Abstract
Background:
Vertical pelvic ring displacement (VPRD) is a serious injury and needs assessment. Pelvic outlet radiographs are routinely taken. However, relationship of radiographic and actual VPRD is still in question. Thus, measurement of VPRD from pelvic radiographs was studied.
Materials and Methods:
2 dry pelvic bones and 1 sacrum from same cadaver was reconstructed to be the pelvic ring. Five specimens were enrolled. 10, 20 and 30 mm vertical displacement of right pelvic bone was performed at levels of sacroiliac joint and pubic symphysis for representing right VPRD. Then, the pelvis was set sacral inclination at 60° from X-ray table for outlet and anteroposterior pelvic radiographs. Right VPRD was measured by referring to superior most pelvic articular surface of both sacroiliac joints and sacral long axis. Radiographic VPRD and actual displacement were analyzed by Pearson correlation coefficient at more than 0.90 for the strong correlation and strongly significant simple regression analysis was set at P < 0.01.
Results:
Radiographic VPRD from outlet and anteroposterior pelvic views at 10 mm actual displacement were 20.12 ± 1.98 and 4.08 ± 3.76 mm, at 20 mm were 40.31 ± 1.97 and 9.94 ± 7.27 mm and at 30 mm were 58.56 ± 2.53 and 11.29 ± 2.89 mm. Statistical analyses showed that radiographic VPRD from pelvic outlet view is 1.95 times of actual displacement with strong correlation at 0.992 coefficient and strongly significant regression analysis (P < 0.001) with 0.984 of R2 value. Whereas, the measurement from anteroposterior pelvic radiograph was not strongly significant.
Conclusion:
Pelvic outlet radiograph provides efficient measurement of VPRD with 2 times of actual displacement.
Keywords: Pelvic outlet radiograph, sacral long axis, sacroiliac joint, vertical pelvic ring displacement, pelvic bone
MeSH terms: Pelvic bones, radiography, fractures
INTRODUCTION
Vertical pelvic bone displacement creates unstable pelvic ring injury that is a serious trauma and life-threatening.1,2,3 Pelvic radiographs include anteroposterior, inlet and outlet views are routinely taken in order to measure pelvic displacement for considering proper management.3,4 Hence, measurement of vertical displacement of the pelvic ring injury from pelvic radiographs were studied.
MATERIALS AND METHODS
Five cadaveric dry bones of normal complete pelvic ring comprising 2 pelvic bones and 1 sacrum from the same cadaver were enrolled. The specimens were obtained from three males and two females, age ranged from 25 to 75 years old, no history of pelvic fracture, hip arthroplasty and metabolic bone diseases. Both pelvic bones and 1 sacrum were anatomically reconstructed to be a pelvic ring. Left pelvic bone was anatomically joined to sacrum in order to construct left sacroiliac joint by fixing pelvic and sacral articular surfaces of sacroiliac joint with two surface adhesive tape and secured the stability of the sacroiliac joint by plastic tape between left first sacral foramen and iliac wing. 10, 20, and 30 mm vertical displacement of right pelvic bone along the sacroiliac joint were performed in order to represent vertical displacement of right pelvic ring injury. Right sacroiliac joint was anatomically reconstructed. Then, middle of superior aspect of right sacroiliac joint was marked at pelvic and sacral sites at A and B respectively [Figure 1, left]. After that right pelvic bone was removed and viewed pelvic articular surface of right sacroiliac joint. AC line was drawn from A along the articular surface perpendicularly to superior articular surface of sacroiliac joint at A and ended at inferior articular surface at C. 10, 20, and 30 mm were marked on the AC line for sequentially performing vertical displacement of right pelvic bone by referring to the marker B at sacral site of sacroiliac joint B [Figure 1, middle and right]. The vertical displacement of right pelvic bone without pelvic anterior or posterior rotation was controlled by the same distance of displacement of pubic symphysis. During the displacement, width of the pubic symphysis was maintained by an appropriate rectangular rubber. The displacement of right pelvic bone was fixed by plastic tape between right and left obturator foramens for stabilizing pubic symphysis and two surface adhesive tape between articular surfaces of right sacroiliac joint as well as augmented by plastic tape between right first sacral foramen and iliac wing for stabilizing the sacroiliac joint [Figure 1]. For inlet pelvic radiograph, X-ray beam is parallel to sacrum and vertical displacement of pelvic ring. Therefore, the inlet pelvic radiograph cannot be used for assessing vertical displacement of the pelvic ring. Hence, the study included outlet and anteroposterior pelvic radiographs. Pelvic radiographs were taken at department of radiology. The specimen was laid on 3 cm thickness foam board and adjusted anterior surface of first and second sacrum inclination to be 60° from X-ray table as normal sacral inclination of the patient laid on the X-ray table.5 Outlet and anteroposterior pelvic radiographs were taken. X-ray tube was 40 inches from the specimen and 45° cephalad for the pelvic outlet view and 90° X-ray tube for anteroposterior pelvic view. Using Picture Archiving and Communication system and measurement tools, vertical displacement of right pelvic bone in millimeter was measured. Long axis of sacrum was drawn referring to sacral spinous processes (XY). Superior most pelvic articular surface of right and left sacroiliac joints were identified and marked at D and E respectively. DF and EG lines were drawn from D and E perpendicularly to XY at F and G. GF distance was measured as radiographic vertical displacement of right pelvic bone [Figure 2]. The data with more than 0.80 inter and intra-observer reliability were used for statistical analysis. Correlation between radiographic and actual vertical displacement of the pelvic bone were analyzed by Pearson correlation coefficient and considered more than 0.90 as strong correlation. The data was further analyzed by simple regression analysis and considered as strongly significant alpha level at P < 0.01.
Figure 1.
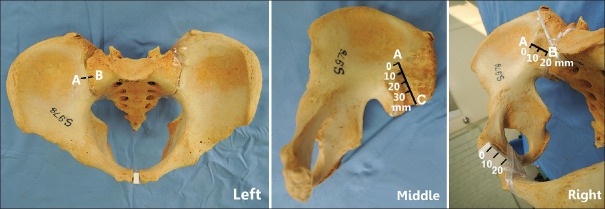
The pelvic ring was anatomically reconstructed by using 2 pelvic bones and 1 sacrum from the same cadaver. Middle superior right sacroiliac joint was marked at pelvic and sacral sites at A and B respectively (left figure). AC line was drawn from A along pelvic articular surface of sacroiliac joint perpendicularly to superior aspect of sacroiliac joint and ended at inferior articular surface at C. 10, 20, and 30 mm were marked along AC line (middle figure). 20 mm of vertical right pelvic bone displacement was performed for representing vertical displacement of pelvic ring injury (right figure)
Figure 2.
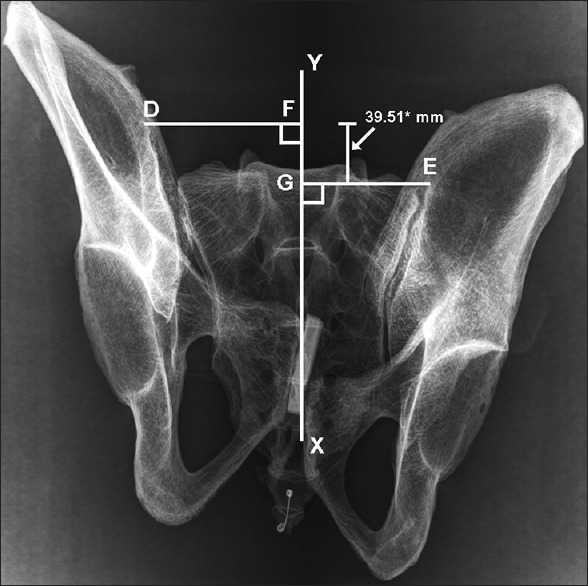
Radiographic vertical displacement of right pelvic bone was measured from pelvic outlet view by using superior pelvic articular surface of both sacroiliac joints and long sacral axis as references
RESULTS
Radiographic vertical right pelvic bone displacement from the outlet and anteroposterior pelvic views at 10 mm actual vertical displacement of the pelvic bone were 20.12 ± 1.98 (95% confidence interval [CI]: 17.66, 22.59) and 4.08 ± 3.76 (95% CI: 0, 8.75) mm, at 20 mm were 40.31 ± 1.97 (95% CI: 37.87, 42.76), 9.94 ± 7.27 (95% CI: 0.92, 18.97) mm and at 30 mm were 58.56 ± 2.53 (95% CI: 55.41, 61.70), 11.29 ± 2.89 (95% CI: 7.71, 14.88) mm respectively. Inter and intra observer reliability of the measurements from pelvic outlet radiograph was 0.86 and from anteroposterior pelvic radiograph was 0.82. The statistical analysis of radiographic vertical displacement of the pelvic bone from pelvic outlet view and actual displacement showed a strong correlation with 0.992 of Pearson correlation coefficient and simple regression analysis was also strongly significant (P < 0.001). In addition, simple regression equation showed that radiographic vertical displacement of the pelvic bone from pelvic outlet view was 1.95 times of actual displacement with 0.984 of R2 value [Table 1 and Figure 3]. Whereas, analysis of measurement of vertical displacement of the pelvic bone from anteroposterior pelvic radiograph and actual displacement showed no strong correlation with 0.539 of the correlation coefficient as well as no strongly significant simple regression analysis (P = 0.038). Moreover, R2 value for simple regression equation is only 0.290 [Table 1].
Table 1.
Data of radiographic and actual vertical pelvic bone displacements, correlation and simple regression analysis
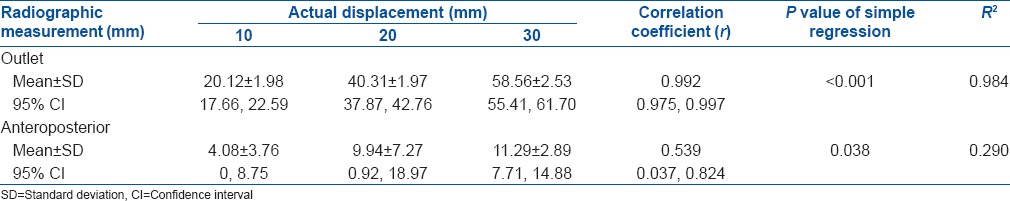
Figure 3.
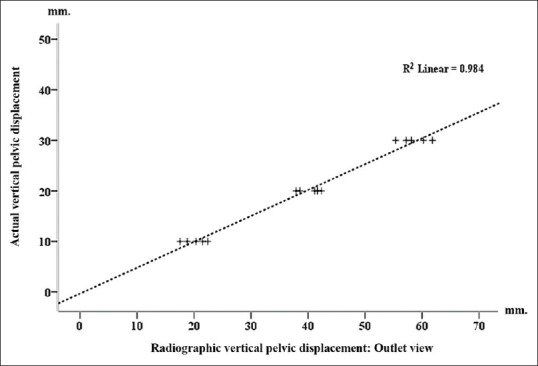
Regression analysis graph showing relationship between radiographic vertical pelvic bone displacement from outlet pelvic view and actual displacement was about 2 times
DISCUSSION
Vertical displacement of pelvic ring injury is a serious condition.1,2 The injury occurs as dislocation or fracture dislocation of sacroiliac joint and pubic symphysis.3,4 The injury creates unstable pelvic ring.1,2,3,4,6,7 Pelvic radiographs provide information about pelvic displacement in term of widening pelvic symphysis and vertical displacement of pelvic ring injury. Anteroposterior pelvic view is a familiar radiograph. However, the study showed the measurement of vertical displacement of pelvic bone from anteroposterior pelvic radiograph was inconsistent and did not strongly correlate to the actual displacement (R2 showed low value). Whereas, the measurement of vertical pelvic bone displacement from pelvic outlet radiograph showed strongly significant and consistent correlation about 2 times of actual displacement with high R2 value. This might be the result of different degrees of X-ray beam related to pelvic position between the outlet and anteroposterior pelvic radiographs. Vertical displacement of the pelvic bone in the study was performed along the plane of sacroiliac joint. The displacement of the pelvic bone at level of sacroiliac joint was equal to displacement of pubic symphysis. This resulted the measurement of vertical displacement of pelvic bone with neither anterior nor posterior rotation of the pelvic ring. Moreover, the pelvic inclination was set 60° at anterior surface of first and second sacrum. This represented pelvic inclination of lying patient.5 In the study, vertical displacement of the pelvic bone was measured by using superior most of pelvic articular surface of both sacroiliac joints and long axis of the sacrum as references. Both radiographic references were clearly viewed and identified especially in pelvic outlet radiograph. Moreover, the measurement of vertical pelvic bone displacement was directly performed at sacroiliac joint in term of upward displacement of articular surfaces. This measurement technique of vertical displacement of pelvic ring injury can be performed although the pelvic ring injury associated with fracture of ala sacrum.
In conclusion, the results of study showed that pelvic outlet radiograph provides efficient measurement of vertical displacement of pelvic bone with 2 times of actual displacement. Hence, we recommended that vertical displacement of pelvic ring injury in term of pelvic bone displacement should be measured by using pelvic outlet radiograph and consider a half of the measurement as actual displacement of the pelvic ring injury.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Sen RK, Veerappa LA. Outcome analysis of pelvic ring fractures. Indian J Orthop. 2010;44:79–83. doi: 10.4103/0019-5413.58610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reddy VS, Murthy GV, Nandan DA. Pelvic fractures. Indian J Orthop. 1997;31:203–5. [Google Scholar]
- 3.Dalal SA, Burgess AR, Siegel JH, Young JW, Brumback RJ, Poka A, et al. Pelvic fracture in multiple trauma: Classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29:981–1000. [PubMed] [Google Scholar]
- 4.Matta JM, Tornetta P., 3rd Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996:329129–40. doi: 10.1097/00003086-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Ricci WM, Mamczak C, Tynan M, Streubel P, Gardner M. Pelvic Inlet and Outlet Radiographs Re-Defined. J Bone Joint Surg Am. 2010;92:1947–1953. doi: 10.2106/JBJS.I.01580. [DOI] [PubMed] [Google Scholar]
- 6.Failinger MS, McGanity PL. Unstable fractures of the pelvic ring. J Bone Joint Surg Am. 1992;74:781–91. [PubMed] [Google Scholar]
- 7.Padalkar P, Pereira BP, Kathare A, Sun KK, Kagda F, Joseph T. Trans-iliosacral plating for vertically unstable fractures of sacral spine associated with spinopelvic dissociation: A cadaveric study. Indian J Orthop. 2012;46:274–8. doi: 10.4103/0019-5413.96376. [DOI] [PMC free article] [PubMed] [Google Scholar]


