Abstract
Background & objectives:
Morbidity is self reported at a higher rate among the rich than the poor. However, objective measures suggest the contrary. We examined the role of epidemiological transition in wealth related inequalities in self-reported morbidity (SRM).
Methods:
We analyzed data of two States, Bihar and Kerala, from 60th Round of National Sample Survey (NSS). Bivariate analysis was performed to study the associations between various socio-demographic variables and self-reported morbidity. A prediction model based on hierarchical logistic regression was developed to identify determinants of self-reported morbidity.
Results:
In Bihar, acute morbidities (26 per 1000) were reported more often than chronic morbidities (19 per 1000) while in Kerala the reverse was true (89 acute and 123 chronic morbidities per 1000 person). In both the states, the rate of SRM showed an increasing trend from the poorest to the richest quintiles. The rising gradient in the odds of SRM across increasing socio-economic strata was more pronounced in Bihar [OR (richest)=2.52; 1.85-3.42] as compared to Kerala [OR (richest) =1.66; 1.37-2.0]. Moreover, this gradient was more on account of chronic diseases [OR (richest) =2.7; 1.8-4.0] for Bihar; [OR (richest) =1.6; 1.26-2.0 for Kerala] than the acute diseases [OR (richest) =1.82; 1.1-2.9 for Bihar]; [OR (richest) =1.4; 1.1-1.8 for Kerala].
Interpretation & conclusions:
The present analysis shows that the epidemiologic transition results in higher prevalence and reporting of chronic ailments by the rich than the poor. This phenomenon is more evident in the early stages of transition. In later stages of transition, positional objectivity plays an important role to explain wealth related inequalities in SRM.
Keywords: Epidemiologic transition, inequalities in health status, inequity, positional objectivity, self-reported morbidity
Despite rapid gains on economic and health fronts worldwide, including India, there are widespread inequalities in both income growth and health status1,2,3,4. Health status of a society is probably the best measure of its social well-being5, which brings us to the question of measurement of health status. There are various objective and subjective measures of health status which include measures of morbidity, mortality, disability and quality of life. The information on health status can be obtained from myriad sources namely self-reporting, care-givers, physician records, hospitalization records, death registers, etc. depending on the nature, course, severity and outcome of the illness.
Self-reported morbidity (SRM) is one of the common methods used in large nationwide surveys to assess the health status of a population6,7,8. Such self-reported morbidity based studies find the rich reporting more illnesses. However, the objective measures like life expectancy or mortality rates reveal the contrary; the poor afflicted more than the rich. This ‘reporting heterogeneity bias9 is common in self reports of health status. Hence, despite their advantages it is essential to interpret these with caution given the various influences these are subject to10. Though SRM has good face validity, problems arise when comparisons are made across classes11.
One of the explanations for the differences in the self-reported morbidity and objective measurements of well-being is the concept of positional objectivity12. The rich may be more aware and conscious about their health status and thus in a better position to appraise their own health status than the poor. The poor, on the other hand, are afflicted by the unmet basic needs of life which push health further down in their priority list. In addition to poor awareness of ill-health, health care accessibility and affordability issues further discourage the poor from recognizing, reporting and seeking care for ill health. Another probable explanation for this dichotomy in objective measurements of health status and self-reported ill health is differential rates of epidemiological transition between different socio-economic strata13. India has been facing rapid epidemiologic transition and hence is burdened by communicable and non-communicable diseases (NCD) alike14. An intra-nation analogy would be that the richer States are ahead of poorer States in epidemiologic transition. The NCDs are chronic diseases with longer duration and high prevalence and are likely to be reported in the reference period. If the rates of NCDs are different in different strata of the society, this can affect the rate of SRM. We used the National Sample Survey (NSS) data from the 60th Round on Morbidity and Health Care15 to test this hypothesis, i.e. whether the higher rates of SRM among the rich were contributed by the higher rates of chronic NCDs among the rich. In this study we analysed the self-reported morbidity patterns of Kerala and Bihar States in India, apparently at the extremes of the performance with respect to demographic and epidemiological transition and economic development.
Material & Methods
Data source: The National Sample Survey 60th Round on Morbidity and Health Care was a nationwide sample survey carried out on a nationally representative sample of households. The 60th Round covered the whole of Indian Union except few geographically inaccessible areas. Data on household consumer expenditure, employment-unemployment and morbidity and healthcare were collected7. The baseline socio-economic and demographic characteristics of the households were collected. The inquiry on morbidity was conducted with a reference period of 15 days. Ailment was defined as illness or injury, any deviation from the state of physical and mental well-being. All spells of ailment suffered by each member, both present as well as the deceased, of the sample household, during the 15 days preceding the date of enquiry, whether or not, the patient sought treatment, were covered in the survey.
Rational for choice of two States: Bihar and Kerala: Kerala and Bihar are at different levels of epidemiological transition. Kerala has apparently entered the third or final phase of the demographic transition characterized by low death rate and declining birth rate leading to a slowdown in the growth rate of population. Thus, as of 2011 census, the birth rate in Kerala was estimated as a little over 14.7 (per 1000 population), as against 22.5 for all-India. The crude death rate of Kerala was 6.8 (per 1000 population), compared to the national average of 7.3.
The mortality trends of Kerala have been reported to be comparable to that of industrialized nations with a predominance of NCD deaths. Death rates from non-infectious diseases in rural Kerala are as high as in parts of the developed world16,17,18. Kerala and Bihar are at extremes of health and development related indicators infant mortality rate (IMR, 13 vs 48), maternal mortality ratio (MMR, 95 vs 312), crude birth rate (CBR, 14.7 vs 28.5), crude death rate (CDR, 6.8 vs 8.1), female literacy rate (87.72 vs 33.12) and total fertility rate (TFR, 1.7 vs 3.9)2. The recent figures for cardiovascular diseases (CVD) risk factor prevalence in rural Kerala suggested that in people aged 20 yr or older, 20 per cent had type 2 diabetes mellitus, 42 per cent had hypertension, 70 per cent had hypercholesterolaemia, and 40 per cent were overweight (body mass index >25 kg/m2). Kerala has a cardiovascular mortality rate twice that of the USA16,17,18,19.
Analysis: The data from Kerala and Bihar were analyzed and the reported ailments were classified into acute and chronic based on the nature of ailments entered in the data sheet. Infections of the gastrointestinal, reproductive and respiratory tracts, skin and eye infections and febrile illnesses including malaria were classified as acute ailments. Diseases of the cardiovascular system, obstructive lung diseases, tuberculosis, cancer, neurological and psychiatric conditions were classified as chronic ailments. Ailments like ‘other diagnosed’ and ‘other undiagnosed’ that were ambiguous and could not be classified as acute or chronic were excluded.
The morbidity rate is presented as the proportion of ailing persons (PAP) which is the proportion of persons reporting ailment suffered at any time during the reference period. Bivariate analysis was performed to study the associations between various socio-demographic variables and PAP of the States. Some variables were merged in view of small data size, e.g. among religion, Christianity and others was merged. The factors affecting PAP for both the States were analyzed separately and combined to understand the inter- State and intra- State associations between variables. A prediction model based on logistic regression was developed to represent the predictors or determinants of self-reported morbidity. Other socio-demographic factors representing social inequalities in health in India were controlled20 like area (rural or urban), age, sex, education, religion and caste21. State-wise separate models were developed for predicting the reporting of any ailment and for specifically reporting acute or chronic morbidity. For Bihar and Kerala, a hierarchical regression model was developed by adding variables one by one in model. The final model was arrived at based on the Log likelihood function and chi-square statistic.
Results
A total of 37184 respondents, 23851 from Bihar and 13333 from Kerala constituted the sample. The proportion of respondents aged above 60 yr was 6.8 per cent in Bihar and 12.8 per cent in Kerala. Females constituted 47 and 53 per cent of the respondents from Bihar and Kerala, respectively. The proportion of respondents from Bihar who were illiterate was 56.9 per cent as against to only 21.3 per cent from Kerala. Among the respondents, 84.1 per cent from Bihar and 64.8 per cent from Kerala were residents of rural areas. Thirty four per cent respondents from Bihar belonged to the poorest quintile compared to only 8.1 per cent from Kerala.
In Bihar, 1093 patients reported suffering from any ailment during the 15 days reference period amounting to a PAP rate of 45 per 1000. In Kerala, the PAP rate was 212 per 1000. In Bihar, acute morbidities were reported at a rate of 26 per 1000 and chronic morbidities at a rate of 19 per 1000 population accounting for 57.6 and 42.4 per cent of the total morbidities, respectively. In Kerala, acute and chronic morbidities were reported at the rate of 89 and 123 per 1000 population, respectively (Table I).
Table I.
Self-reported morbidity rates (per 1000 population) for acute and chronic ailments in Bihar and Kerala
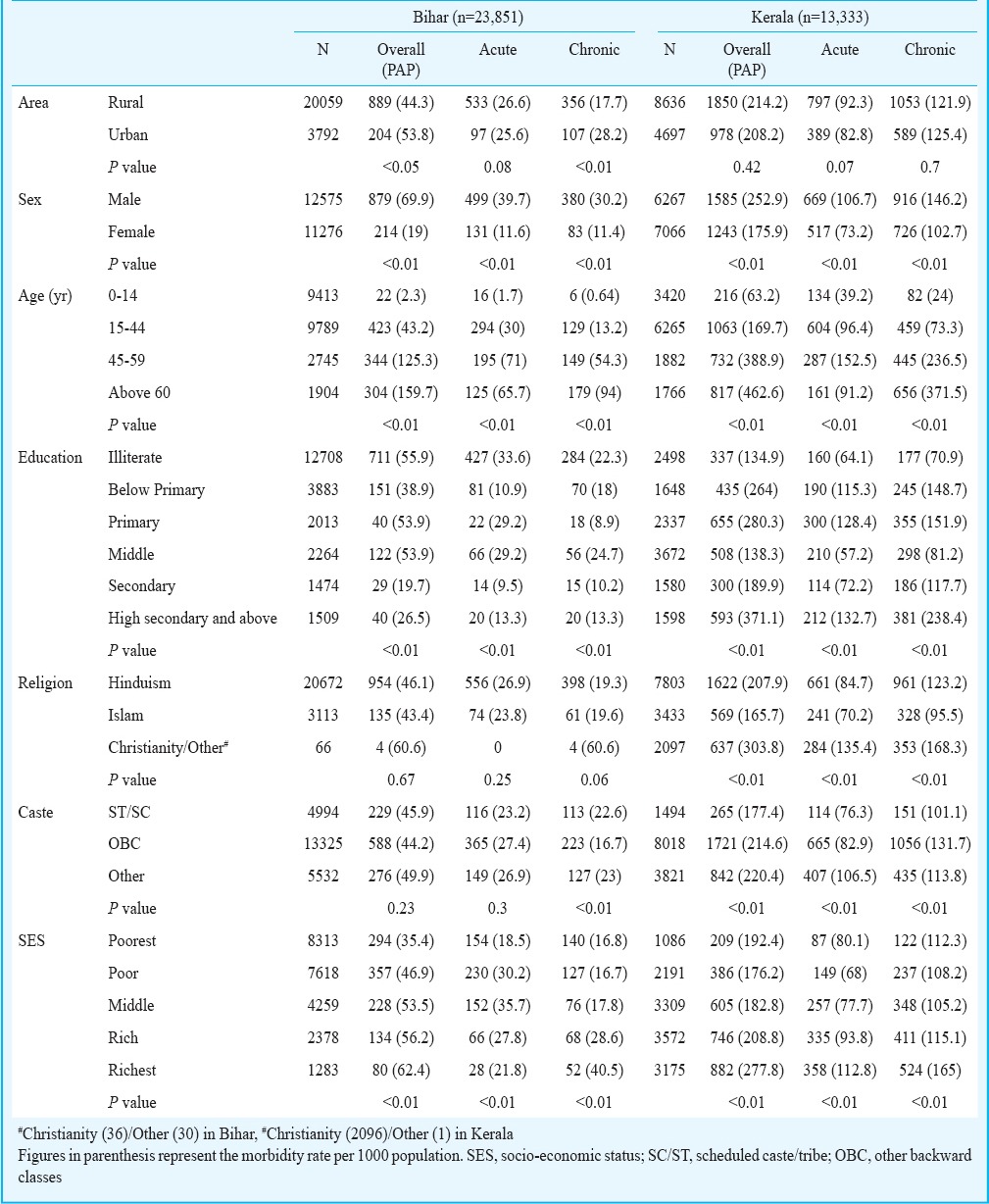
Bivariate analysis: In Bihar, urban residents, males and those aged more than 50 yr had a higher PAP rate. Urban residents in Bihar reported more chronic morbidities (28 per 1000) than acute (26 per 1000) but the difference was not statistically significant. Similarly, people aged more than 50 yr and those with education secondary and above reported more chronic than acute morbidities in Bihar. The overall PAP rate in Kerala was higher among rural respondents, males, those aged more than 44 yr and Christians. Chronic morbidities were uniformly reported more than acute, across areas, sex, religion, caste and educational status. The only exception to the trend was age group between 0 to 44 yr who reported more acute morbidities than chronic (Table I). The PAP per 1000 in Kerala was found to be more than Bihar across all age groups, sex, religions, caste and income quintiles (Table I).
Socio-economic status and self-reported morbidity: Socio-economic status was significantly associated with the reporting of morbidities in both the States. The rate of PAP showed an increasing trend from the poorest to the richest quintiles in both the States. The poorest quintile in Bihar had a PAP rate at 35 per 1000 as against the richest who had a PAP rate of 62 per 1000. In Kerala, the poorest and richest quintile had a PAP rate of 192 per 1000 and 278 per 1000, respectively (Table I). The rising gradient in the odds of self-reported morbidity across increasing socio-economic strata was more pronounced in Bihar as compared to Kerala.
Using multivariable analysis it was found that in Bihar, the richest quintile reported more illnesses (OR=2.52, P<0.01) and a steady increasing gradient was observed in the odds for reporting more illnesses with increasing affluence. The gradient was more pronounced for the chronic diseases (2.7, 1.8-4.0) compared to acute diseases (1.82, 1.15-2.86) (Table II). Similarly in Kerala, the odds of reporting any illness were 1.66 (1.4-2.0) times higher among the richest. Again, the gradient was higher for chronic (OR=1.6, 1.26-2.01) than the acute (OR= 1.41, 1.1-1.82) ailments (Table III).
Table II.
Predictors of self-reported morbidity, total, acute and chronic, in Bihar using hierarchal logistic regression analysis
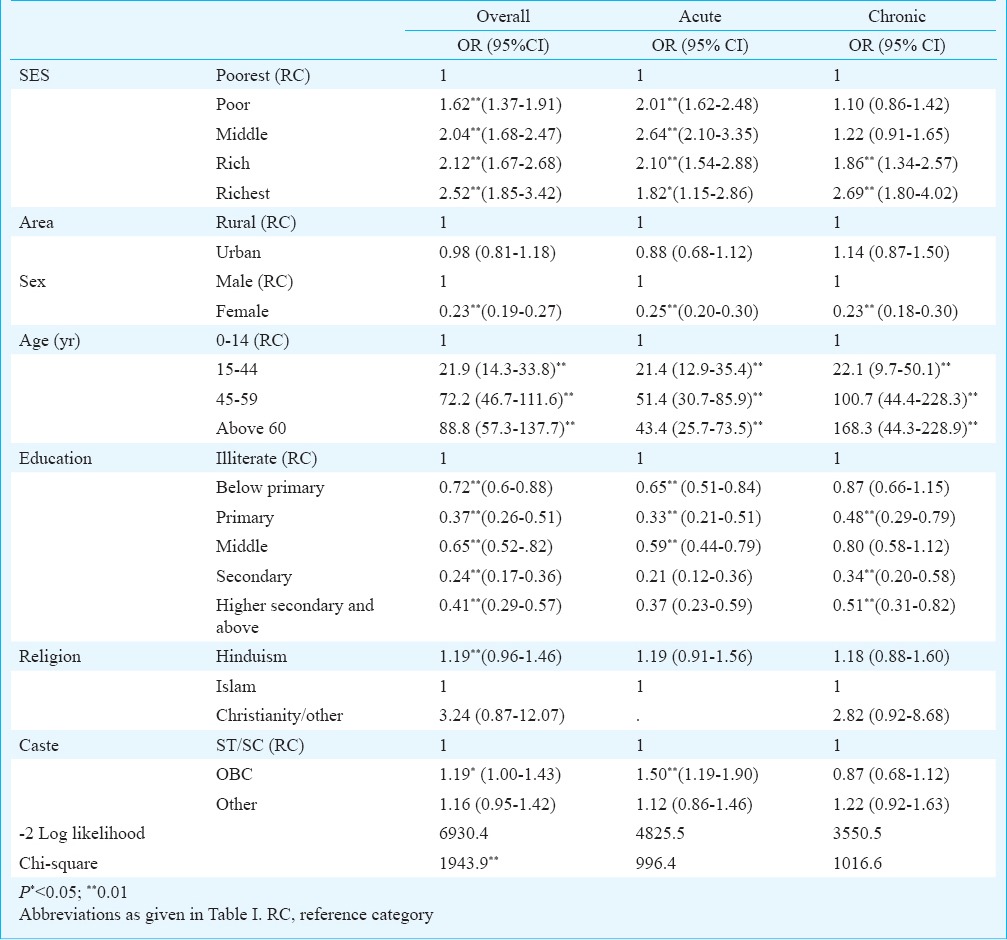
Table III.
Predictors of self reported morbidity, total, acute and chronic, in Kerala using hierarchal logistic regression analysis
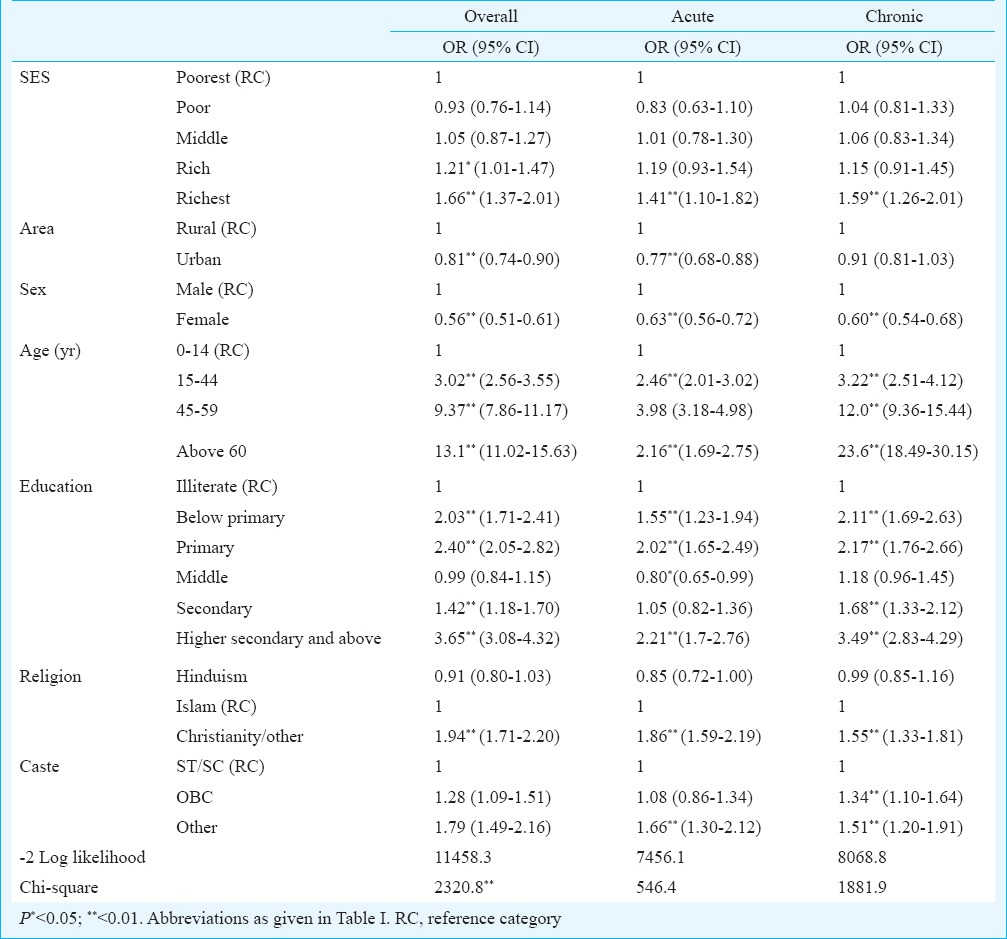
Other socio-demographic factors significantly associated with SRM in Bihar were older age (OR=88.8, P<0.01), being illiterate and being a male (Table II). People belonging to older age groups were reporting significantly more acute and chronic illnesses compared to the younger respondents, though the OR was found to be stronger for chronic illnesses (OR=168.3, P<0.01) compared to that for acute illnesses (OR=43.4, P<0.01) (Table II). In Kerala, in addition to the above mentioned factors for Bihar, hailing from a rural area was also associated with self-reporting of any illness (Table III).
Discussion
Our study was based on the analysis of data on self-reported morbidity from a representative sample of two States of India namely Kerala and Bihar. Overall, it was found that Kerala had higher rates of self-reported ailments, both acute and chronic, as compared to those from Bihar. Kerala and Bihar have been subject to comparison in earlier studies to highlight differences in mortality rates and self-reported morbidities10,11. Kerala is one of the well-performing States in India with good health indicators22. Quite contrarily, Bihar is one of the poor performing States with poor health indicators.
Our findings showed that in Kerala, chronic diseases were more commonly reported than acute while the respondents from Bihar reported significantly more acute illnesses than chronic except those who belonged to the richest quintile, were from urban areas and belonged to age group more than 60 years. This correlates well with what has been studied in terms of objective measures also. For example, the mortality trends of Kerala has been reported to be comparable to that of industrialized nations with a predominance of NCD deaths18. Thus, the State is in a more advanced stage of epidemiologic transition as compared to Bihar. In the initial stages of epidemiological transition, as in Bihar, affluence is associated with higher incidence of NCDs. However, as the transition progresses, as in Kerala, a reversal of social gradient occurs with an increase in incidence of NCDs among poor leading to equalization of rates of NCDs14,23,24. Bhojani et al25 have also stressed that in the initial phase of epidemiologic transition, the affluent are affected more by chronic conditions followed by a reversal of the social gradient in the later stages. A similar idea has been reported by Mohan et al24 who suggest that as the NCD epidemic matures and reaches the next stage of transition, the rich and affluent will rapidly change their activity patterns and start making healthier food choices and ultimately the diabetes and heart disease will decrease in this section of the society. Within the developed world, which has reached later stages of epidemiologic transition, the prevalence of diabetes and cardiovascular diseases are higher among the lower socio-economic group and in rural areas compared to higher socio-economic group and urban areas24. Thus, the differential rates of SRM could be partially attributed to the differential rates of NCDs among the rich and poor. Such a situation is more likely to be exacerbated during the early phases of the transition and could explain the different SRM rates across socio-economic strata.
A person aged more than 60 yr in Kerala was 23.6 times more likely to report a chronic illness as compared to someone aged between 0 to 14 yr, while a person aged more than 60 years in Bihar was 168 times more likely to report a chronic illness as compared to a person aged 0 to 14 yr. This also strengthens our observation that the epidemiologic transition is in its early stages in Bihar facing double burden of infectious and chronic diseases while Kerala might have progressed further ahead in epidemiologic transition with blurring differentials in profile of morbidities across age groups.
The relationship between socio-economic status and SRM has been documented earlier in India in the context of diabetes mellitus where one quintile rise in wealth was associated with an OR of 1.31 for self-reported diabetes26. The richest quintile in Kerala was 1.59 times more likely to report a chronic illness as compared to the poorest, and in Bihar the strength of association was 2.69. This indicates that the rich-poor gap in the burden of disease is more pronounced in Bihar. Safraj et al27 documented that in Kerala, the prevalence of self-reported diabetes mellitus increased as one ascended the socio-economic ladder.
Affluence directly leading to higher incidence28 and hence higher reporting of chronic illness explains only a part of the picture as the rich were found to report more acute illnesses as compared to their poor counterparts. Hence, positional objectivity could be a strong plausible explanation, wherein the rich who have better awareness, accessibility and affordability have a tendency to perceive and report more morbidity than the poor who are grappling with more basic needs to live.
There was a possible bias in the data. Since self-reported morbidity takes a point prevalence measure of morbidity, an incidence prevalence bias (Neyman bias)29 may cause the investigator to miss an acute illness which is either transient or of sinister nature to have caused mortality and thus missed. Hence the chronic diseases are more likely to be captured in a cross-sectional survey due to their prolonged nature. However, since this bias is likely to prevail equally across all socio-economic strata, this does not affect the validity of our observations on wealth related inequalities in SRM. We have not attempted to validate the self-reported morbidity against any objective measure of health status like life expectancy or mortality rates. Further, we have also not accounted for multiple episodes of same illness and multiple illnesses in same person during the reference period.
In conclusion, our analysis showed that the richer Kerala population reported more morbidity than the poorer population in Bihar. Further, it was found that the gradient of rich reporting more was evident within each of the two States. However, the gradient was being influenced by the presence of chronic NCDs. This was more apparent in Bihar being in the early stage of epidemiological transition. As NCDs are chronic diseases, these are likely to be reported in any reference period. Thus in States and countries which are passing through early stages of epidemiological transition wherein the NCDs are more among the rich, this phenomenon also affects the finding of higher self-reported morbidity by the rich. This was an exploratory study which used existing data to test the hypothesis that epidemiologic transition, besides positional objectivity, might contribute in varying proportions to the differences in SRM. However, it did not conclusively prove this hypothesis and would require extrapolation of the study results to other populations.
References
- 1.New Delhi: Registrar General of India 1; 2011. [accessed on January 13, 2014]. Census 2011. Available from: censusindia.gov.in . [Google Scholar]
- 2.Registrar General of India. SRS Bull. 2011;35:1–6. [Google Scholar]
- 3.Victora CG, Barros AJ, Axelson H, Bhutta ZA, Chopra M, Franca GV, et al. How changes in coverage affect equity in maternal and child health interventions in 35 Countdown to 2015 countries: an analysis of national surveys. Lancet. 2012;380:1149–56. doi: 10.1016/S0140-6736(12)61427-5. [DOI] [PubMed] [Google Scholar]
- 4.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 5.Sen A. Why health equity? Health econ 2002. 11:659–66. doi: 10.1002/hec.762. [DOI] [PubMed] [Google Scholar]
- 6.National Family Health Survey (NFHS-3), 2005-06. India. Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro international. [Google Scholar]
- 7.New Delhi: National Sample Survey Organisation, Ministry of Statistics and Programme Implementation, Government of India; 2006. Mar, Morbidity, health care and the condition of the aged. Report No.: 507 (60/25.0/1) [Google Scholar]
- 8.Mumbai: International Institute for Population Sciences, Ministry of Health and Family Welfare, Government of India; 2010. Apr, District Level Household and Facility Survey (DLHS-3) 2007-08. [Google Scholar]
- 9.Bago d’Uva T, Van Doorslaer E, Lindeboom M, O’Donnell O. Does reporting heterogeneity bias the measurement of health disparities? Health econ. 2008;17:351–75. doi: 10.1002/hec.1269. [DOI] [PubMed] [Google Scholar]
- 10.Sen A. Health: perception versus observation: self reported morbidity has severe limitations and can be extremely misleading. BMJ. 2002;324:860–1. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Subramanian SV, Subramanyam MA, Selvaraj S, Kawachi I. Are self-reports of health and morbidities in developing countries misleading? Evidence from India. Soc Sci Med. 2009;68:260–5. doi: 10.1016/j.socscimed.2008.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sen A. Positional objectivity. Philos public aff. 1993;22:126–45. [Google Scholar]
- 13.Prinja S, Jeet G, Kumar R. Validity of self-reported morbidity. Indian J Med Res. 2012;136:722–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Srinath Reddy K, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 15.New Delhi: MOSPI; 2004. India National Sample Survey Office, Ministry of Statistics and Programme Implementaion (MOSPI), Government of India. Survey on Morbidity and Health Care, NSS 60th Round: January 2004-June 2004. [Google Scholar]
- 16.Thankappan K, Shah B, Mathur P, Sarma P, Srinivas G, Mini GK, et al. Risk factor profile for chronic non-communicable diseases: results of a community-based study in Kerala, India. Indian J Med Res. 2010;131:53–63. [PubMed] [Google Scholar]
- 17.Sivasankaran S, Thankappan KR. Prevention of noncommunicable diseases requires a life course approach: a case study from Kerala. Indian j med res. 2013;137:874–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Soman CR, Kutty VR, Safraj S, Vijayakumar K, Rajamohanan K, Ajayan K. Profile Study Group. All-cause mortality and cardiovascular mortality in Kerala State of India: Results from a 5-year follow-up of 161,942 rural community dwelling adults. Asia Pac J Public Health. 2011;23:896–903. doi: 10.1177/1010539510365100. [DOI] [PubMed] [Google Scholar]
- 19.Mohan S, Reddy KS. Health transition and the rising threat of chronic non-communicable diseases in India. In: Lewis MJ, MacPherson KL, editors. Health transitions and the double disease burden in Asia and the Pacific: Histories of responses to non-communicable and communicable diseases. Oxon, UK: Routledge; 2012. p. 76. [Google Scholar]
- 20.Subramanian SV, Ackerson LK, Subramanyam MA, Sivaramakrishnan K. Health inequalities in India: The Axes of stratification. Brown J World Aff. 2008;14:127–39. [Google Scholar]
- 21.Arokiasamy P, Jain K, Goli S, Pradhan J. Health inequalities among urban children in India: a comparative assessment of Empowered Action Group (EAG) and south Indian states. J biosoc sci. 2013;45:167–85. doi: 10.1017/S0021932012000211. [DOI] [PubMed] [Google Scholar]
- 22.Family Welfare Statistics in India 2011. New Delhi: Statistics Division, Ministry of Health and Family Welfare, Government of India [Google Scholar]
- 23.Kar S, Thakur JS, Virdi NK, Jain S, Kumar R. Risk factors for cardiovascular diseases: is the social gradient reversing in northern India. Natl Med J India. 2010;23:206–9. [PubMed] [Google Scholar]
- 24.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian j med res. 2007;125:217–30. [PubMed] [Google Scholar]
- 25.Bhojani U, Beerenahalli TS, Devadasan R, Munegowda CM, Devadasan N, Criel B, et al. No longer diseases of the wealthy: prevalence and health-seeking for self-reported chronic conditions among urban poor in Southern India. BMC health serv res. 2013;13:306. doi: 10.1186/1472-6963-13-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corsi DJ, Subramanian SV. Association between socioeconomic status and self-reported diabetes in India: a cross-sectional multilevel analysis. BMJ Open. 2012;2:e000895. doi: 10.1136/bmjopen-2012-000895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Safraj S, Anish T, Vijayakumar K, Kutty VR, Soman CR. Socioeconomic position and prevalence of self-reported diabetes in rural Kerala, India: Results from the PROLIFE study. Asia Pac J Public Health. 2012;24:480–6. doi: 10.1177/1010539510387822. [DOI] [PubMed] [Google Scholar]
- 28.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–53. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 29.Sackett DL. Bias in analytic research. J chronic dis. 1979;32:51–63. doi: 10.1016/0021-9681(79)90012-2. [DOI] [PubMed] [Google Scholar]


