Abstract
Background:
Incidence of vertebral compression fractures (VCFs) is increasing due to increase in human life expectancy and prevalence of osteoporosis. Vertebroplasty had been traditional treatment for pain, but it neither attempts to restore vertebral body height nor eliminates spinal deformity and is associated with a high rate of cement leakage. Balloon kyphoplasty involves introduction of inflatable balloon into the fractured body of vertebra for elevation of the end-plates prior to fixation of the fracture with bone cement. This study evaluates short term functional and radiological outcomes of balloon kyphoplasty. The secondary aim is to explore short-term complications of the procedure.
Materials and Methods:
A retrospective study of 199 kyphoplasty procedures in 135 patients from March 2009 to March 2012 were evaluated with short form-36 (SF-36) score, visual analogue scale (VAS), detailed neurological and radiological evaluations. The mean followup was 18 months (range 12–20 months). Statistical analysis including paired sample t-test was done with statistical package for social sciences.
Results:
Statistically significant improvements in SF-36 (from 34.29 to 48.53, an improvement of 14.24, standard deviation (SD) - 20.08 P < 0.0001), VAS (drop of 4.49, from 6.74 to 2.24, SD - 1.44, P < 0.0001), percentage restoration of lost vertebral height (from 30.62% to 16.19%, improvement of 14.43%, SD - 15.37, P < 0.0001) and kyphotic angle correction (from 17.41° to 10.59°, improvement of 6.82, SD - 7.26°, P < 0.0001) were noted postoperatively. Six patients had cement embolism, 65 had cement leak and three had adjacent level fracture which required repeat kyphoplasty later. One patient with history of ischemic heart disease had cardiac arrest during the procedure. No patients had neurological deterioration in the followup period.
Conclusions:
Kyphoplasty is a safe and effective treatment for VCFs. It improves physical function, reduces pain and corrects kyphotic deformity.
Keywords: Kyphoplasty, osteoporosis, percutaneous, vertebral compression fractures
MeSH terms: Vertebroplasty, osteoporotic fracture, bone cements, vertebrae bone fractures
INTRODUCTION
Osteoporotic vertebral compression fractures (VCFs) are a major healthcare problem.1 Symptomatic VCFs can be associated with decreased quality-of-life and increased mortality in the elderly.2 Disability associated with VCFs is apparently caused by changes in the alignment of the spine and related to the severity of spinal deformity. Standard management includes bed rest, analgesia, bracing or a combination of these.3 Prolonged bed rest leads to further loss of bone mass while bracing cannot restore spinal alignment and often is poorly tolerated by older patients. Open surgical treatment is reserved to the rare cases of progressive deformity and neurological deterioration or to more frequent cases of persistent, intractable pain. Vertebroplasty and Kyphoplasty are well known percutaneous vertebral body augmentation procedures that provide pain relief when used to treat osteoporotic VCFs. Vertebroplasty has been used to treat pain, it neither attempts to restore vertebral body height nor eliminates spinal deformity and is associated with a high rate of cement leakage.4,5,6,7,8,9,10 Percutaneous balloon kyphoplasty involves introduction of the inflatable balloon into the fractured body of the vertebra for elevation of the end-plates prior to fixation of the fracture with bone cement.11,12,13,14 This study was conducted to evaluate functional and radiological outcomes of balloon kyphoplasty in acute VCFs and pseudarthrosis.
MATERIALS AND METHODS
All 135 patients who sustained VCFs in total 199 vertebrae due to osteoporosis, malignancy or traumatic event and were operated with balloon kyphoplasty between March 2009 and March 2012 at our tertiary referral center, were included in this retrospective study. All the patients had painful, stable, wedge compression fractures without breach of posterior cortex. The neurological status was normal and there were no active signs of infection. None of the patients included in the study had history of intervention for spine ailments or history of allergy to polymethylmethacrylate bone cement.
Patients with coagulation disorders, unstable fractures or complete vertebral collapse with posterior cortical defects, vertebral fractures with neurological deficits, signs of active infection and history of known allergy to polymethylmethacrylate cement were excluded from the study. Patients undergoing repeat kyphoplasty for a new fracture or due to previous kyphoplasty procedures were excluded from the study.
All patients were explained in detail about their diagnosis and treatment options available both nonoperative and operative. Detailed history, physical examination, laboratory investigations and evaluation by physician, anesthetists and cardiologists were done before the procedure. Preoperative radiological percentage loss of vertebral height and kyphotic angle were measured. Preoperative pain and quality of life were analyzed by visual analogue scale (VAS)15 and short form-36 (SF-36)16 score. The VAS is a psychometric response scale. Operationally, it is usually a horizontal line, 100 mm in length, anchored by word descriptors at each end. The patient marks on the line the point that they feel represents their perception of their current state. The VAS score is determined by measuring in millimeters from the left hand end of the line to the point that the patient marks. As such an assessment is clearly highly subjective, these scales are of most value when looking at change within individuals and are of less value for comparing across a group of individuals at 1-time point. The SF-36 health survey consists of eight scaled scores (vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning and mental health). The final score is a weighted sum of the questions in each section. Each scale is directly transformed into a 0-100 scale on the assumption that each question carries equal weight. The lower the score, the more disability. The higher the score, the less disability. All patients underwent preoperative magnetic resonance imaging (MRI) scan to determine levels of vertebrae involved. The detailed written informed consent was taken from each patient.
Operative procedure
Patients were positioned prone on radiolucent C-arm operating table with properly positioned bolsters [Figure 1a]. Extra padding was placed beneath head, chest, pelvis and extremities. The procedures were performed under cover of 1.5 g intravenous cefuroxime antibiotic. After disinfection and draping diluted 1% lidocaine HCl was injected to anesthetize local area. Kyphoplasty was performed according to the procedure described by DaFonseca et al.17 and Voggenreiter18 Using fluoroscopic guidance, bilateral transpedicular or parapedicular access to the fractured vertebral body was obtained by insertion of guide wires at the 2 O’clock position of the right pedicle and the 10 O’clock position of the left pedicle. The opening was progressively enlarged using successively larger cannulas [Figure 1b]. The balloon tamps were then inserted through the cannulas and placed inside the anterior 3/4 of the vertebral body on the lateral view and covering both sides to the midline on the anteroposterior view. The balloons were then slowly inflated with dye containing fluid to reduce the compression fracture and create a void for cement injection. The inflation was stopped when the pressure gauge read 300 psi or if the balloon made contact with the end-plate [Figure 2a]. The volumes of the balloons were noted at this time. The cement was then mixed and time was allowed to pass until it hardened to an appropriate viscosity before injection. The balloons were then deflated and removed from the vertebral bodies and cannulas. The bone filling devices were filled with cement and placed through the cannulas into the anterior aspect of the void created by the balloons. The polymethylmethacrylate cement was injected incrementally to fill the void in a retrograde fashion from anterior to posterior [Figure 2b]. As the void was filled, the bone filling devices were pulled back gradually. Regular fluoroscopic imaging was performed to ensure no extravasations occurred. The volume of cement injected was equal to or less than the inflation volume of the balloon tamps. The bone filling devices were then pulled back slightly but kept in until the cement hardened. They were then twisted to break off any connected cement to prevent cement from being left in the pedicle when removing these devices from the cannulas.
Figure 1.
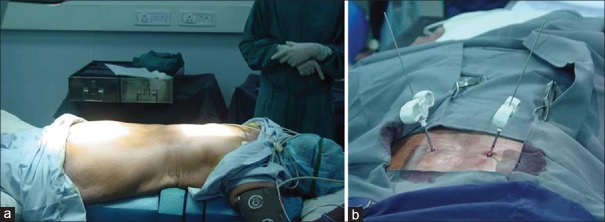
Clinical photograph showing (a) Position of patient. (b) Canula in situ
Figure 2.
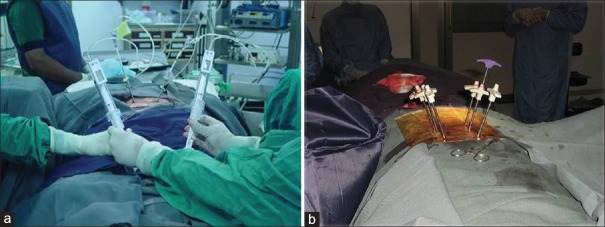
Peroperative clinical photographs showing (a) Inflating balloon (b) Polymethylmethacrylate cement insertion after balloon inflation
A number of precautions were taken to reduce cement extravasation as one of the most common kyphoplasty complications. These included a thorough analysis of the computed tomography (CT) scans, especially of the posterior wall; exact placement of the balloons and removal only immediately prior to cement delivery; injection of the cement at the correct viscosity and continuous fluoroscopic monitoring during cement delivery to rapidly spot any form of extravasation of the cement [Figures 1a, b and 2a, b].
Postoperative management
During the first 24 hours following kyphoplasty, circulation, motor and sensory functions of the extremities were monitored every 2 hourly. Besides the conventional radiographs in two planes, a CT scan of the area of interest was also used to establish any cement leakage, when in doubt. After the first postoperative day, patients were mobilized under the supervision of physiotherapists. Clinical (VAS and SF-36 scores) and radiological (restoration of vertebral height and kyphotic angle were measured19) followups were conducted at 1, 3, 6, 12, 18 and 20 months postoperatively. Radiographs were evaluated by independent radiologists with the help of computer measurement software preoperatively, postoperatively and at last followup. Intra operative and postoperative complications such as an allergic reaction to cement, cement embolism, cement leak, infection, neurological deficits and adjacent vertebral body fractures were noted [Figures 3 and 4].
Figure 3.

X-ray dorsolumbar spine anteroposterior view showing (a) osteoporotic fracture of vertebral body (b) cementing with restoration of height
Figure 4.
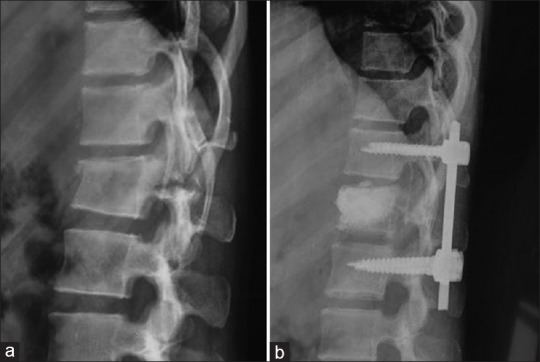
(a) Preoperative traumatic compression fracture. (b) Kyphoplasty with instrumentation
Statistical analysis
All data were evaluated using Statistical Package for the Social Sciences (SPSS) version 21.0 software, a statistical data analysis product from SPSS Inc., Chicago, IL, USA. by a professional statistician. Paired t-test was used to analyze mean difference at 95% level of significance between preoperative and postoperative values of variables such as VAS score, SP-36 score, X-ray kyphotic angle, loss of vertebral height. Distribution of age, gender, indication, number of levels, cement leak and its direction were also analyzed.
The mean in the paired samples t-test of all variables displays the average difference in each pair. The standard deviation (SD) displays the SD of the average difference in each score. The standard error mean values provide an index of the inter and intra observer variability in repeated random samples of 135 patients. Inter and intra observer variability was not found to be statistically significantly different. The 95% confidence interval of the difference of variables provides an estimate of the boundaries between which the true mean difference lies in 95% of all possible random samples of 135 patients in this study.
Magnetic resonance imaging scan provides valuable information about nature of the disease (i.e., osteoporotic, neoplastic and traumatic) and duration of fracture. We follow above illustrated treatment protocol. After 1-month of failed conservative treatment we consider vertebroplasty in patients with persistent painful fractures and compression <30% and kyphoplasty in fractures that had progressed to a vertebral body collapse equal or higher than 30% within the 3rd month. Kyphoplasty must be performed earlier than 3 months in order to maximize the possibility of improvement in spinal sagittal alignment. In all fractures presenting after 3 months duration vertebroplasty was performed [Figure 5].
Figure 5.
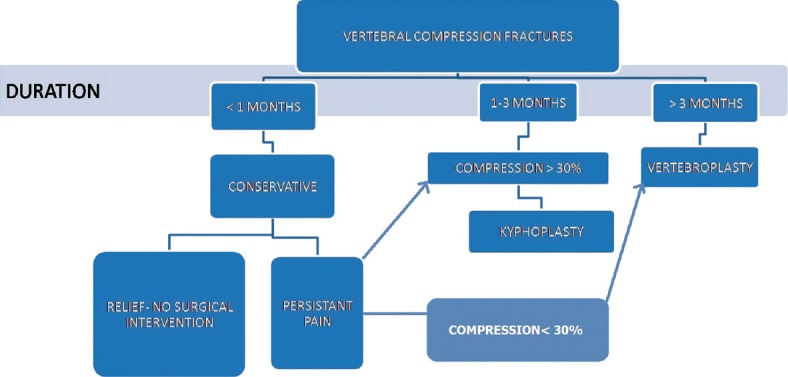
Treatment algorithm
RESULTS
There were total 135 patients included in the study (males: 52 [38.5%], females: 83 [61.5%]). Mean age was 67 years (range 19–88 years, mean: 67.45, median: 68 and mode: 65). Etiology of compression fracture was osteoporosis in 115 (85.2%) patients, malignancy in 17 (12.6%) patients and trauma in three (2.2%) patients. All patients underwent MRI of the spine in order to decide the level of vertebral involvement and pathology. Majority, 91 (67.4%) patients, had single vertebral level involved, two vertebral levels were involved in 30 (22.2%) patients, 8 (5.9%) patients had three level involvement, while rest 6 (4.4%) had four levels involved. 127 (94.07%) patients had kyphoplasty only while 8 (5.93%) patients had kyphoplasty with instrumentation procedure. The mean followup was 18 months (range 12-20 months).
Across 135 subjects VAS level witnessed drop of 4.49, from preoperative 6.74 to postoperative 2.24 (SD - 1.44, P < 0.0001). Short form-36 score improved from 34.29 to 48.53, an improvement of 14.24 (SD - 20.08 P < 0.0001).
Radiological outcome
Improvement of X-ray kyphotic angle from preoperative mean of 17.41° to postoperative mean 10.59°, mean improvement of 6.82° (SD - 7.26 P < 0.0001). Restoration of preoperative mean percentage loss of anterior vertebral height from 30.62% to postoperative 16.19% mean improvement of 14.43% (SD - 15.37, P < 0.0001).
Sixty-five (48.14%) patients had cement leak out of which 25 (18.52%) had antero lateral leak, 8 (5.93%) had postero lateral leak, 10 (7.41%) had leak in inferior disc, 19 (14.07%) had leak in superior disc, 3 (2.222%) had leak through pedicle. Although kyphoplasty is supposed to reduce the chances of cement leakage as it creates space for introduction of cement under lower pressure, we had significant number of cases with cement leakage. We contribute this finding to morphology and degree of comminution of fractures in those patients. Patients with either superior or inferior end-plate fracture had more chances of leakage into respective discs. With the breach of antero-lateral or postero lateral wall of the body, patients had leakage in the respective direction and cement was found to be leaked in pedicle when cannula was removed before cement was expected to have hardened or when breaking of connected cement was unsuccessful despite adequate twisting of cannula. Patients with cement leak were monitored for neurological or cardio-vascular deterioration postoperatively. None had any detectable complication. Three patients (2.4%) developed adjacent single vertebra fracture within 2 months of the index procedure. Two had upper adjacent vertebra involved, and one had lower one involved. All of them underwent immediate repeat kyphoplasty as they had severe pain and the deformity was more than 30°. They didn’t have any further complications. Intra-operative image intensifier showed uptake of cement in tributaries of the azygous vein in 6 (4.45%) patients. However, none progressed to frank pulmonary embolism. All patients were monitored in Intensive Care Unit and were managed conservatively. One patient (0.74%) with history of ischemic heart disease, developed cardiac arrest at the end of the procedure. Urgent cardiologist intervention was sought. There were no neurological deficits, infection and allergic reaction to cement in any of the patients postoperatively.
DISCUSSION
Back pain is the principal manifestation of an acute VCF.20,21 Pain is expected to subside as the fracture heals, over a period of approximately 3 months.22 However, it is estimated that one-third23 to three-quarters24 of such patients may then develop chronic back pain. The causes may be attributed to pseudarthrosis or to osteoporotic spinal deformity such as kyphosis or kyphoscoliosis. The degree of kyphosis correlates well with the patient's physical function, the risk of further fractures, compression of the spinal cord, mental well-being and pulmonary function, any of which may contribute to increased mortality rate.25,26,27 Traditional vertebroplasty has been used to treat pain, however, it makes no attempt to restore the height of a collapsed vertebral body and is associated with high rates of extravertebral cement leakage.4,5,6,7,8,9,10
Kyphoplasty is a new technique that involves the introduction of inflatable bone tamps into the vertebral body. As the tamp is inflated, vertebral body height is restored, and a cavity is created within the vertebral body, allowing for low-pressure cement filling of the cavity. Restoration of the sagittal alignment of the spine will bring about a change of the displaced center of gravity backwards, thereby decreasing the risk for secondary fractures.11,12,13,14 The creation of a void within the vertebral body surrounded by impacted trabeculae allows the insertion of viscous bone cement with moderate pressure, obviating leakage of cement. Hence, kyphoplasty reduces chances of complications associated with vertebroplasty and improves functional outcome by correcting kyphotic deformity.
In a prospective multicenter US study,28 there was an average of 60% reduction in pain (preoperative VAS = 7.5, 7 days postoperative VAS = 3, P < 0.01). Ledlie and Renfro29 reported similar results, with a continuation in the improvement at 1-year. Coumans et al.30 reported that, in 78 patients with 188 fractures, patient quality-of-life significantly improved following balloon kyphoplasty, as reflected by marked improvement in SF-36 (from preoperative 35.5 to postoperative 50.12 P < 0.001) and statistically significant improvement in function as shown by Oswestry disability index (preoperative 49 to postoperative 34, P < 0.001 at final followup). Theodorou et al.31 found that the average kyphosis decreased from 26° to 16° after balloon kyphoplasty in 24 fractures treated. Phillips et al.32 reported that the local angulation for 52 fractures prospectively treated with balloon kyphoplasty decreased from 17.5° to 8.7°, resulting in a mean local angular deformity correction of 8.8° (range, 0–29°). Theodorou et al.31 reported that the vertebral bodies were, on average, 79% of the predicted height before treatment and 92% of the predicted height after balloon kyphoplasty. In Ledlie and Renfro29 average anterior vertebral body height was 66% of the predicted value before balloon kyphoplasty and 89% of the predicted value after balloon kyphoplasty. Garfin et al.14 reported an average anterior vertebral body height of 68% of the predicted value before balloon kyphoplasty and 84% of the predicted value after balloon kyphoplasty. Multicenter US study,28 Lieberman et al.11 Theodorou et al.31 reported 30.2%, 35% and 66% lost vertebral height restored at midline respectively in all fractures.
Results of our study are similar to above mentioned results published in the literature. We have noted statistically significant improvement of symptoms in the form of improved VAS score (drop of 4.49, from preoperative 6.74 to postoperative 2.24) and SF-36 scores (improvement of 14.24, from preoperative 34.29 to postoperative 48.53). We also noted statistically significant improvement of kyphotic angle (mean improvement of 6.82°, from preoperative 17.41° to postoperative 10.59°) and percentage restoration of anterior vertebral body height (mean improvement of 14.43%, from preoperative loss of vertebral height of 30.62% to postoperative 16.19%).
Complications with kyphoplasty are less than that documented with vertebroplasty. Adjacent vertebrae fracture is a unique complication associated with Kyphoplasty, which occurs because of the increased strength of the stabilized vertebral bodies in an osteoporotic spine. We witnessed three such patients, all of them were managed conservatively. Adjacent vertebral fractures can be prevented by correctly recognizing and performing kyphoplasty in all fractured vertebrae identified by preoperative MRI scan. Furthermore, reported inevitable side effects of long term analgesic medication in patients with chronic pain can be avoided.33,34 Another disadvantage of kyphoplasty is the high cost of the equipment.35,36 The procedure takes longer and is more painful than vertebroplasty and may require general anesthesia and more radiation.
The principle limitations of this study were its nonrandomized design, hence, our results require confirmation by randomized controlled trials. In addition, there remain unresolved questions about kyphoplasty. There was no significant correlation between the degree of height restoration and the observed improvement of pain or mobility. Internal stabilization and thus prevention of permanent microfracturing may also cause pain reduction,37 because previous retrospective observations of patients after vertebroplasty with no effect on vertebral morphology also showed a significant reduction of pain.38,39 To establish cost-effectiveness, a formal study is required to confirm a potential reduction in downstream health resources with kyphoplasty.40 Other treatment options for pain caused by vertebral fractures such as brace treatment also have yet to be evaluated with regard to costs in a prospective controlled study.41
To conclude in this retrospective nonrandomized study, we observed a positive effect of kyphoplasty on vertebral morphology and patients’ pain and level of activity after minimum 12 months. Therefore, kyphoplasty performed in appropriately selected patients with severely painful acute vertebral fractures or nonunions is a promising addition to current pharmacological treatment. However, multicentric randomized controlled trails are required before reaching to significant conclusion.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Hall SE, Criddle RA, Comito TL, Prince RL. A case-control study of quality of life and functional impairment in women with longstanding vertebral osteoporotic fracture. Osteoporos Int. 1999;9:508–15. doi: 10.1007/s001980050178. [DOI] [PubMed] [Google Scholar]
- 2.Leidig-Bruckner G, Minne HW, Schlaich C, Wagner G, Scheidt-Nave C, Bruckner T, et al. Clinical grading of spinal osteoporosis: Quality of life components and spinal deformity in women with chronic low back pain and women with vertebral osteoporosis. J Bone Miner Res. 1997;12:663–75. doi: 10.1359/jbmr.1997.12.4.663. [DOI] [PubMed] [Google Scholar]
- 3.Pradhan BB, Bae HW, Kropf MA, Patel VV, Delamarter RB. Kyphoplasty reduction of Osteoporotic vertebral compression fractures: Correction of local kyphosis versus overall sagittal alignment. Spine. 2006;31:435–41. doi: 10.1097/01.brs.0000200036.08679.1e. [DOI] [PubMed] [Google Scholar]
- 4.Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33:166–8. [PubMed] [Google Scholar]
- 5.Kaemmerlen P, Thiesse P, Bouvard H, Biron P, Mornex F, Jonas P. Percutaneous vertebroplasty in the treatment of metastases. Technic and results. J Radiol. 1989;70:557–62. [PubMed] [Google Scholar]
- 6.Kaemmerlen P, Thiesse P, Jonas P, Bérard CL, Duquesnel J, Bascoulergue Y, et al. Percutaneous injection of orthopedic cement in metastatic vertebral lesions. N Engl J Med. 1989;321:121. doi: 10.1056/NEJM198907133210214. [DOI] [PubMed] [Google Scholar]
- 7.Cotten A, Dewatre F, Cortet B, Assaker R, Leblond D, Duquesnoy B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: Effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical followup. Radiology. 1996;200:525–30. doi: 10.1148/radiology.200.2.8685351. [DOI] [PubMed] [Google Scholar]
- 8.Lapras C, Mottolese C, Deruty R, Lapras C, Jr, Remond J, Duquesnel J. Percutaneous injection of methyl-metacrylate in osteoporosis and severe vertebral osteolysis (Galibert's technic) Ann Chir. 1989;43:371–6. [PubMed] [Google Scholar]
- 9.Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: Technical aspects. AJNR Am J Neuroradiol. 1997;18:1897–904. [PMC free article] [PubMed] [Google Scholar]
- 10.Cortet B, Cotten A, Boutry N, Flipo RM, Duquesnoy B, Chastanet P, et al. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: An open prospective study. J Rheumatol. 1999;26:2222–8. [PubMed] [Google Scholar]
- 11.Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2001;26:1631–8. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 12.Dudeney S, Lieberman IH, Reinhardt MK, Hussein M. Kyphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. J Clin Oncol. 2002;20:2382–7. doi: 10.1200/JCO.2002.09.097. [DOI] [PubMed] [Google Scholar]
- 13.Fourney DR, Schomer DF, Nader R, Chlan-Fourney J, Suki D, Ahrar K, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 2003;98:21–30. doi: 10.3171/spi.2003.98.1.0021. [DOI] [PubMed] [Google Scholar]
- 14.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 2001;26:1511–5. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 15.Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M. Development and validation of the Visual Analogue Scale (VAS) Spine Score. Unfallchirurg. 2001;104:488–97. doi: 10.1007/s001130170111. [DOI] [PubMed] [Google Scholar]
- 16.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 17.DaFonseca K, Baier M, Grafe I, Libicher M, Noeldge G, Kasperk C, et al. Balloon kyphoplasty in the treatment of vertebral fractures. Unfallchirurg. 2006;109:391–9. doi: 10.1007/s00113-006-1075-8. [DOI] [PubMed] [Google Scholar]
- 18.Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2005;30:2806–12. doi: 10.1097/01.brs.0000190885.85675.a0. [DOI] [PubMed] [Google Scholar]
- 19.Rea JA, Chen MB, Li J, Marsh E, Fan B, Blake GM, et al. Vertebral morphometry: A comparison of long term precision of morphometric X-ray absorptiometry and morphometric radiography in normal and osteoporotic subjects. Osteoporos Int. 2001;12:158–66. doi: 10.1007/s001980170149. [DOI] [PubMed] [Google Scholar]
- 20.Lyritis GP, Mayasis B, Tsakalakos N, Lambropoulos A, Gazi S, Karachalios T, et al. The natural history of the osteoporotic vertebral fracture. Clin Rheumatol. 1989;8 Suppl 2:66–9. doi: 10.1007/BF02207237. [DOI] [PubMed] [Google Scholar]
- 21.Sinaki M. Exercise and physical therapy. In: Riggs L, Melton J, editors. Osteoporosis: Etiology, Diagnosis and Management. New York: Raven Press; 1988. p. 401. [Google Scholar]
- 22.Eck JC, Hodges SD, Humphreys SC. Vertebroplasty: A new treatment strategy for osteoporotic compression fractures. Am J Orthop (Belle Mead NJ) 2002;31:123–7. [PubMed] [Google Scholar]
- 23.Cyteval C, Sarrabère MP, Roux JO, Thomas E, Jorgensen C, Blotman F, et al. Acute osteoporotic vertebral collapse: Open study on percutaneous injection of acrylic surgical cement in 20 patients. AJR Am J Roentgenol. 1999;173:1685–90. doi: 10.2214/ajr.173.6.10584820. [DOI] [PubMed] [Google Scholar]
- 24.Old JL, Calvert M. Vertebral compression fractures in the elderly. Am Fam Physician. 2004;69:111–6. [PubMed] [Google Scholar]
- 25.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: A prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–20. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 26.Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int. 1998;8:261–7. doi: 10.1007/s001980050063. [DOI] [PubMed] [Google Scholar]
- 27.Linville DA., 2nd Vertebroplasty and kyphoplasty. South Med J. 2002;95:583–7. [PubMed] [Google Scholar]
- 28.Garfin SR, Buckley RA, Ledlie J Balloon Kyphoplasty Outcomes Group. Balloon kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine. 2006;31:2213–20. doi: 10.1097/01.brs.0000232803.71640.ba. [DOI] [PubMed] [Google Scholar]
- 29.Ledlie JT, Renfro M. Balloon kyphoplasty: One-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg. 2003;98:36–42. doi: 10.3171/spi.2003.98.1.0036. [DOI] [PubMed] [Google Scholar]
- 30.Coumans JV, Reinhardt MK, Lieberman IH. Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg. 2003;99:44–50. doi: 10.3171/spi.2003.99.1.0044. [DOI] [PubMed] [Google Scholar]
- 31.Theodorou DJ, Theodorou SJ, Duncan TD, Garfin SR, Wong WH. Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures. Clin Imaging. 2002;26:1–5. doi: 10.1016/s0899-7071(01)00350-3. [DOI] [PubMed] [Google Scholar]
- 32.Phillips FM, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 2003;28:2260–5. doi: 10.1097/01.BRS.0000085092.84097.7B. [DOI] [PubMed] [Google Scholar]
- 33.Moulin DE, Iezzi A, Amireh R, Sharpe WK, Boyd D, Merskey H. Randomised trial of oral morphine for chronic non-cancer pain. Lancet. 1996;347:143–7. doi: 10.1016/s0140-6736(96)90339-6. [DOI] [PubMed] [Google Scholar]
- 34.Liegibel UM, Sommer U, Tomakidi P, Hilscher U, Van Den Heuvel L, Pirzer R, et al. Concerted action of androgens and mechanical strain shifts bone metabolism from high turnover into an osteoanabolic mode. J Exp Med. 2002;196:1387–92. doi: 10.1084/jem.20021017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hillmeier JS, Meeder PJ, Noledge G, Kasperk C. Minimally invasive reduction and stabilization of osteoporotic vertebral body fractures (balloon kyphoplasty) Oper Orthop Traumatol. 2003;15:343–63. [Google Scholar]
- 36.Fisher A. Percutaneous Vertebroplasty: A Bone Cement Procedure for Spinal Pain Relief. Canadian Coordinating Office for Health Technology Assessment (CCOHTA) 2002. [Last accessed on 2009 Nov 12]. http://www.ccohta.ca/publications/PDF/196_vertebroplasty_cetap_e.PDF .
- 37.Nakano M, Hirano N, Matsuura K, Watanabe H, Kitagawa H, Ishihara H, et al. Percutaneous transpedicular vertebroplasty with calcium phosphate cement in the treatment of osteoporotic vertebral compression and burst fractures. J Neurosurg. 2002;97:287–93. doi: 10.3171/spi.2002.97.3.0287. [DOI] [PubMed] [Google Scholar]
- 38.Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96:56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 39.Watts NB, Harris ST, Genant HK. Treatment of painful osteoporotic vertebral fractures with percutaneous vertebroplasty or kyphoplasty. Osteoporos Int. 2001;12:429–37. doi: 10.1007/s001980170086. [DOI] [PubMed] [Google Scholar]
- 40.Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ., 3rd Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int. 2001;12:1042–9. doi: 10.1007/s001980170015. [DOI] [PubMed] [Google Scholar]
- 41.Ethgen O, Tellier V, Sedrine WB, De Maeseneer J, Gosset C, Reginster JY. Health-related quality of life and cost of ambulatory care in osteoporosis: How may such outcome measures be valuable information to health decision makers and payers? Bone. 2003;32:718–24. doi: 10.1016/s8756-3282(03)00089-9. [DOI] [PubMed] [Google Scholar]


