Abstract
Objective
Nurse telephone counseling can improve the management of chronic conditions, but the effectiveness of this approach in underserved populations is unclear. This study evaluated the use of bilingual nurse-delivered telephone counseling in Korean Americans (KAs) participating in a community-based intervention trial to improve management of hypertension.
Methods
KAs were randomized to receive 12 months of hypertension-related telephone counseling that was more intensive (bi-weekly) or less intensive (monthly). Counseling logs were kept for 360 KAs who completed the pre- and post-intervention evaluations.
Results
The overall success rate for the intervention was 80.3%. The level of success was significantly influenced by the dose of counseling, employment status, and years of US residence. Over the 12-month counseling period, both groups showed improvement with regard to medication-taking, alcohol consumption, and exercise but not smoking, with no significant group differences.
Conclusion
Bilingual telephone counseling could reach monolingual KAs and improve their hypertension management behavior.
Practice implications
Bilingual nurse telephone counseling may have wide applicability, serving as an effective means of disseminating evidence-based chronic disease management guidelines to a linguistically isolated community with limited health resources and information.
Keywords: Telephone, Telephone counseling, Nurse counseling, High blood pressure, Korean Americans
1. Introduction
Although some counter-examples exist [1–3], telephone counseling has been generally successful in promoting medication adherence, healthy diet, and other lifestyle modifications among patients with high blood pressure (HBP) [4–6] and cardiovascular disease [7,8]. The advantages of telephone-delivered interventions include: ease of implementation [9,10]; cost-effectiveness [10]; and the capacity to reach a large group of people [11]. Nevertheless, the literature points to the over-representation of middle-class whites in the previous studies [11,12]. Furthermore, information concerning the optimal number of phone calls or duration of intervention has rarely been reported [10].
HBP is a common chronic disease that affects more than 65 million adults in the US [13]. The prevalence of HBP is known to increase when immigrants migrate to a more developed country, in part because of the stress related to acculturation and the changes in diet and lifestyle [14–17]. Indeed, epidemiological studies of Korean Americans (KAs), one of the most recent immigrant groups [18], reported heightened rates of HBP by 10–20% [19,20], with only one fourth of KAs having HBP control [19,20], as compared to 51% in the general population [21]. Barriers to adequate HBP care experienced by KAs have been identified, including lack of English proficiency [22] and lack of health insurance [23,24], primarily because of their disproportionate engagement in self-employed, small retail businesses (due in large part to their limited English skills) [25,26]. Taken together, these statistics indicate a significantly limited access to care encountered by KAs, making them one of the underserved populations in the country.
The Self-Help Intervention Program for HBP Care (SHIP-HBP) was developed and evaluated as a means of addressing the lack of adequate HBP care and control among KAs [27,28]. The SHIP-HBP consisted of psycho-behavioral education, together with self-monitoring of BP, and telephone counseling. Our purpose was two-fold: (1) to characterize the receptivity of the telephone counseling as a function of the sociodemographic and disease-related characteristics of the sample; and (2) to compare key behavioral outcomes by the dose of counseling. In particular, we hypothesized that more frequent, intensive telephone counseling would be significantly related to better behavioral outcomes (i.e., less smoking and alcohol consumption; greater levels of exercise and antihypertensive medication-taking).
2. Methods
The SHIP-HBP was a community-based trial (September 2003 to August 2008) targeting middle-aged KAs. The intervention had three components: (1) structured psycho-behavioral education; (2) home BP monitoring with a tele-transmission system; and (3) telephone counseling by a bilingual nurse. After a 6-week education and a 6-week test period for home BP monitoring, telephone counseling was begun and continued for 12 months. The changes in BP outcomes have been reported elsewhere [28].
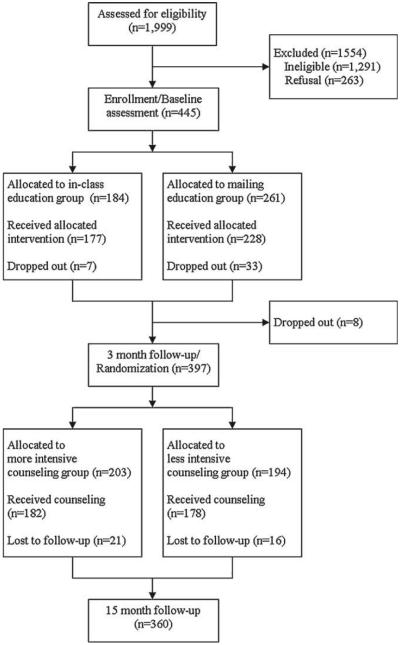
Study eligibility criteria were: 40–64 years of age; systolic BP ≥ 140 mm Hg and/or diastolic BP ≥ 90 mm Hg on two separate occasions or being on antihypertensive medication [13]; and self-identification as a KA. Given that today’s KAs are predominantly monolingual [29], massive outreach efforts were made at ethnic churches, groceries and through ethnic media. We screened over 1999 KAs and identified 708 eligible potential participants. Of these, 445 (63%) agreed and completed baseline assessment. Over the entire duration of this trial, 85 participants dropped out, resulting in 360 KAs at the 15-month evaluation (Fig. 1).
Fig. 1.
Participant tracking.
After IRB approval, participants received either in-class or mail-based HBP education for 6 weeks. Upon completion of the education component, participants were given a BP monitor with a tele-transmission system and were asked to measure BP at home and transmit the BP data via phone over the following 6 weeks. During this 6-week test period, we made sure all the participants were able to transmit their BP readings. At 3 months, participants were randomly assigned to either the more intensive (MI) bi-weekly or less intensive (LI) monthly telephone counseling groups.
Our telephone counseling was based on the Learned Resourcefulness Model [30,31]. The model recognizes individual factors that affect HBP behaviors (e.g., immigration status, living arrangements, daily needs). The primary goal of telephone counseling was to reinforce the evidence-based HBP knowledge learned through the education portion of the SHIP-HBP, while providing social support and opportunities to discuss the participant’s progress toward HBP control. At each counseling session, bilingual nurse counselors, together with the participants, reviewed BP reports generated from transmitted BP data and discussed their BP control status. This discussion was followed by topics critical to HBP management such as medication-taking, a low-salt diet, exercise, smoking cessation, home BP monitoring, or stress management [13] (Table 1).
Table 1.
Flow of content for the first nurse telephone counseling session.
| Duration | Discussed topicsa | Goals |
|---|---|---|
| 5min | Step 1. Opening | Build a rapport with the patient Set personal goal(s) to achieve BP control |
| 5min | Step 2. Home BP monitoring | Identify and address potential barriers and participants’ burden related to BP measures and transmission Provide tailored feedback to encourage regular BP check-ups |
| 5min | Step 3. Medications, side effects | Check the type, dose, and frequency of medication-taking Provide suitable advice when side effects are reported |
| 5–10 min | Step 4. Adoption and/or maintenance of a healthy lifestyle in the areas of diet, exercise, weight control, smoking, and alcohol consumption |
Help identify personal barriers to adopting and/or maintaining a healthy lifestyle for BP control Help identify effective strategies to address the barriers discussed |
| 5–10 min | Step 5. Life adversities (e.g., stress, lack of social support, other issues related to immigrant life) |
Probe other barriers relevant to life issues affecting BP control and management |
| 5min | Step 6. Closing | Reinforce personal goals by emphasizing the importance of BP control and care for the prevention of cardiovascular disease |
Steps 2–5 were repeated in the following sessions. The Step 1 goal was modified in the later sessions to involve reviewing the goals set during the prior session, with a brief introduction by the counselor.
We used data from a previous meta-analysis [32] to calculate sample size. In the meta-analysis, the effect size (Cohen’s d) of behavioral interventions to improve HBP management behaviors ranged from 0.40 to 0.70. To detect an effect size of 0.40 with 90% power and type I error of 0.05 (two-sided), the required sample size was 266 (133 for each group). We incorporated an attrition rate of 35%, yielding a total sample size of 360. Analysis was performed on an intention-to-treat basis. The sample characteristics and telephone outreach were compared between groups, using t-tests for continuous and chi-square tests for categorical variables. Chi-square tests were used to determine the effects of the telephone counseling on behavioral outcomes. Hierarchical regression was employed to identify factors that influenced the level of success in telephone outreach, after controlling for the intervention dose. The level of success in telephone outreach was calculated by dividing the number of successful counseling sessions by the number of scheduled sessions. Statistical significance was defined as p ≤ 0.05.
3. Results
The mean age of the sample was about 52 years, and close-to-equal gender representation was attained. Most were married (94.4%) and had at least a high school level of education (88.9%). About 55% reported being employed, but only 40% had health insurance. KAs had lived in the US for about 16 years. The majority (74.7%) reported a family history of HBP. Fewer than two-thirds (65.2%) were taking antihypertensive medication. Nearly 1 in 10(9.4%) reported smoking, and 36.7% reported drinking alcohol, whereas 54.6% indicated they had been performing exercise at the time of randomization. None of these characteristics differed by group assignment (Table 2). In addition, there was no difference in the distribution of the two initial educational modes between groups.
Table 2.
Characteristics of the two intervention groups at the time of randomization (3 months).
| Variable | Telephone counseling intervention |
||
|---|---|---|---|
| More intensive (n = 182) | Less intensive (n = 178) | Total (N = 360) | |
| Age, years (mean±SD) | 51.8±5.7 | 51.9±5.8 | 51.9±5.7 |
| Gender (%) | |||
| Male | 47.3 | 47.2 | 47.2 |
| Female | 52.7 | 52.8 | 52.8 |
| Married (%) | 94.5 | 94.4 | 94.4 |
| Education (%) | |||
| Less than high school | 8.2 | 14.0 | 11.1 |
| High school | 31.3 | 36.5 | 33.9 |
| College or more | 60.4 | 49.4 | 55.0 |
| Employed (%) | 58.2 | 51.1 | 54.7 |
| Have health insurance (%) | 42.3 | 37.6 | 40.0 |
| Years of residence in US (mean±SD) | 15.4±8.1 | 16.9±8.2 | 16.2±8.2 |
| Years of HBP (mean±SD) | 4.8±7.1 | 3.7±4.8 | 4.2±6.1 |
| Family history of HBP (%) | 75.3 | 74.2 | 74.7 |
| Having comorbidity (%) | 13.7 | 15.7 | 14.7 |
| Being on antihypertensive medication (%)a | 65.0 | 65.3 | 65.2 |
| Current smoking (%) | 8.8 | 10.1 | 9.4 |
| Alcohol consumption (%) | 38.5 | 34.8 | 36.7 |
| Exercise (%) | 56.6 | 52.5 | 54.6 |
Data available for 313 participants only.
For the patients who received the nurse telephone counseling, 360 (90.7%) completed the intervention. Over the 12-month counseling period, a total of 11,415 phone calls were placed; 5090 calls of which were successful. Success rates of telephone outreach were 74.2% (about 18 calls per person) for the MI and 86.5% (about 10 calls per person) for the LI groups (p ≤ 0.001). On average, nurses made about two phone calls for each scheduled session completed. The length of calls was longest for the first counseling session (18.1 ± 7.8 min). The average length of the subsequent counseling sessions for the MI group was longer than that for the LI group (p < 0.001) (Table 3).
Table 3.
Implementation of the telephone counseling intervention.
| More intensive (n = 182) | Less intensive (n = 178) | Total (N = 360) | ||
|
| ||||
| Number of total calls placed | 7,112 | 4,303 | 11,415 | |
| Number of successful calls | 3,242 | 1,848 | 5,090 | |
|
| ||||
| Mean±SD (range) |
||||
| More intensive (n = 182) | Less intensive (n = 178) | Total (N = 360) | ||
|
| ||||
| Success rates in telephone outreach (%)a,*** | 74.2±12.8 (29.2-95.8) | 86.5±14.7 (8.3-100.0) | 80.3±15.1 (8.3-100.0) | |
| Number of counseling sessions completed | 17.8±3.1 (4-23) | 10.4±1.8 (1-12) | 14.1±4.5 (1-23) | |
| Number of calls placed per scheduled sessionb | 1.9±0.6 (1-5) | 2.0±0.8 (1-6) | 2.0±0.7 (1-6) | |
| Length of first session, minutes | 18.4±7.7 (4-42) | 17.8±7.9 (4-50) | 18.1±7.8 (4-50) | |
| Length of subsequent session, minutes*** | 9.9±4.8 (1-45) | 8.6±4.5 (12-45) | 9.4±4.8 (12-45) | |
Number of successful telephone calls divided by the number of scheduled sessions (i.e., 24 sessions for the MI and 12 sessions for the LI group).
Includes only successful telephone calls for a particular scheduled counseling session.
p<0.001.
Employment status and years of residence in the US were significant predictors of the level of success in telephone outreach. Those who were unemployed (β = −0.165) and those with a longer duration of residence in the US (β = 0.177) were more likely to be reached successfully, after the dose of intervention was controlled for. The final model explained 30.1% of the variance in the dependent variable, though most of the explained variance was attributable to the dose of counseling (Table 4).
Table 4.
Factors influencing telephone outreach.a.
| Variable | B | β | R 2 | R2 change | Test of significance |
|---|---|---|---|---|---|
| Step 1 | 0.229 | 0.229 | F = 86.294*** | ||
| Dose of counseling | −.117 | −.460*** | |||
| Step 2 | 0.291 | 0.062 | F = 16.727*** | ||
| Age | .000 | .008 | |||
| Gender | −.016 | −.065 | |||
| Years of education | .002 | .038 | |||
| Employment | −.042 | −.165** | |||
| Health insurance | −.013 | −.051 | |||
| Years of residence in US | .003 | .177** | |||
| Step 3 | 0.301 | 0.010 | F = 12.149*** | ||
| Years of HBP | −.002 | −.076 | |||
| Family history | .019 | .067 | |||
| Comorbidity | −.009 | −.024 |
A multiple hierarchical regression model was used (N= 350 after removing 10 participants with extreme values). The dose of counseling was coded as 0 = LI and 1 = MI; gender was coded as 0 = male and 1 = female; employment was coded as 0 = unemployed and 1 = employed (full- or part-time); health insurance was coded as 0 = no insurance and 1 = yes; family history was coded as 0 = no and 1 = yes; comorbidity was coded as 0 = no comorbidity and 1 = yes.
p≤0.01.
p ≤ 0.001
At 3 months, the proportion of patients taking antihypertensive medication was similar for both groups. Over the 12-month counseling period, both groups showed a positive trend toward an increase in medication-taking. The MI group showed a slightly greater increase in the number of patients reporting medication-taking (6.5%, p = 0.041 for the within-group change), while the increase in the LI group was 5.4% (p > 0.05 for the within-group change). Other health behaviors improved significantly, except for smoking, with a reduction in alcohol consumption and increase in exercise for both groups (p < 0.01 for all within-group tests). None of these behavioral outcomes differed between the two groups (Table 5).
Table 5.
Comparison of behavioral outcomes.a.
| Variable | At randomization (3 months) |
At 15 months |
||
|---|---|---|---|---|
| More intensive (n = 182) | Less intensive (n = 178) | More intensive (n = 182) | Less intensive (n = 178) | |
| Being on medication (%)b | 65.0 | 65.3 | 71.5* | 70.7 |
| Smoking (%) | 8.8 | 10.1 | 8.2 | 9.6 |
| Alcohol consumption (%) | 38.5 | 34.8 | 30.2** | 24.7** |
| Exercise (%) | 56.6 | 52.5 | 84.6*** | 79.2*** |
McNemar tests were performed to examine within-group differences for each behavioral outcome.
Data available for 313 participants (n for the more intensive group = 162, n for the less intensive group = 151) only.
p<0.05.
p<0.01.
p<0.001.
4. Discussion and conclusion
4.1. Discussion
Telephone counseling by a bilingual nurse was feasible and accepted by KAs, one of the most underserved minority populations. Even though it is difficult to directly compare our success rates to those of previous studies because of the lack of similar studies, we are encouraged by the fact that participants could be reached after an average of two phone calls per session. This finding suggests that telephone interventions can reach participants and be successfully implemented in this linguistically isolated population.
The success of telephone outreach was influenced by the dose of the intervention, the participant’s employment status, and the number of years of residence in the US. The lower rates of success obtained for the MI group can probably be explained by the fact that the protocol required more frequent calls to this group. A plausible explanation for our findings regarding employment status and years of residence may be that employed participants and those with shorter duration of residence in the US found it difficult to receive phone calls because of work commitments or their different life priorities as a result of being recent immigrants [33]. Further research is needed to determine whether the timing of the telephone counseling (i.e., daytime vs. evening or weekend) influences the receipt of telephone counseling by ethnically diverse populations.
There were no significant differences in behavioral outcomes between the MI and LI groups. Instead, both groups showed improvement in these HBP management behaviors, with the exception of smoking. The result suggests that monthly telephone counseling for 12 months may be as effective as more frequent, bi-weekly counseling in promoting medication-taking and a healthy lifestyle among KAs. The optimal number of calls or duration of telephone interventions to promote HBP management is as yet unknown. A recent systematic review [10] of 26 studies using the telephone as the primary intervention method for physical activity and dietary change concluded that telephone counseling lasting 6–12 months and including 12 or more sessions produce more positive outcomes than did interventions lasting less than 6 months and having six or fewer sessions. More comparative studies are needed to investigate the effects of different doses and duration of telephone counseling on promoting healthy behaviors related to HBP management.
Our sample represented a well-educated, yet linguistically isolated group of immigrants. The level of success in telephone outreach that we achieved might have been a result of rare opportunities for KAs to receive reliable health information in their native language [33]. However, the success of this approach provides direct support for the utility of telephone-based health counseling as an effective strategy for disseminating health information to a linguistically isolated community and thereby addressing their unequal cardiovascular burden [19,20,27]. The participants’ behavioral outcomes were all self-reported. Studies have indicated, however, that self-report of antihypertensive medication is correlated with electronic monitoring [34,35]. We attempted to minimize potential bias by utilizing data collectors who did not provide telephone counseling to the participants. Finally, there was no “control” group in the study and hence it is not possible to determine whether the intervention is better than usual care.
4.2. Conclusion
Our study allowed us to obtain detailed procedural information regarding telephone counseling. The improvements in HBP management behaviors that we observed, together with the increased adherence to medication-taking and other lifestyle modifications demonstrated in previous studies [5–7], help support the theoretical basis for the telephone intervention. The results suggest that an intervention approach using bilingual nurse counselors may have wide applicability to linguistically isolated immigrant populations.
4.3. Practice implications
Our study provides a successful example of translating evidence-based HBP management guidelines [13] into an easily adaptable telephone counseling protocol for health professionals working in a linguistically isolated community with limited health resources and information. Given the increasing prevalence of chronic conditions and the costs associated with the care, interventions that demonstrate a positive influence on lifestyle modifications are essential, particularly if they can be implemented in an underserved population such as KAs. It will be important to confirm the cost-effectiveness of this type of intervention approach in the next phase of such investigations.
Acknowledgements
This research was supported by the Agency for Healthcare Research and Quality (R01 HS13160, Clinical Trials Registry NCT00473681).
Footnotes
Conflict of interest
The authors declared no conflict of interest.
References
- [1].Afifi AA, Morisky DE, Kominski GF, Kotlerman JB. Impact of disease management on health care utilization: evidence from the “Florida: A Healthy State (FAHS)” Medicaid Program. Prev Med. 2007;44:547–53. doi: 10.1016/j.ypmed.2007.02.002. [DOI] [PubMed] [Google Scholar]
- [2].Holmes-Rovner M, Stommel M, Corser WD, Olomu A, Holtrop JS, Siddiqi A, Dunn SL. Does outpatient telephone coaching add to hospital quality improvement following hospitalization for acute coronary syndrome? J Gen Intern Med. 2008;23:1464–70. doi: 10.1007/s11606-008-0710-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Woollard J, Burke V, Beilin LJ. Effects of general practice-based nurse-counselling on ambulatory blood pressure and antihypertensive drug prescription in patients at increased risk of cardiovascular disease. J Hum Hypertens. 2003;17:689–95. doi: 10.1038/sj.jhh.1001593. [DOI] [PubMed] [Google Scholar]
- [4].Gerin W, Tobin JN, Schwartz JE, Chaplin W, Rieckmann N, Davidson KW, Goyal TM, Jhalani J, Cassells A, Feliz K, Khalida C, Diaz-Gloster M, Ogedegbe G. The medication Adherence and Blood Pressure Control (ABC) trial: a multi-site randomized controlled trial in a hypertensive, multi-cultural, economically disadvantaged population. Contemp Clin Trials. 2007;28:459–71. doi: 10.1016/j.cct.2007.01.003. [DOI] [PubMed] [Google Scholar]
- [5].Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, Debusk RF. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17:921–7. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- [6].Marquez Contreras E, Vegazo Garcia O, Claros NM, Gil Guillén V, de la Figuera von Wichmann M, Casado Martínez JJ, Fernández R. Efficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension. ETECUM-HTA study. Blood Press. 2005;14:151–8. doi: 10.1080/08037050510008977. [DOI] [PubMed] [Google Scholar]
- [7].Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, Ho BP, Newman RW, McNeil JJ, Coach study group Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003;163:2775–83. doi: 10.1001/archinte.163.22.2775. [DOI] [PubMed] [Google Scholar]
- [8].Hagstrom B, Mattsson B, Rost IM, Gunnarsson RK. What happened to the prescriptions? A single, short, standardized telephone call may increase compliance. Fam Pract. 2004;21:46–50. doi: 10.1093/fampra/cmh110. [DOI] [PubMed] [Google Scholar]
- [9].Bosworth HB, Olsen MK, Gentry P, Orr M, Dudley T, McCant F, Oddone EZ. Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Educ Couns. 2005;57:5–14. doi: 10.1016/j.pec.2004.03.011. [DOI] [PubMed] [Google Scholar]
- [10].Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med. 2007;32:419–34. doi: 10.1016/j.amepre.2007.01.004. [DOI] [PubMed] [Google Scholar]
- [11].Castro CM, King AC. Telephone-assisted counseling for physical activity. Exerc Sport Sci Rev. 2002;30:64–8. doi: 10.1097/00003677-200204000-00004. [DOI] [PubMed] [Google Scholar]
- [12].McBride CM, Rimer BK. Using the telephone to improve health behavior and health service delivery. Patient Educ Couns. 1999;37:3–18. doi: 10.1016/s0738-3991(98)00098-6. [DOI] [PubMed] [Google Scholar]
- [13].National Heart, Lung, and Blood Institute . The seventh report of the joint national committee on detection, evaluation, and treatment of high blood pressure. NIH Publications; Washington, DC: 2003. [PubMed] [Google Scholar]
- [14].He J, Klag MJ, Whelton PK, Chen JY, Mo JP, Qian MC, Mo PS, He GQ. Migration, blood pressure pattern, and hypertension: the Yi Migrant Study. Am J Epidemiol. 1991;134:1085–101. doi: 10.1093/oxfordjournals.aje.a116012. [DOI] [PubMed] [Google Scholar]
- [15].Pollard TM, Carlin LE, Bhopal R, Unwin N, White M, Fischbacher C. Social networks and coronary heart disease risk factors in South Asians and Europeans in the UK. Ethn Health. 2003;8:263–75. doi: 10.1080/1355785032000136452. [DOI] [PubMed] [Google Scholar]
- [16].Mustacchi P. Stress and hypertension. West J Med. 1990;153:180–5. [PMC free article] [PubMed] [Google Scholar]
- [17].Singh LP, Kaur B. Impact of migration, environment and socioeconomic conditions on blood pressure of Sikhs. J Biosoc Sci. 1998;30:155–64. doi: 10.1017/s0021932098001552. [DOI] [PubMed] [Google Scholar]
- [18].U.S. Census Bureau DP-1. Profile of general demographic characteristics. 2000 [updated 2003, accessed 24.11.08] http://www.census.gov/prod/cen2000/index.html.
- [19].Kim MT, Kim KB, Juon HS, Hill MN. Prevalence and factors associated with high blood pressure in Korean Americans. Ethn Dis. 2000;10:364–74. [PubMed] [Google Scholar]
- [20].Kim MT, Juon HS, Hill MN, Post W, Kim KB. Cardiovascular disease risk factors in Korean American elderly. West J Nurs Res. 2001;23:269–82. doi: 10.1177/01939450122045140. [DOI] [PubMed] [Google Scholar]
- [21].Giles T, Aranda JM, Jr, Suh DC, Choi IS, Preblick R, Rocha R, Frech-Tamas F. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens (Greenwich) 2007;9:345–54. doi: 10.1111/j.1524-6175.2007.06432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shin H, Bruno R. Language use and English-speaking ability. 2000 [updated 2003, accessed 8.10.09] http://www.census.gov/prod/2003pubs/c2kbr-29.pdf.
- [23].Yu EY, Choe P. Social and economic indicators by race and Asian ethnic groups and Korean population density map: top 5 metropolitan areas. 2000 [accessed 8.10.09] http://www.calstatela.edu/centers/ckaks/census/Top_5_Metro_Areas.ppt.
- [24].Hipple S. Self-employment in the United States. Mon Labor Rev. 2004:13–23. [Google Scholar]
- [25].Centers for Disease Control and Prevention Health insurance coverage. 2008 [accessed 8.10.09] http://www.cdc.gov/nchs/FASTATS/hinsure.htm.
- [26].Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Public Health. 2004;25:357–76. doi: 10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- [27].Han HR, Kim KB, Kang J, Jeong S, Kim EY, Kim MT. Knowledge, beliefs, and behaviors about hypertension control among middle-aged Korean Americans with hypertension. J Community Health. 2007;32:324–42. doi: 10.1007/s10900-007-9051-y. [DOI] [PubMed] [Google Scholar]
- [28].Kim MT, Kim EY, Han HR, Jeong S, Lee JE, Park HJ, Kim KB, Hill MN. Mail education is as effective as in-class education in hypertensive Korean patients. J Clin Hypertens (Greenwich) 2008;10:176–84. doi: 10.1111/j.1751-7176.2008.07571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Barnes JS, Bennett CE. The Asian population: 2000. U.S. Census Bureau; Washington, DC: 2002. [Google Scholar]
- [30].Braden CJ. Learned self-help response to chronic illness experience: a test of three alternative learning theories. Sch Inq Nurs Pract. 1990;4:23–41. [PubMed] [Google Scholar]
- [31].Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, Gonzalez VM, Laurent DD, Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39:1217–23. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- [32].Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138–61. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- [33].Han HR, Kang J, Kim KB, Ryu JP, Kim MT. Barriers to and strategies for recruiting Korean Americans for community-partnered health promotion research. J Immigr Minor Health. 2007;9:137–46. doi: 10.1007/s10903-006-9022-x. [DOI] [PubMed] [Google Scholar]
- [34].Schroeder K, Fahey T, Hay AD, Montgomery A, Peters TJ. Adherence to anti-hypertensive medication assessed by self-report was associated with electronic monitoring compliance. J Clin Epidemiol. 2006;59:650–1. doi: 10.1016/j.jclinepi.2005.10.013. [DOI] [PubMed] [Google Scholar]
- [35].Schoenthaler A, Ogedegbe G. Patients’ perceptions of electronic monitoring devices affect medication adherence in hypertensive African Americans. Ann Pharmacother. 2008;42:647–52. doi: 10.1345/aph.1K640. [DOI] [PubMed] [Google Scholar]