Abstract
Background & objectives:
Malaria is a major public health problem in many States of the country, particularly, in Madhya Pradesh where both Plasmodium vivax and P. falciparum are endemic. Although many studies have been conducted to investigate risk factors for malaria, but only a few have examined household and socio-economic risk factors. The present study was, therefore, undertaken to explore the relationship of different socio-demographic, socio-economic and behavioural risk factors with malaria prevalence in tribal areas of Madhya Pradesh, India.
Methods:
This study was undertaken in all 62 villages of Bargi Primary Health Centre from May 2005 to June 2008. These villages comprised 7117 households with an average family size of five members. Fortnightly fever surveys were conducted in all villages to assess prevalence of malaria infection in the community. The distinct univariate and multivariate logistic regression models were fitted on the data set.
Results:
The important socio-demographic risk factors like age of household head, social group, occupation and family size; socio-economic factors like type of walls of house, place of drinking water source, irrigated land, cash crop; and behavioural variables like place of sleeping, use of bed nets, etc. were found significantly associated with malaria in univariate analyses. In multivariate analyses only social groups, family size, type of walls of house, and place of sleeping had strong significant association with prevalence of malaria.
Interpretation & conclusions:
The study shows that in tribal areas where people are living in poor quality of houses with no proper use of preventive measures, malaria is firmly established. We conclude that community based interventions which bring improvement in standard of living, access to healthcare facilities and health awareness, will have a significant impact on malaria prevention in these areas.
Keywords: Central India, Madhya Pradesh, Malaria, Plasmodium falciparum, poverty, risk factors of malaria, tribal area
Malaria is a major public health problem in African countries and South East Asia Region (SEAR) countries1. Malaria epidemiology and its control are complicated by poverty as it is a dominant disease in poverty stricken societies2. In India, two-third of all malaria cases are reported from six states - Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh (MP), West Bengal and the states in North East3. Predominantly, these are the states having large populations of ethnic tribes where malaria is an enormous health and development problem and all five species of malaria are found4,5.
Malaria in MP is caused by Plasmodium vivax and P.falciparum and these parasites are highly seasonal in their distribution, P.vivax during summer and monsoon and P. falciparum during post-monsoon and autumn. P. malariae is also found occasionally6. Peoples from all age groups are affected by both the parasites7. Malaria in most parts of MP is mainly transmitted by two efficient vectors, viz. Anopheles culicifacies and An.fluviatilis7,8. Malaria control is mainly based on two tools, i.e. vector control by indoor residual spray, two rounds of DDT /synthetic pyrethroids annually along with insecticide treated bed nets (ITNs) or long lasting insecticide treated nets (LLINs) and chemotherapy using chloroquine (CQ) /artemisinin based combination therapy (ACT) for treatment of malaria cases9. One of the difficulties associated with achieving a reduction in the malaria incidence is that a combination of many diverse factors contributes to the maintenance of its transmission compounded by socio-demographic and socio-economic factors relating to malaria. Housing condition and environmental factors significantly contribute to the variations in malaria incidence. In Sri Lanka10 a strong association was found between malaria incidence and the type of housing construction. Similarly, in Ethiopia household factors such as earth, roof, sharing the house with livestock, presence of windows and open eaves were significantly associated with malaria incidence11.
Many studies have been conducted to investigate risk factors of malaria10,11,12,13,14, however, very few have examined household and socio-economic factors affecting malaria incidence particularly in India15. Therefore, the present study was undertaken in certain tribal areas of Jabalpur, MP, India, to assess the socio-demographic, socio-economic and household behavioural factors that play a role in malaria incidence in rural and tribal settings.
Material & Methods
Study area and population: This study was a part of a large research project on preparation of a field site for malaria vaccine trial in and around Jabalpur and the study site was Bargi Primary Health Centre (PHC) of Jabalpur district, MP. The study area is a region of hills, hillocks and valleys with thick dense forest. Most of the tribal villages are formed of three to eight hamlets and lies in undulating terrain with patches of forest. The villages are thinly populated with scattered housing divided in geographically discrete hamlets. Most of the villages are encircled by a perennial stream which provides numerous breeding sites for mosquitoes throughout the year. Communication is very poor and it is very difficult to reach a village during rainy season. Houses are small, made of mud, thatch and bamboo with low doors and windows. Very few houses are cemented or walls made up of bricks. Often domestic animals are sheltered in the house.
The inhabitants are mostly illiterate, scantily clothed and work mainly in forest nurseries or on road construction and maintenance. Employment opportunities are very limited. The local economy is agriculture based, with the villagers subsisting on the products of primitive agriculture. The ethnic tribes spend most of their time outside the dwellings and sleep on the floor of the verandah or out-of-doors. Medical facilities are poorly existent and mostly non-functional. Use of bed nets is not very common.
All 62 villages of Bargi PHC were covered in the study and these villages comprised 7117 households with an average family size of five members. The ethnic tribe ‘Gond’ lives with other economically backward social groups in this area.
Study design: The baseline household census was carried out during May to December 2005 in Bargi PHC to establish study by collecting socio-economic and demographic information of all individuals in the study area. The study had two major components, viz. targeted population and community based fever surveys. Study included all pregnant women, their husbands, infant and siblings and they were followed on monthly basis with or without fever for three years or till woman became pregnant for next time or withdrew from the study. These targeted groups were encouraged to report any occurrence of fever, or symptoms of fever and blood smears were taken. Fortnightly fever surveys were conducted in all villages to assess the prevalence of malaria infections in the community. Quality assurance was maintained by conducting re-interview of five per cent randomly selected households. The fever surveys were conducted upto June 2008.
Blood samples collected from all febrile cases either in fever surveys or in enrolled subjects (study cohort) were included in this study. These samples were examined on the same day for malaria parasites in laboratories at National Institute for Research in Tribal Health (NIRTH), Jabalpur.
Data analysis: Locally designed software was used for data entry. The software was developed based on the MS-SQL 2000, following data collection and entry guidelines of Household Registration System Software, (Population Council Inc., NY, USA). Later, the data were transferred to SPSS-20.0 statistical software package (SPSS, Chicago, USA). The logistic regression technique was used and P<0.05 was considered significant. Unadjusted (univariate) and adjusted (multivariate) odds ratios with their 95% confidence intervals (CI) were calculated to determine the relationship of socio-demographic and socio-economic variables with the malaria prevalence.
The socio-demographic, socio-economic and behavioural risk factors of malaria were divided in three broad groups, viz. characteristics of head of household (age, education occupation of head of households, social group to which family belongs and family size), housing characteristics (type of house construction, sources of drinking water and cooking fuel, agricultural land and asset index) and behavioural factors (mixed dwelling i.e. co-residence with animals, sleeping habit of household members, and preventive measures for mosquito biting). Univariate analysis of all categorical and binary factors yields unadjusted OR and 95 % CI. Multivariate analyses for variables significant in univariate analysis were performed by using unconditional logistic regression for all set of variables independently. finally, a logistic regression with backward elimination method was performed to construct a model that included all significant factors that remained significant in presence of other significant factors. For all types of analyses unit of analysis was household.
The study was approved by the Institute Ethical Committees (IEC) of National Institute of Malaria Research (NIMR), New Delhi; NIRTH, Jabalpur and Centers for Disease Control and Prevention (CDC), Atlanta (Partners for large research project). Before taking blood samples a written consent was obtained from all adults and from parents/guardians in case of children. All fever cases were given presumptive treatment and all subjects found positive for malaria were treated as per guidelines of National Vector Borne Disease Control Programme (NVBDCP) within 24 h9.
Results
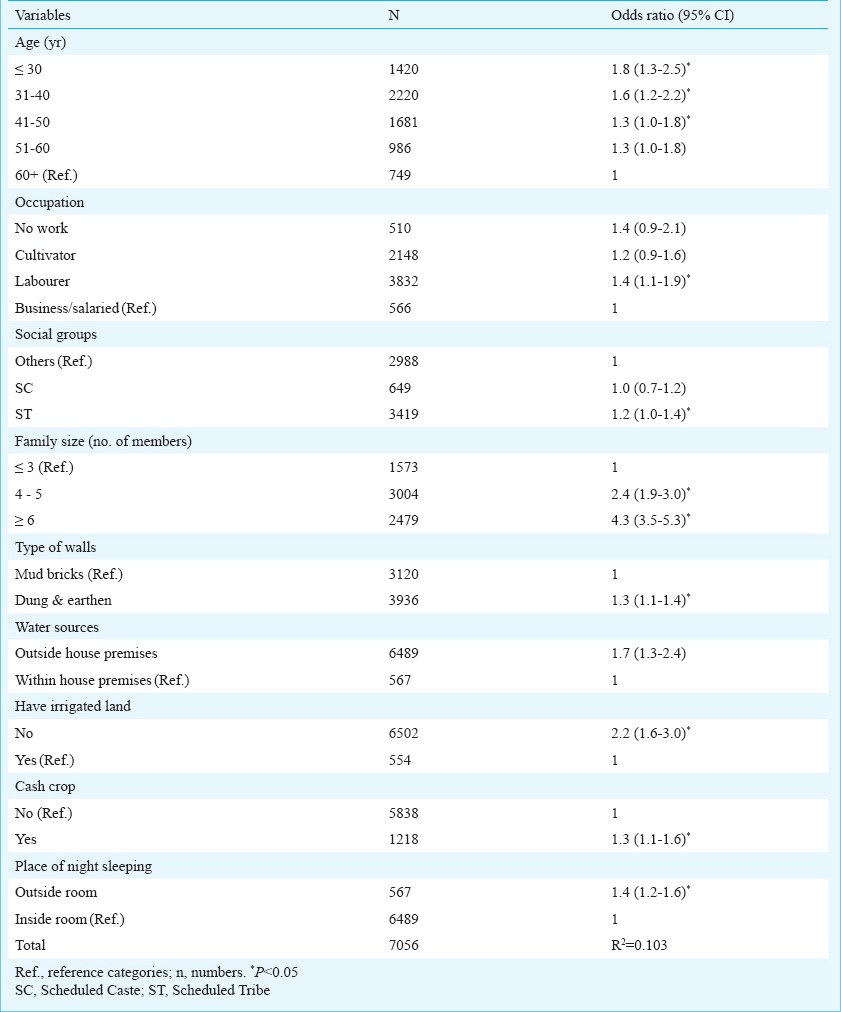
To assess the impact of various socio-demographic and socio-economic variables on malaria different models were tried. In the first model association of various characteristics of household heads with malaria (Table I) was examined. In the second model, the association of housing characteristics (Table II) and in the third model association of some behaviour variables (Table III) with malaria were examined. Finally, a model (Table IV) including all significant variables of the first three models was fitted using logistic regression with backward elimination method.
Table 1.
Some characteristics of head of household and their association with malaria (May 2005 to June 2008)
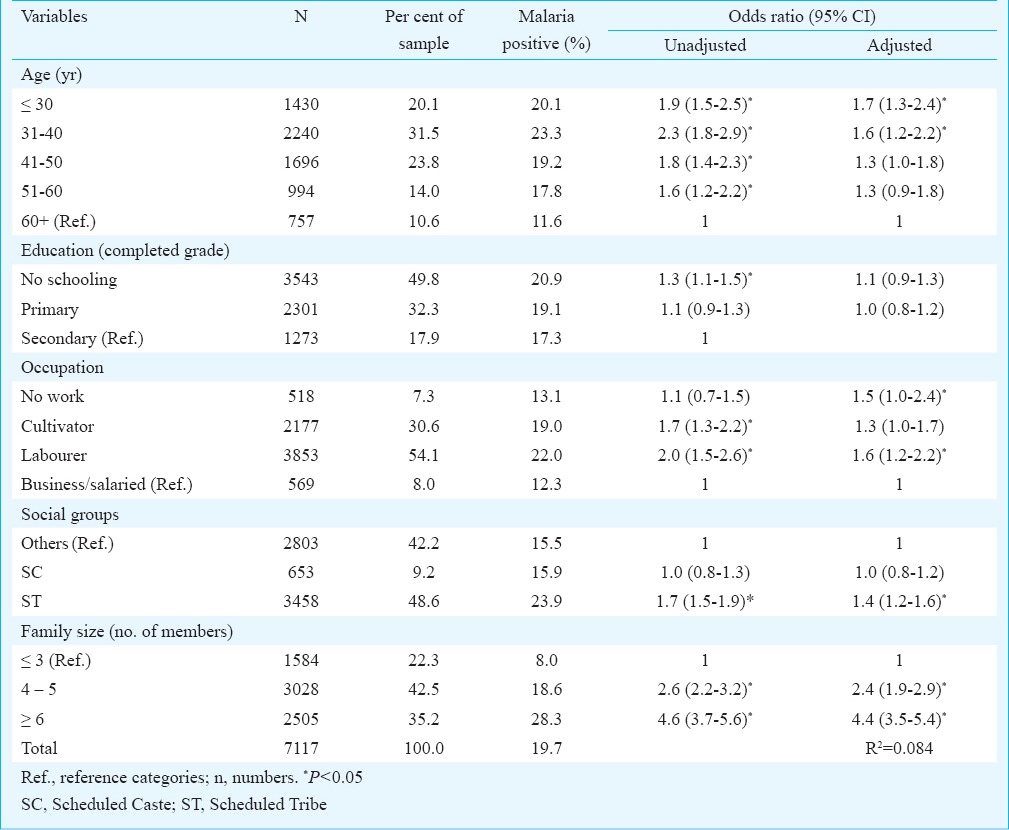
Table II.
Housing characteristics and their association with malaria (May 2005 to June 2008)
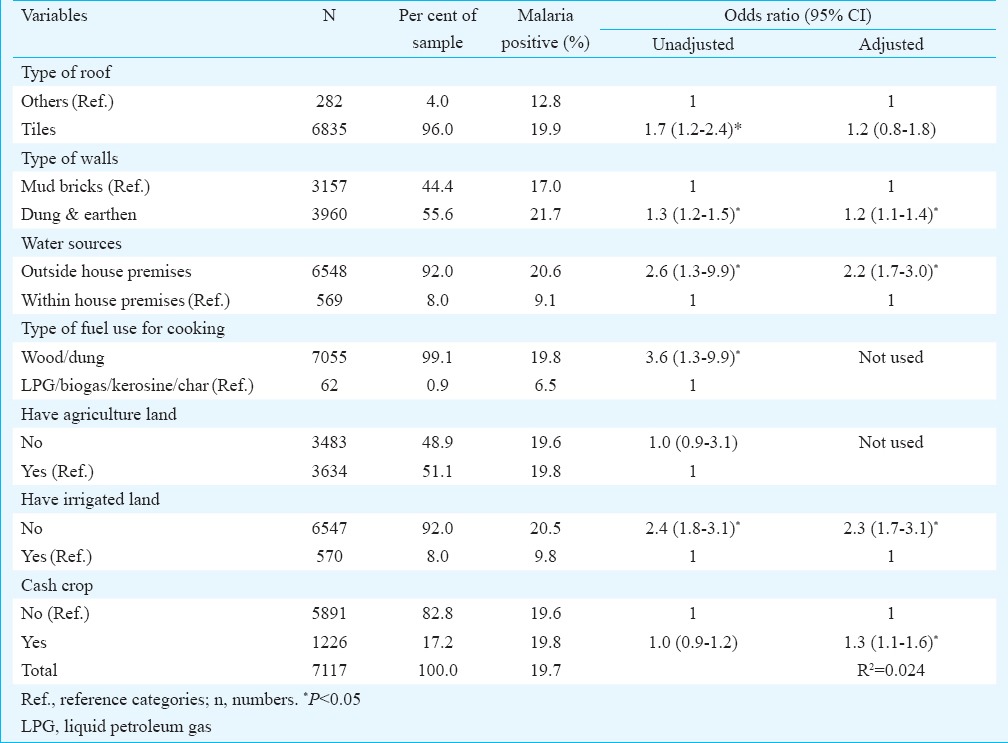
Table III.
Household behavioural indicators and their association with malaria (May 2005 to June 2008)
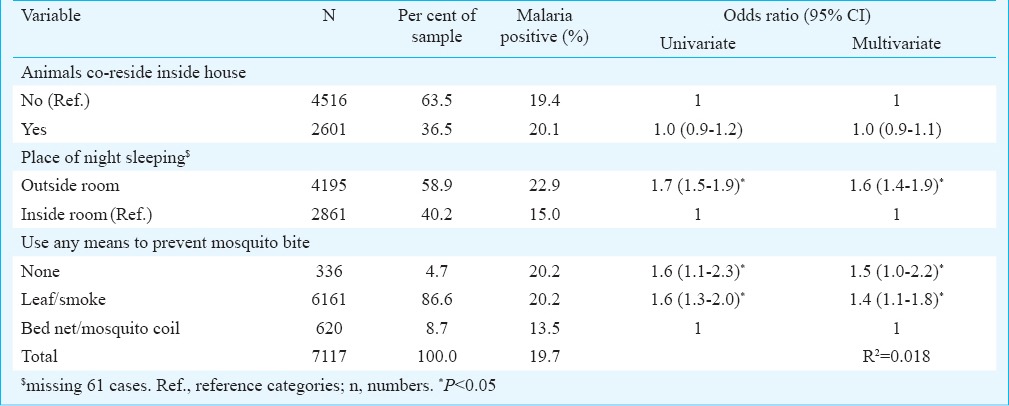
Table IV.
Socio-demographic, socio-economic and behavioural determinant of malaria (Result of logistic regression with backward elimination method) (May 2005 to June 2008)
During the study period (May 2005-June 2008) on an average every selected village was visited 70-72 times and overall, 5049, 9280, 9343 individuals were screened for malaria, respectively during 2006, 2007, and 2008, of whom 19, 15 and 14 per cent were found positive for malaria with 69, 63, and 46 per cent P. falciparum, respectively during these years. Overall ratio of P.falciparum and P.vivax was 5.9:4.1 and significantly more malaria and P.falciparum (P<0.001) was recorded in children (>1-14 yr) as compared to older age groups (>14 yr).
Association of different socio-demographic characteristics with malaria: Head's age demonstrated a negative effect, indicating that younger heads (≤ 40 yr) had relatively more chances of finding a patient in the household, ceteris paribus. A household with 30 yr or younger and 31-40 yr old head had respectively 1.7 and 1.6 times more chances to have a malaria patient at household as compared to a household with 60 year or older heads (Table I). The education level of head of household was not significantly (adjusted cases) associated with malaria. But occupation of household head had significant impact of malaria occurrence. Households with labourer heads had significantly more chances of having malaria cases as compared to households with salaried/business man as head (Table I). The scheduled tribes (ST) households had significantly more malaria cases, i.e. 1.4 times more to have a malaria cases as compared to other social groups households (mainly other backward classes). Crowding at household (family size) was also significantly associated with malaria, even when controlled for other characteristics of head (Table I), and controlled for all other variables (Table IV). A household with 4-5 members and households with six or more members were 2.4 and 4.4 times more likely to have a malaria patient as compared to households with three or less members (Table I).
Association of different socio-economic variables with malaria: Impact of different housing characteristics and economic variables on malaria is shown in Table II. The housing construction features, material used in construction of walls and roof showed a significant association (unadjusted) with malaria (Table II), but when these results were controlled for other household characteristics, the variable ‘type of roof’ had no significance. Thus, type of roof construction was not included in final model (Table IV). After controlling for all other significant variables, bricks made walls significantly reduced chances of malaria. The houses with brick (mainly mud bricks) walls had significantly less chances to have a malaria case as compared to houses with walls made of dung and earth, or thatch/grass bricks (Table IV).
A source of drinking water within household also minimized the risk of malaria. Households using wood and dung cakes as cooking fuel were significantly more at risk to have malaria cases, but this result could be possible because of sample bias as about 99 per cent households were using wood and dung cakes as cooking fuel in the study area. Thus, this indicator was not used in multivariate analyses. Possession of irrigated land significantly reduced the chances of having malaria. Thus, only dummy variable for irrigated land was used in subsequent multivariate analyses (Tables II & IV). However, cash crop cultivators had significantly more chance to have a malaria patient in households.
Association of different household behavioural variables with malaria: Household behavioural variables such as mixed dwelling, place of sleeping of household members and use of mosquito nets or other preventive means for malaria are known to have significant impact on malaria. However, the variable ‘mixed dwelling’ had no significance in presence of other behavioural variables. Sleeping outside house and no use of bed nets or any other preventive means, substantially increased the risk of malaria at household level (Table III). In the final model, when analysis was controlled for other socio-demographic and socio-economic variables, use of preventive measures lessened the significance and was thus eliminated from the final model. Hence, among behavioural variables only place of sleeping was significant and included in final model.
Discussion
Several studies have reported the significance of head's age in the probability of the presence of malaria patient in the household. The present study also showed that even after controlling for other socio-demographic and socio-economic and behaviour risk factors, the age of head had significant negative association with malaria. Such results are expected, as head's age is a proxy of maturity and familiarity with symptoms and preventive methods of malaria12. The houses with younger heads had younger children in household having higher risk of malaria patient at home.
It was assumed that educated heads and members had a better understanding of health related issues. Results of univariate analysis supported this hypothesis, but when model was controlled for socio-demographic (multivariate) variables, education reduced its significance. In studies from Southeast Asia13,14 overall education levels of guardians were not found to be significantly associated with malaria in their children.
Agricultural labourers are known to be at a higher risk through increased risk of contact with malaria vector at field11,15,16. Similarly, workers engaged in inferior occupation categories have higher risk of malaria as compared to those engaged in better professions/jobs17,18. Workers are at higher risk of malaria due to their outdoor sleeping, frequent movement and inadequate treatment18. In the present analysis also occupation of household head showed significant effect on malaria – labourers had higher chances of having malaria cases as compared to salaried and businessmen.
The reasons for higher chances of malaria in socio-economicall weaker groups as compared with the other social and economically forward groups may be centered around the lifestyle compounded by poverty19. This study also showed that considerably more tribal households had malaria cases as compared with others social group households. The collection of firewood and other forest product, outdoor activities, poor housing, outdoor sleeping habits are common characteristics of tribes, and are determinants of malaria transmission in tribal areas15.
One of the highly significant socio-demographic variables in the study was family size. Families with 4-5 members and six or more members had considerable higher chances of having a malaria case as compared with family with ≤3 members. This finding has also been confirmed by many other earlier studies, even though using different proxies, i.e. including number of people in the house12, number of rooms available for sleeping11 and the number of people per room20,21.
House quality is known to affect the entry of mosquitoes in dwelling places. A Sri Lankan study10 showed that housing type was more important determinant of variability in malaria risk than the socio-economic differences that accompanied it. However, in presence of other socio-demographic variables, type of roof construction demoted and only walls construction remained significant. Many earlier studies have also drawn similar inference13,21,22,23. The mud housing are often mentioned as a drawback in the conventional malaria control programme using insecticides because of the practice of mud plastering soon after spray24,25. Further, this study demonstrated that dependence on outside water sources substantially increased chances of having malaria infection.
Literature on the effect of cattle near to or in the house in relation to malaria is inconsistent26. An African study showed that keeping cattle in the house was a risk factor for occurrence of malaria among children27. The present study did not show any such association when controlled for sleeping habits and use of bed nets. The use of bed nets or other preventive measures significantly reduced the chances of malaria, but presence of other socio-demographic and socio-economic variables reduced its significance and was dropped from the final model. Our study revealed that sleeping habits, for instance, sleeping outside house or in open verandas, significantly increased the chances of having malaria. Many other studies have also concluded the same28,29.
This study had some limitations. As this was a part of a large research project, detailed information such as movement/migration history was not recorded during the baseline and subsequent fortnight fever surveys. Information on socio-economic aspect of household was also collected during baseline survey only and not updated during subsequent surveys. It was assumed that this would have remained constant throughout the study period. Even if a person was found positive during the study period, the household was classified as a household with malaria. Further, information on knowledge, attitude and practices (KAP) was also not collected.
In conclusion, this study confirms that in tribal areas where poverty is rampant and lifestyle comprises poor housing quality, lack of knowledge, availability and use of preventive means, malaria is firmly established. Improvements in standard of living, good access to healthcare facilities, health awareness, large-scale community based interventions that either prevent infection or reduce the rate or intensity of exposure will have a significant impact in future in these areas.
References
- 1.World Malaria Report 2013. Geneva: World Health Organization; 2013. [accessed on March 11, 2014]. WHO. Available from: www.who.int/iris/bitstream/10665/97008/1/9789241564694_eng.pdf . [Google Scholar]
- 2.Weller TH. Encyclopedia Britannica. Chicago: William Bennet; 1958. Tropical medicine; pp. 495–7. [Google Scholar]
- 3.Narain JP. Malaria in the south-east Asia region: myth and the reality. Indian J Med Res. 2008;128:1–3. [PubMed] [Google Scholar]
- 4.Singh R, Jain V, Singh PP, Bharti PK, Thomas T, Basak S, et al. First report of detection and molecular confirmation of Plasmodium ovale from severe malaria cases in Central India. Trop Med Int Health. 2013;18:1416–20. doi: 10.1111/tmi.12184. [DOI] [PubMed] [Google Scholar]
- 5.Tyagi PK, Das MK, Singh SS, Sharma YD. Discordance in drug resistance-associated mutation patterns in marker genes of Plasmodium falciparum and Plasmodium knowlesi during coinfections. J Antimicrob Chemother. 2013;68:1081–8. doi: 10.1093/jac/dks508. [DOI] [PubMed] [Google Scholar]
- 6.Bharti PK, Chand SK, Singh MP, Mishra S, Shukla MM, Singh R, et al. Emergence of a new focus of Plasmodium malariae in forest villages of district Balaghat, Central India: implications for the diagnosis of malaria and its control. Trop Med Int Health. 2013;18:12–7. doi: 10.1111/tmi.12005. [DOI] [PubMed] [Google Scholar]
- 7.Singh N, Chand SK, Bharti PK, Singh MP, Chand G, Mishra AK, et al. Dynamics of forest malaria transmission in Balaghat district, Madhya Pradesh, India. PLoS One. 2013;8:e73730. doi: 10.1371/journal.pone.0073730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh N, Mishra AK, Chand SK, Sharma VP. Population dynamics of Anopheles culicifacies and malaria in tribal area of central India. Am J Mosquito Control Assoc. 1999;15:283–90. [PubMed] [Google Scholar]
- 9.National Drug Policy on malaria. Delhi: Directorate of National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India; 2013. [accessed on June 17, 2014]. National Vector Borne Disease Control Programme. Available from: http://nvbdcp.gov.in/Doc/National-Drug-Policy-2013.pdf . [Google Scholar]
- 10.Gamage-Mendis AC, Carter R, Mendis C, De Zoysa AP, Herath PR, Mendid KN. Clustering of malaria infections within an endemic population: risk of malaria associated with the type of housing construction. Am J Trop Med Hyg. 1991;45:77–85. doi: 10.4269/ajtmh.1991.45.77. [DOI] [PubMed] [Google Scholar]
- 11.Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes M, Linday SW, et al. Household risk factors for malaria among children in the Ethopian highlands. Trans R Soc Trop Med Hyg. 2000;94:17–21. doi: 10.1016/s0035-9203(00)90424-3. [DOI] [PubMed] [Google Scholar]
- 12.Mensah OA, Kumaranayake L. Vol. 68. Health Pol; 2004. Malaria incidence in rural Benin: does economics matter in endemic area? pp. 93–102. [DOI] [PubMed] [Google Scholar]
- 13.Butraporn P, Sornmani S, Hungsapruek T. Social, behavioural, housing factors and their interactive effects associated with malaria occurrence in east Thailand. Southeast Asian J Trop Med Public Health. 1986;17:577–83. [PubMed] [Google Scholar]
- 14.Fungladda W, Sornmani S, Klongkamnuankarn K, Hungsapruek T. Sociodemographic and behavioural factors associated with hospital malaria patients in Kanchanaburi, Thailand. J Trop Med Hyg. 1987;90:233–7. [PubMed] [Google Scholar]
- 15.Singh N, Mishra AK, Shukla MM, Chand SK. Forest malaria in Chhindwara, Madhya Pradesh (central India) - A case study in an ethnic tribal community. Am J Trop Med Hyg. 2003;68:602–7. doi: 10.4269/ajtmh.2003.68.602. [DOI] [PubMed] [Google Scholar]
- 16.Dysoley L, Kaneko A, Eto H, Mita T, Socheat D, Börkman A, et al. Changing patterns of forest malaria among the mobile adult male population in Chumkiri District, Cambodia. Acta Trop. 2008;106:207–12. doi: 10.1016/j.actatropica.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Tshikuka JG, Scott ME, Gray-Donald K, Kalumba ON. Multiple infection with Plasmodium and helminthes in communities of low and relatively high socio-economic status. Ann Trop Med Parasitol. 1996;90:277–93. doi: 10.1080/00034983.1996.11813053. [DOI] [PubMed] [Google Scholar]
- 18.Singh N, Nagpal AC, Saxena A, Singh MP. Changing scenario of malaria in central India, the replacement of Plasmodium vivax by Plasmodium falciparum (1986-2000) Trop Med Int Health. 2004;9:364–71. doi: 10.1046/j.1365-3156.2003.01181.x. [DOI] [PubMed] [Google Scholar]
- 19.Worrall E, Basu S, Hanson K. The relationship between socio-economic status and malaria: a review of the literature. [accessed on March 11, 2014]. Available from: http://siteresources.worldbank.org/INTMALARIA/Resources/SESMalariaBackground Paper.pdf .
- 20.Koram KA, Bennett S, Adiamah JH, Greenwood BM. Socio-economic risk factors for malaria in a peri-urban area of The Gambia. Trans R Soc Trop Med Hyg. 1995;89:146–50. doi: 10.1016/0035-9203(95)90471-9. [DOI] [PubMed] [Google Scholar]
- 21.Guthmann JP, Hall AJ, Jaffar S, Palacios A, Lines J, Llanos-Cuentas A. Environmental risk factor for clinical malaria: a case-control studying the Grau region of Peru. Trans R Soc Trop Med Hyg. 2001;95:577–83. doi: 10.1016/s0035-9203(01)90084-7. [DOI] [PubMed] [Google Scholar]
- 22.Somi MF, Butler JR, Vahid F, Njau JD, Kachur SP, Abdulla S. Is there evidence for dual causation between Malaria and Socioeconomic status. Findings from Rural Tanzania? Am J Trop Med Hyg. 2007;77:1020–7. [PubMed] [Google Scholar]
- 23.Somi MF, Butler JR, Vahid F, Njau JD, Kachur SP, Abdulla S. Use of proxy measures in estimating socio-economic inequalities in malaria prevalence. Trop Med Int Health. 2008;13:354–64. doi: 10.1111/j.1365-3156.2008.02009.x. [DOI] [PubMed] [Google Scholar]
- 24.Dhillon HS, Kar SB. Malaria eradication: An investigation of cultural patterns and belief among tribal populations in India. J Health Edu. 1965;1:31–40. [Google Scholar]
- 25.Arora DD, Salu B. Extent and frequency of mud plastering tribal units of Orissa state. NMEP News. 1976:16–26. [Google Scholar]
- 26.Bouma M, Rowland M. Failure of passive zooprophylaxis: cattle ownership in Pakistan is associated with a higher malaria prevalence. Trans R Soc Trop Med Hyg. 1995;89:351–3. doi: 10.1016/0035-9203(95)90004-7. [DOI] [PubMed] [Google Scholar]
- 27.Seyoum A, Balcha F, Balkew M, Ali A, Gebre-Michael T. Impact of cattle keeping on human biting rate of anopheline mosquitoes and malaria transmission around Ziway, Ethopia. East Afr Med J. 2002;79:485–90. doi: 10.4314/eamj.v79i9.9121. [DOI] [PubMed] [Google Scholar]
- 28.Datta HM, Datta K. Malaria ecology: A global perspective. Soc Sci Med. 1978;12:69–84. [PubMed] [Google Scholar]
- 29.MacCormack CP. Human ecology and behaviour in malaria control in tropical Africa. Bull World Health Organ. 1984;62:81–7. [PMC free article] [PubMed] [Google Scholar]


