Abstract
Background:
Glomus tumors are benign hamartomas arising from the glomus body, mostly occurring in the subungual region of the digits. A triad of excruciating pain, localized tenderness and cold sensitivity is the key to diagnosing these tumors. Two surgical approaches are described in the literature for excision of subungual glomus tumors-transungual and periungual. We reviewed retrospectively the results of subungual glomus tumors of the hand treated by transungual excision.
Materials and Methods:
Twelve patients (9 females and 3 males) with histopathologically confirmed subungual glomus tumors of the hand were treated by transungual excision at our institute. The mean age of the patients was 40.5 years (range 28–63 years). All patients presented with pain in the nail bed and cold sensitivity. A bluish-brown discoloration was present in 6 patients. Love's pin test was positive in all and Hildreth's test was positive in 8 patients. The mean duration of followup was 38 months (range 8–72 months).
Results:
All patients had complete pain relief. There was no new nail deformity and no recurrence till last followup. One patient had deformity of the nail preoperatively due to previous surgery, which persisted after excision of the tumor. All of them returned to their preoperative occupation and regained full function of the hand.
Conclusions:
The transungual approach provides good access to the entire lesion and facilitates complete excision. Contrary to reported literature, we did not find the development of any new nail deformity with this approach.
Keywords: Glomus tumors, nail-plate, subungual, transungual
MeSH terms: Tumors, glomus tumor, neoplasms, hand, surgical procedure
INTRODUCTION
Glomus tumors are rare benign hamartomas of vascular origin, arising from the glomus body.1 The majority of these tumors occur in the subungual region of the digits.1,2,3,4,5 They pose a unique challenge to the unwary orthopedic surgeon. They cause severe pain and disability to the patient, with only subtle clinical signs,6 which can be easily missed unless specifically looked for by a meticulous clinical examination. Magnetic resonance imaging (MRI) is useful in the diagnosis of these occult lesions.7
Surgical excision is the only known treatment option for subungual glomus tumors.2,5,6,8 Two surgical approaches are described in literature-transungual and periungual (lateral).1,2,3,5,6,8,9 Complications of surgery include recurrence of symptoms and deformity of the nail. Recurrence of symptoms is, usually due to incomplete excision of the lesion rather than true recurrence of the tumor.2,10 Although the transungual approach is described as classical,1,2,5,11 the literature reveals a high incidence of postoperative nail deformity.5,11,12,13,14
This retrospective study reviewed the results of subungual glomus tumors of the hand treated by transungual excision. We hypothesized that the transungual approach allows good access to the entire lesion facilitating complete excision and meticulous repair of the nail bed minimizes chances of nail deformity.
MATERIALS AND METHODS
12 patients with histopathologically confirmed subungual glomus tumors of the hand were treated in our institute between 2007 and 2012. Data were obtained retrospectively from hospital records and the patients were called for clinical followup.
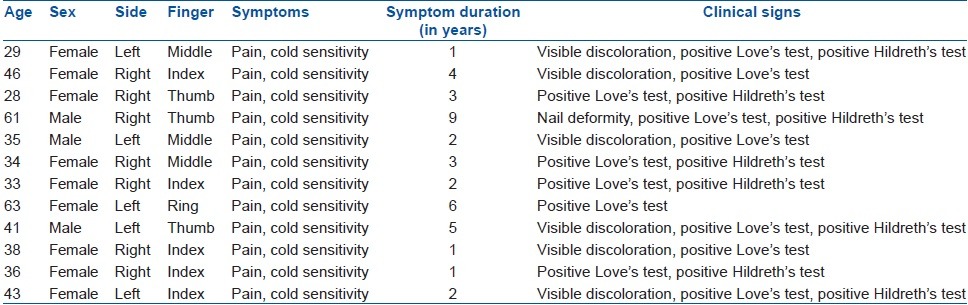
There were 9 females and 3 males. The mean age of the patients at the time of surgery was 40.5 years (range 28–63 years) [Table 1]. The right hand was affected in 7 patients. The index finger was the most common digit to be involved (n = 5), followed by the middle finger and the thumb (n = 3 each) and the ring finger (n = 1).
Table 1.
Clinical details of patients
A history of blunt trauma to the affected fingertip prior to onset of symptoms was present in 4 patients. The mean duration of symptoms before diagnosis was 3.25 years (range 1–9 years). All patients presented with complaints of pain in the nail bed and had localized tenderness. The pain was aggravated by immersing the hand in cold water. A bluish brown discoloration could be seen through the nail plate in 6 patients [Figure 1a and b]. Exquisite tenderness demonstrated by the Love's pin test4 (the patient experiences severe excruciating pain when the nail-plate over the lesion is pressed with a pin head or tip of a ball point pen) was positive in all. The Hildreth's test15 (disappearance of pain and tenderness over the lesion after application of a tourniquet cuff proximally in the arm) was positive in 8 patients.
Figure 1.
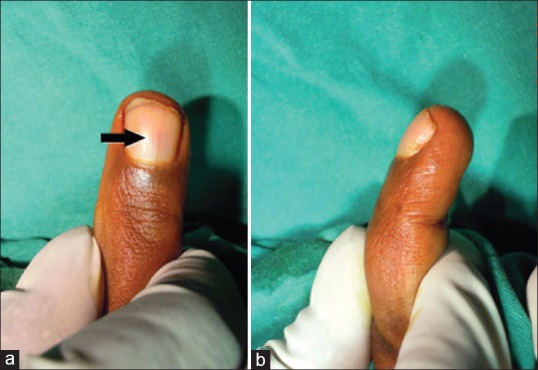
(a and b) Preoperative clinical photographs showing the faint bluish discoloration visible under the nail (arrow)
One patient, who was symptomatic for 9 years, had undergone an unsuccessful surgery for a subungual glomus tumor of the thumb 5 years ago at another institute. He presented to us with a nail deformity and persistence of the symptoms after the index procedure. None of the other patients had any nail deformity.
Plain radiographs did not reveal any abnormality in any of the patients. An MRI scan was obtained in all cases, but only in 8 cases it could identify the lesion [Figure 2]. In the remaining 4 patients, surgery was done based on clinical diagnosis.
Figure 2.
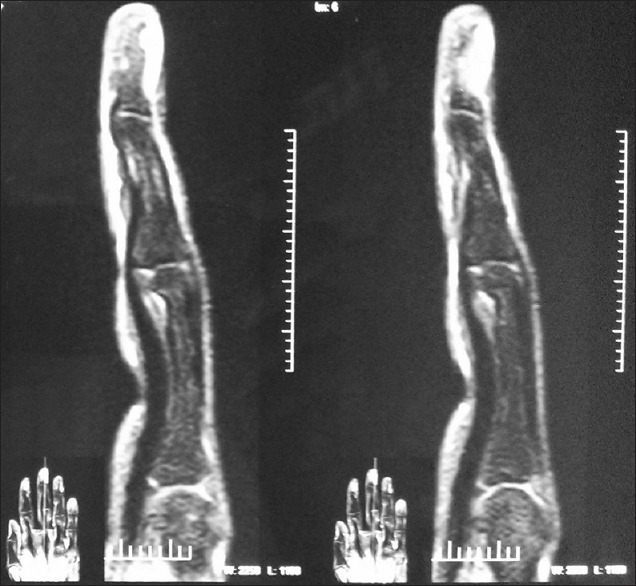
T2-weighted magnetic resonance imaging showing the subungual glomus tumor as a hyperintense lesion
After obtaining informed consent, surgical excision of the tumor was performed under general anesthesia or supraclavicular block using a tourniquet. A transungual approach was used in all the patients.2 The nail plate was carefully elevated with a mosquito hemostat, taking care to preserve the germinal matrix of the nail. The tumor mass was identified by the bluish-red discoloration in the nail bed [Figure 3a]. A longitudinal incision was made in the nail bed over the tumor [Figure 3b]. The nail bed was retracted and the tumor was excised completely [Figure 3c]. Hemostasis was secured after release of a tourniquet and the incision in the nail bed was approximated with 5.0 Vicryl (Ethicon, Johnson and Johnson, US) [Figure 3d]. The nail plate was repositioned without suturing over the nail bed and compression dressing was given to the finger [Figure 4a].
Figure 3.
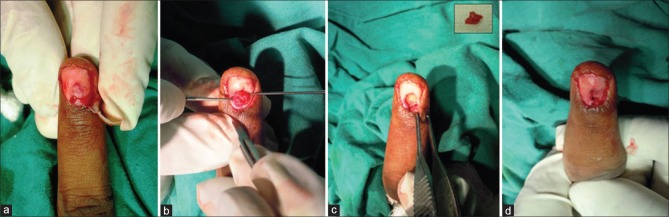
Peroperative clinical photographs showing (a) tumor visualized through the nail bed after elevation of the nail plate (b) tumor exposed after incision given in the nail bed (c) tumor excised and cavity curetted. Inset shows the excised tumor in toto (d) nail bed repaired with absorbable sutures
Figure 4.

Clinical photographs showing (a) nail plate replaced to act as a biological dressing (b) At 8 weeks, postoperative new nail is forming from the intact germinal matrix (c) no nail deformity or tumor recurrence noted at 2 years followup
All excised specimen were confirmed to be glomus tumors on histo pathological examination. Postoperative first dressing was done on 4th or 5th day. The nail plate, usually, fell off in 4–6 weeks and a new nail completely formed in 8–10 weeks [Figure 4b]. The mean duration of followup was 38 months (range 8–72 months). Consent from all patients was obtained for using the clinical data for publication.
RESULTS
Histopathology confirmed the diagnosis of glomus tumors in all patients. One patient also had a neuroma arising from the digital nerve from the radial volar aspect of the same (middle) finger detected incidentally on MRI, which was also excised. All patients had complete relief of pain. None of the patients had recurrence of the tumor till the last followup. One patient had deformity of the nail preoperatively due to previous surgery, which persisted after excision of the tumor. None of the remaining 11 patients developed any deformity of the new nail [Figure 4c]. All of them returned to their preoperative occupation and regained full function of the hand.
DISCUSSION
The principal finding of this study was that the transungual approach of excision for subungual glomus tumors allows good access to the entire lesion facilitating complete excision and there was no occurrence of new nail deformity. The glomus body is an arterio venous anastomosis found most abundantly beneath the nails and on the ventral surface of the finger tips. The function of the glomus body is regulation of cutaneous circulation.1
The glomus tumor arises from the glomus body. It is a hamartoma and not a true neoplasm. Grossly, the tumor forms a pink or purple soft mass less than a cm in size.1,2 Microscopically, the lumen of the anastomotic vessel is tortuous and dilated, lined by a single layer of endothelium. This endothelial layer is supported by a fibrous layer, which is surrounded by cuboidal or rounded endothelial cells, the glomus cells. A collagen fiber stroma is present between the endothelial cells, which contains nerve fibers.13 Infiltration of surrounding tissues is not seen; sometimes an incomplete capsule surrounding the lesion is present.2
The incidence of glomus tumors is 1–5% of all tumors of the hand.1,2,3,13 50–90% of these tumors occur in the subungual region of the digits.1,2,3,4,5,6 The pulp and the para ungual regions are the next most common sites.3,4,5,16 In our series, all the 12 glomus tumors were subungually located. The tumor is most commonly seen between 30 and 50 years of age, with women being affected 4 times more often than men.2,3,4,5,11,12,16 The mean age in our series was 40.5 years (range 28–63 years) and nine of our patients were women. Various studies show that a long duration of symptoms with various erroneous diagnosis seems to be the rule rather than the exception.2,4,5,11,12,16 In our study, the mean duration of symptoms was 3.25 years (range 1–9 years).
The three largest reported series of subungual glomus tumors emphasize the importance of clinical diagnosis based on the classical triad of excruciating pain, localized tenderness, and cold sensitivity.2,5,16 In our series, all 12 patients had these three clinical features. The Love's test which confirms the diagnosis and serves to clinically localize the tumor preoperatively,2,4,13,15,16 was positive in all 12 patients. The Hildreth's test-which is reported to be reliable and “virtually pathognomonic” of a glomus tumor13,14,15,16 was positive in eight of our patients. According to the literature, 26–50% of the subungual lesions are visible through the nail plate as a bluish discolouration.2,3,5 In our series, 6 patients had visible discoloration under the nail. Nail deformity or ridging can occur in subungual lesions.5 Preoperatively, none of our patients had any nail deformity, except 1 patient who had undergone a previous unsuccessful surgery elsewhere.
The condition can be confused with neuroma, chronic paronychia, angioma, subungual exostosis, radiculitis, Raynaud's phenomenon and even conversion reaction.2,16 The literature reveals that erroneous diagnosis has led to patients being subjected to a variety of procedures such as sympathectomy, radiation therapy, laminectomy, posterior rhizotomy, section of the scalenus anterior muscle and even amputation of digits.2 In our series also, patients had multiple consultations before coming to us, with inconclusive investigations and nonspecific treatment.
Although bony erosions of the terminal phalanx may be visible in plain radiographs in long standing lesions,2,6,7,13,17 none of our patients had any radiographic abnormality. The size, location and extent of the tumor are visualized well on MRI, which helps in complete excision of the tumour.7,10 We maintain that the diagnosis of subungual glomus tumors is essentially clinical and MRI acts only to confirm the clinical diagnosis, and to localize the lesion.18
Surgical excision is the treatment of subungual glomus tumours.2,5,6,8,9,10 Regional or general anesthesia and tourniquet are used. The transungual approach is the “classical” approach recommended by Carroll and Berman and Van Geertruyden et al.,1,2,5,11 which we have used in all our patients. The other approach is the periungual (or paraungual) approach described for pulp lesions and lesions partially under the nail.2 In this approach, a lateral incision close to the edge of the nail is given followed by excision of the tumor in the subperiosteal plane.3,9
The complications of surgery are nail deformity and recurrence of the tumor. The literature states that the transungual approach can cause “significant” nail deformity.3 The incidence of nail deformity after transungual approach varies from 3.3% to as high as 26.3%.5,12,14 In the periungual approach, as the germinal matrix of the nail is not disturbed, the incidence of nail deformity is said to be lower.1,3,9,12,16 We have employed the direct transungual approach in all our patients. We feel that this approach does not cause nail deformity if the nail plate is carefully elevated without damaging the germinal matrix and meticulous repair of the nail bed is performed. The nail falls off over the course of a few weeks and is replaced by a new nail in 8–10 weeks. Contrary to reported literature,5,11,12,13,14 none of our patients developed any new postoperative nail deformity. One patient had deformity of the nail preoperatively, which persisted after excision of the lesion. Lee et al. have also reported no postoperative nail deformity with the transungual approach, but with only a 10 months followup.19
Any recurrence of symptoms is probably related to incomplete excision of the original lesion, rather than true recurrence of the tumor.10 True recurrence of the tumor is rare.2 Carroll and Berman reported recurrence of the tumor in two out of 28 patients and Van Geertruyden et al. reported recurrence in two out of 51 patients.2,5 We feel transungual approach gives good access to the subungual tumor, facilitating complete excision. We had no recurrence of the lesion at a mean followup of 38 months.
A limitation of our study is that this is a retrospective study and we have not compared the transungual and the periungual approaches. Prospective, randomized trials comparing the exposure provided by these approaches and their functional outcomes are an avenue for future research.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.McDermott EM, Weiss AP. Glomus tumors. J Hand Surg Am. 2006;31:1397–400. doi: 10.1016/j.jhsa.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 2.Carroll RE, Berman AT. Glomus tumors of the hand: Review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972;54:691–703. [PubMed] [Google Scholar]
- 3.Vasisht B, Watson HK, Joseph E, Lionelli GT. Digital glomus tumors: A 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg. 2004;114:1486–9. doi: 10.1097/01.prs.0000138752.36175.d5. [DOI] [PubMed] [Google Scholar]
- 4.Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br. 2002;27:229–31. doi: 10.1054/jhsb.2001.0746. [DOI] [PubMed] [Google Scholar]
- 5.Van Geertruyden J, Lorea P, Goldschmidt D, de Fontaine S, Schuind F, Kinnen L, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21:257–60. doi: 10.1016/s0266-7681(96)80110-0. [DOI] [PubMed] [Google Scholar]
- 6.Netscher DT, Aburto J, Koepplinger M. Subungual glomus tumor. J Hand Surg Am. 2012;37:821–3. doi: 10.1016/j.jhsa.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 7.Shih TT, Sun JS, Hou SM, Huang KM, Su TT. Magnetic resonance imaging of glomus tumour in the hand. Int Orthop. 1996;20:342–5. doi: 10.1007/s002640050093. [DOI] [PubMed] [Google Scholar]
- 8.Green DP, Pederson WC, Hotchkiss RN, Wolfe SW. 5th ed. New York: Elsevier Churchill Livingstone; 2005. Green's Operative Hand Surgery. [Google Scholar]
- 9.Muramatsu K, Ihara K, Hashimoto T, Tominaga Y, Taguchi T. Subungual glomus tumours: Diagnosis and microsurgical excision through a lateral subperiosteal approach. J Plast Reconstr Aesthet Surg. 2014;67:373–6. doi: 10.1016/j.bjps.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Lin YC, Hsiao PF, Wu YH, Sun FJ, Scher RK. Recurrent digital glomus tumor: Analysis of 75 cases. Dermatol Surg. 2010;36:1396–400. doi: 10.1111/j.1524-4725.2010.01647.x. [DOI] [PubMed] [Google Scholar]
- 11.Tomak Y, Akcay I, Dabak N, Eroglu L. Subungual glomus tumours of the hand: Diagnosis and treatment of 14 cases. Scand J Plast Reconstr Surg Hand Surg. 2003;37:121–4. doi: 10.1080/02844310310005676. [DOI] [PubMed] [Google Scholar]
- 12.Takata H, Ikuta Y, Ishida O, Kimori K. Treatment of subungual glomus tumour. Hand Surg. 2001;6:25–7. doi: 10.1142/s0218810401000394. [DOI] [PubMed] [Google Scholar]
- 13.Samaniego E, Crespo A, Sanz A. Key diagnostic features and treatment of subungual glomus tumor. Actas Dermosifiliogr. 2009;100:875–82. [PubMed] [Google Scholar]
- 14.Grover C, Khurana A, Jain R, Rathi V. Transungual surgical excision of subungual glomus tumour. J Cutan Aesthet Surg. 2013;6:196–203. doi: 10.4103/0974-2077.123401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giele H. Hildreth's test is a reliable clinical sign for the diagnosis of glomus tumours. J Hand Surg Br. 2002;27:157–8. doi: 10.1054/jhsb.2001.0724. [DOI] [PubMed] [Google Scholar]
- 16.Gandon F, Legaillard P, Brueton R, Le Viet D, Foucher G. Forty-eight glomus tumours of the hand. Retrospective study and four-year followup. Ann Chir Main Memb Super. 1992;11:401–5. doi: 10.1016/s0753-9053(05)80277-7. [DOI] [PubMed] [Google Scholar]
- 17.Matloub HS, Muoneke VN, Prevel CD, Sanger JR, Yousif NJ. Glomus tumor imaging: Use of MRI for localization of occult lesions. J Hand Surg Am. 1992;17:472–5. doi: 10.1016/0363-5023(92)90353-q. [DOI] [PubMed] [Google Scholar]
- 18.Al-Qattan MM, Al-Namla A, Al-Thunayan A, Al-Subhi F, El-Shayeb AF. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30:535–40. doi: 10.1016/j.jhsb.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Lee IJ, Park DH, Park MC, Pae NS. Subungual glomus tumours of the hand: Diagnosis and outcome of the transungual approach. J Hand Surg Eur Vol. 2009;34:685–8. doi: 10.1177/1753193408104799. [DOI] [PubMed] [Google Scholar]


