Abstract
It is believed that the tribal people, who constitute 8.6 per cent of the total population (2011 census of India), are the original inhabitants of India. Glucose-6-phosphate-dehydrogenase (G6PD) deficiency is an X-linked genetic defect, affecting around 400 million people worldwide and is characterized by considerable biochemical and molecular heterogeneity. Deficiency of this enzyme is highly polymorphic in those areas where malaria is/has been endemic. G6PD deficiency was reported from India more than 50 years ago. The prevalence varies from 2.3 to 27.0 per cent with an overall prevalence of 7.7 per cent in different tribal groups. Since the tribal populations live in remote areas where malaria is/has been endemic, irrational use of antimalarial drugs could result in an increased number of cases with drug induced haemolysis. Therefore, before giving antimalarial therapy, routine screening for G6PD deficiency should be undertaken in those tribal communities where its prevalence is high.
Keywords: Deficiency, G6PD, malaria, tribes, variant
Introduction
Glucose is the main source of energy for the red cell, which is metabolized by two major routes; the glycolytic pathway and the hexose monophosphate (HMP) shunt. Glucose-6-phosphate-dehydrogenase (G6PD) is an X-linked enzyme that catalyses the first step in the HMP pathway of glucose metabolism and it produces NADPH, which is required for the maintenance of reduced glutathione (GSH). GSH is essential for protecting red cells from oxidative damage1. Hence, this enzyme is important in red cell metabolism and its deficiency renders the red cell extremely vulnerable to any kind of oxidative stress. The major clinical manifestations of this disorder are drug induced haemolytic anaemia and/or neonatal jaundice and a small proportion of G6PD deficient individuals have chronic non-spherocytic haemolytic anaemia (Class I G6PD deficiency)2.
G6PD deficiency is an example of balanced polymorphism, in which high rate of mortality caused by this disorder is offset by the protection that it offers against Plasmodium falciparum malaria3. Alleles of the G6PD gene that encode a deficient enzyme attain high frequencies in areas where malaria is or has been endemic4. It is believed that this disorder is selected due to malarial endemicity in many regions of the country. A correlation was found between high prevalence of malaria due to P. falciparum and incidence of G6PD deficiency5.
G6PD deficiency is very common among humans, affecting around 400 million people worldwide and is characterized by considerable biochemical and molecular heterogeneity6. A higher incidence of G6PD deficiency is seen in tropical and subtropical zones of the world. Molecular analysis has revealed that each population has a characteristic profile of deficient variants. The G6PD A- variant is mainly found in African populations while G6PD Mediterranean variant is predominant throughout the Mediterranean region, Middle East and India2.
Tribes of India
The most remarkable feature of the Indian population structure is the clear division of its population into strictly defined endogamous castes, tribes and religious groups. India has the largest concentration of the tribal population in the world. It is generally believed that the tribal people, who constitute 8.6 per cent of the total population (2011 census of India)7, are the original inhabitants of India and are generally called “Adivasis”. The tribals can be classified according to their ethnic origin, language, race, socio-economy and cultural pattern. The total number of tribal groups is estimated to be 461 who speak about 750 dialects that belong to one of the four language groups, Austro-Asiatic, Indo-Europeans, Dravidian and Tibeto-Burman8,9. The tribals are found in all the states except in Punjab, Haryana, and Jammu & Kashmir.
Majority of the tribal people live below the poverty line. They generally reside in isolated hilly and forest areas and are not accessible at most of the times during the year. There is a consensus agreement that the health status of tribal populations is very poor and is even worse among the primitive tribes because of their isolation as a consequence of their residing in remote areas and thus being largely unaffected by the developmental processes going on in the country.
Geographical distribution of G6PD deficiency among the tribes
Data reported herein have been collected from various field surveys by different workers. Considerable differences were seen in the methods adopted for field surveys and also the mode of collection of blood samples for screening for G6PD deficiency. Frequencies of the Gd- (G6PD deficient) gene are recorded as have been reported in various studies, however, studies where the sample size was small have not been considered.
A total of 72 tribal groups from 56 districts of 16 states and two Union Territories of India were studied. The Figure shows the districts wise distribution of G6PD deficiency among the tribal groups in different States of India. The prevalence of G6PD deficiency varied from 2.3 to 27.0 per cent with an overall prevalence of 7.7 per cent. The frequencies of the Gd- gene in different states of India showed a heterogeneous picture. Comparatively a higher frequency (>10%) of the Gd- gene is observed among the tribal groups of Nagaland, Chhattisgarh, West Bengal, Dadra & Nagar Haveli and Gujarat. On the other hand, uniformly low frequencies (<5%) of Gd- gene have been reported in Tripura followed by Himachal Pradesh, Uttarakhand, Andhra Pradesh and Madhya Pradesh. Gene frequency data of G6PD deficiency in various regions are summarized below:
Fig.
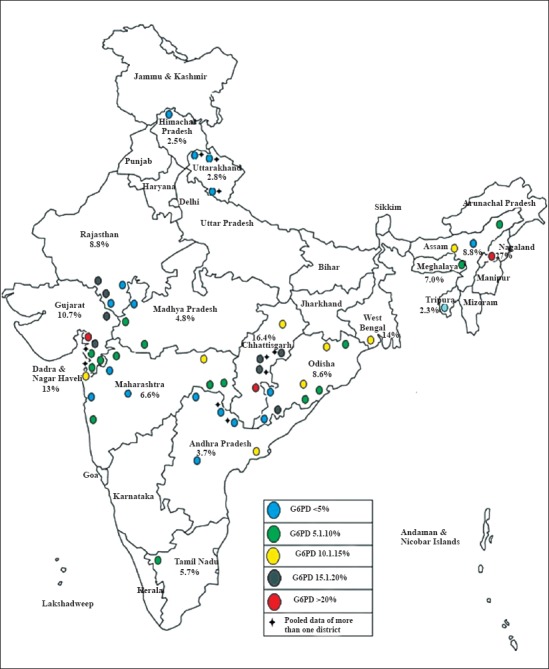
District-wise distribution of G6PD deficiency among the tribal groups in different States of India.
Western India: Comparatively large data have accumulated in western India comprising of Rajasthan, Gujarat, Dadra & Nagar Haveli and Maharashtra10,11,12,13,14,15. A total of 22 tribal groups were studied and the prevalence varied from 1.4 to 31.4 per cent. It is apparent that considerable heterogeneity in G6PD deficiency exists in this region. Among the tribal groups studied, a very high frequency of G6PD deficiency was observed in the Gamits (31.4%), Dhankas (20.4%), Warlis (19.6%), Dhodias (17.8%), Bhils (16.3%) and Garasiyas (15.2%). Bhils from Nasik district of Maharashtra have a very low frequency (1.4%). A complete absence of Gd- gene was observed among the Mahadev Kolis from Ahmednagar district of Maharashtra.
Central India: Central India comprises Madhya Pradesh and Chattisgarh state, and Gonds and Bhils are the major tribal groups. Among Gonds, the prevalence of G6PD deficiency varies from 13.0 to 21.3 per cent10,16,17 while in the Bhils the prevalence varies from 3.4 to 6.7 per cent10,17. A high frequency of G6PD deficiency is observed in Kawars (21.5%) and Oraons (13.4%)17.
Southern India: In 1964, Meera Khan reported a high incidence of G6PD deficiency in the Koya Dora tribal groups of Andhra Pradesh18. Subsequent studies10 in other tribal groups of Andhra Pradesh exhibited frequencies of 0 to 6.1 per cent. In Tamil Nadu, tribal groups of Nilgiri hills were studied and the prevalence varied from 0 to 10.6 per cent10,15. In Kerala, only Kadar tribal group has been studied and none of the individuals showed the presence of G6PD deficiency10.
Eastern India: In West Bengal, Santals from Midnapur district showed a high prevalence of G6PD deficiency10. In Odisha, the prevalence of G6PD deficiency varied from 1.3 to 17.4 per cent10,15,19,20. A very high frequency has been observed in the Parajas (17.4%), Juangas (15.6%), Kondhas (12.5%), Bhumizs (12.2%) and Kolhas (10.7%)15,20 while the lowest frequency is found among the Bondos from Malkangiri district15.
North India: Data from North India were uniformly low and the prevalence varied from 1.2 to 4.4 per cent10.
North-East India: G6PD deficiency was present in all the tribal groups studied from North-East India. A very high frequency was observed in Angami Nagas (27.0%) from Nagaland followed by Rabhas (15.8%) and Mikirs (15.6%) from Assam10.
Andaman & Nicobar Islands: A total of 29 Great Andamanese individuals, a primitive Negrito tribe of the Andaman and Nicobar Islands, India, with a total population of 37 were studied and one female was found to be G6PD deficient21.
Laboratory investigations
The diagnosis of red cell enzyme deficiency usually depends on the demonstration of decreased enzyme activity either through a quantitative assay or a screening test. There are several methods available for the diagnosis of G6PD deficiency. However, fluorescent spot test and dichlorophenol indophenol (DPIP) decolourisation method were found to be useful and suitable for routine use. The fluorescent spot test is based on the fluorescence of NADPH which has been generated by G6PD while in the DPIP dye decolourisation method; presence of G6PD in red cells is detected by the decolourisation of the dye within a specified time. It has an advantage over fluorescent spot test in that the heterozygotes can be easily detected and a large number of samples can be processed together at the same time. It is the method of choice along with quantitation of enzyme while screening large population22. Quantitation of enzyme activity involves the measurement of reduction of NADP to NADPH spectrophotometrically in the presence of G6P and haemolysate.
Molecular pathology of G6PD deficiency
In India, the spectrum of mutations causing G6PD deficiency has not been well elucidated. However, earlier studies have revealed that the G6PD Mediterranean mutation (563C→T) is the most common deficient variant followed by G6PD Kerala-Kalyan (949G→A) and G6PD Odisha (131C→G)22. G6PD Mediterranean was found to have significantly lower red cell enzyme activity and more severe clinical manifestations than the other two22. Of the three common mutations, G6PD Odisha and G6PD Mediterranean were found to be the main mutational event causing G6PD deficiency among the tribal groups of Maharashtra, Odisha and Gujarat23,24,25,26 while G6PD Namoru (208 T→C) was exclusively found among the Dravidian speaking tribes of Nilgiri district, Tamil Nadu, which further supported the human migration from Africa to Australia along the coast of southern India27. Besides these mutations, G6PD Chatam, G6PD Coimbra, G6PD Nilgiri, and G6PD Gond have also been reported in the Indian tribal populations25,28,29.
Alleles of the G6PD gene that encode a deficient enzyme attain high frequencies in areas where malaria is or has been endemic. Decreased parasitaemia has been observed among the patients with G6PD deficiency and the malarial parasite also does not grow well in G6PD deficient red cells as compared to normal cells30. In India, it is believed that this disorder is selected due to malarial endemicity in many regions of the country5. A wide variability in the prevalence of G6PD deficiency has been observed in the tribal population groups even within small geographical areas, as the design of these studies and the methodology used have not been uniform. At the same time, the clinical manifestations of these deficient cases are not well documented. Based on the epidemiological studies, it has been estimated that more than four million male tribal individuals are G6PD deficient and, therefore, the irrational use of antimalarial drugs causes concern in the medical fraternity about the occurrence of haemolysis in these individuals. Most of the individuals are underdiagnosed due to lack of awareness and testing facilities.
Our earlier study suggested that the use of antimalarial drugs could result in an increase in the number of cases with drug induced haemolysis. Ciprofloxacin alone also caused haemolytic anaemia31. This is a burden on the National Health Programme and highlights the need to undertake systematic studies on G6PD deficiency in the Indian tribal population. There is a consensus agreement that the health status of tribal populations is very poor and is even worse among the primitive tribes because of their isolation as they reside in remote areas where malaria is or has been endemic. Therefore, it is recommended that the vulnerable tribal communities should be screened before administering the oxidative drugs. In the tribal areas, the medical officer of the primary health centres should be made aware of this fact so that the oxidant drugs are prescribed with caution.
References
- 1.Beutler E. G6PD deficiency. Blood. 1994;84:3613–36. [PubMed] [Google Scholar]
- 2.Beutler E. G6PD: Population genetics and clinical manifestations. Blood Rev. 1996;10:45–52. doi: 10.1016/s0268-960x(96)90019-3. [DOI] [PubMed] [Google Scholar]
- 3.Luzzatto L, Bienzle U. The malaria/G-6-P.D. hypothesis. Lancet. 1979;1:1183–4. doi: 10.1016/s0140-6736(79)91857-9. [DOI] [PubMed] [Google Scholar]
- 4.Nagel RL, Roth EF., Jr Malaria and red cell genetic defects. Blood. 1989;74:1213–21. [PubMed] [Google Scholar]
- 5.Mohanty D, Sukumar S, Mukherjee MB, Colah RB. G6PD deficiency and malaria in India. Am J Hematol. 2003;72:150–1. doi: 10.1002/ajh.10276. [DOI] [PubMed] [Google Scholar]
- 6.Luzzatto L, Mehta A. Glucose-6-phosphate-dehydrogenase deficiency. In: Scriver CR, Beaudet AL, Sly WS, Valle D, editors. The metabolic basis of inherited disease. 5th ed. New York: McGraw Hill; 1995. pp. 2237–65. [Google Scholar]
- 7.Census of India 2011, Office of the Registrar General and Census Commissioner. Ministry of Home Affairs, Govt of India. [accessed on March 27, 2015]. Available from: http://www.censusindia.gov.in .
- 8.Kosambi DD. New Delhi: Vikas Publishing House; 1991. The culture and civilisation of ancient India in historical outline. [Google Scholar]
- 9.Singh KS. Calcutta, India: Anthropological Survey of India; 1992. People of India: an introduction. [Google Scholar]
- 10.Bhatia HM, Rao VR, editors. Bombay: Institute of Immunohaematology (ICMR); 1987. Genetic atlas of the Indian tribes. [Google Scholar]
- 11.Rao VR, Gorakshakar AC. Sickle cell hemoglobin, β- thalassemia and G6PD deficiency in tribes of Maharashtra, India. Gene Geogr. 1990;4:131–4. [PubMed] [Google Scholar]
- 12.Mukherjee MB, Gangakhedkar RR, Sathe MS. Abnormal haemoglobin, G6PD deficiency and their pattern of interaction in the tribal population of Valsad district (Gujarat) Indian J Hematol Blood Transf. 1993;11:227–31. [Google Scholar]
- 13.Jain RC, Mehta J, Mehta NL, Joshi KC, Gupta OP, Andrew AM. Sickle cell trait, thalassaemia and glucose-6-phosphate dehydrogenase deficiency in the Bhil tribe of Southern Rajasthan. Indian J Med Res. 1981;73:548–53. [PubMed] [Google Scholar]
- 14.Choubisa SL. Sickle cell haemoglobin, thalassaemia and G-6-PD enzyme deficiency genes in Garasiya tribe inhabited malaria endemic areas of Sirohi district, Rajasthan (India) J Commun Dis. 2009;41:13–8. [PubMed] [Google Scholar]
- 15.New Delhi: Indian Council of Medical Research; 2010. Report of the ICMR Multicentric Task Force on Intervention programme for nutritional anemia and haemoglobinopathies amongst some primitive tribal populations of India. [Google Scholar]
- 16.Thakur A, Verma IC. Interaction of malarial infection and glucose-6-phosphate dehydrogenase deficiency in Muria Gonds of district Bastar, central India. Trop Geogr Med. 1992;44:201–5. [PubMed] [Google Scholar]
- 17.Sathe M, Gorakshakar AC, Rao VR, Mukherjee M, Vasantha K, Bhatia HM. Red cell genetic abnormalities in the tribes of five districts of Madhya Pradesh. Indian J Med Res. 1987;86:808–11. [PubMed] [Google Scholar]
- 18.Meera Khan P. Glucose-6-phosphate dehyrogenase deficiency in rural India. J Genet. 1964;59:14–8. [Google Scholar]
- 19.Balgir RS. Community expansion and gene geography of sickle cell trait and G6PD deficiency, and natural selection against malaria: experience from tribal land of India. Cardiovasc Hematol Agents Med c. 2012;10:3–13. doi: 10.2174/187152512799201190. [DOI] [PubMed] [Google Scholar]
- 20.Chhotray GP, Ranjit MR. Prevalence of G-6-PD deficiency in a malarial endemic tribal area of Orissa (India) Indian J Med Res. 1990;92:443–6. [PubMed] [Google Scholar]
- 21.Murhekar KM, Murhekar MV, Mukherjee MB, Gorakshakar AC, Surve R, Wadia M, et al. Red cell genetic abnormalities, β-globin gene haplotypes and APOB polymorphism in the Great Andamanese, a primitive Negrito Tribe of Andaman and Nicobar Islands, India. Hum Biol. 2001;73:739–44. doi: 10.1353/hub.2001.0070. [DOI] [PubMed] [Google Scholar]
- 22.Mohanty D, Mukherjee MB, Colah RB. Glucose-6-phosphate-dehydrogenase deficiency in India. Indian J Pediatr. 2004;71:525–9. doi: 10.1007/BF02724295. [DOI] [PubMed] [Google Scholar]
- 23.Kaeda JS, Chhotray GP, Ranjit MR, Bautista JM, Reddy PH, Stevens J, et al. A new glucose-6-phosphate dehydrogenase variant G6PD Orissa (44 Ala→Gly) is the major polymorphic variant in tribal populations in India. Am J Hum Genet. 1995;57:1335–41. [PMC free article] [PubMed] [Google Scholar]
- 24.Sukumar S, Mukherjee MB, Colah RB, Mohanty D. Molecular basis of G6PD deficiency in India. Blood Cells Mol Dis. 2004;33:141–5. doi: 10.1016/j.bcmd.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Chalvam R, Colah RB, Mohanty D, Ghosh K, Mukherjee MB. Molecular heterogeneity of glucose-6-phosphate dehydrogenase deficiency among the tribals in western India. Blood Cells Mol Dis. 2009;43:156–7. doi: 10.1016/j.bcmd.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Nishank SS, Chhotray GP, Kar SK, Ranjit MR. Molecular variants of G6PD deficiency among certain tribal communities of Orissa, India. Ann Hum Biol. 2008;35:355–61. doi: 10.1080/03014460801961289. [DOI] [PubMed] [Google Scholar]
- 27.Chalvam R, Mukherjee MB, Colah RB, Mohanty D, Ghosh K. G6PD Namoru (208T→C) is the major polymorphic variant in the tribal populations in southern India. Br J Haematol. 2007;136:512–3. doi: 10.1111/j.1365-2141.2006.06463.x. [DOI] [PubMed] [Google Scholar]
- 28.Chalvam R, Kedar PS, Colah RB, Ghosh K, Mukherjee MB. A novel R198H mutation in the glucose-6-phosphate dehydrogenase gene in the tribal groups of the Nilgiris in Southern India. J Hum Genet. 2008;53:181–4. doi: 10.1007/s10038-007-0225-3. [DOI] [PubMed] [Google Scholar]
- 29.Sarkar S, Biswas NK, Dey B, Mukhopadhyay D, Majumder PP. A large, systematic molecular-genetic study of G6PD in Indian populations identifies a new non-synonymous variant and supports recent positive selection. Infect Genet Evol. 2010;10:1228–36. doi: 10.1016/j.meegid.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Roth J, Jr, Schulman S. The adaptation of plasmodium falciparum to oxidative stress in G6PD deficient human erythrocytes. Br J Haematol. 1988;70:363–7. doi: 10.1111/j.1365-2141.1988.tb02495.x. [DOI] [PubMed] [Google Scholar]
- 31.Sukumar S, Colah R, Mohanty D. G6PD gene mutations in India producing drug-induced haemolytic anaemia. Br J Haematol. 2002;116:671–2. doi: 10.1046/j.0007-1048.2001.03328.x. [DOI] [PubMed] [Google Scholar]


