Abstract
Background & objectives:
There has been limited investigation on the prevalence of tuberculosis (TB) in tribal communities in India, a vulnerable section of Indian society. The lack of a population-based estimate prompted us to conduct a meta-analysis of existing studies to provide a single, population-based estimate of the TB prevalence for tribals.
Methods:
Literature search was conducted in PubMed using the keywords - “tuberculosis”, “tribals”, “India”, “prevalence”, and “survey”. References cited in the articles retrieved were also reviewed, and those found relevant were selected. TB prevalence rates estimated by the studies were used for our calculation of a pooled-estimate.
Results:
The pooled estimate, based on the random effects model, was 703 per 100,000 population with a 95 % CI of 386-1011. The associated heterogeneity measures in terms of Cochran's Q was significant (P=0 0.08 <0.1) and I2 was moderate at 48 per cent.
Interpretation & conclusions:
The meta-analysis demonstrated a large variability in pulmonary TB prevalence estimates among the different studies with poor representation of the various tribal groups. The moderate level of heterogeneity found across the studies suggests that the pooled-estimate needs to be treated with caution. Our findings also highlight the need to assess the pulmonary TB burden in India.
Keywords: Culture positive, India, pulmonary tuberculosis, smear positive, TB prevalence, tribal community
According to the report of Government of India, the tribal population in India is estimated to be 104.28 million, representing 8.6 per cent of the country's total population1. There is great heterogeneity across different tribal groups2, which include a sub-category of particularly vulnerable tribes known as primitive tribes1 now renamed as particularly vulnerable tribal groups (PVTG). There are gaping disparities in health status between tribals and inhabitants of metropolitan areas.3 Tribals face a number of health risks, including infant and maternal mortality, malnutrition, anaemia, and malaria4. Their vulnerability can be attributed to high rates of poverty, illiteracy, smoking, and alcohol use, as well as harsh and isolated living environments and poor access to healthcare2,5,6. The combination of increased susceptibility to health afflictions and poor health seeking behaviour is a cause of concern with regard to the management of highly prevalent, communicable diseases, such as tuberculosis (TB).
In 1997, the Government of India launched the Revised National TB Control Programme (RNTCP) to mitigate the high TB burden in the country7. The RNTCP introduced targeted pro-poor approaches for TB control, implementing specific tribal action plans. The National Sample Survey for Tuberculosis, carried out between 1955 and 1958, did not include tribal groups and, therefore, there are no nationwide TB burden estimates available for the tribal population8. However, there are a few epidemiological studies involving tribal communities9,10,11,12,13,14,15,16,17,18,19. Due to lack of a population-based estimate we carried out an in-depth review of these studies and conducted a meta-analysis to arrive at a single meaningful estimate of the TB prevalence for the tribal population.
Material & Methods
Identification and eligibility of studies: As the aim was to ascertain the prevalence of pulmonary TB among the tribal population in India, we selected and reviewed all tribal-focused, community studies, targeting a demographic population above or equal to 15 yr of age. Only those studies in which individuals were examined for TB through initial screening for standard TB symptoms (cough for > 2 wk, fever for > 2 wk, chest pain, and haemoptysis), and subsequently had their diagnosis confirmed by sputum smear and/or culture tests, were selected. Though X-ray screening was also used when TB was suspected, this was not a required procedure given the potential inaccessibility of X-ray equipment in remote areas inhabited by tribal communities.
Search criteria: For the purpose of this meta-analysis, we attempted to include all population based, cross-sectional and cohort studies, both published and unpublished. No language restrictions were applied. Literature searches were conducted in PubMed using the following combination of keywords: “pulmonary tuberculosis”, “tribals”, “India”, “prevalence”, and “survey”. The references cited in the articles retrieved were also reviewed, and those found relevant were selected. Additionally, research institutes working on tribal health were approached for TB prevalence reports. Only published studies were included in this meta-analysis.
Eligibility of studies: The studies obtained through the search were included only if the following criteria were met: (i) should be community-based TB prevalence studies; (ii) have targeted members of tribal communities aged 15 yr and above; (iii) have done initial screening for standard TB symptoms (cough for > 2 wk, fever for > 2 wk, chest pain, and haemoptysis); (iv) have both smear (for acid-fast bacilli, AFB) and culture tests done on the sputum samples collected. A positive case for TB is defined as being positive either by smear and or culture; and (v) reported an outcome measure – the TB prevalence based on smear and/or culture results.
Once qualifying studies for the meta-analysis were identified, TB positives reported in each study were adjusted to account for all eligible individuals in the sample who did not participate in TB screenings and/or sputum testing (i.e. non-coverage). Based on these adjusted figures, TB prevalence rates (per 100,000 population) were estimated for each of the studies. These estimates were used for the analysis.
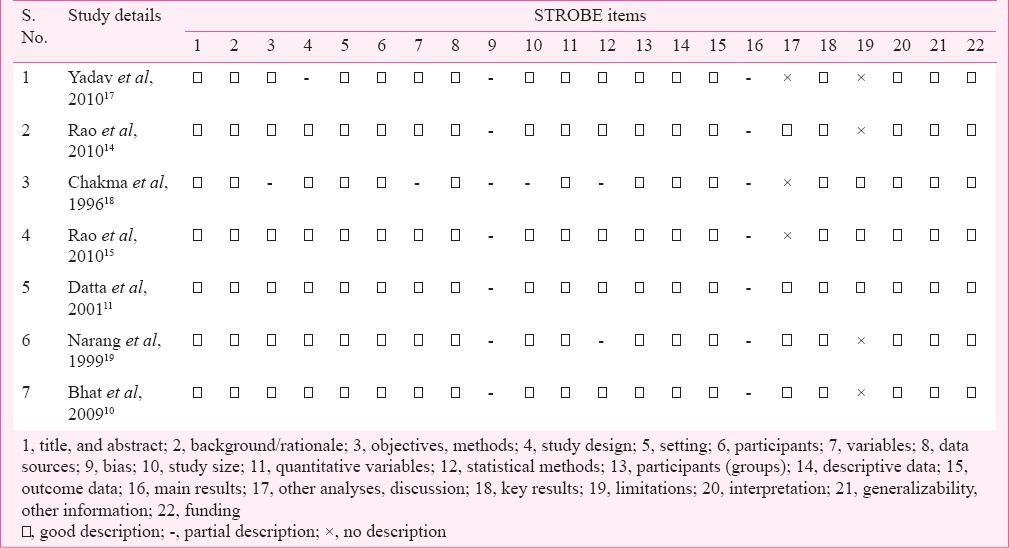
The quality of the reporting of the included studies was assessed using the 22 items recommended by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement20 is shown in Table I. Items fulfilling the STROBE statement were considered positive.
Table I.
Assessment of quality of studies according to STROBE criteria
Data analysis: As the studies were observational in nature, a random effects model was applied21, to account for the possibility of heterogeneity among the studies, which was tested in terms of Cochran's Q statistic which is distributed as a chi-square statistic with k (number of studies) minus 1 degrees of freedom and P<0.1 is considered significant.
Further, the I2 which describes the percentage of variation across studies, along with its 95 % uncertainty intervals (UI) was used to quantify heterogeneity. Power analysis for the effect size was also carried out.
Funnel plots, Begg's test and Egger tests were used to assess the publication bias. A sensitivity analysis by “remove one study” method21 was performed to determine the stability of the analysis. An excel worksheet was used for the calculations.
Results
Study selection and data collection: Two authors (AS and CM), independently carried out the literature search, identified studies, and assessed their eligibility. A total of 20 studies were identified based on the keywords. Two additional studies were identified through a manual search of the retrieved articles’ listed references. Additionally, institutes working with the tribal populations were contacted for TB studies. However, all recommended studies were published and, therefore, already covered by our search. Of the 22 studies, only 12 studies involved TB prevalence surveys of individuals aged 15 yr and above in tribal communities. Of the 10 studies that were not included, four were annual risk of infection studies involving children aged 1-9 yr22,23,24, two were reviews8,16, two surveyed general tribal health25,26, one study only examined the microbiological aspect of TB27, and one was a TB risk factor analysis28. Full texts of the publications were retrieved for the 12 selected studies. These publications were reviewed in-depth and independently by the two authors. Five9,12,13,29,30 of the 12 studies were discarded by both, as these did not adhere to the inclusion criteria. Table II provides details of the studies included in the meta-analysis.
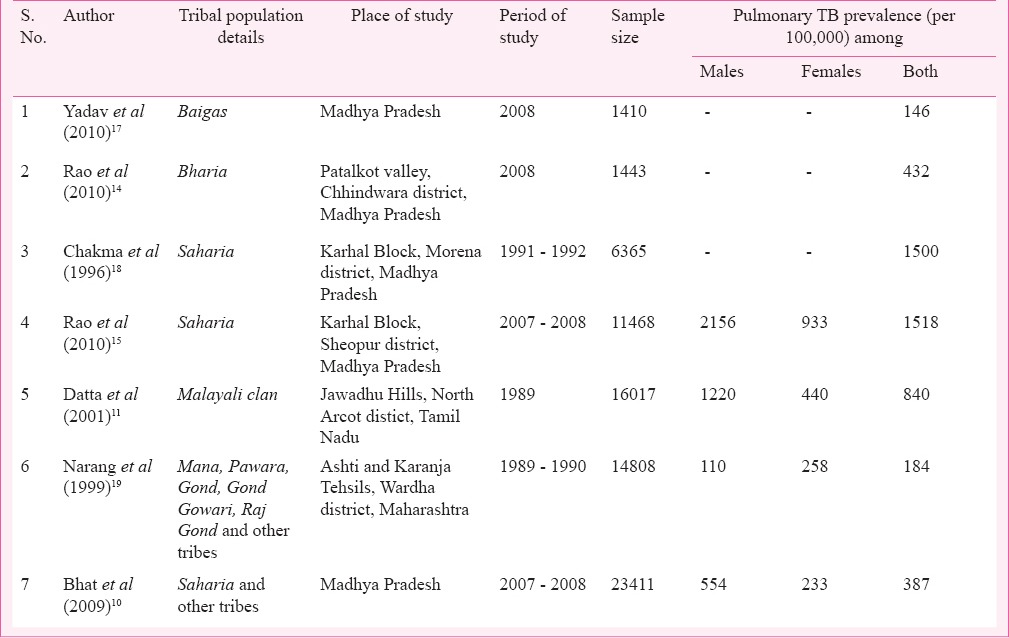
Table II.
Characteristics of the studies included in the meta-analysis
Reasons for exclusion: In a study conducted in the Kashmir valley12, culture tests alone were performed (no smear tests were conducted). Furthermore, the study focused on culture negative individuals with abnormal X-ray findings. The number of culture positive cases was not provided.
In a large scale prevalence study in the Car Nicobar Islands13, only smear tests were performed for detection of TB cases. Culture tests were not done. Similarly, in a study carried out in the Thiruvannamalai district, Tamil Nadu9, only smear examinations were done. In a study in central India29, the targeted population comprised individuals who were symptomatic and voluntarily visited a hospital and those who were identified in prior TB surveys. As this was not a community-based study, it was excluded. In a study in Madhya Pradesh30, no sampling design was followed. The individuals were neither screened for TB symptoms nor X-rayed to assess their sputum eligibility. Sputum samples were randomly collected from individuals in selected communities. As the study did not screen for TB in the targeted community, it was excluded.
Included studies: Characteristics of the selected studies such as targeted population, type of sampling design adopted, community sample size, gender specific and overall TB prevalence per 100,000 population are shown in Table II.
Studies in Madhya Pradesh: There were five TB prevalence studies carried out in this region.
1. In 2008 a TB prevalence survey was conducted in the Madhya Pradesh region, targeting Baigas, one of the primitive tribes that reside in the Baiga Chak area of Dindori district17. Due to logistical constraints, only 25 per cent of the population was surveyed. Five villages were randomly selected to achieve a sample size of 2100 and a complete census was carried out in these villages. All individuals aged 15 years and above were screened for chest symptoms indicative of pulmonary tuberculosis. Of the total population included in the study, 1410 were eligible for screening, of whom 1374 were screened. Of those screened, 115 (8.4%) were chest symptomatic. Two sputum samples were collected from each symptomatic individual. Only two of 115 tested positive based on smear and/or culture testing, translating to a TB prevalence of 146 per 100,000 population. Gender-wise estimate of the TB prevalence was not provided. The study suggested that TB was not a major health problem among the Baigas, but continuous monitoring and implementation of TB control measures were necessary to keep the disease in check.
2. In 2008, a TB prevalence survey was conducted among the Bharia tribes residing in all 12 villages of the Patalkot Valley of the Chindwara district14. A complete census of the population in these villages was carried out and individuals aged 15 years and above were screened for chest symptoms. Of the 2586 individuals in these villages, 1443 were eligible for screenings, of whom 1390 were screened. Of the screened individuals, 92 (6.6%) were found to be chest symptomatic. Two sputum samples were collected from every symptomatic person, resulting in a coverage of 100 per cent. Of these 92, six were found to be positive for AFB, translating to a TB prevalence of 432 per 100,000 population. Gender-wise data were not reported. The study revealed that the TB disease burden among Bharias did not vary from the TB burden among non-tribals estimated in other studies.
3. In 1996, a TB prevalence survey was conducted in 37 villages located in the Karhal block of the Morena district targeting the Saharia tribe (a primitive tribal group)18. These villages were randomly selected based on the probability proportional to size method (PPS). Both tribals (Saharias) and non-tribals residing in the selected villages were included. Of the 11097 individuals (aged 15 years and above) included in the study, 6365 were tribals and 4732 were non-tribals. All eligible individuals were screened for chest symptoms suggestive of TB. Among the tribal group, 445 individuals were chest symptomatic. Two sputum samples (spot and overnight testing) from 436 individuals were collected. Ninety six individuals tested positive for TB (by smear and/or culture tests), translating to a TB prevalence of 1500 per 100,000 for tribals. Gender-wise data have not been reported. Children between three months and nine years underwent tuberculin skin tests, revealing an overall infection rate of 16.9 per cent.
4. Between 2007 and 2008, a community based TB prevalence survey was conducted in the Karhal block of the Sheopur district among the Saharia tribes15. All tribal villages with a predominant tribal population (>80%) were considered for the study. Villages from this pool were randomly selected till the required sample size of 11,000 was achieved. A complete census was carried out in selected villages and all individuals aged 15 years and above were screened for chest symptoms. Two sputum samples were collected from those who were symptomatic or had a previous history of TB treatment. Of the 11468 eligible individuals, 11116 were screened for chest symptoms. Of these, 1269 (11.4%) were found to be chest symptomatic, with males recording a significantly higher rate than females (15.2 and 8.0%, respectively). Sputum samples were obtained from 1268 individuals, resulting in a coverage of 99.9 per cent. Of these, 166 (13.1%) were found to be TB positive by smear and/or culture tests, translating to a TB prevalence of 1518 per 100,000 population. Males had a TB prevalence of 2156 per 100,000, which was significantly higher than that of females (933 per 100,000). There was a positive relationship between age and TB prevalence, with an increase in prevalence from 546 per 100,000 in individuals aged 15-24 yr to 3086 per 100,000 for individuals over 55. This study also reported that there was no improvement in the TB situation for Saharias 15 years after the initial survey was completed, despite the involvement of the National TB Control Programme (NTP) in the region. The study also suggested that the high TB prevalence found among the Saharia tribe in this study needed further investigation, considering that a similar study among the same tribe reported a significantly lower prevalence (387 per 100,000), similar to that of the non-tribal population in the country.10
5. In 2009, another TB prevalence study was carried out targeting the Saharia tribe in Madhya Pradesh10. A multi-stage stratified cluster sampling design was adopted. In the first stage, 25 per cent of districts were selected using systematic sampling. In stage II, 25 per cent of the blocks in these districts were randomly selected. In stage III, the required number of villages (65) was randomly selected using the PPS method. A survey of individuals aged 15 yr and above was carried out in the selected villages and details regarding TB chest symptoms and previous history of TB were elicited. Two sputum samples were collected from persons with chest symptoms or a previous history of TB treatment. Of the 23411 individuals, 22270 were screened for symptoms. Of these, 1770 (7.9%) were chest symptomatic, with males recording a significantly higher rate than females (9.1 and 6.9%, respectively). Sputum samples were collected from 1703 individuals. Of these, 83 tested positive for TB, as confirmed by smear and/or culture tests, translating to a TB prevalence of 387 per 100,000 population. The findings revealed that the TB prevalence among males (554 per 100,000 population) was more than double than that observed for females (233 per 100,000 population). Additionally, the study reported a significant, positive relationship between TB prevalence and age, with an increase in prevalence from 174 per 100,000 population for individuals aged 15-24 yr to 990 per 100,000 population in individuals over 55.
Study in Maharashtra: In 1998, a study was conducted on the prevalence of sputum-positive TB among Ashti and Karanja tahsils in the Wardha district19. Both tribals and non-tribals were surveyed. A total of 46 tribes were included in the survey, with three predominant tribes (Gond, Gond Gawari, and Raj Gonds) constituting 87 per cent of the total tribal population. The remaining population included individuals from Mana and Pawara primitive tribes among others. Of the 14,808 tribals aged 15 yr and above, 2.1 per cent (2.7% of males and 1.5% of females) presented with chest symptoms. These figures were less than those observed for non-tribals (2.1% for males, 1.3% for females, and 1.7% combined). Two sputum samples were collected from each symptomatic individual and a TB prevalence of 184 per 100,000 (confirmed by smear and/or culture test) was calculated after subtracting the figures related to 5-14 yr of age. Females were found to have a significantly lower prevalence (110 per 100,000) than males (257 per 100,000). It was also observed that while predominant Gond tribes had TB prevalence similar to that of the non-tribal population in India (ranging from 100 to 196 per 100,000 population), primitive tribes, namely Mana and Pawara, had significantly higher prevalence (ranging from 612 to 730 per 100,000 population). Additionally, all TB cases in Mana tribes were found among females, while all cases in Pawara tribes were found among males.
Study in Tamil Nadu: In 1989, a TB prevalence study was implemented targeting a Malayali tribal community in the North Arcot District of Tamil Nadu in the Jawadhu Hills11. A stratified simple random sample selected from 24 panchayats formed the study population. All villages in the selected panchayats were enumerated. A total of 16017 individuals aged 15 years and above were screened for chest symptoms and also X-rayed. Of these, 3347 (20.9%) had chest symptoms or abnormal radiological findings (24.6% for males and 17.0% females). Two sputum samples were collected from 3301 individuals resulting in a coverage of 99 per cent. One hundred and twenty six tested positive for TB (using smear and/or culture tests), translating to a TB prevalence of 840 per 100,000 population. Drug susceptibility tests were also conducted for 78 culture positive cases. Eighty eight per cent were sensitive to all three drugs: isoniazid, rifampicin, and streptomycin. Twelve percent were resistant to isoniazid and 1.6 per cent were resistant to both isoniazid and rifampicin. The study also documented the influence of screening methods on prevalence estimates, as both symptom screenings and X-rays were carried out. TB detection was more accurate when both methods were employed. Additionally, age and gender specific patterns were reported. There was a significantly higher TB prevalence observed for males (1220 per 100,000) than for females (440 per 100,000). A positive relationship between TB prevalence and age was also found, with an increase in prevalence from 260 per 100,000 individuals aged 15-24 to 1500 per 100,000 for individuals above 55.
Meta-analysis:
Overall estimate - The pooled estimate, based on the random effects model, was 703 per 100,000 population with a 95% CI of 386-1011. The heterogeneity measure of Cochran's Q of 11.0 was significant, resulting in a P value of 0.08 and an I2 of 48 per cent (with a 95% UI of 0-78%). A power analysis of the effect size by the random effects model showed this study had 51 per cent power. A forest plot with the pooled estimated (marked as a diamond with a vertical dotted line) with a 95% CI, as obtained from the random effects model, is displayed in Fig. 1. Also depicted are the TB prevalence estimates from the individual studies (marked as circles) along with their 95% CIs. Our calculations indicated that 48 per cent of the variation observed in the pooled estimate was due to heterogeneity among the studies, suggesting that there were inconsistencies across the studies included in this analysis. Subgroup analyses to determine possible causes of heterogeneity and publication bias could not be performed, given the limited number of studies.
Fig. 1.
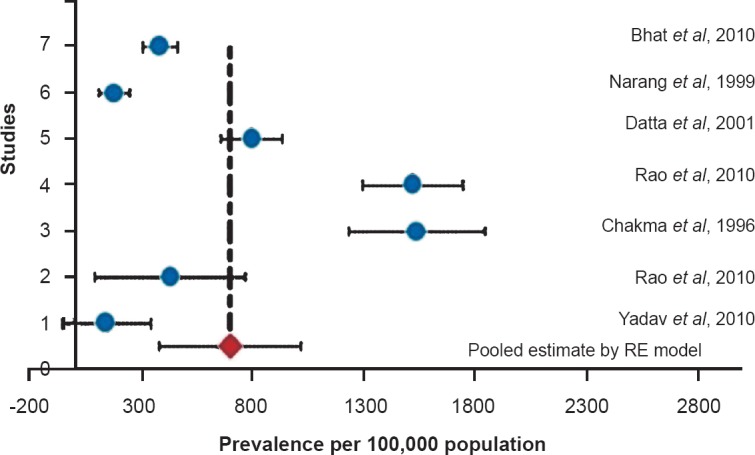
Forest plot of meta-analysis of the TB prevalence among tribals based on seven studies.
Gender-wise estimates - Of the seven studies, four provided gender-wise TB prevalence rates. Estimated TB prevalence based on the random effects model indicated that females had a lower prevalence (398 per 100,000 with a 95% CI of 167–628) than males (999 per 100,000 with a 95% CI of 444 -1553). However, the heterogeneity statistic, I2, was 53 and 54 per cent for females and males, respectively, further suggesting inconsistencies across the studies.
Publication bias - An attempt was made to assess the publication bias, however, the funnel plot method and other tests were underpowered due to small number of studies. Hence, we could not assess the publication bias.
Sensitivity analysis - A sensitivity analysis was performed, which indicated that when a particular study was removed, the resulting pooled estimate still fell within the 95% CI of the original pooled estimate. Though this suggested the stability of our results, heterogeneity among studies persisted. The sensitivity analysis is graphically depicted in Fig. 2, where the vertical dotted line is the actual pooled estimate we calculated using the random effects model along with its 95% CI. Also displayed in parentheses is the heterogeneity measure, I2 obtained after the removal of a study.
Fig. 2.
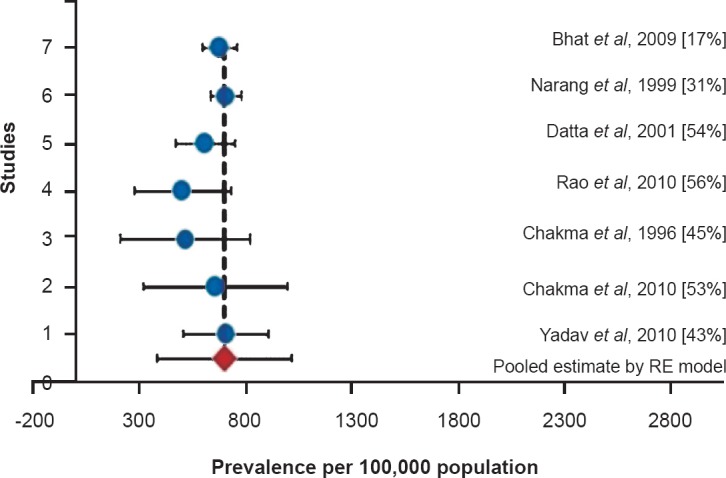
Sensitivity analysis showing the changes in pooled estimate along with the hetetogeneity measure when that study is removed. Percentage given in parentheses are I2 values.
Discussion
This meta-analysis pointed to a pooled pulmonary TB prevalence estimate of 703 per 100,000 for the tribal population which was significantly higher than that estimated for India (256 per 100,000)31. This estimate greatly differs from the RNTCP annual report estimation of only 80 smear positive cases per 100,000 tribal population (RNTCP report, 2011, unpublished). This variance may be attributed to methodological differences in determining the prevalence of TB. The studies reviewed here adopted active case finding, entailing large-scale screening and testing of individuals in tribal communities as compared to passive case finding adopted in RNTCP. Taking into consideration the limited number of studies among the tribal population, this estimate was higher than the culture positive TB prevalence estimates among the non-tribal populations in a rural district of Bangalore32 (Nelamangala: 152 per 100,000 population) and Tamil Nadu33 (Thiruvallur: 388 per 100,000 population). This pooled estimate however, needs to be treated with caution, considering the level of heterogeneity across the studies. While I2 statistic indicated moderate heterogeneity, Q statistic demonstrated a significant heterogeneity among studies, indicating that there were differences among the studies, rather than due to chance. The possible reason for a power of 51 per cent for this analysis could be the small number of studies. Heterogeneity could be due to variations in study characteristics including (i) the time period when the studies took place (between 1991 and 2010) (ii) areas covered (particularly for the Saharia tribe) (iii) methodological approach (two studies did a complete enumeration of the study population, while the other studies reported multi-stage cluster or stratified random sampling procedures for the surveys), and (iv) the composition of the studied population (only one study19 reported the tribal composition of the targeted community).
The variance could also be attributed to the influence of various screening methods adopted to assess the TB prevalence rates. In the study conducted in Tamil Nadu11, it was found that the TB prevalence was underestimated when symptom screenings or X-rays alone were performed. When both methods were used, there was a 25 per cent increase in detection of pulmonary TB. Also, in this study a drug susceptibility testing was performed, revealing that approximately 12 per cent of TB cases were isoniazid resistant and 1.6 per cent were both isoniazid and rifampicin resistant. These findings suggest the need for a standardized method of TB and resistant TB screening to ensure timely interventions.
This review has also provided insight into some of the socio-demographic patterns of TB among the tribal populations studied. Two studies indicated that TB prevalence among males was higher than that observed among females10,15. These studies have also reported that the prevalence of chest symptomatic was higher for males than for females, with one study reporting prevalence of chest symptomatic among males being twice of what was observed in females (554 per and 233 per 100,000 respectively)10. Higher TB prevalence rates in men than in women have been reported among the general population also. This has been attributed to alcohol use/drugs, smoking, work environment and differences in exposure, risk of infection, and progression from infection to disease34,35,36,37,38,39. It has also been observed that TB incidence in males and females differ significantly from the age of 25 yr and that men are more likely than women to develop the disease from this age40. These findings could also be applicable to understanding the higher prevalence rates of TB among the tribal male population.
Some of the studies in this analysis reported an age dependent trend, with older individuals being more at risk10,11,15. These patterns are similar to those observed in the non-tribal population10,18,41,42,43,44,45,46,47,48. This may be because older people are more likely to be under diagnosed and be infected with the disease from a latent infection acquired years or decades ago. Other possible issues may be attributed to delays in seeking care49 low socio-economic status, poor nutrition and metabolism and co-infection or previous disease. The observed high prevalence of pulmonary TB among the older age groups in tribal population needs to be further understood.
The studies included in this analysis were limited in number and target only a few (around seven) of the numerous tribal groups (over 600) found throughout the country1. Further, five of the seven studies included were based on the tribal population from the State of Madhya Pradesh alone. Therefore, the pooled estimate does not accurately reflect the pulmonary TB prevalence in the tribal population as a whole and needs to be treated with caution. Due to this limited number it was not possible to perform an assessment of the publication bias (an important measure for any systematic review or meta-analysis) as the relevant tests were underpowered due to small number of studies, or a subgroup analysis, necessary to identify the specific reasons for heterogeneity among the studies.
In conclusion, our findings indicate a large variation in pulmonary TB prevalence estimates among different studies and limited coverage of the tribal population, highlighting the imperative need to comprehensively and accurately assess the TB burden among the tribal population in India. The findings also suggest the need for a standardized method of TB and resistant TB screening to ensure timely interventions. Methodological strategies need to be considered to reach the unreached and obtain a true estimation of the disease burden. Further, it is critical to understand the health-seeking behaviours of tribal people, especially of chest symptomatic, to increase their access to healthcare services. The potential role of the tribal community in TB control activities, including the identification and referral of symptomatic for care, also needs to be explored.
Acknowledgment
The authors acknowledge Priya Govindaraj (Intern student of MPH, Columbia University) and Senthanro Ovung (Research Assistant, NIRT) for assisting in editing this manuscript.
References
- 1.Government of India. Tribal Profile at a Glance - May 1. 2013. [accessed on November 1, 2014]. available from: http://tribal.nic.in/WriteReadData/CMS/Documents/201306061001146927823STProfileataGlance.pdf .
- 2.Government of India. The National Tribal Policy (Draft): A Policy for the Scheduled Tribes of India 2006. [accessed on November 1, 2014]. Available from: http://www.legalpundits.com/Content_folder/tribalpolicy.pdf .
- 3.Basu SK. A health profile of tribal India. Health Millions. 1994;2:12–4. [PubMed] [Google Scholar]
- 4.Mysore: Proceedings of the National Seminar on Tribal Health in India: Issues & Challenges 2013; 2013. Feb 11-12, Foundation of Healthcare Technologies Society (FHTS) [Google Scholar]
- 5.Shah A, Sah DC. Poverty among Tribals in South West Madhya Pradesh: has anything changed over time? J Hum Dev. 2004;5:249–63. [Google Scholar]
- 6.Subramanian SV, Davey Smith G, Subramanyam M. Indigenous health and socioeconomic status in India. PLoS Med. 2006;3:e421. doi: 10.1371/journal.pmed.0030421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agarwal SP, Chauhan LS. New Delhi: Directorate General of Health Services/Ministry of Health and Family Welfare; 2005. Tuberculosis control in India. [Google Scholar]
- 8.Chakraborty AK. Epidemiology of tuberculosis: current status in India. Indian J Med Res. 2004;120:248–76. [PubMed] [Google Scholar]
- 9.Balasubramanian R, Sadacharam K, Selvaraj R, Xavier T, Gopalan BN, Shanmugam M, et al. Feasibility of involving literate tribal youths in tuberculosis case-finding in a tribal area in Tamil Nadu. Tuberc Lung Dis. 1995;76:355–9. doi: 10.1016/s0962-8479(05)80036-x. [DOI] [PubMed] [Google Scholar]
- 10.Bhat J, Rao VG, Gopi PG, Yadav R, Selvakumar N, Tiwari B, et al. Prevalence of pulmonary tuberculosis amongst the tribal population of Madhya Pradesh, central India. Int J Epidemiol. 2009;38:1026–32. doi: 10.1093/ije/dyp222. [DOI] [PubMed] [Google Scholar]
- 11.Datta M, Radhamani MP, Sadacharam K, Selvaraj R, Rao DL, Rao RS, et al. Survey for tuberculosis in a tribal population in North Arcot District. Int J Tuberc Lung Dis. 2001;5:240–9. [PubMed] [Google Scholar]
- 12.Mayurnath S, Anantharaman DS, Baily GV, Radhamani MP, Vallishayee RS, Venkataraman P, et al. Tuberculosis prevalence survey in Kashmir valley. Indian J Med Res. 1984;80:129–40. [PubMed] [Google Scholar]
- 13.Murhekar MV, Kolappan C, Gopi PG, Chakraborty AK, Sehgal SC. Tuberculosis situation among tribal population of Car Nicobar, India, 15 years after intensive tuberculosis control project and implementation of a national tuberculosis programme. Bull World Health Organ. 2004;82:836–43. [PMC free article] [PubMed] [Google Scholar]
- 14.Rao VG, Bhat J, Yadav R, Gopi PG, Selvakumar N, Wares DF. Prevalence of pulmonary tuberculosis among the Bharia, a primitive tribe of Madhya Pradesh, central India. Int J Tuberc Lung Dis. 2010;14:368–70. [PubMed] [Google Scholar]
- 15.Rao VG, Gopi PG, Bhat J, Selvakumar N, Yadav R, Tiwari B, et al. Pulmonary tuberculosis: a public health problem amongst the Saharia, a primitive tribe of Madhya Pradesh, Central India. Int J Infect Dis. 2010;14:e713–6. doi: 10.1016/j.ijid.2010.02.2243. [DOI] [PubMed] [Google Scholar]
- 16.Rao VG, Gopi PG, Yadav R, Sadacharam K, Bhat J, Subramani R, et al. Tuberculous infection in Saharia, a primitive tribal community of Central India. Trans R Soc Trop Med Hyg. 2008;102:898–904. doi: 10.1016/j.trstmh.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Yadav R, Rao VG, Bhat J, Gopi PG, Selvakumar N, Wares DF. Prevalence of pulmonary tuberculosis amongst the Baigas - a primitive tribe of Madhya Pradesh, Central India. Indian J Tuberc. 2010;57:114–6. [PubMed] [Google Scholar]
- 18.Chakma T, Rao PV, Pall S, Kaushal LS, Datta M, Tiwary RS. Survey of Pulmonary tuberculosis in a primitive tribe of Madhya Pradesh. Indian J Tuberc. 1996;43:85–9. [Google Scholar]
- 19.Narang P, Tyagi NK, Mendiratta DK, Jajoo UN, Bharambhe MS, Nayar S. Prevalence of sputum-positive pulmonary tuberculosis in tribal and non-tribal populations of the Ashti and Karanja tahsils in Wardha district, Maharashtra State, India. Int J Tuberc Lung Dis. 1999;3:478–82. [PubMed] [Google Scholar]
- 20.Elm EV, Altman DG, Egger M, Pocock SJ, Gotzche PC, Vandenbroucke JP. Strengthening the reporting of observational stuides in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DerSimonian R, Laired N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 22.Chadha VK, Banerjee A, Ibrahim M, Jaganatha PS, Kumar P. Annual risk of tuberculous infection in Khammam a tribal district of Andhra Pradesh. J Commun Dis. 2003;35:198–205. [PubMed] [Google Scholar]
- 23.Rao VG, Gopi PG, Yadav R, Subramani R, Bhat J, Anvikar AR, et al. Annual risk of tuberculosis infection among tribal population of central India. Trop Med Int Health. 2008;13:1372–7. doi: 10.1111/j.1365-3156.2008.02152.x. [DOI] [PubMed] [Google Scholar]
- 24.Yadav R, Rao VG, Bhat J, Gopi PG, Wares DF. Annual risk of tuberculosis infection among the tribal children of Jhabua, Madhya Pradesh. Indian Pediatr. 2011;48:43–5. [PubMed] [Google Scholar]
- 25.Haddad S, Mohindra KS, Siekmans K, Mak G, Narayana D. “Health divide” between indigenous and non-indigenous populations in Kerala, India: population based study. BMC Public Health. 2012;12:390. doi: 10.1186/1471-2458-12-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerketta AS, Bulliyya G, Babu BV, Mohapatra SS, Nayak RN. Health status of the elderly population among four primitive tribes of Orissa, India: a clinico-epidemiological study. Z Gerontol Geriatr. 2009;42:53–9. doi: 10.1007/s00391-008-0530-2. [DOI] [PubMed] [Google Scholar]
- 27.Bhat J, Selvakumar N, Rao VG, Gopi PG, Yadav R, Wares DF. Yield of culture of Mycobacterium tuberculosis complex in sputum samples transported from tribal areas. Int J Tuberc Lung Dis. 2011;15:478–82. doi: 10.5588/ijtld.10.0234. [DOI] [PubMed] [Google Scholar]
- 28.Rao VG, Yadav R, Bhat J, Tiwari BK, Bhondeley MK. Knowledge and attitude towards tuberculosis amongst the tribal population of Jhabua, Madhya Pradesh. Indian J Tuberc. 2012;59:243–8. [PubMed] [Google Scholar]
- 29.Raj P, Prakash R, Mishra G, Singh TD, Poojary S, Mehra NK, et al. Prevalence of smear-positive pulmonary tuberculosis in different ethnic groups in India: evaluation of public health. Public Health. 2011;126:295–9. doi: 10.1016/j.puhe.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 30.Sharma PR, Jain S, Bamezai RNK, Tiwary PK. Increased prevalence of pulmonary tuberculosis in male adults of Sahariya tribe of India: A revised survey. Indian J Community Med. 2010;35:267–71. doi: 10.4103/0970-0218.66887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Annual Status Report. New Delhi: RNTCP; 2013. Revised National Tuberculosis Control Programme (RNTCP). Zero TB deaths, Stop TB: In my lifetime: TB India 2013; p. 225. [Google Scholar]
- 32.Chadha VK, Kumar P, Anjinappa SM, Singh S, Narasimhaiah S, Joshi MV, et al. Prevalence of pulmonary tuberculosis among adults in a rural sub-district of South India. PLoS One. 2012;7:e42625. doi: 10.1371/journal.pone.0042625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kolappan C, Subramani R, Radhakrishna S, Santha T, Wares F, Baskaran D, et al. Trends in the prevalence of pulmonary tuberculosis over a period of seven and half years in a rural community in south India with DOTS. Indian J Tuberc. 2013;60:168–76. [PubMed] [Google Scholar]
- 34.Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43000 adult male deaths and 35000 controls. Lancet. 2003;362:507–15. doi: 10.1016/S0140-6736(03)14109-8. [DOI] [PubMed] [Google Scholar]
- 35.Harrison PF, Howson CP. The life span approach to female morbidity and mortality: an application to female health in sub-Saharan Africa. Curr Issues Public Health. 1996;2:226–31. [PubMed] [Google Scholar]
- 36.Holmes CB, Hausler H, Nunn P. A review of sex differences in the epidemiology of tuberculosis. Int J Tuberc Lung Dis. 1998;2:96–104. [PubMed] [Google Scholar]
- 37.Jimenez-Corona ME, Garcia-Garcia L, DeRiemer K, Ferreyra-Reyes L, Bobadilla-del-Valle M, Cano-Arellano B, et al. Gender differentials of pulmonary tuberculosis transmission and reactivation in an endemic area. Thorax. 2006;61:348–53. doi: 10.1136/thx.2005.049452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uplekar MW, Rangan S, Weiss MG, Ogden J, Borgdorff MW, Hudelson P. Attention to gender issues in tuberculosis control. Int J Tuberc Lung Dis. 2001;5:220–4. [PubMed] [Google Scholar]
- 39.Ursov IG, Leonov OG. The social profile and medical characteristics of a first-time registered patient with tuberculosis of the respiratory organs. Probl Tuberk. 1990;5:14–8. [PubMed] [Google Scholar]
- 40.Stival A, Chiappini E, Montagnani C, Orlandini E, Buzzoni C, Galli L, et al. Sexual dimorphism in tuberculosis incidence: children cases compared to adult cases in Tuscany from 1997 to 2011. PLoS One. 2014;9:e105277. doi: 10.1371/journal.pone.0105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baily GV. Tuberculosis prevention Trial, Madras. Indian J Med Res. 1980;72(Suppl):1–74. [PubMed] [Google Scholar]
- 42.Balasubramanian R, Garg R, Santha T, Gopi PG, Subramani R, Chandrasekaran V, et al. Gender disparities in tuberculosis: report from a rural DOTS programme in south India. Int J Tuberc Lung Dis. 2004;8:323–32. [PubMed] [Google Scholar]
- 43.Gopi PG, Subramani R, Radhakrishna S, Kolappan C, Sadacharam K, Devi TS, et al. A baseline survey of the prevalence of tuberculosis in a community in south India at the commencement of a DOTS programme. Int J Tuberc Lung Dis. 2003;7:1154–62. [PubMed] [Google Scholar]
- 44.Gothi GD, Chakraborty AK, Nair AS, Ganapathy KT, Banerjee GC. Prevalence of tuberculosis in a South Indian district - twelve years after initial survey. Indian J Tuberc. 1979;26:121–4. [Google Scholar]
- 45.Gothi GD, Narayan R, Nair SS, Chakraborty AK, Srikantaramu N. Estimation of prevalence of bacillary tuberculosis on the basis of chest X-ray and/or symptomatic screening. Indian J Med Res. 1976;64:1150–9. [PubMed] [Google Scholar]
- 46.Pamra SP, Prasad G, Mathur GP. Causes of failure of domiciliary chemotherapy in pulmonary tuberculosis. Tubercle. 1973;54:185–94. doi: 10.1016/0041-3879(73)90023-8. [DOI] [PubMed] [Google Scholar]
- 47.Subramani R, Radhakrishna S, Frieden TR, Kolappan C, Gopi PG, Santha T, et al. Rapid decline in prevalence of pulmonary tuberculosis after DOTS implementation in a rural area of South India. Int J Tuberc Lung Dis. 2008;12:916–20. [PubMed] [Google Scholar]
- 48.Tuberculosis Centre, New Delhi. Study of epidemiology of TB in an urban population of Delhi: Report on 30 years follow-up. Indian J Tuberc. 1999;36:113–24. [Google Scholar]
- 49.Charles N, Thomas B, Watson B, Raja Sakthivel M, Chandrasekeran V, Wares F. Care seeking behavior of chest symptomatics: a community based study done in South India after the implementation of the RNTCP. PLoS One. 2010;5:e12379. doi: 10.1371/journal.pone.0012379. [DOI] [PMC free article] [PubMed] [Google Scholar]


