Abstract
Background:
Cervical pedicle screw fixation is an effective method for treating traumatic and non traumatic injuries. But many studies have reported higher incidence of cervical pedicle penetration, so many research efforts have aimed at improving the accuracy of cervical screw fixation. Most of the anatomical studies on cervical pedicle screw placement previously published focused on the measurements of anatomical parameters, the entry point of pedicle screw is vague. We preliminarily designed a C3, C4 and C5 pedicle screw fixation method that had clear entry point and clinical cases confirmed that this method is feasible and safe. So we did this study of cervical pedicle screw fixation for C6 and C7 vertebrae.
Materials and Methods:
Fifteen cervical vertebrae specimens were prepared and bilateral pedicle screws were manually inserted into C6 and C7. The intersection of the horizontal line through the midpoint of the transverse process root and the vertical line through the intersection of the posterolateral and posterior planes of the isthmus was the entry point. The screws were inserted along the axis of the pedicle, with the screw axis coinciding with the pedicle. The pedicle was truncated axially and sagittally along the trajectory and the narrowest pedicular height (PH), pedicular width (PW), overall length of the screw channel (LSC), transverse angle (E) and vertical angle (F) were measured.
Results:
In C6, the PW and PH were 6.12 ± 0.78 and 7.48 ± 0.81 mm, respectively. In C7, the PW and PH were 6.85 ± 0.73 and 8.03 ± 0.38 mm, respectively. The LSC was 30.83 ± 0.91 mm. Two E angles were identified, namely E1 and E2 and their values were 89.61 ± 1.24 and 59.71 ± 1.10°, respectively. Meanwhile, F averaged 75.86 ± 1.12°.
Conclusion:
The intersection of the horizontal line through the midpoint of the transverse process root and vertical line through the intersection of the posterolateral and posterior planes of the isthmus can be used as an entry point for C6 and C7 pedicle screw fixation. The screws should be inserted at 60 or 90° with the posterolateral isthmus in the horizontal plane and at 75° with the posterior isthmus in the sagittal plane. The LSC should not exceed 30 mm.
Keywords: C6, C7, cervical vertebra, pedicle screw, cadaver
MeSH terms: Spine, clavicle, vertebrae, bone screw, fracture fixation, cadaver
INTRODUCTION
Cervical pedicle screw fixation is an effective method for the treatment of cervical disease.1,2 Biomechanical studies confirmed that the biomechanical stability of cervical pedicle screw fixation is better than that of other posterior fixation methods.3,4,5
Many studies have focused on cervical pedicle screw fixation, presumably because of its superior biomechanical stability. Currently, cervical pedicle screw fixation can be divided into two types. The first type is based on the use of the median sagittal and horizontal planes as references for inserting the screw, whereas the second type is navigation-assisted screw fixation.6,7,8,9,10,11,12,13,14,15,16,17,18,19 Using either method leads to a higher incidence of cervical pedicle penetration, as reported in the literature.1,2,3 For instance, Abumi et al.1 studied a total of 669 cases of cervical pedicle screw fixation and found that 45 screws (6.7%) penetrated the cortical bone. A study by Jeanneret et al.8 suggested that C5 screws have the highest incidence of cortex penetration, followed by C3 and C4 screws, whereas C6 and C7 screws have the lowest incidence. Karaikovic et al.12 analyzed the accuracy of cervical pedicle screw fixation and argued that penetration was greatest at C3, C4 and C5. The navigation drift leads to a higher incidence of cervical pedicle penetration with navigation-assisted screw fixation.2,3 Whether the vertebral body anatomic landmark can be considered a reference to improve the accuracy of screw fixation should be determined. We preliminarily designed a C3, C4 and C5 manual screw fixation method20 and a large number of clinical cases confirmed that the fixation method is feasible and safe.
This study aimed to develop a safer and more consistent method of C6 and C7 pedicle screw fixation through an anatomical study of this procedure.
MATERIALS AND METHODS
15 cervical vertebrae specimens (previously immersed in formalin) with no bone fracture, deformities or pathological damage were provided by the department of anatomy of the school of basic medical sciences of jilin university. The C6 and C7 vertebral segments were obtained.
Determination of the frame of reference
Two frames of reference were determined, namely the isthmus and the midpoint of the transverse process root. The area below the lower edge of the superior articular process, above the upper edge of the inferior articular process, and between the medial and lateral edges of the superior articular process of the same cervical segment was defined as the “isthmus.”20 The isthmus was divided into three equal parts and two vertical lines were drawn, with the medial third serving as the posterior plane of the isthmus and the lateral third serving as the posterolateral plane of the isthmus [Figure 1a]. The axis of the pedicle on the horizontal plane ran along the vertical line through the intersection of the posterolateral and posterior planes of the isthmus and the position of the pedicle was constant. In addition, the midpoint of the transverse process root was the midpoint between the upper and lower edges of the transverse process root, which was the junction of the transverse process and the vertebral body [Figure 1a]. The axis of the pedicle on the sagittal plane ran along a horizontal line through the midpoint of the transverse process root and the position of the axis was also constant. By establishing these constant parameters, we established frames of reference that could be used to determine the proper placement of pedicle screws and that will be minimally affected by inter individual variation or disease states.
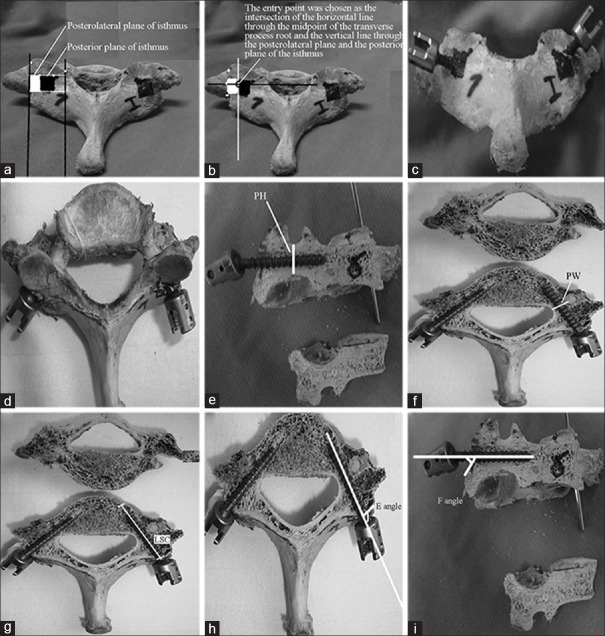
Figure 1.
Pedicle screw placement and measurements. (a) The isthmus, posterior plane and posterolateral plane of the isthmus; (b) The entry point; (c and d) Pedicle screw placement; (e) PH (pedicle height); (f) PW (pedicle width); (g) The length of screw channel (LSC); (h) E angle (transverse angle); (i) F angle (vertical angle)
Placement of pedicle screws
The entry point was chosen as the intersection of the horizontal line through the midpoint of the transverse process root and the vertical line and the line through the posterolateral and posterior planes of the isthmus, which was the vertical line through the mediolateral third of the isthmus [Figure 1b]. Screws of 3.5 mm in diameter and of appropriate lengths (Medtronic, vertex cervical pedicle screw) were selected and inserted along the axis of the pedicle under direct vision, with the axis of the screw coinciding with that of the pedicle and the front end of the screw penetrating the vertebral body or superior endplate [Figure 1c and d].
Pedicle measurements
To determine the optimal pedicle screw size, we made a number of measurements on the pedicles of C6 and C7. The pedicle was truncated axially and sagittally along the trajectory and the narrowest pedicular height (PH) [Figure 1e], narrowest pedicular width (PW) [Figure 1f] and overall length of the screw channel (LSC, defined as the linear distance between the entry point and the exit point) [Figure 1g] were measured using a vernier caliper (with an accuracy of 0.02 mm). The transverse angle (E angle, the angle between the axis of the screw and posterolateral of the “ischium” in the horizontal plane; shown in Figure 1h) and vertical angle (F angle, the angle between the axis aspect of the screw and posterolateral plane of the “ischium” in the sagittal plane; shown in Figure 1i) were measured using a protractor (with an accuracy of 1°).
Statistical analysis
Because the data was normally distributed, the measurements were compared by a paired t-test using SPSS software (Statistical Product and Service Solutions, version 13.0, SPSS Inc, Chicago, IL), with the level of significance set at P < 0.05.
RESULTS
The C6 and C7 vertebral segments of 15 cervical vertebrae specimens were bilateral based on the measurements of the PH, PW, LSC, E angle and F angle [Table 1]. No significant differences were observed (P > 0.05), which indicates a normal distribution and thus, the t-test was used.
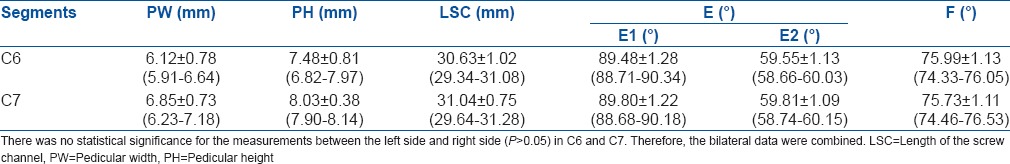
Table 1.
The results of relating pedicle parameters (n=15×2, χ̄±s)
Analysis of the measured data
The PW and PH were both larger in C7 than in C6 (P < 0.05, α = 0.05). However, within the same segment, PW was smaller than PH (P < 0.05, α = 0.05). No significant differences in the LSC and F angle were observed between C6 and C7 (P > 0.05). Therefore, the data for the two segments were combined [Table 2].
Table 2.
The combined result for the LSC, E1, E2 and F in C6 and C7
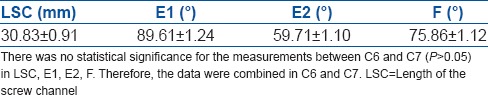
Hierarchical cluster analysis of the data was performed and the results illustrated that two E angles exist, namely E1 and E2. When the E angle was E1, the posterior and posterolateral planes of the isthmus formed an angle, indicating that they were in different planes. When the transverse angle was E2, the posterior and posterolateral planes of the isthmus were in the same plane, as shown in Figure 2. Among the specimens, E1 was observed in 11 C6 specimens and 8 C7 specimens, whereas E2 was noted in 4 C6 specimens and 7 C7 specimens.
Figure 2.
Relation of posterolateral plane and posterior plane A angulation of posterolateral plane and posterior plane B the posterolateral plane and posterior plane in the same plane. (a) The posterior and posterolateral plane of the isthmus was apparently angled; (b) The posterior and posterolateral part of the isthmus was in the same plane
No significant differences were found in E1, E2 and the F angle between C6 and C7 (P > 0.05), and the data were combined [Table 2]. According to the t-test, E1 was not significantly different from 90° and E2 was not significantly different from 60°. In the actual operation, the operative angle is difficult to control. Therefore, we suggest that in cervical pedicle screw fixation on C6 and C7, the screws should be inserted at 60 or 90° with the posterolateral plane of the isthmus in the horizontal plane (depending on whether the posterior and posterolateral planes of the isthmus form an angle) and at 75° with the posterior plane of the isthmus in the sagittal plane. The screw length should not exceed 30 mm.
DISCUSSION
Three-dimensional (3D) computer-assisted navigation systems have high accuracy rates in thoracic and lumbar pedicle screw placements, which can reach 89–100%.21 However, Ishikawa et al.22,23 discussed in two reports that the application of a navigation system in cervical vertebrae screw placement was associated with the postoperative cortex penetration rates of 11.1–18.7%, respectively, according to computed tomography (CT) analysis and the application of the navigation system based screw placement was associated with greater bone penetration than the traditional manual placement method with X-ray monitoring during the operation, indicating that the navigation can also lead to disastrous consequences, the intraoperative patients need high dose radiation and the long operation time. Navigation systems are associated with less accurate screw fixation in the cervical pedicle than in the thoracic and lumbar spine, which may explain why the neck is in a suspended state (remaining in a stationary state as in the thoracic and lumbar surgery can be difficult) irrespective of the type of head bracket used. In the screw placement process, cervical activity and navigation are difficult to synchronize and a large drift occurs. Therefore, manual placement is the preferred method.
Many studies reported10,15,24,25 that most surgeons select the sagittal, horizontal, or upper endplate plane of the spine as the reference and that the screw can be inserted at the proper angle using this reference. However, all of these references are hypothesized to exist and they are not intuitive, in addition to their spatial distance from the screw entry point. Some patients may experience cervical rotation or lateral bending, as well as dislocation and abnormal structure. In addition, considering the deep location of the lateral mass screw, when the screw is inserted, the cervical vertebra may dangle under the stress and all of the aforementioned factors could compromise the relationship between the axis of the pedicle and the selected reference, resulting in a great risk of injury and difficulty in screw fixation. The popularity of other auxiliary methods such as digging a hole in the entrance with a drill and intra operative X-ray monitoring, regardless of the strength of the screw, has been restricted because of fixation speed. Abumi et al.1 analyzed 669 cases of cervical pedicle screw fixation and found that 45 pedicle screws (6.7%) penetrated the bone cortex of the vertebral pedicle.
We introduced the “isthmus” concept into the cervical pedicle screw fixation technique. The area between the horizontal line through the nadir of the inferior margin of the superior articular process and the apex of the superior margin of the inferior articular process and the vertical line passing the lateral margin of the superior articular process is known as the “isthmus,” on which the posterior part of the vertebral pedicle projects. Karaikovic12 described this area as the base of the vertebral pedicle. This area is similar to the lumbar isthmus in the vertebral development process, and thus, we designated it as the cervical “isthmus,” which was considered a reference for screw fixation.
The “isthmus” is used as a reference for pedicle screw fixation angle to avoid the aforementioned disadvantages. The “isthmus” is the intersection of the inferior articular process and the superior articular process and that of the vertebral pedicle with the transverse process. Its anatomical structure is constant and rarely affected by factors such as location and dislocation.
In surgery, the lateral mass should be dissected further laterally until it is exposed. As long as the exposed plane does not exceed the cortex posterior of the transverse process, the vertebral artery and nerve root will remain undamaged. The internal and external edges of the superior articular process, as well as the upper and lower edges of the transverse process roots, can be explored using the probes, which is practical. We selected an entry point consistent with the projection of the posterior plane of the isthmus, which is a more appropriate entry point, permitting us more accurately to fix the pedicle screws along the axial direction.
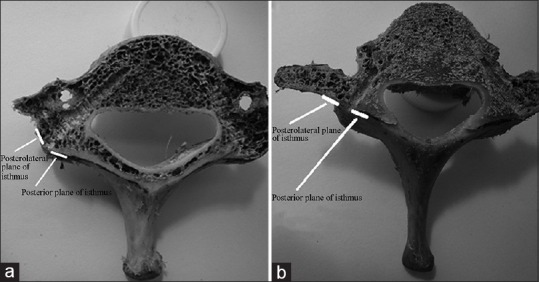
Abumi7 identified the entry point as slightly external to the lateral mass center and at the posterior edge of the superior articular process, and Jeanneret8 suggested an entry point located at the middle sagittal line of the lateral mass and 3 mm to the lower edge of the superior articular process. Thus, the two entry points were selected in the lower edge of the superior articular surface and the perpendicular bisector of the posterior lateral mass. Lee14 designated the entry point as 2 mm medial of the lateral mass center depression. In screw fixation, we found that the lower edge of the superior articular process is always located above the projection of the axis of the cervical pedicle entrance in the posterior isthmus, which is slightly superior. Thus, Abumi's entry point position is not in the axis of the pedicle, but it is slightly superior to this site, and the direction in which Abumi inserts the screw at the diagonal of the pedicle in the sagittal plane. The perpendicular plane of the posterior lateral mass is often located on the inner side of the projection of the pedicle axis in the posterior plane of the isthmus and inserting the screw at the perpendicular, bisecting the lateral mass may be slightly internal. Thus, Jeanneret's entry point is slightly internal, considering that the entry point is not in the pedicle of the axis. To make the screws pass through the pedicle, the screw direction should deviate from the axis, which is located along the diagonal of the pedicle in the horizontal plane. The disadvantages of not inserting the screw in the pedicle axis include the hardness of those parts of the cortex and the potential difficulty of the insertion, in addition to the potential for the screw to enter the spinal canal or transverse foramen. We designed an insertion method that does not expand the entrance point of the screw with a drill and also further strengthens the stability of the screws. When inserting the screw in accordance with the pedicle axis, the screw penetration point might occasionally be located on the endplate, opposed to in front of the vertebral body [Figure 3].
Figure 3.
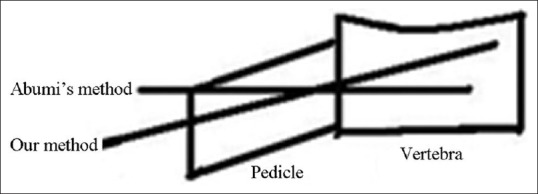
A line diagram showing the pedicle screw track contrast of our method to Abumi's method
Krag26 found that a screw length of 80% might be associated with 32.5% greater strength than a screw length of 50%, which is a significant difference. However, no significant differences were observed between the 80% and 100% screw lengths. We measured the screw length in the range of 29.34–31.28 mm, with a mean of 30.83 mm, but to avoid penetrating the upper endplate into the disk space, we propose that the screw length of C6 and C7 should be 24 mm, at which length the screw cannot penetrate the upper endplate into the gap but may achieve sufficient strength. In the statistical analysis, we identified two horizontal angles, namely E1 and E2. When the tE angle was E1, the posterior and posterolateral planes of the isthmus formed an angle [Figure 2a], indicating that they were in different planes. When the E angle was E2, the posterior and posterolateral planes of the isthmus were in the same plane [Figure 2b]. The t-test was performed in reference to angles of 60° and 90°, and the results identified no differences (P > 0.05). The F angle averaged 75.86 ± 1.12°. According to the measurement results of E1 and E2, maximum to a minimum difference of F angle should be no more than 2° and the angle was neither the maximum nor the minimum angle. If the angle is too large, then the screws will injure the vertebral artery and nerve root and if the angle is too small, then the screw can penetrate into the spinal cord and cause spinal cord injury. We suggested that the screw insertion angle should be in accordance with the mean value. In the operation, the angle cannot be determined, and thus, we suggest that the E angle of C6 and C7 should be 60° or 90° (according to whether the posterior and posterolateral planes of the isthmus form an angle), and the longitudinal angle should be controlled at 75°. Our results indicate that the insertion direction should depend on the angle, and according to the surgical experience of the surgeon and behavior of the pedicle probe during the operation, the direction can be adjusted when entering along the pedicle axis.
The limitations of this experiment included an insufficient number of samples and the measurement did not consider differences in gender and age. Thus, the measurement results for screw lengths, horizontal angles and F angles require further verification. We recommend that in clinical application, each value should refer to the preoperative 3D CT findings. However, the entry point and reference system we designed in this paper are feasible.
In summary, the method demonstrated in this study is different from previously described procedures. The use of this landmark to determine the screw entry point and angle can significantly reduce the incidence of tissue and provide a standardized measurement that compensates for interindividual variation in bone shape and size and differences arising from various diseases, which was previously lacking.
Footnotes
Source of Support: Nil
Conflict of Interest: All authors have no conflict of interest regarding this paper.
REFERENCES
- 1.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–9. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 2.Hasegawa K, Hirano T, Shimoda H, Homma T, Morita O. Indications for cervical pedicle screw instrumentation in nontraumatic lesions. Spine. 2008;33:2284–9. doi: 10.1097/BRS.0b013e31818043ce. [DOI] [PubMed] [Google Scholar]
- 3.Johnston TL, Karaikovic EE, Lautenschlager EP, Marcu D. Cervical pedicle screws vs. lateral mass screws: Uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006;6:667–72. doi: 10.1016/j.spinee.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 4.Dunlap BJ, Karaikovic EE, Park HS, Sokolowski MJ, Zhang LQ. Load sharing properties of cervical pedicle screw-rod constructs versus lateral mass screwrod constructs. Eur Spine J. 2010;19:803–8. doi: 10.1007/s00586-010-1278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kothe R, Ruther W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29:1869–75. doi: 10.1097/01.brs.0000137287.67388.0b. [DOI] [PubMed] [Google Scholar]
- 6.Panjabi MM, Duranceau J, Goel V, Oxland T, Takata K. Cervical human vertebral: Quantitative three-dimensional anatomy of middle and lower regions. Spine. 1991;16:861–9. doi: 10.1097/00007632-199108000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: Description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 8.Jeanneret B, Gebhard JS, Magerl F. Transpedicular screw fixation of articular mass fracture-separation: Results of an anatomical study and operative technique. J Spinal Disord. 1994;7:222–9. doi: 10.1097/00002517-199407030-00004. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Xu R, Richard A, Yeasting RA. Morphometric evaluation of lower cervical pedicle and its projection. Spine. 1997;22:1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 10.Miller RM, Ebraheim NA, Xu R, Yeasting RA. Anatomic consideration of transpediclar screw placement in the cervical spine: An analysis of two approaches. Spine. 1996;21:2317–22. doi: 10.1097/00007632-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 11.Panjabi MM, Shin EK, Chen NC, Wang JL. Internal morphology of human cervical pedicles. Spine. 2000;25:1197–205. doi: 10.1097/00007632-200005150-00002. [DOI] [PubMed] [Google Scholar]
- 12.Karaikovic EE, Yingsakmongkol W, Robet W. Accuracy of cervical pedicle screw placement using the funnel technique. Spine. 2001;26:2456–62. doi: 10.1097/00007632-200111150-00012. [DOI] [PubMed] [Google Scholar]
- 13.Hacker AG, Molloy S, Bernard J. The contralateral lamina: A reliable guide in subaxial cervical pedicle screw placement. Eur Spine J. 2008;17:1457–61. doi: 10.1007/s00586-008-0756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SH, Kim KT, Suk KS, Lee JH, Son ES, Kwack YH, et al. Assessment of pedicle perforation by the cervical pedicle screw placement using plain radiographs. Spine. 2012;37:280–5. doi: 10.1097/BRS.0b013e31822338ad. [DOI] [PubMed] [Google Scholar]
- 15.Langston TH, Kevin TF. Percutaneous placement of posterior cervical screws using three-dimensional fluoroscopy. Spine. 2006;31:536–40. doi: 10.1097/01.brs.0000201297.83920.a1. [DOI] [PubMed] [Google Scholar]
- 16.Rene S, Heiko K, Hans JW, Brade J, Zenner J, Meier O, et al. The impact of cervical pedicle screws for primary stability in multilevel posterior cervical stabilizations. Spine. 2010;35:E1167–71. doi: 10.1097/BRS.0b013e3181e6bc59. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine: Comparative accuracy of three techniques. Spine. 2000;25:1655–67. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 18.Bozbuga M, Ozturk A, Ari Z, Sahinoglu K, Bayraktar B, Cecen A. Morphometric evaluation of subaxial cervical vertebrae for surgical application of transpedicular screw fixation. Spine. 2004;29:1876–80. doi: 10.1097/01.brs.0000137065.62516.01. [DOI] [PubMed] [Google Scholar]
- 19.Rao BR, Marawar SV, Stemper BD, Yoganandan N, Shender BS. Computerized tomographic morphometric analysis of subaxial cervical spine pedicle in young asymptomatic volunteers. J Bone Joint Surg Am. 2008;90:1914–21. doi: 10.2106/JBJS.G.01166. [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Li Y, Wu Y, Zhu Q. A novel method of cervical pedicle screw placement from C3 to C5 and its clinical applications. Spine. 2013;38:E504–12. doi: 10.1097/BRS.0b013e3182880065. [DOI] [PubMed] [Google Scholar]
- 21.Ioannis DG, Nikolaos KP, Emilios EP, Politis AN, Arnaoutoglou CM, Karageorgos AC, et al. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21:247–55. doi: 10.1007/s00586-011-2011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishikawa Y, Kanemura T, Yoshida G, Matsumoto A, Ito Z, Tauchi R, et al. Intraoperative, full-rotation, three-dimensional image (o-arm)-based navigation system for cervical pedicle screw insertion. J Neurosurg Spine. 2011;15:472–8. doi: 10.3171/2011.6.SPINE10809. [DOI] [PubMed] [Google Scholar]
- 23.Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, Ohno S. Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: A retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine. 2010;13:606–11. doi: 10.3171/2010.5.SPINE09993. [DOI] [PubMed] [Google Scholar]
- 24.Shin EK, Panjabi MM, Chen NC, Wang JL. The anatomic variability of human cervical pedicles: Considerations for transpedicular screw fixation in middle and lower cervical spine. Eur Spine J. 2000;9:61–6. doi: 10.1007/s005860050011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hirano T, Hasegawa K, Takahashi HE, Uchiyama S, Hara T, Washio T, et al. Structural characteristics of the pedicle and its role in screw stability. Spine. 1997;22:2504–9. doi: 10.1097/00007632-199711010-00007. [DOI] [PubMed] [Google Scholar]
- 26.Krag MH, Beynnon BD, Pope MH, DeCoster TA. Depth of insertion of transpedicular vertebral screws into human vertebrae effect screw vertebra interface strength. J spinal Disord. 1986;1:287–94. doi: 10.1097/00002517-198800140-00002. [DOI] [PubMed] [Google Scholar]