Abstract
Background & objectives:
The Revised National Tuberculosis Control Programme (RNTCP) provides free diagnostic and treatment services to all tuberculosis (TB) patients registered under it. Equitable access, implying a preference for the most hard-to-reach groups particularly for tribal areas, is a major concern for RNTCP. This study was conducted to assess the performance of RNTCP in terms of case detection and cure rates in areas dominated by tribal groups in India.
Methods:
We used the RNTCP data collected by the Central TB Divison, Government of India. RNTCP has a systematic monitoring mechanism which tracks the outcome of every patient put on treatment. There is a standardized recording and reporting structure in place; indicators are monitored regularly at every level of the health system; and regular supervision ensures quality of the Programme. The main indicators include the number of cases diagnosed and the percentage of patients who are successfully treated. These indicators were used to assess the RNTCP performance in tribal areas.
Results:
We observed a poor performance in terms of case detection rate (CDR) in tribal and backward districts as compared with other districts in India. Among tribal districts 53 per cent in 2010, 45 per cent in 2011 and 56 per cent in 2012 had CDR of new smear positive <70%. It was also observed that 26 per cent of tribal dominated districts had CDR of <51 per cent in 2012. More than 50 per cent of tribal districts were not able to achieve more than 85 per cent of cure rate.
Interpretation & conclusions:
The findings of this study suggested that the overall RNTCP performance in tribal areas was not optimal, and the target of >85 per cent of core rate was achieved by less than half of the tribal districts.
Keywords: DOTS, India, programme performance, RNTCP, tribal, tuberculosis
In early 1990s it was shown that tuberculosis declined if socio-economic conditions improved1. It has been convincingly demonstrated in practice that TB can be controlled in almost any socio-economic circumstances2,3. A recent WHO report showed that TB incidence rates declined only by two per cent per year in all six WHO regions4. Global concerted efforts over the last two decades have helped make remarkable progress in global TB control. It has also been shown that TB related Millennium Development Goal targets can be achieved in advance, and the global TB epidemic has now been halted and begun to reverse5. However, the persisting burden of 8.7 million new TB cases and 1.4 million TB deaths annually, and the slow decline of TB incidence at about two per cent a year, demand for an enhancement of current efforts. Enhanced action should also address the enormous socio-economic burden that the poor people have to bear as a consequence of the disease6. In the absence of an effective vaccine, diagnosing and treating active TB cases has been the principal public health strategy for TB control. Under the DOTS strategy, countries strived to meet the recommended targets of detecting 70 per cent of the estimated cases and curing 85 per cent of them7. The DOTS strategy consists of political commitment, laboratory-based diagnosis, regular supply of short-course anti-TB drugs, direct observation of treatment, and systematic monitoring and accountability.
Under the Revised National TB Control Programme (RNTCP) in India, diagnostic and treatment services are integrated within the general health system. Now RNTCP is an integral part of the National Rural Health Mission (NRHM). For quality diagnosis, designated microscopy centres have been established for every one lakh population in the general areas and for every 50,000 population in the tribal, hilly and difficult areas8.
The TB prevalence surveys conducted among Saharia tribes showed high prevalence rate in that population with poor access to health care services9,10. Equitable access with a preference for the most hard-to-reach groups such as in tribal areas has led the RNTCP to scale up TB control activities particularly for the tribal population. In this study an attempt was made to assess the performance of RNTCP in terms of case detection and cure rates in areas dominated by tribal groups.
Material & Methods
The data of all TB patients who were diagnosed and registered for treatment under the RNTCP during a period of 2010 to 2012 were used for this study. The total districts reported under RNTCP in 2010 were 658, 662 in 2011 and 674 in 2012. Of the total 674 districts reported in 2012, 12 per cent were classified as tribal, 17 per cent as backward and 70 per cent other districts. The tribal districts in India were classified as per RNTCP norms (those district had >50% tribal population)11. Nagaland had highest number of tribal districts (11) followed by Arunachal Pradesh (10), Odisha (8), Mizoram (8), Meghalaya (6), Manipur (6), Jharkhand(6), Madhya Pradesh (5), Chhattisgarh (5) and Gujarat (3).
Data collection and analysis: The RNTCP performance indicators were collected from the RNTCP annual reports of 2006 to 201212 and entered in the Excel sheet. Data were analysed using Statistical Package for Social Sciences (SPSS/PC version 20.0; SPSS Inc., Chicago, IL, USA) package. The performance of the Revised National Tuberculosis Control Programme is presently being monitored on the basis of new smear positive (NSP) treatment success rate and new smear positive case detection rates (CDR). These output indicators were used for the present analysis. In univariate analysis, the frequency distribution of districts by their performance was done. Trend analysis was performed to find out the Programme performance over a period of tribal areas. Chi square test was used to compare the performance of RNTCP in tribal and non-tribal areas.
Results
Smear positive case detection rate: In India the annual new smear sputum positive (NSP) case detection rate in 43 per cent of districts in 2010 and 2011, 47 per cent in the year 2012 had ≤70 per cent CDR. The proportion of districts that had low CDR was almost significantly similar in all categories (backward, tribal and others) during 2010 and 2012. Among tribal districts 53 per cent in 2010, 45 per cent in 2011 and 56 per cent in 2012 had NSP CDR of ≤70 per cent (Table I). The districts CDR below the expected level was similar in tribal and backward districts and this was significantly lower as compared to other districts (OR 1.9 in 2011; 1.8 in 2012; P<0.05). It was also observed that 27 per cent of tribal dominated districts had CDR of <51 per cent in 2012 (Fig. 1).
Table 1.
Comparison of annual smear positive case detection rate in districts dominated with different communities

Fig. 1.
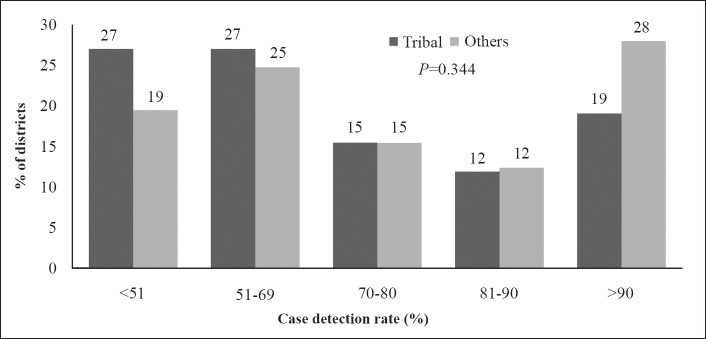
Comparison of case detection rate in tribal dominated districts with other districts in 2012.
Cure rate: Table II shows the cure rate of new smear positive patients treated during 2010 to 2012. It was observed that over a period more than 50 per cent of tribal districts were not able to achieve more than 85 per cent of cure rate which is the expected level under RNTCP. However, cure rates observed in tribal districts were better as compared with backward districts. It was also observed that 39 per cent of tribal dominated districts had cure rate of <81 per cent in 2012 (Fig. 2).
Table II.
Comparison of cure rate in districts dominated with different communities
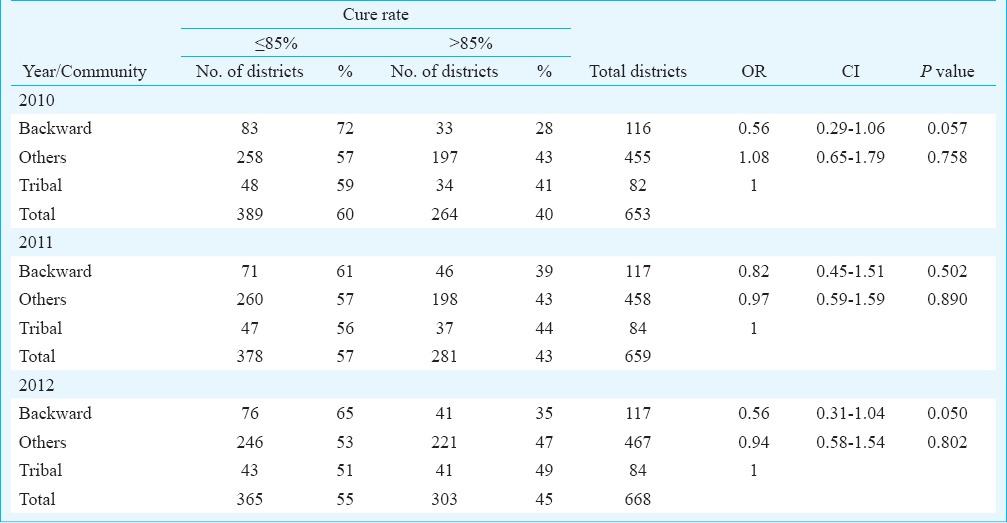
Fig. 2.

Comparison of cure rate in tribal dominated districts with other districts in 2012.
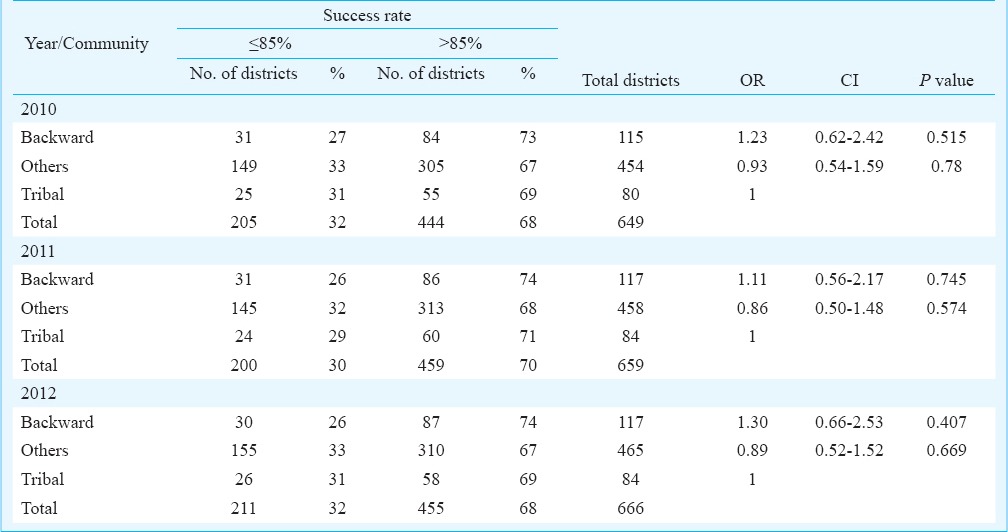
Success rate: One third of the districts in India had ≤85 per cent of success rate during 2010 to 2012. Among tribal districts one fourth districts had ≤85 per cent of success rate. Over a period the performance in terms of success rate was almost similar in all districts (Table III).
Table III.
Comparison of success rate in districts dominated with different communities
Discussion
The major finding of this study was that around half of the districts in India were detecting ≤70 per cent of estimated cases of TB in the community. The reasons for less than 75 per cent new smear positive CDR in inter districts comparison (Kinnour, Chamba) were due to the tribal areas and difficult geographical locations with shortage of medical human resource13. It is extremely important for TB control programme to focus on early and complete detection of all TB cases including smear positive and smear negative TB cases. This means that more attention is to be paid on the processes involved in case detection and case holding and strategies to ensure that all TB patients have access to early case detection and effective treatment facilities particularly in tribal and backward districts.
TB cure rate is most important indicator to evaluate the effectiveness of a TB control programme. The main goal of RNTCP is to achieve 85 per cent cure rate among new smear positive patients. By achieving a high cure rate, the rate of transmission of TB in the community will reduce. This will result in a decrease in TB incidence in younger age group and gradually in older age group14. Overall the performance of RNTCP in all India is satisfactory with respect to the programme indicators15. This implies that DOTS strategy is implemented effectively in this country. However, in the present study, 65 per cent of backward districts, 51 per cent tribal districts and 53 per cent of other districts reported cure rate of ≤85 per cent in 2012. In clinical trials, cure rates above 90 per cent have been documented16; the treatment success rate among smear-positive cases of pulmonary TB reported to WHO reached 87 per cent at the global level in 200917. Current results suggest that cure rate remains lower than expected in more than half of the districts. There is a need to apply successful experiences or generic models of service delivery to the tribal and backward areas to improve cure rate18.
This study was not aimed to provide the reasons for not achieving high case detection and cure rate in tribal dominated districts. The critical factors for poor case detection and cure rate may be due to low prevalence of TB in these areas. It is difficult to interpret whether this poor performance was due to activities of RNTCP. This aspects needs to be studied further.
In conclusion, the findings of this study indicated that the existing service delivery strategy was not sufficient to improve TB control in certain tribal and backward districts. More than half of the tribal districts could not achieve a cure rate of >85 per cent. There is a need to focus specifically on improving the case detection and cure rate in the tribal dominated areas.
Acknowledgment
The authors acknowledge Dr Neeru Singh, Director, NIRTH, Jabalpur for encouragement and support, the Central TB Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, New Delhi, for providing data, and thank Ms Preeti Tiwari, Shrimati Priyashri Tiwari Pandey and Ms Sneha Patel for data entry and cleaning.
References
- 1.Frieden TR. Tuberculosis control and social change. Am J Public Health. 1994;84:1721–3. doi: 10.2105/ajph.84.11.1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frieden TR, Fujiwara PI, Washko RM, Hamburg MA. Tuberculosis in New York City - turning the tide. New Engl J Med. 1995;333:229–33. doi: 10.1056/NEJM199507273330406. [DOI] [PubMed] [Google Scholar]
- 3.Marrero A, Caminero JA, Rodriguez R, Billo NE. Towards elimination of tuberculosis in a low-income country: the experience of Cuba, 1962-97. Thorax. 2000;55:39–45. doi: 10.1136/thorax.55.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO/HTM/TB/2013.11. Geneva: WHO; 2013. World Health Organization (WHO). Global tuberculosis report 2013. [Google Scholar]
- 5.WHO/HTM/TB/2012.6. Geneva: WHO; 2012. World Health Organization (WHO). Global tuberculosis report 2012. [Google Scholar]
- 6.Lonnroth K, Castro KG, Chakaya JM, Chauhan LS, Floyd K, Glaziou P, et al. Tuberculosis control and elimination 2010-50: cure, care, and social development. Lancet. 2010;375:1814–29. doi: 10.1016/S0140-6736(10)60483-7. [DOI] [PubMed] [Google Scholar]
- 7.New Delhi: Central TB Division, Directorate General of Health Services. Ministry of Health and Family Welfare; 2000. Managing the revised national tuberculosis control programme in your area: a training course-Modules 1-4; pp. 5–10. [Google Scholar]
- 8.Rao VG, Gopi PG, Yadav R, Sadacharam K, Bhat J, Subramani R, et al. Tuberculosis infection in Saharia, a primitive tribal community of Central India. Trans R Soc Trop Med Hyg. 2008;102:898–904. doi: 10.1016/j.trstmh.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Rao VG, Bhat J, Yadav R, Gopi PG, Selvakumar N, Wares DF. Prevalence of pulmonary tuberculosis among the Bharia, a primitive tribe of Madhya Pradesh, Central India. Int J Tuberc Lung Dis. 2010;14:368–70. [PubMed] [Google Scholar]
- 10.Yadav R, Rao VG, Bhat J, Gopi PG, Selvakumar N, Wares DF. Prevalence of pulmonary tuberculosis among the Baigas - a primitive tribe of Madhya Pradesh, Central India. Indian J Tuberc. 2010;57:114–6. [PubMed] [Google Scholar]
- 11.New Delhi: RNTCP Status Report, Central TB Division, DGHS; 2007. Central TB Division, Directorate General of Health Services (DGHS) p. 105. [Google Scholar]
- 12.New Delhi: RNTCP Status Reports; [accessed on April 20, 2015]. Central TB Division, Directorate General of Health Services. Available from: http://www.tbcindia.nic.in/documents . [Google Scholar]
- 13.Gupta SN, Gupta N, Gupta S. Surveillance data analysis of Revised National Tuberculosis Control Program of Kangra, Himachal Pradesh. J Family Med Prim Care. 2013;2:250–5. doi: 10.4103/2249-4863.120730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Venkatachalappa BV, Nagaraju S. Performance of Revised National Tuberculosis Control Programme in Rajasthan and Tamil Nadu during 2nd quarter 2001 to 1st quarter 2002. NTI Bull. 2003;39:36–42. [Google Scholar]
- 15.New Delhi: Central TB Division, DGHS, Ministry of Health & Family Welfare; 2014. Central TB Division, Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare. RNTCP status report: TB India 2014; p. 51. [Google Scholar]
- 16.HO/HTM/TB/2011.16. Geneva: WHO; 2011. World Health Organization (WHO). Global tuberculosis control: WHO report 2011. [Google Scholar]
- 17.Geneva: WHO; 2014. World Health Organization (WHO). Making fair choices on the path to universal health coverage. Final report of the WHO Consultative Group on Equity and Universal Health Coverage. [Google Scholar]
- 18.Addlakha R, Seeberg J, editors. Accessing TB services in a tribal district. Delhi: DANTB; 2005. Danish Assistance to the Revised National Tuberculosis Control Programme (DANTB) The Malkangiri Project, Orissa. [Google Scholar]


