Abstract
Background & objectives:
Malaria is a serious public health concern in several parts of India, particularly in tribal areas of Madhya Pradesh (MP). Dindori district inhabitated by Baiga tribe, contributes about 15 per cent to the total malaria burden in MP. The tribal and other local inhabitants believe in magico-religious treatment of malaria and use modern health facilities only as second line of treatment. The present study was planned in the villages of one of the particularly vulnerable tribal group of MP, the Baigas. The objective of the study was to generate awareness and utilization of health services for malaria by establishing a communication strategy using local students and unemployed youths as agents of change.
Methods:
The study was undertaken in 47 villages and the need based IEC (information, education and communication) intervention was evaluated within four months of initiation by adopting before and after with control design. For both baseline and resurvey the households covered each time were 2350.
Results:
The baseline data generated revealed that around 53 per cent of the people in the study villages were aware of malaria. Among the non Baigas, 59 per cent were aware of malaria, while among the Baigas it was 49 per cent. IEC intervention could raise the level of awareness to malaria significantly with a net intervention effect of 23 per cent. The IEC intervention also improved the utilization of modern health services significantly.
Interpretation & conclusions:
The IEC strategy designed by using local children and youths was effective as the malaria was on decline in the study area. The same strategy with necessary modifications may be replicated in other areas pandemic for malaria.
Keywords: Baiga tribe, folk theatre, IEC intervention, malaria
Malaria is found throughout the tropical and sub-tropical regions of the world and causes more than 300 to 500 million cases of acute illness and at least one million deaths annually1,2,3,4. In India, malaria is a major public health concern5. According to an estimate, 89 per cent of the India's population are at risk of malarial infection6 and 80 per cent of malaria reported in the country is confined to areas consisting of 20 per cent of population residing in tribal, hilly, difficult and inaccessible areas7. India has the highest number of malaria deaths outside of the African continent with an estimated 200,000 deaths annually8. According to an estimation based on National Vector Borne Disease Control Programme (NVBDCP) data approximately 50 per cent of all malaria deaths in India occur in tribal dominated areas9.
In Madhya Pradesh malaria control is complex because of its difficult geographical set up such as deep valleys, hills and hillocks with thick dense forest along with large tribal settlement (15% of India's tribal population)10,11,12 and poorly understood sociological factors13. Among the vulnerable tribal areas of Madhya Pradesh, Dindori district, inhabited by the Baiga tribes contributes 12-15 per cent of malaria cases in the State with the blocks Bajag, Samnapur and Karanjia14,15. During the period 1999 to 2008 the overall malaria in the above blocks showed a declining trend, however, per cent Plasmodium falciparum (Pf) cases has increased considerably. The per cent Pf+ cases at Samnapur was 10.93 during 1999 and it increased to 22.04 in 2003 and 91.04 in 2008. Similarly per cent Pf+ cases was 4.87 in 1999 at Bajag and it increased to 13.78 in 2003 and 50.00 in 2008. The similar figures for Karanjia were 64.59 per cent in 1999, 81.22 per cent in 2003 and 88.17 per cent in 200815.
The Baigas are aboriginal group and invariably lead an isolated life and are at the low levels of education and have poor social cultural development. They are still guided by magico-religious treatment of the diseases and utilize modern medical facilities available to them as second line of treatment leading to underutilization of health services16. The underutilization of health services among the scheduled tribes has been revealed by the Reproductive and Child Health surveys and three rounds of National Family Health surveys17,18,19. There is a need to investigate the magnitude of the problem, inter-relationship with their socio-cultural habits, and to plan suitable information, education and communication (IEC) intervention strategy to educate them to accept the health services provided to them20. There is no standard health educational format; however, there are various forms of delivering health messages21. The present study was aimed to establish a sustainable communication strategy in tribal areas of Dindori district in MP using various mass media tools including folk theatre based approach involving local school going children and unemployed youths as agents of change for prevention and management of malaria.
Material & Methods
The study was initiated in 2011 and continued up to 2014 in Baiga Chak area of Dindori district of Madhya Pradesh by the National Institute for Research in Tribal Health (NIRTH) formerly known as Regional Medical Research Centre for Tribals (RMRCT), Jabalpur, by recruiting 51 temporary field staff specially for this study. The staff included 47 village facilitators, three block monitors and one field coordinator. Further, 235 local school going students of VIII to XII standard and unemployed youths were selected from 47 Baiga tribal dominated villagers as IEC activists/agents of change.
Dindori district situated at the eastern part of Madhya Pradesh. As per 2011 census22 the district has a population of 7,04,524 people, of which more than 50 per cent are of tribal population10. Around 64 per cent of the total population belongs to the Scheduled Tribes (ST) groups. Total area of the district is 6128 sq.km with seven administrative blocks. Sixty five per cent of the area falls under the tribal zone. Literacy rate was 65 per cent (Census 2011)22. The present intervention included mainly the Baiga dominated tribal villages in Baiga Chak area comprising Bajag, Samnapur and Karanjia blocks. Baigas are one of the particularly vulnerable tribal groups (PVTG) of Madhya Pradesh. Their population as per the 2001 Census10 was 332936 and as per 2011 Census22 was 4,14,526. The Baiga Chak villages are mainly located at forests. Being forest villages these are located in very remote areas where excess to health care facilities is meagre16.
Study design: The objective was to establish a communication strategy designed for prevention against malaria by harnessing local school going children and unemployed youths as agents of change. For evaluating the effect of the strategy within a short interval of four months a quasi experimental design including controls was adopted. For baseline survey (conducted during November 2011 to February 2012) the minimum sample size estimated for each of the three blocks under study was kept constant as also during re-evaluation survey conducted in July 2012. The earlier study carried out in selected villages in the same area showed that only 37.6 per cent respondents reported about malaria transmission through mosquitoes23. Thus assuming the awareness to malaria about 40 per cent in study population, at 95 % level of confidence, five per cent absolute precision and total population of Baiga dominated villages in selected blocks as 10,000 tribal population (N=10,000) using formula and design effect equal to 2, a minimum sample of 712 was required from each block. Thus, selecting 50 households randomly from a selected village and interviewing one respondent per household, we included about 700-800 respondents from a block (depending on number of tribal villages in a block). A total of 2350 households from 47 villages (850 households from 17 villages in Bajag, 800 households from 16 villages in Samnapur and 700 households from 14 villages in Karanjia) were enrolled. Looking into the homogeneity of the level of awareness on malaria from baseline survey for the three study blocks and keeping in mind the distance and geographic locations of the 47 villages, Karanjia block was kept as control, while villages in Bajag and Samnapur were considered for IEC intervention.
The ethical clearance for the study protocol was obtained from the ethics committee of NIRTH, Jabalpur. Informed written consents were obtained from the respondents both during baseline and resurvey.
Language used in interviews/IEC activities: Survey queries were made in local Hindi language so as to make it easy for the tribals to understand and respond. The IEC sensitization programme was also conducted in Hindi. Local popular terms related to various aspects of malaria were noted during the pre-testing of survey instrument and were used both in surveys and during IEC activities.
Survey: Door-to-door survey was undertaken interviewing only one eligible respondent who can understand and respond to the queries from each household. In both the surveys households were selected randomly. The survey schedule was administered by selected students in their own villages in both the surveys after they were specially trained by organizing 12 one day survey orientation workshops in 12 contact locations in the three studied blocks.
Qualitative in-depth interviews were undertaken to know the issues and local terminologies related to malaria and these helped to develop interview schedule for quantitative survey. The schedule was pre-tested and modified before it was finally used in the field. The broad aspects covered in the schedule included queries on to assess the knowledge and perception on malaria, queries on preventive aspect, record suffering from malaria and treatment seeking behaviour.
Information, education and communication (IEC) activities: In the initial phase, a rapid appraisal study was undertaken to identify the aspects hindering control and also the prevailing myths and misconceptions. There was low awareness on causes and consequences of malaria, low usage of mosquito nets, unwillingness to use mosquito nets and mosquito repellents and casual approach towards proper health seeking behaviour. There was also low awareness on anti-malarial drugs and over reliance on herbal medicine or the occult practices (by traditional spiritual healer). Under such a scenario, a unique theatre based approach was used to effectively reach out to the vast vulnerable tribal groups for making them aware of the deadly consequences of malaria, its transmission mechanism, method and source of curability as well as initiate preventive measures by mobilizing the target beneficiaries.
Besides the village facilitator, five school going children/ unemployed youths were recruited from each of the study villages by organizing personal interview with the help of block administrative authorities of the Government of Madhya Pradesh. In all 235 students/youths and 47 facilitators selected from 47 villages acted as agents of change. These students were imparted training on various aspects of malaria at different workshops. Thirty six workshops were carried out at 12 contact locations covering 47 villages across the three blocks- Bajag, Samnapur and Karanjia for 84 days. Health providers like Block Medical Officers and others were invited during workshops to make them understand the effectiveness of such campaigns in their local area. Village facilitators, block monitors and field coordinator were involved in conducting the shows, thus ensuring their hands on experience in conducting such campaigns in the field independently and village level plans were passed on to them for further monitoring and control. These activities were carried out in both the intervention blocks (Bajag and Samnapur) exclusively until resurvey was done after four months of initiation. After resurvey similar workshops were organized in control block Karanjia.
After sensitization the IEC activities were initiated by the students and village facilitators at their respective villages, usually once every fortnightly for 30 to 40 minutes at their convenient time without disturbing their routine life and studies. Their activities were closely monitored by the block monitors and field coordinator.
Statistical analysis: The data entry was done into CS-Pro-4 format specially designed for the study. The data were analysed using SPSS-10 software (SPSS Inc., Chicago, USA). Test of significance was attempted and shown with estimates of net intervention effects following before and after with control design. The test of significance was shown for the difference that existed between post intervention outcome variables compared with the change in control group. Multivariate logistic regression was attempted with baseline data to give an insight in to some of the background correlates of awareness to malaria. Fever was noted as an important symptom of malaria, the self suffering from this symptom by the respondent was recorded for three months preceding the survey in both baseline and resurvey. The variables for which net intervention effect was estimated, were treated as outcome variables.
Results
Around 56 per cent of the studied population was literate. Nearly 77 per cent of the literate had studied up to middle standard. Majority of them were engaged as agricultural and unskilled labourer. Most of them (95%) resided in kachcha and only one per cent in pukka houses. Cattles were by and large placed outside the main dwelling separately (77%), while in 13 per cent households, residents share space with cattle in the same house or in the room. The baseline survey revealed that a little more than 50 per cent of the studied population was aware of malaria. Among non-Baiga population 59 per cent were aware of malaria compared to Baigas (49%) and results of the logistic regression revealed the differences as significant (P<0.05).
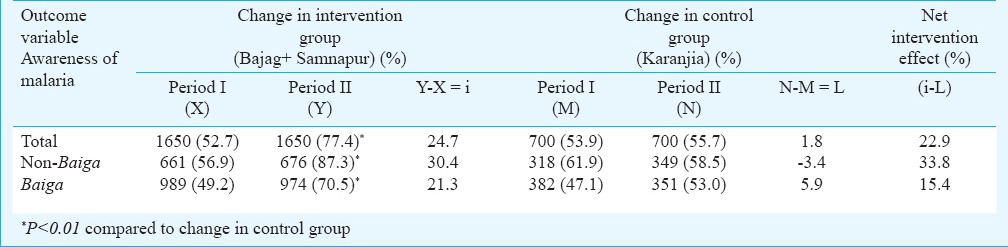
Further, the logistic regression also indicated that males were better aware than females (P<0.05) and higher the level of education better was the awareness (P<0.05). Other predictors considered in the model were age of the respondents, marital and professional work status. The implementation of IEC strategy was instrumental in improving significantly the awareness to malaria in intervention group villages. Overall, the improvement was 77 per cent in intervention group compared to 56 per cent in control group (P<0.05). The IEC intervention effect in improving the awareness to malaria was higher among the non-Baiga population (34%) compared to Baigas (15%) (Table I). As promoted by the IEC strategy, village health workers proved to be the best source of information for malaria prevention and cure.
Table I.
IEC (information, education and communication) intervention effect on awareness to malaria
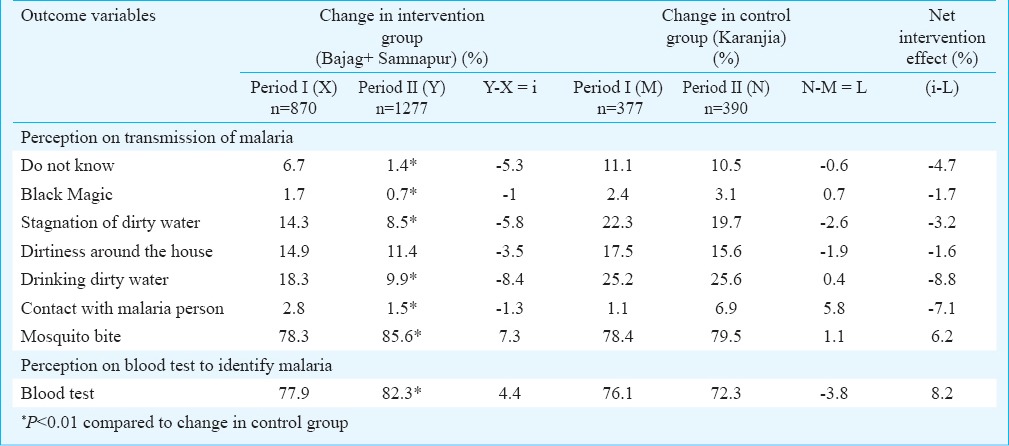
More than 78 per cent reported the reason of transmission by mosquito bite and the IEC intervention could improve the perception significantly in intervention villages (86%) compared to control area (80%) (P<0.01). The net IEC intervention effect was 6.2 per cent. Sharp reductions in all types of misconception were noticed after IEC intervention. People's perception on blood test to diagnose malaria was also recorded. The intervention could significantly improve their perception on blood test to diagnose malaria in intervention area by 82.3 per cent compared to those in control area (72.3%) (P<0.01) (Table-II). The negative figures of net intervention effect in this Table indicates decline in misconception/not aware of transmission of malaria. In the control area the anti-malarial activity of the national programme included distribution of long lasting insecticide treated nets (LLIN), indoor residual spray (IRS), use of larvivorous fishes and prompt diagnosis and treatment by accredited social and health activists (ASHA)/malaria workers, and these activities to some extent helped to improve the perception of the people on right diagnosis of malaria in the area.
Table II.
IEC intervention effect on perception of transmission of malaria and its diagnosis by blood test
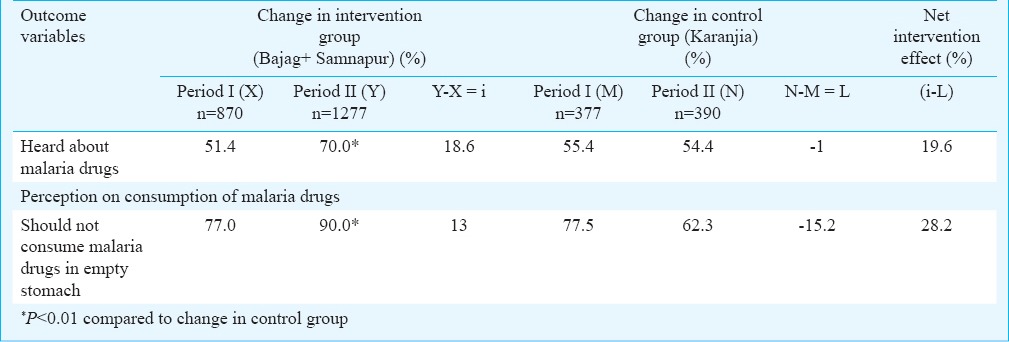
Those who were aware of malaria were further checked to understand their level of awareness regarding drugs used for treatment of malaria. IEC intervention could improve the awareness to anti-malaria drugs in intervention area (70%) compared to control area (54%) (P<0.01) with a net intervention effect of 20 per cent. Further, intervention could improve their perception that malaria drugs should not be consumed in empty stomach by 28 per cent (Table III).
Table III.
IEC intervention effect on awareness to anti-malaria drugs
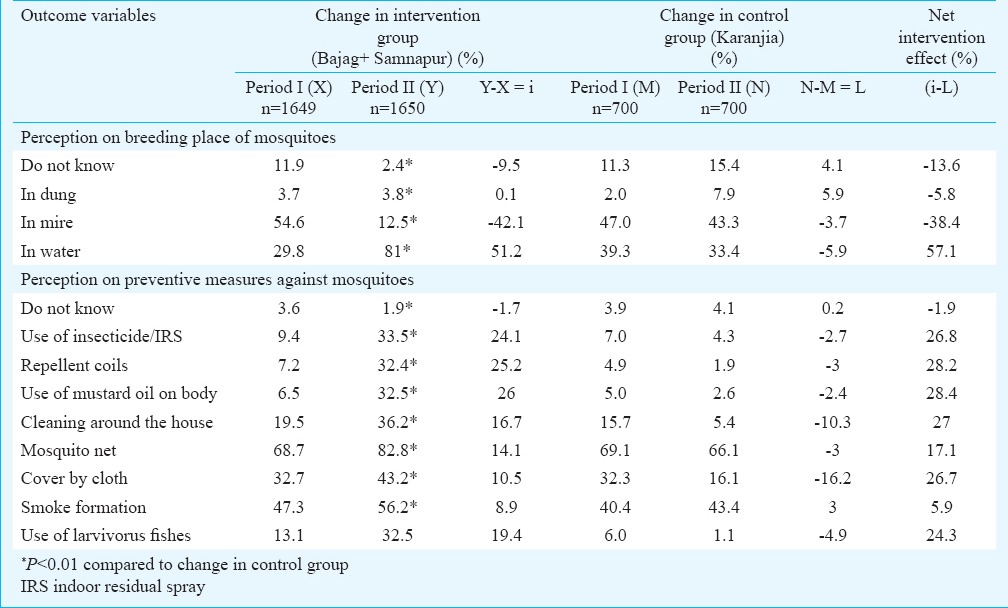
The perceptions of breeding place and preventive measures against mosquitoes were also recorded and effort was made through IEC strategy to reduce their misconceptions. IEC intervention significantly reduced their misconception on the breeding place (P<0.01). There was also a sizeable reduction in the proportion of respondents who were not at all aware of the breeding place.
There was significant improvement in the knowledge in intervention area where 81 per cent understood about mosquito breeding in stagnate water, while the same in control area was 33 per cent (P<0.01) with a net intervention effect of 57 per cent. Intervention also improved their perception regarding the preventive measures against mosquitoes. The net intervention effect on their perception regarding proper use of bed nets was 17 per cent, for use of mosquito repellent coil (28%) and for the use of insecticide particularly indoor residual spray by the malaria workers was 27 per cent (Table IV). The negative figures of net intervention effect in this Table indicates decline in misconception/not aware of breeding place and preventive measures against mosquitoes.
Table IV.
IEC intervention effect on perception of breeding place and preventive measures against mosquitoes
During baseline survey, around 52 per cent of the respondents revealed their first choice as traditional village healer for treatment for fever, followed by locally available private medical practitioner (17%) and treatment by local shopkeepers having medicines (11%). Only 14 per cent expressed their first choice as government health posts (hospital, PHC (primary health centres)/SC (sub centres) and only five per cent for malaria/ASHA workers. IEC strategy was designed to explain and motivate the community regarding the importance of modern government health services, and their proper utilization to prevent morbidity and mortality. Thrust was given to change the people's preference as first choice for easily available unqualified local health providers. The IEC intervention changed significantly the treatment preferences for fever as first choice by government hospital/PHC/SC in intervention area by 50 per cent compared to control area (20%) (P<0.01) with net intervention effect of 35 per cent. The intervention also led to improvement in treatment preference for malaria worker/ASHA and local private doctors (Table V). The negative figures of net intervention effect in this Table indicates decline in preference of the people for treatment of fever from unqualified traditional sources.
Table V.
IEC intervention effect on treatment preference for fever as first choice
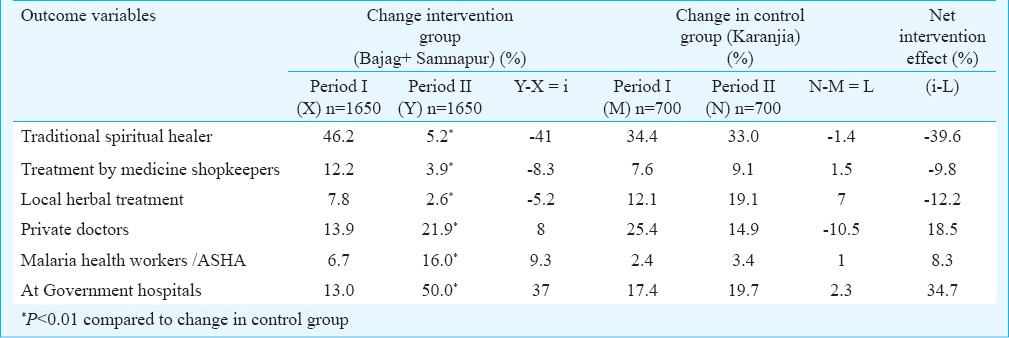
To know the actual utilization of health services from various sources, those who suffered from fever during three months preceding both the surveys (baseline and resurvey) were considered. In baseline survey, 61 per cent (1441/2350) reported suffered from fever, 86 per cent (1231/1441) of these availed any treatment. In those who could not avail treatment (209 respondents) the main reasons reported were economic problem (71%) followed by inaccessible location of health posts (5%), irregularity of health staff (4%), ineffective medicine (3%) and perception that fever gets cured without treatment (17%). IEC intervention could improve significantly the utilization of treatment services for fever in intervention area (98%) compared to control area (91%) (P<0.01) with net intervention effect of 11 per cent. The IEC intervention improved the utilization of health services for fever from government hospitals/PHC/SC (31%), local private doctors (23%) and malaria health workers/ASHA (4%), while there was a decline in health services from other village level unqualified traditional health providers.
Discussion
Malaria is a major public health challenge specifically in tribal areas in central India. Though mortality due to malaria in different age groups has been reported7,24, malaria is preventable and curable if diagnosed quickly25 and proper treatment is taken. The results of the present study revealed that around half of the respondents were aware of malaria and even among this group there existed misconception regarding transmission of the infection and treatment seeking. IEC intervention improved the level of awareness to malaria significantly among intervention group compared to controls. The improvement was much pronounced for non-Baigas compared to Baiga population in the same villages. Some community based health education studies undertaken in Africa and also in India revealed remarkable improvement in awareness and change in attitude about malaria and its control strategies4,21. In the intervention area there was a decline in the misconceptions on transmission mechanism of malaria infection. There were misconceptions about malaria diagnosis also. However, more than three-fourth of the respondents were aware of blood test to diagnose malarial infection. Though the IEC intervention improved their knowledge about malaria diagnosis, but net intervention effect was not high as the knowledge was already higher. The IEC intervention also improved significantly their awareness to malaria drugs and the process of consumption.
The IEC interventions also focussed on preventive measures against mosquitoes for control of malaria. The thrust was on to promote IRS by the malaria health workers in the villages, proper use of mosquito nets during sleeping, and use of larvivorous fishes. It was observed that government health services were not popular in the study area. There is a need to identify these unqualified locally popular health providers and provide them with information and training on prevention, diagnosis and treatment of malaria, so that they can act as intermediate behaviour change communicator. The study showed that merely providing some current tools would not serve the purpose in such areas. There is a need to improve the inter-sectoral cooperation between various heterogeneous groups operating in the area for the prevention of malaria. The children and the youths can be utilized if properly sensitized. The present study was aimed to sensitize and mobilize this young group as agents of change by using strong mass media tools like folk theatre, interactive methods for prevention of malaria. During the period of IEC activities there was a sharp drop in the malaria cases in the Baiga Chak area26. Studies conducted by NIRTH, Jabalpur revealed that 2012 onward there was 50 per cent reduction in overall malaria slide positivity rate and P. falciparum, while P. vivax showed 65 per cent reduction compared to earlier situation in Baiga Chak area26. Though there could be multiple factors responsible for the reduction in malaria cases in this area, but it is believed that the IEC model also played a significant role in reduction of the malaria cases. The present study also acts as an effective model of government and non-government partnership and can be replicated in other backward areas particularly in tribal areas with necessary modifications for prevention and management of the burden of malaria.
Acknowledgment
Authors thank Department of Tribal Welfare, Government of Madhya Pradesh for funding this study with special assistance from Ministry of Tribal Affairs, Government of India. Authors acknowledge Shri G.B.Mukherjee, (IAS Retd.) former Secretary, Ministry of Tribal Affairs, Government of India for his support and guidance, Collector, Dindori, Chief Executive Officers and Block Education Officers of the Blocks Bajag, Samnapur and Karanjia for their cooperation and help during the initiation of the study and continuous support, and staff of i-land Informatics Ltd, Kolkata for their help and cooperation during workshop with children. Authors thank Dr Alpana Abbad, Shiv K. Singh, Sneha Patel and Mithun K. Vishwakarma of NIRTH, Jabalpur for secretarial support and Dr Samiran Bisai of NIRTH and Dr Uma C. Saha, XIDAS, Jabalpur for suggestions.
References
- 1.Gramicia G, Beales PF. The recent history of malaria control and its eradication. In: Wernsdofer W, McGregor I, editors. Malaria, principles, and practices of malariology. Philadelphia: Churchill Livingstone; 1988. p. 1335. [Google Scholar]
- 2.Najera JA. Malaria control: achievements, problems and strategies. Parasitologia. 2001;43:1–89. [PubMed] [Google Scholar]
- 3.Carter R, Mendia KN. Evolutionary and historical aspects of the burden of malaria. Clin Microbiol Rev. 2002;15:564–94. doi: 10.1128/CMR.15.4.564-594.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amoron OE. Impact of health education intervention on malaria prevention practices among nursing mothers in rural communities in Nigeria. Niger Med J. 2013;54:115–22. doi: 10.4103/0300-1652.110046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sabin LL, Rizal A, Brooks MI, Singh MP, Tuchman J, Wylie BJ, et al. Attitudes, knowledge and practices regarding malaria prevention and treatment among pregnant women in eastern India. Am J trop Med Hyg. 2010;82:1010–6. doi: 10.4269/ajtmh.2010.09-0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh N, Singh PK. Insecticide treated nets for malaria control: Challenges and opportunities. Tribal Health Bull. 2013;19:1–9. [Google Scholar]
- 7.Malaria National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India. [accessed on May 12, 2014]. Available from: http://nvbdcp.gov.in/malaria3.html .
- 8.World Malaria Report 2013. Geneva: World Health Organization; 2013. [accessed on March 11, 2014]. WHO. Available from: http://www.who.int/iris/bitstream/10665/97008/1/9789241564694_eng.pdf . [Google Scholar]
- 9.Sharma RK, Thakor HG, Saha KB, Sonal GS, Dhariwal AC, Singh N. Malaria situation in India with special reference to tribal areas. Indian J Med Res. 2015;141:537–45. doi: 10.4103/0971-5916.159510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bisai S, Saha KB, Sharma RK, Muniyandi M, Singh N. An overview of tribal population in India. Tribal Health Bull. 2014;20:1–126. [Google Scholar]
- 11.Singh N, Dash AP, Thimasarn K. Fighting malaria in Madhya Pradesh (Central India): are we losing the battle? Malar J. 2009;8:93. doi: 10.1186/1475-2875-8-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh N, Dash AP, Varun BM, Kataria O. Tribal malaria. ICMR Bull. 2004;34:1–10. [Google Scholar]
- 13.Singh N, Mishra AK, Shukla MM, Chand SK. Forest malaria in Chhindwara, Madhya Pradesh, central India: a case study in a tribal community. Am J Trop Med Hyg. 2003;68:602–7. doi: 10.4269/ajtmh.2003.68.602. [DOI] [PubMed] [Google Scholar]
- 14.Bharti PK, Alam MT, Boxer R, Shukla MM, Gautam SP, Sharma YD, et al. Therapeutic efficacy of chloroquine and sequence variation in pfcrt gene among patients with falciparum malaria in central India. Trop Med Int Health. 2010;15:33–40. doi: 10.1111/j.1365-3156.2009.02425.x. [DOI] [PubMed] [Google Scholar]
- 15.Singh N, Shukla MM, Chand G, Bharti PK, Singh MP, Shukla MK, et al. Epidemic of Plasmodium falciparum malaria in central India, an area where chloroquine has been replaced by artemisinin-based combination therapy. Trans R Soc Trop Med Hyg. 2011;105:133–9. doi: 10.1016/j.trstmh.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Saha KB, Saha UC, Sharma RK, Pandey A. Reaching tribal men to improve awareness to sexual morbidities: experience from Baiga tribe of Central India. Indian J Med Res. 2013;137:928–34. [PMC free article] [PubMed] [Google Scholar]
- 17.Mumbai: IIPS and Calverton, MD: MEASURE DHS+ORC Macro; 2001. International Institute for Population Sciences (IIPS). Reproductive and child health project: Rapid household survey (Phase I and II); 1998-1999. [Google Scholar]
- 18.National Family Health Survey (NFHS-1), India 1992-93, Madhya Pradesh. Mumbai: IIPS; 1993. International Institute for Population Sciences (IIPS) [Google Scholar]
- 19.National Family Health Survey (NFHS-2) India 1998-99. Madhya Pradesh Mumbai: IIPS; 1999. International Institute for Population Sciences (IIPS) and MEASURE DHS ORC MACRO. [Google Scholar]
- 20.Verma A, Saha KB, Kumar D. Infant mortality in tribals of central India. Curr Sci. 2005;89:596–7. [Google Scholar]
- 21.Ghosh SK, Patil RR, Tiwari S, Dash AP. A community-based health education programme for bio-environmental control of malaria through folk theatre (Kalajatha) in rural India. Malar J. 2006;5:123. doi: 10.1186/1475-2875-5-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Census of Inida 2011. [accessed on June 26, 2014]. Available from: http://www.censusindia.gov.in/2011 census/PCA/ST.html .
- 23.Soan V, Chand G. Knowledge, attitude and practice towards malaria in tribal community of Baigachak area, Dindori district (M.P.) In: Singh N, Qamra SR, Bhat J, Sharma RK, Rao KVK, Ray J, editors. proceedings of National Symposium on Tribal Health October 19-20, 2006. Jabalpur, India: Regional Medical Research Centre for Tribals; 2007. pp. 75–84. [Google Scholar]
- 24.Dhingra N, Jha P, Sharma VP, Cohen AA, Jotkar RM, Rodriguez PS, et al. Adult and child malaria mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1768–74. doi: 10.1016/S0140-6736(10)60831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh N, Bharti PK, Singh MP, Mishra S, Shukla MM, Sharma RK, et al. Comparative evaluation of bivalent malaria rapid diagnostic tests versus traditional methods in field with special reference to heat stability testing in central India. PLo s. 2013;8:e58080. doi: 10.1371/journal.pone.0058080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Annual Report 2012-13, Regional Medical Research Centre for Tribals, ICMR, Jabalpur. [accessed on May 12, 2015]. Available from: http://www.nirth.res.in .


