 3 studies for which source of study support was unclear
*** 77 studies reported both fixed and random effects models, 38 studies did not report models used
**** Consistency only reported for studies with a closed loop
Reference
- 1. Chambers JD, Naci H, Wouters OJ, Pyo J, Gunjal S, Kennedy IR, et al. (2015) An Assessment of the Methodological Quality of Published Network Meta-Analyses: A Systematic Review. PLoS ONE 10(4): e0121715 doi:10.1371/journal.pone.0121715 [DOI] [PMC free article] [PubMed] [Google Scholar]