Abstract
Background:
Sickle cell (SC) disease leading to endarteritis induces skeletal changes in the form of osteitis, sclerosis of femoral canal and osteonecrosis of the femoral head. All these make total hip arthroplasty (THA) difficult and prolonged. There is increased risk of infection, SC crisis and increased complication rate. Our paper aims to highlight preoperative, intraoperative and postoperative hurdles encountered in performing THA in sicklers and the short term outcome using cementless implants.
Materials and Methods:
Thirty-nine patients with SC disease, who had osteonecrosis of the femoral head, were operated between 2007 and 2011. The mean age of patients was 22 years (range 13–49 years). There were twenty eight females and 11 males. Bilateral cementless total hip replacement (THR) was performed in 11 patients (22 hips) and in the rest unilateral (28 hips). Preoperative and postoperative modified Harris hip score was evaluated. The average followup was 3.8 years (range 2-6 years).
Results:
The average operating time was 96 min (range 88–148 min). The average blood loss was 880 ml (range 650–1200 ml). The average intraoperative blood transfused was 2.3 units (range 2–5 units). All patients showed an improvement in Harris hip score from 42 points preoperatively to 92 points at latest followup. Intraoperatively, one patient had a periprosthetic fracture. Six patients developed acute SC crisis and were managed in intensive care unit. Three patients developed wound hematoma. Three patients developed limb length discrepancy less than 1 cm. None had early or late dislocations, infection, heterotopic ossification, sciatic nerve palsy and aseptic loosening.
Conclusion:
THA in sicklers involves considerable challenge for the orthopedic surgeon. Management requires a multidisciplinary approach involving the anesthetist, hematologist and the orthopedic surgeon. Contrary to previous reports, THA in sicklers now has a predictable outcome especially with the use of cementless implants.
Keywords: Cementless implants, sickle cell disease, total hip arthroplasty, avascular necrosis, femoral head
MeSH terms: Arthroplasty, replacement, hip, haemoglobin disease, sickle cell anemia, avascular necrosis of bone, osteonecrosis
INTRODUCTION
Sickle cell (SC) disease is endemic in African subcontinent but is also common in parts of Orissa ans Andhra Pradesh in India. SC disease patients have repeated sickling episodes leading to avascular necrosis of the femoral head. SC disease leading to endarteritis induces skeletal changes in the form of osteitis, sclerosis of the femoral canal and osteonecrosis of femoral head.1 All these make surgery difficult and prolonged. Total hip replacement in cases of osteonecrosis of the hip secondary to SC disease poses a considerable challenge to the treating orthopedic surgeon. The focal sclerotic marrow poses problem with reaming and placement of the implant. Narrow femoral canals may require the use of small/shorter femoral stems. The soft spongy bone in sicklers is at risk of fracture and bleeds a lot. There is increased risk of infection, SC crisis and increased complication rate in these patients.2,3,4,5
This study highlights the preoperative, intraoperative and postoperative hurdles encountered in performing a total hip replacement in patients with SC hemoglobinopathy and the short term outcome using cementless implants.
MATERIALS AND METHODS
Thirty nine patients with SC disease, with osteonecrosis of the femoral head, operated between 2007 and 2011 were included in this study. The mean age of patients was 22 years (range 13–49 years). There were twenty eight female and 11 male patients. Nineteen patients were homozygous for SC (hemoglobin SS), 15 had hemoglobin (Hb) S/C and rest were hemoglobin S/beta thalassemia. Bilateral cementless total hip replacement was performed in 11 patients (22 hips) and the rest had unilateral involvement (28 hips). Only one hip was operated at a time with an interval of 5–7 days between the surgeries. All patients were classified according to Steinberg staging developed by the University of Pennsylvania system.6 Twenty six were stage V, 9 were stage IV and 4 were stage III avascular necrosis hip. Preoperative Hb level was maintained to 8–10 gm%. The preoperative HbS load was decreased to <30%. This was done by giving aggressive preoperative transfusions or using plasmapheresis and exchange transfusion [Figure 1].7 Intraoperative medullary canal sclerosis [Figure 2a] was cleared using a high speed burr (50% of patients). All patients were operated using the Hardinge lateral approach to the hip. The operating room temperature was maintained at 220C and the patient was kept hydrated and warm using a bair hugger blanket to prevent hypothermia. Patients were given warm intravenous (iv) fluids. All patients were operated using cementless implants (Accolade stem, hydroxyapatite-coated acetabular cup, 28 mm/36 mm CoCr head and polyethylene liner, Stryker Howmedica, UK). Suction drains were placed in all patients.
Figure 1.

Clinical photograph showing the patient undergoing exchange transfusion using the plasmapheresis machine
Figure 2.
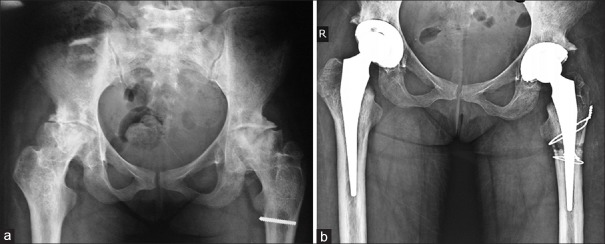
(a) Anteroposterior radiograph of the pelvis with both hips showing the sclerosis in the proximal femora and narrow medullary canals. Left femur shows a broken screw left from previous surgery (b) Postoperative anteroposterior radiograph of the pelvis with both hips showing cementless implants
Postoperatively, intravenous fluids were given at the rate of 120 ml/hour to maintain adequate hydration. Humidified oxygen was given at 5 L/min for 48–72 h. O2 saturation monitoring was carried up to 7 days postoperatively and maintained at 97%. Anticoagulation was started 12 h postoperatively and continued for 30 days postoperatively. Postoperative haemoglobin levels were maintained at >9 gm%.8 Patients were mobilized toe touch weight bearing with the help of a walker next day. The spongy bone in sicklers is so soft that the stability of the cementless implant (bone in growth) may be jeopardized leading to early loosening. So as a precaution, the patients were only allowed partial toe touch weight bearing from first postoperative day and full weight bearing was started at 6 weeks [Figure 4]. Patients were followed clinically and radiologically at 2 weeks, 1 month, 3 months and then yearly [Figures 2b and 3]. Preoperative and postoperative modified Harris hip score was evaluated.7
Figure 4.

(a) Preoperative (b) postoperative radiograph of thirteen years girl who underwent total hip replacement due to AVN hip secondary to sicking (c) Clinical photograph of same girl showing toe touch walking
Figure 3.

(a) Preoperative anteroposterior view of the pelvis with both hips showing advanced stage osteonecrosis of femoral heads in a 22 year old male (b) Anteroposterior radiograph of the pelvis with both hips after THA on the left side (c) Anteroposterior radiograph of both hips at 2 years followup after THA on both sides with no signs of aseptic loosening
RESULTS
The average followup was 3.8 years (range 2-6 years). The average operating time was 96 min (range 88–148 min). The average blood loss in patients was 880 ml (range 650–1200 ml). The average intraoperative blood (leukodepleted packed red blood cells) transfused were 2.3 units (range 2–5 units) to maintain a hemoglobin level of 8–10 gm% and dilute the HbS load. All the patients showed an improvement in Harris Hip score which improved from average 42 points preoperatively to average 92 points at latest followup. Intraoperatively, one patient had a periprosthetic fracture for which stainless steel cerclage wiring was done. Postoperatively, the average drain output was 450 ml (range 120–700 ml). Six patients developed acute SC crisis and were managed in Intensive Care Unit. Five of these required exchange transfusion. Three patients developed postoperative wound hematoma and were reexplored. Two patients had persistent wound discharge for 5–7 days. Cultures from their wounds were sterile. None of the patients had infection. Three patients developed limb length discrepancy less than 1 cm. None of the cases had aseptic loosening as assessed on serial radiographs. Subsidence was not noticed in any of the cases till latest followup. There were no early or late dislocations. No heterotopic ossification was seen in any of the cases. There were no cases of sciatic nerve palsy.
DISCUSSION
Sickle cell disease is the most common cause of avascular necrosis in childhood. The incidence of avascular necrosis in sicklers has been reported to be between 10% and 30%.9,10 Avascular necrosis of femoral head has been reported more commonly in SC disease (29%) and 19% in adults with SS disease.11,12,13
Preoperatively, average 4–5 units of leukodepleted packed red cells should be arranged in each case to attain a hemoglobin level of 8–10 gm%. This reduces the chances of development of postoperative acute SC crisis.3 All patients should be evaluated for antibodies in the blood as these patients have high chances of antibody levels due to repeated transfusions. These antibodies if not matched carry a high chance of alloimmunization and transfusion reactions. It is recommended to decrease the preoperative HbS level to <30% especially in patients who have a history of acute SC crisis, acute chest syndrome, previous cerebrovascular accidents and Hb <5 gm%. National preoperative transfusion in SC group recommends that conservative preoperative transfusion, to bring Hb 9–11 gm%, is as effective as aggressive transfusion regimen in which the HbS level was reduced to <30%.5
Surgery in SC can be prolonged due to increased blood loss, difficulty in dislocation secondary to protrusio or adhesions. Bleeding occurs from the vascular channels that enter the bone from the capsule. We found bone wax very handy to block these vascular channels. This step is important as this can prevent profuse blood loss. Al-Mousawi et al. have reported an average operative time of 2.2 h and a mean operative blood loss of 1275 ml.14 Blood loss encountered was also less due to shorter operative time, meticulous hemostasis while exposing and use of bone wax to seal the vascular sinusoids.
Hernigou et al. performed hip arthroplasty in 244 patients (312 hips) with SC disease and found medullary sclerosis in 46 femora.8 This increases the risk of perforation and fractures. Hanker et al. and others have described increased perforation rates.2,3 Intraoperative medullary canal sclerosis can be cleared by drilling a 4.5 mm drill bit or a high speed burr. This is followed by introduction of the guide wire into the femoral canal followed by enlargement of the canal using incrementally sized conical reamers. Hugh et al. have described making an anterior metaphyseal cortical window to identify the true medullary canal and facilitate femoral component implantation.15 We did not encounter any perforations because of the precautions and techniques used. SC hemoglobinopathy hinders the growth and development of bones in these patients. This may result in smaller bones and the resultant need to use small stems while performing a THA.16 Mosawi et al. recommend to keep a small size implant handy to avoid over preparation at the expense of bone stock.5 We did not need to use specialized short stems in our cases. We managed to put a minimum (size 0 accolade) uncemented stem in 9 hips we operated.
THA in SC disease is met with increased postoperative complications such as hematoma formation requiring evacuation, increased and persistent drainage, infection and acute SC crisis including the acute chest syndrome. Acute chest syndrome was managed by exchange transfusion, maintaining O2 saturation beyond 97%, pain control and iv hydration. Patients with SC disease are more prone to infection due to poor immune status and poor circulation of blood in the bone. Prolonged operative time added to the risk.17,18 We did not encounter any cases on acute chest syndrome. There is a high risk of osteomyelitis in sicklers. Patent organisms have been grown from femoral head cultures.19 We recommend that aspirates and tissue specimens should be collected from 6 different sites (subcutaneous tissue, capsule, acetabular floor, proximal femur, femoral canal and femoral head) from the hip and sent for cultures. If positive cultures are obtained, iv antibiotics should be continued for 6 weeks postoperatively. It is recommended to use antibiotic impregnated palacos cement in cemented THA.2 Hernigou et al. in their series of THA performed in SC hemoglobinopathy have reported that a preoperative infection had occurred in 21 of 312 hips (7%) and postoperative infection rate of 3% was seen in sicklers in their series. They advocated a two-stage revision at an interval of 45 days.8 We had no cases of deep infection which is contrasting to an earlier series that reported a high infection rate. The authors attribute this to shorter operative time, meticulous hemostasis, laminar air flow, preoperative correction of anemia, and SC load.
Sene et al. described a consecutive series of 38 patients including 48 cemented THR followed over a period of 7 years (mean followup 5 years). Normal hip function was achieved in 64% cases with a high complication rate of 19%.20 Cemented THA has its limitations because of the difficulty in cementing bleeding bone. Hernigou et al. have used the “French Paradox” technique where they used a rectangular stem to fill the canal without trying to obtain a continuous cement mantle. This provides a direct load transfer to bone by close cortical contact and also provides intrinsic stability that may protect the cement mechanically.8
Cementless stems are easier and quicker to place and have proven benefits in the young. The problem with cementless implants is the risk of fracture while placement of the stem and failure of the acetabular cup to incorporate in sclerotic bone. Ekere et al. have excellent results using uncemented hip replacement in two of their earliest cases done in Nigeria.21 Issa et al. compared 32 SC patients (42 hips) with 87 non-SC patients with hip osteonecrosis followed for >7 years and found no difference in aseptic implant survivorship (95% vs. 97%). They believed that the outcome of THA in SC patients can be improved by optimizing medical management and use of cementless prosthetic devices.22 We have used cementless implants in our series and have found them to shorten surgical time, are bone conserving and have a predictable outcome at mid term.
High rates of aseptic loosening in THA in sicklers have been reported in the literature.3,23,24 Hernigou et al. in their review of 312 hip arthroplasties performed in 244 patients with SC disease at mean followup of 13 years reported an aseptic loosening rate of 8%20 cups and 5%16 stems. They also mentioned that the risk of aseptic loosening was less than that reported in the literature.8 Although it is prematute to speak of loosening at 2 years of followup. We have had no aseptic loosening in our series and agree that loosening rates have decreased with the use of cementless implants.
The limitations of our study is that it has a short term followup. Further followup is warranted to judge the future of total hip arthroplasty using cementless implants in patients with SC disease.
CONCLUSION
Management in sicklers require a multidisciplinary approach involving the anesthetist, hematologist and the orthopedic surgeon. The hematologists need to reduce the SC load preoperatively by exchange transfusion and build hemoglobin to >9 gm%, the anesthetist need to keep the patient warm and hydrated to reduce sickling and the orthopedic surgeon needs to be meticulous and quick in technique and achieve adequate hemostasis during surgery. During the postoperative period, care needs to be taken to maintain hemoglobin >9 gm%, reduce SC load by aggressive transfusions, hydration and oxygenation, to avoid SC crisis. Contrary to previous reports, THA in sicklers now has a predictable outcome, less complications and failure rates especially with the use of cementless implants and better patient management in the pre, intra and postoperative periods.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Chung SM, Alavi A, Russell MO. Management of osteonecrosis in sickle-cell anemia and its genetic variants. Clin Orthop Relat Res. 1978;130:158–74. [PubMed] [Google Scholar]
- 2.Clarke HJ, Jinnah RH, Brooker AF, Michaelson JD. Total replacement of the hip for avascular necrosis in sickle cell disease. J Bone Joint Surg Br. 1989;71:465–70. doi: 10.1302/0301-620X.71B3.2722941. [DOI] [PubMed] [Google Scholar]
- 3.Hanker GJ, Amstutz HC. Osteonecrosis of the hip in the sickle-cell diseases. Treatment and complications. J Bone Joint Surg Am. 1988;70:499–506. [PubMed] [Google Scholar]
- 4.Hickman JM, Lachiewicz PF. Results and complications of total hip arthroplasties in patients with sickle-cell hemoglobinopathies. Role of cementless components. J Arthroplasty. 1997;12:420–5. doi: 10.1016/s0883-5403(97)90198-4. [DOI] [PubMed] [Google Scholar]
- 5.Vichinsky EP, Neumayr LD, Haberkern C, Earles AN, Eckman J, Koshy M, et al. The perioperative complication rate of orthopedic surgery in sickle cell disease: Report of the National Sickle Cell Surgery Study Group. Am J Hematol. 1999;62:129–38. doi: 10.1002/(sici)1096-8652(199911)62:3<129::aid-ajh1>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 6.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77:34–41. [PubMed] [Google Scholar]
- 7.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. [PubMed] [Google Scholar]
- 8.Hernigou P, Zilber S, Filippini P, Mathieu G, Poignard A, Galacteros F. Total THA in adult osteonecrosis related to sickle cell disease. Clin Orthop Relat Res. 2008;466:300–8. doi: 10.1007/s11999-007-0069-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hernigou P, Galacteros F, Bachir D, Goutallier D. Deformities of the hip in adults who have sickle-cell disease and had avascular necrosis in childhood. A natural history of fifty-two patients. J Bone Joint Surg Am. 1991;73:81–92. [PubMed] [Google Scholar]
- 10.Ware HE, Brooks AP, Toye R, Berney SI. Sickle cell disease and silent avascular necrosis of the hip. J Bone Joint Surg Br. 1991;73:947–9. doi: 10.1302/0301-620X.73B6.1955442. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds J. Springfield III: Charles C. Thomas; 1965. The Roentgenological Features of Sickle Cell Disease and Related Hemoglobinopathies. [Google Scholar]
- 12.Baumgaurd SH, Leach RE. Avascular necrosis of femoral head secondary to sickle cell disease: Case report of two Caucasian sisters. Clin Orthop. 1970;69:207–12. [PubMed] [Google Scholar]
- 13.Gunderson C, D’Ambrosia RD, Shoji H. Total hip replacement in patients with sickle-cell disease. J Bone Joint Surg Am. 1977;59:760–2. [PubMed] [Google Scholar]
- 14.Al-Mousawi F, Malki A, Al-Aradi A, Al-Bagali M, Al-Sadadi A, Booz MM. Total hip replacement in sickle cell disease. Int Orthop. 2002;26:157–61. doi: 10.1007/s00264-002-0337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hug KT, Gupta AK, Wellman SS, Bolognesi MP, Attarian DE. Creation of a femoral cortical window to facilitate total hip arthroplasty in patients with sickle cell hemoglobinopathies. J Arthroplasty. 2013;28:323–5. doi: 10.1016/j.arth.2012.06.021. [DOI] [PubMed] [Google Scholar]
- 16.Platt OS, Rosenstock W, Espeland MA. Influence of sickle hemoglobinopathies on growth and development. N Engl J Med. 1984;311:7–12. doi: 10.1056/NEJM198407053110102. [DOI] [PubMed] [Google Scholar]
- 17.Bishop AR, Roberson JR, Eckman JR, Fleming LL. Total hip arthroplasty in patients who have sickle-cell hemoglobinopathy. J Bone Joint Surg Am. 1988;70:853–5. [PubMed] [Google Scholar]
- 18.Booz MM, Hariharan V, Aradi AJ, Malki AA. The value of ultrasound and aspiration in differentiating vaso-occlusive crisis and osteomyelitis in sickle cell disease patients. Clin Radiol. 1999;54:636–9. doi: 10.1016/s0009-9260(99)91081-4. [DOI] [PubMed] [Google Scholar]
- 19.Lifeso R. Total joint replacement in sickle cell disease. Orthop Trans. 1985;9:453. [Google Scholar]
- 20.Sene M, Dansoko A, Ndiaye A, Mbaye E, Niang CD, Faye M. Total hip arthroplasty after avascular necrosis due to sickle cell disease in Senegal: Series of 48 replacements. Med Trop (Mars) 2009;69:573–6. [PubMed] [Google Scholar]
- 21.Ekere AU, Eze CB, Ebirim LN. A report of two cases of uncemented total hip replacement in patients with sickle cell disease. Niger J Clin Pract. 2008;11:257–9. [PubMed] [Google Scholar]
- 22.Issa K, Naziri Q, Maheshwari AV, Rasquinha VJ, Delanois RE, Mont MA. Excellent results and minimal complications of total hip arthroplasty in sickle cell hemoglobinopathy at mid term followup using cementless prosthetic components. J Arthroplasty. 2013;28:1693–8. doi: 10.1016/j.arth.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Acurio MT, Friedman RJ. Hip arthroplasty in patients with sickle-cell haemoglobinopathy. J Bone Joint Surg Br. 1992;74:367–71. doi: 10.1302/0301-620X.74B3.1587879. [DOI] [PubMed] [Google Scholar]
- 24.Moran MC, Huo MH, Garvin KL, Pellicci PM, Salvati EA. Total hip arthroplasty in sickle cell hemoglobinopathy. Clin Orthop Relat Res. 1993;294:140–8. [PubMed] [Google Scholar]


