SUMMARY
Free fibula flap is routinely used for mandibular reconstructions. For contouring the flap, multiple osteotomies should be shaped to reproduce the native mandibular contour. The bone segments should be fixed using a reconstructive plate. This plate is usually manually bent by the surgeon during surgery. This method is efficient, but during reconstruction it is complicated to reproduce the complex 3D conformation of the mandible and recreate a normal morphology with a mandibular profile as similar as possible to the original; any aberration in its structural alignment may lead to aesthetic and function alterations due to malocclusion or temporomandibular disorders. In order to achieve better morphological and functional outcomes, we have performed a customised flap harvest using cutting guides. This study demonstrates how we have performed customised mandibular reconstruction using CAD-CAM fibular cutting guides in 20 patients undergoing oncological segmental resection.
KEY WORDS: Fibula free flap, Mandibular reconstruction, CAD-CAM technique, Cutting guide
RIASSUNTO
Il lembo libero di fibula è routinariamente utilizzato per le ricostruzioni mandibolari. Al fine di ottenere una modellazione del lembo che consenta di ricostruire l'arco mandibolare, sono necessarie multiple osteotomie della fibula. Queste vengono, di norma, eseguite manualmente dal chirurgo; così come la modellazione della placca ricostruttiva che avrà il ruolo di solidarizzare i vari segmenti ossei di fibula. Questo metodo è consolidato, ma ha il difetto di essere incostante in termini di risultati estetici e molto operatore-dipendente. Si ricordi come alterazioni a livello del profilo mandibolare ricostruito costituiscono non solo un difetto estetico, ma possano inficiare anche la funzione articolare e masticatoria. Per queste ragioni vogliamo presentare il nostro workflow CAD-CAM utilizzato in 20 casi di ricostruzioni mandibolari customizzate, in cui il progetto chirurgico virtuale è stato trasferito in sala operatoria mediante l'utilizzo di guide di taglio ossee per la mandibola e la fibula.
Introduction
Free flaps, combining a high success rate with low donor site morbidity, are considered the gold standard for the reconstruction of tissues lost during oncologic surgery 1-3. Free fibula flap is routinely used for large jaw reconstructions 4 5. This can be considered a safe surgical procedure even in elderly head and neck cancer patients 1.
For contouring the flap, multiple osteotomies should be shaped to reproduce the native mandibular contour. The bone segments should be fixed using a reconstructive plate. This plate is usually manually bent by the surgeon during surgery, eventually performing the pre-plating technique using the native mandible as a template, or repositioning template 4-6. This method is efficient, but during reconstruction it is complicated to reproduce the complex 3D conformation of the mandible and recreate a normal morphology with a mandibular profile as similar as possible to the original; any aberration in its structural alignment may lead to aesthetic and function alterations due to malocclusion or temporomandibular disorders.
Modern techniques, such as computer-aided design/computer- aided manufacturing (CAD-CAM), offer new solutions for planning of maxillofacial reconstructive surgery in relation to aesthetic outcomes and the final prosthetic and functional rehabilitation 7.
This study aimed to show how we have performed customised mandibular reconstruction using CAD-CAM fibular cutting guides in 20 patients undergoing oncological segmental resection.
Clinical techniques and technology
CAD-CAM-based mandibular reconstruction procedures using vascularised fibula free flap transfers were performed in 20 cases between 2011 and 2014 at Maxillofacial Surgery Unit of Policlinico "S. Orsola-Malpighi", Bologna, Italy. Histological tumour type, type of mandibular resection and number of fibular segments are summarised in Table I.
Table I.
Histological classification, type of defect and type of flap.
| Patient | Tumour | Resection | Fibula segments |
|---|---|---|---|
| Pt. 1 | Ameloblastoma | B | 1 |
| Pt. 2 | Fibrosarcoma | B+R+C | 2 |
| Pt. 3 | Keratocyst | R+C | 2 |
| Pt. 4 | Ameloblastoma | B+S | 3 |
| Pt. 5 | Squamous cell carcinoma | B+SH | 2 |
| Pt. 6 | Squamous cell carcinoma | S+B+R | 3 |
| Pt. 7 | Osteosarcoma | B+S+B | 3 |
| Pt. 8 | Squamous cell carcinoma | S+B | 2 |
| Pt. 9 | Ameloblastoma | B+S+B | 4 |
| Pt. 10 | Squamous cell carcinoma | C+R+B | 2 |
| Pt. 11 | Squamous cell carcinoma | B | 1 |
| Pt. 12 | Squamous cell carcinoma | B+S | 3 |
| Pt. 13 | Squamous cell carcinoma | B+S+B | 2 |
| Pt. 14 | Squamous cell carcinoma | S+B+R | 3 |
| Pt. 15 | Ameloblastoma | R | 1 |
| Pt. 16 | Aneurysmal cyst | B+S | 3 |
| Pt. 17 | Ameloblastoma | R+B | 3 |
| Pt. 18 | Squamous cell carcinoma | R+B | 3 |
| Pt. 19 | Osteosarcoma | R+B | 3 |
| Pt. 20 | Squamous cell carcinoma | B+S+B | 3 |
C: condyle; R: ramus; B: body; S: symphysis.
Virtual planning and CAD procedures were performed as described previously by our group 3: planning began with the acquisition of a high-resolution CT-scan of the craniofacial region and the lower leg as a donor site.
DICOM format data were processed by the surgeons using CMF software, version 6.0 (Materialise, Lueven, Belgium). Using this software, the surgeon allowed creation of 3D virtual models of the maxillofacial skeleton and the fibula and simulation of mandibular and fibular osteotomies (Fig. 1).
Fig. 1.
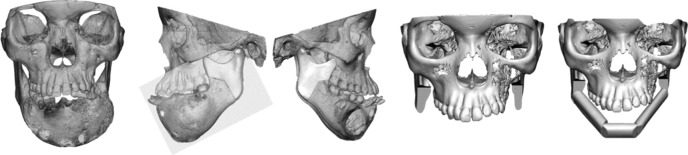
3D virtual models of the mandibular tumour (on the left); virtual simulation of surgical defect and reconstruction planned using three fibular bone segments (on the right).
The planned surgery was used to design and manufacture customised surgical cutting guides for mandible and fibula flap performed by Sintac s.r.l. Trento (Fig. 2).
Fig. 2.
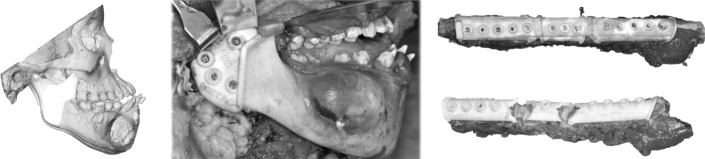
Mandibular (left) and fibular (right) cutting guides used to perform osteotomies, exactly as pre-operatively planned.
The computer-aided design of the surgical device was conducted using Rhino software, version 4.0 (Robert Mc- Neel & Associates, Seattle, WA, USA).
Fibular osteotomy guides were used to allow the free flap to fit the defect accurately, as planned virtually preoperatively (Fig. 3). Reconstructive plates were manufactured by a direct metal laser sintering method, as described previously 3. The customised reconstructive bone plate that supported the fibula free flap was designed by thickening the outer surface of the healthy side of the mandible to obtain an ideal aesthetic contour and avoid bone deformities on the side affected by the tumour. Since the holes of the fixing screws of the guides are the same of those in the bone plate, it is very easy to insert all fibular segments in the final planned position anchored to the reconstructive plate.
Fig. 3.
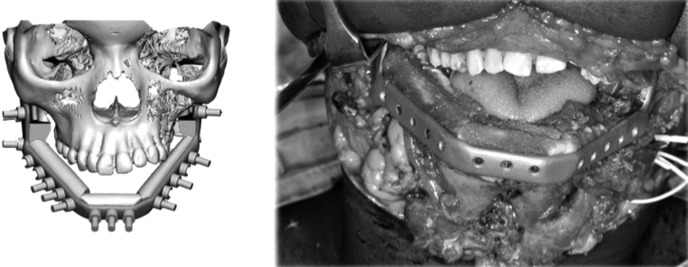
Fibular segments insetting after cutting guide removal.
Linear osteotomies and wedge ostectomies were performed using a piezoelectric device (Fig. 4). No microvascular complications, in terms of partial or total flap loss, were observed in any patient.
Fig. 4.
Bone flap osteotomies performed using piezoelectric saw (Mectron s.p.a.).
Discussion
CAD/CAM technologies have been introduced in the field of maxillofacial bone reconstruction to increase precision and reduce morbidity and operation time 7.
This virtual environment permits ideal pre-surgical planning for reconstruction: native mandibular morphology can be obtained with a very high precision 8. The mandibular cutting guide allowed the site and orientation of the planned osteotomies to be duplicated during surgery.
Moreover, a custom-made cutting guide for the fibular bone helps the surgeon to set the osseous free flap. The straight fibula flap is contoured to resemble the neo-mandible using a surgical cutting guide that is planned, choosing the fibular osseous fragment virtually and the orientation that is most suitable for future implanted-supported prosthesis insertion. In mandible-wide reconstruction, it is possible to accurately measure the length of the bone component of the free flap and the extent of the vascular pedicle.
Fibular bone segmentation, using a cutting guide and a piezoelectric saw, can be safely performed. Performing piezoelectric osteotomies, the surgeon achieves better procedural control and increases the precision of bone segmentation. The use of a cutting guide and piezoelectric saw significantly reduce the risk of damaging the vascular bundle that runs along the bone. The continuity of the periosteum was preserved and the vascular bundle was not dissected off or protected during the osteotomy. The fact that microvascular failure of the vascularised bone segments was absent in this series, including when the segment's length was very short, is consistent with the hypothesis of less thermal and mechanical damage after osteotomies with piezosurgery compared with traditional saw damage.
Each segment can be readily osteotomised because both the length and the cutting angle are precisely indicated by the guide. This consistently reduces sectioning time and allows the surgeon to section the fibula into units less than 3.0 cm long, affording a better morphological result upon reconstruction. Our microvascular success rate was 100%, confirming the safety of the procedure.
The morphological results are significantly better than those achieved with standard technique (Fig. 5).
Fig. 5.
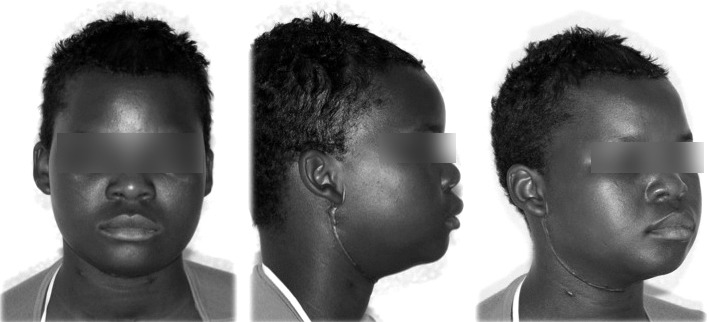
Post-operative morphological appearance in a patient who underwent subtotal mandibulectomy and reconstruction using CAD-CAM technique.
Last but not least, an advantage of the CAD-CAM protocol is that it can be used to educate fellow reconstructive surgeons. The availability of precise cutting guides for bone sectioning make performance of good surgery possible, even by surgeons at the beginning of their learning curves.
There are also some difficulties/limits that surgeons may encounter during surgery using this method that should kept in mind: when a skin paddle is necessary for a composite reconstruction, it may be difficult to pre-operatively plan the correct position of the guide in relation to the musculocutaneous perforators. In our series, only one case needed an osteocutaneous flap and in this case the perforator vessels were identified by angiography-CT of the leg. However, this could be a limitation of the proposed technique.
In conclusion, the new techniques facilitate all steps that, in the past, required highly skilled operators to restore correct anatomy by manually sectioning the fibula and inserting bone using a manually bent standard bone plate.
References
- 1.Tarsitano A, Pizzigallo A, Sgarzani R, et al. Head and neck cancer in elderly patients: is microsurgical free-tissue transfer a safe procedure? Acta Otorhinolaryngol Ital. 2012;32:371–375. [PMC free article] [PubMed] [Google Scholar]
- 2.Deganello A, Gitti G, Parrinello G, et al. Cost analysis in oral cavity and oropharyngeal reconstructions with microvascular and pedicled flaps. Acta Otorhinolaryngol Ital. 2013;33:380–387. [PMC free article] [PubMed] [Google Scholar]
- 3.Baj A, Beltramini GA, Demarchi M, et al. Extended-pedicle peroneal artery perforator flap in intraoral reconstruction. Acta Otorhinolaryngol Ital. 2013;33:282–285. [PMC free article] [PubMed] [Google Scholar]
- 4.Pellini R, Mercante G, Spriano G. Step-by-step mandibular reconstruction with free fibula flap modelling. Acta Otorhinolaryngol Ital. 2012;32:405–409. [PMC free article] [PubMed] [Google Scholar]
- 5.Tarsitano A, Sgarzani R, Betti E, et al. Vascular pedicle ossification of free fibular flap: is it a rare phenomenon? Is it possible to avoid this risk? Acta Otorhinolaryngol Ital. 2013;33:307–310. [PMC free article] [PubMed] [Google Scholar]
- 6.Berrone M, Crosetti E, Succo G. Repositioning template for mandibular reconstruction with fibular free flaps: an alternative technique to pre-plating and virtual surgical planning. Acta Otorhinolaryngol Ital. 2014;34:278–282. [PMC free article] [PubMed] [Google Scholar]
- 7.Tarsitano A, Mazzoni S, Cipriani R, et al. The CAD-CAM technique for mandibular reconstruction: An 18 patients oncological case-series. J Craniomaxillofac Surg. 2014;42:1460–1464. doi: 10.1016/j.jcms.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 8.Ciocca L, Marchetti C, Mazzoni S, et al. Accuracy of fibular sectioning and insertion into a rapid-prototyped bone plate, for mandibular reconstruction using CAD-CAM technology. J Craniomaxillofac Surg. 2015;43:28–33. doi: 10.1016/j.jcms.2014.10.005. [DOI] [PubMed] [Google Scholar]



