SUMMARY
Orbital approaches provide significant trajectory to the skull base and are used with differently designed pathways. The aim of this study is to investigate the feasibility of a combined transorbital and transnasal approach to the anterior and middle cranial fossa. Cadaveric dissection of five silicon-injected heads was used. A total of 10 bilateral transorbital approaches and 5 extended endonasal approaches were performed. Identification of surgical landmarks, main anatomical structures, feasibility of a combined approach and reconstruction of the superior orbital defect were examined. Rod lens endoscope (with 0° and 45° lenses) and endoscopic instruments were used to complete the dissection. The transorbital approach showed good versatility and provides the surgeon with a direct route to the anterior and middle cranial fossa. The transorbital avascular plane showed no conflict with major nerves or vessels. Large exposure area from crista galli to the third ventricle was demonstrated with significant control of different neurovascular structures. A combined transorbital transnasal approach provides considerable value in terms of extent of exposure and free hand movement of the two surgeons, and allows better visualisation and control of the ventral skull base, thus overcoming the current surgical limits of a single approach. Combination of these two minimally invasive approaches should reduce overall morbidity. Clinical trials are needed to evaluate the virtual applications of this approach.
KEY WORDS: Skull base, Transorbital, Transnasal, Endoscopic, Reconstruction, Minimally invasive
RIASSUNTO
Gli approcci transorbitari permettono di ottenere un'ampia via d'accesso al basicranio e sono utilizzati in diverse procedure chirurgiche. Lo scopo di questo studio è valutare la fattibilità di un approccio endoscopico combinato transobitario e transnasale alla fossa cranica anteriore e media. Su cinque teste iniettate con silicone, sono stati eseguiti un totale di 10 approcci endoscopici transorbitari e 5 "extended endonasal approach" (EEA). Durante le procedure sono stati identificati i punti di repere chirurgici e le strutture anatomiche principali, valutando la fattibilità dell'approccio combinato e della successiva ricostruzione del tetto orbitario. Per eseguire la dissezione sono stati utilizzati endoscopi rigidi con sistema a lente cilindrica 0° e 45° e una strumentazione endoscopica dedicata. L'approccio transorbitario ha mostrato grande versatilità ed ha permesso al chirurgo di ottenere un corridoio diretto alla fossa cranica anteriore e media. Il piano transorbitario avascolare non era in conflitto con vasi o nervi maggiori. La dissezione ha mostrato una vasta esposizione del basicranio, dalla crista galli fino al terzo ventricolo, assicurando un controllo efficace sulle strutture neurovascolari circostanti. L'approccio combinato transorbitario e transnasale ha portato dei vantaggi significativi sia nell'ampiezza dell'esposizione che nella manovrabilità della strumentazione chirurgica. L'approccio endoscopico combinato transnasale e transorbitario ha dimostrato una migliore visualizzazione del basicranio ventrale e di poter superare alcune attuali limitazioni dei due singoli approcci. Inoltre la combinazione di due approcci mini-invasivi dovrebbe contribuire a ridurre la morbilità chirurgica. Sono tuttavia necessari studi clinici per validare questo approccio..
Introduction
Several approaches to ventral anterior and middle cranial fossa have been described 1. In recent years, the indications of extended endonasal approach have rapidly expanded to include a wide spectrum of central skull base pathologies 2 3. With all the merits of this approach, it allows limited access to lesions that are crossing neurovascular structures or laterally seated 4 5. Diminished visualisation in such cases might lead to incomplete resection or devastating complications. Comparatively, traditional external approaches have wide exposure and control of the lesion, but are associated with increased postoperative functional and cosmetic sequelae. Thus, the need for a technique that minimises the morbidity of endonasal and external approaches without compromising resectability is desired.
Transorbital approaches have been used to treat orbital lesions 6-8. The peculiar position and extent in the ventral skull base place the orbit in the limelight as a desirable corridor to the skull base.
Ciporen and Moe et al. demonstrated four transorbital approaches in which each of targeted different area of the skull base 9 10.
Herein, we demonstrate the feasibility of combined endonasal and transorbital approach to the anterior and middle cranial base along with evaluation of skull base reconstruction.
Materials and methods
Five cadaveric specimens (10 sides) with intravascular injection of colored silicone were dissected in the anatomy laboratory of University of Tubingen Medical Center following approval by the local institutional ethics board.
Rod-lens Hopkins endoscopes (Karl Storz, Tuttlingen Germany) of 4 mm in diameter and 18 cm in length were used with 0° and 45° lenses and were coupled to a high-definition cameras and monitors (Karl Storz, Tuttlingen Germany). High-speed drills with straight and angled hand pieces, and diamond and cutting burrs were used along with paranasal sinus and skull base endoscopic instruments (Karl Storz, Tuttlingen, Germany). All procedures were documented by high definition camera and AIDA recording system (Karl Storz, Tuttlingen, Germany). A total of 15 procedures were performed, five extended endonasal approaches and 10 bilateral transorbital approaches. Two surgeons dissected the specimens in parallel, standing on both sides of the specimen and using two endoscopes and monitors. One surgeon performed the endonasal approach, while the other performed the transorbital approach.
Surgical steps
The extended endonasal approach was performed on 5 specimens. Bilateral wide maxillary antrostomy, bilateral complete spheno-ethmoidectomy, septectomy, frontal sinosotomy (Draf type III) followed by transcribriform, transplanum, transtuberculum, and transsellar resection were performed in all specimens. Additionally, each specimen underwent a transorbital approach through transpalpebral incision. Transverse supratarsal skin incision was around 10 mm above the upper eyelid edge. The incision went through orbicularis muscle as well. To ovoid injury of the orbital septum, the myo-cutaneous flap was dissected and elevated superiorly and tangentially to orbicularis muscle until reaching the superior bony orbital rim (Fig. 1). The periostium was cut against the bone of the orbital rim to create the plane for superior orbital wall dissection. Attention must be paid in preserving the supraorbital and supratrochlear neurovascular bundles, which are situated at the junction of medial 1/3 and lateral 2/3 of superior orbital rim. The periorbita was preserved and dissected down carefully by an elevator until reaching the anterior and posterior ethmoidal arteries medially, optic nerve posteriorly and superior orbital fissure posterolaterally (Fig. 2). Subsequently, a 0° endoscope was introduced to control the subsequent steps. Mini-craniectomy was performed in the weakest point of superior orbital wall using a high-speed diamond drill. A piece of silastic sheet was applied to protect the orbit during this step and a malleable retractor pushed the orbit downwards to gain space. Widening of the craniectomy was accomplished using Kerrison punch forceps. The medial limit for the craniectomy was the anterior and posterior ethmoidal arteries. The medial orbital wall and lateral portion of the fovea ethmoidalis were preserved to support the skull base reconstruction. The dura was then incised carefully at the edges of the craniectomy.
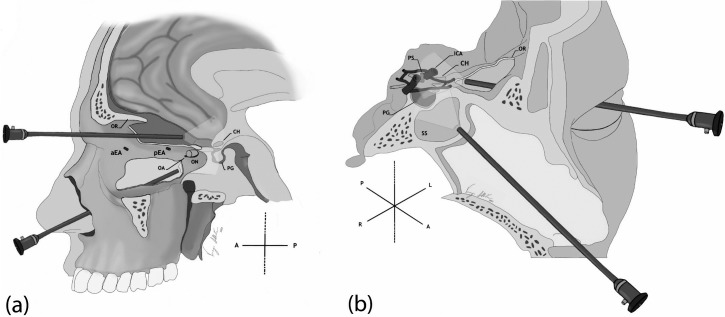
Fig. 1.
Left eye 3D cross-section view shows the plane of the transorbital approach and the supratarsal skin incision that is 10 mm above the tarsus, extending from the middle third of the upper eyelid to the lateral cantus. (A) Elevated muscolocutaneous flap, (B) dashed line shows the correct septal incision that reach the subperiosteal orbital roof plane, (C) levator palpebrae superioris, (D) superior tarsal muscle (Müller muscle).
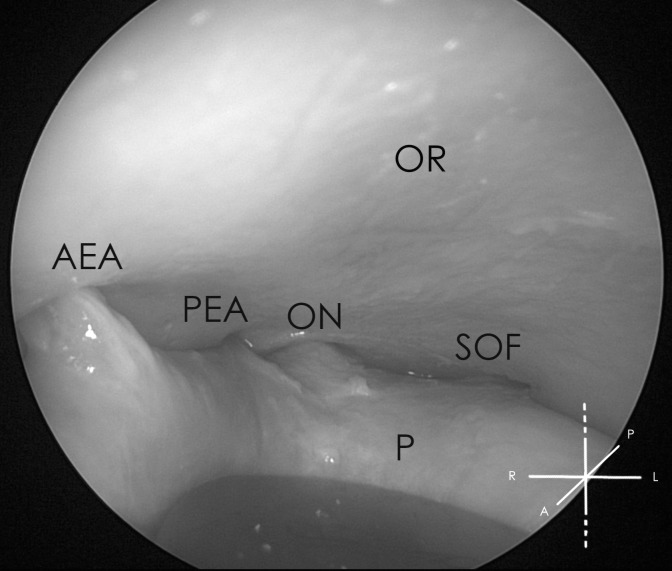
Fig. 2.
Endoscopic view of the left eye shows the major landmarks for designing the craniectomy in the orbital roof (OR): anterior ethmoidal artery (AEA), posterior ethmoidal artery (PEA), optic nerve (ON) and superior orbital fissure (SOF). Malleable retractor applies pressure over the periorbita (P).
Transorbital intracranial endoscopic exploration was carried out to identify the important anatomical structures that can be reached. The ipsilateral and contralateral anterior cranial fossa were explored as well as the middle cranial fossa.
Thereafter, endonasal and transorbital combined exploration was performed by two surgeons through the two approaches to identify structures in the anterior and middle cranial fossa jointly. One surgeon had the access through an endonasal route with an independent monitor and the other has access through a transorbital route with another independent monitor. Accessibility and visualisation of important structures were assessed during this step. Cooperative dissection was performed in the form of bone drilling, precise cutting of the dura and handling important structures such as the optic nerve, cavernous/supra-clinoid internal carotid artery (ICA) and sellar/suprasellar structures. The surgeons alternated the rules and instruments during this part to assess the range of motion and maneuverability. Visualization through one route and dissection through the other or combined dissection were all performed.
A multilayer technique was used for skull base reconstruction. Intracranial intradural layer with synthetic graft was used followed by muco-periosteal septal graft that was used in overlay fashion to cover the superior orbital wall defect.
The main outcome measure of this study was to determine the feasibility of this combined approach in the anterior and middle cranial fossa by assessing the extent of the dissection, the ability to synchronously work intracranially and to perform superior orbital wall reconstruction.
Results
The transorbital endoscopic approach provides the surgeon with a direct route to the anterior and middle cranial fossa. The endoscopic plane is at the same level of the structures of the ventral skull base. Intracranial intradural exploration with 0° and 45° endoscopes demonstrated the accessibility of different areas. The following structures can be seen from anterior to posterior direction: posterior wall of frontal sinus, crista galli, frontal lobe, cribriform plate, olfactory tract, planum sphenoidal, tuberculum sella, anterior/posterior clinoid process, cavernous ICA, supraclinoid ICA, anterior communicating artery, diaphragmatic sella, pituitary gland, hypophyseal stalk, superolateral portion of cavernous sinus, oculomotor nerve, optic nerve, optic chiasm, optic tract and intracranial cisterns (chiasmatic, carotid, sylvian and lamina terminalis) (Fig. 3).
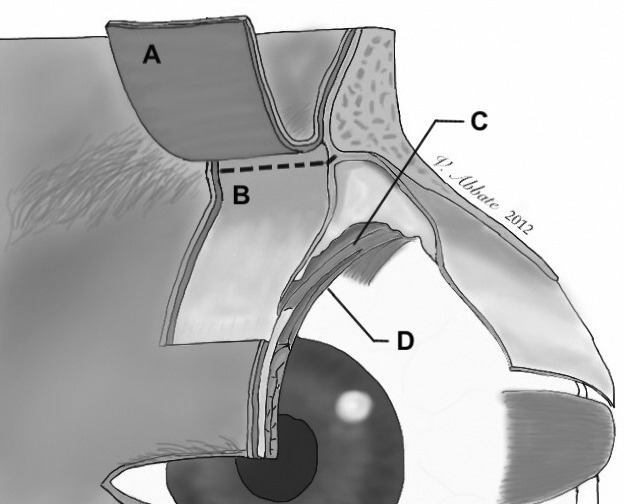
Fig. 3.
Endoscopic intracranial intradural exploration through superior orbital wall craniectomy. a) Right-sided anterior cranial fossa is viewed using a 45° endoscope. A curved probe is used along with an angled endoscope; b) by using a 0° endoscope on the right side, major neurovascular structures can be approached immediately once passing the craniectomy without crossing major structures. The supraclinoid internal carotid artery (ICA), optic nerve (ON) and cavernous sinus are easily visualised; c) left-sided middle cranial fossa is widely accessible with using 0° endoscope. Lesions involving or crossing optic nerve or ICA can be clearly visualised through this approach. (CG) crista galli, (CP) cribriform plate, (PS) planum sphenoidale, (OR) orbital roof, (CNIII) third cranial nerve, (OT) optic tract, (CH) optic chiasm, (PC) posterior clinoid process and (A1) pre-communicating artery.
The transnasal extended approach combined with a transorbital endoscopic approach showed higher visualisation and tissue handling than either single approach alone. The combined approach also provided the surgeon with full visualisation and control of the optic nerve and supraclinoid carotid. Bi-portal intracranial cooperative dissection between the two surgeons was excellent in terms of the capability of lightening deep-seated structures, exchanging roles in dissection and assistance in skull base reconstruction.
Meticulous incision and myo-cutaneous flap elevation is essential to avoid orbital complications. Keeping the plane just under orbicularis oculi muscle will prevent injury to the septum. Preserving the orbital septum makes injury of levator palpebrae superioris muscle or periorbita markedly avoidable. The plane of dissection is avascular which eases flap elevation.
The anterior and posterior ethmoidal arteries are considered landmarks for the medial limit of the craniectomy except in case of pneumatised supraorbital recess. A preoperative CT scan and CT navigation system can help in localising the proper site of craniectomy. However, the size and location of the craniectomy can be adjusted according to the pathology.
We found that standard skull base instruments are satisfactory in the combined approach. However, in order to protect the orbit from introducing angled instruments and to minimise the size of craniectomy, specially designed instruments, such as straight malleable-tips instruments, should be available.
Orbital roof reconstruction with multilayer technique was adequate. The endonasal skull base reconstruction follows the regular principles that have been explained in the literature 11.
Discussion
The transorbital endoscopic approach to the skull base provides a panoramic view of frontobasal area. Through variable size craniectomy in the superior orbital wall, the surgeon can access a wide range of structures in the anterior- posterior axis from posterior wall of frontal sinus to the third ventricle and from para-median to lateral position. Designing the craniectomy to be in close-distance allows early cerebrospinal fluid (CSF) release by opening the cisterns before dissecting the pathology. As a result, frontal lobe sinks spontaneously due to gravity-related relaxation will minimise brain retraction. In addition, performing craniectomy close to the lesion permits short working distance to the tumour without crossing neurovascular structures. Furthermore, transorbital access to the anterior and posterior ethmoidal arteries is possible at the very beginning of the procedure. Thus, ligation of these arteries devascularises the lesion early.
The transnasal transorbital endoscopic combined approach improves visualisation of the field (Fig. 4). One of the merits of this combined approach is control of optic nerve and supraclinoid ICA in the form of 360° visualisation. This advantage is of utmost importance in cases of lesions that might extend laterally or superiorly crossing specifically optic nerve or ICA. Creating a bone window just anterior to the optic nerve along with the transnasal approach permits a direct 4-wall access to the nerve.
Fig. 4.
Cross-sectional a) sagittal and b) parasagittal view show the visual field of the two endoscopes with the combined transorbital and transnasal approach. To allow a correct view, the orbital content and part of the lamina papyracia have been removed in (a). Transorbital approach provides coplanar trajectory of skull base while endonasal view provide basal control. (OR) orbital roof, (aEA) anterior ethmoid artery, (pEA) posterior ethmoid artery, (OA) ophthalmic artery, (ON) optic nerve, (PG) pituitary gland, (CH) optic chiasma, (PS) pituitary stalk, (SS) sphenoid sinus, (ICA) internal carotid artery.
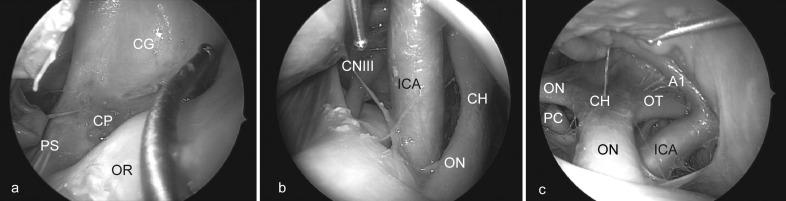
Synchronous work of two surgeons through 2 portals and 2 endoscopes with 2 monitors helps in dissection, visualisation and guiding each other (Fig. 5). Alternating instruments and the roles between the two surgeons was significantly beneficial. Standing of the surgeons on each side of the patient's head while one works through an endonasal route and the other through a contralateral transorbital route creates a large working space between the two surgeon's hands and promotes better maneuverability and freedom that is not provided by a single portal. The "two-team" concept is strengthened since there is no conflict of hands in the operative field.
Fig. 5.
Illustration of the position of the two surgeons during the dissection, one surgeon on the right side using a transnasal corridor and the other surgeon on the left side using a transorbital corridor. Note the space in the operative field that enables the surgeons to move freely without crossing each other.
The additional advantages of this approach are excellent cosmetic results since the incision is within the eyelid natural wrinkle lines, applicable effective skull base reconstruction, less expected morbidity and minimum need for post-operative intensive care admission as well as total days of hospitalisation.
A variety of benign and malignant tumours could be addressed efficiently with these combined corridors like craniopharyngioma, pituitary macroadenoma and meningioma (especially spheno-orbital type).
An expanded endonasal approach is now well recognised as part of the armamentarium of surgical techniques in central skull base surgery 12-16. However, extension of lesions lateral to the central part of the skull base, lesions bounding important neurovascular structures, large-size lesions and poor visualisation in some areas are some limitations of this approach 17-21. For such cases, combined external approach is needed for better control 3 4 22. Many traditional external techniques have been described to manage lesions in the anterior and middle cranial fossa, but significant complications have been reported 7 23-27.
The concept of minimally invasive surgery was behind the initiation of keyhole techniques such as the supraorbital approach. Perneczky and others introduced eyebrow incision that provides endoscopic and microscopic large exposure of the operative field through a small craniectomy 28-34. However, this approach carries some disadvantages that are related to the approach and not to the use of the endoscope. Some of the these disadvantages are: scalp anaesthesia due to supratrochlear or supraorbital injury, transient postoperative frontalis muscle palsy due to risk of frontal branch of facial nerve injury, CSF fistula through an occult frontal sinus opening or frontal sinusitis and mucocele as a consequence of inadvertent traversing frontal sinus 30 35. Cosmetic results of inappropriate fixation of the bone flap or improper clogging of the burrhole and saw lines should be considered as well. Hyper-pneumatised frontal sinus with lateral extension is a major limit for this approach 30.
Utilising a transorbital corridor to reach the orbital roof while preserving orbital rim has been studied by Moe et al. 10. They described four transorbital corridors to different areas, namely: superior eyelid crease, lateral retrocanthal, medial precaruncular and preseptal lower eyelid corridors. They reported successful results without significant neurological, orbital or medical complications in the 20 transorbital procedures that were recorded in their series 9.
Maximum attention should be taken to the orbit when performing the approach. Use of corneal protector or transient tarsorrhaphy, applying silastic sheet or malleable retractor for the periorbita, watchful insertion of instruments and periodic relief of the globe pressure will minimise the risk of unfavourable orbital morbidity 10 36. With careful manipulation of the globe, morbidity is almost negligible. In contrast to what we expect, the globe can withstand certain pressures even for long procedures 36.
There are some limitations to this approach. It needs a well-qualified team of both an otolaryngologist experienced in rhinology and a neurosurgeon with endoscopic skull base and vascular experience. The anatomical limitation of this approach is the degree of supraorbital recess pneumatisation. In case of high pneumatisation posteriorly and laterally, the craniectomy might be limited and another approach should be used 37. Lateral extension of frontal sinus should not be a restriction for this approach, but rather for the supraorbital craniectomy approach 30.
Ultimately, clinical trials could endorse this concept and clinically validate the safety and practicality of the combined approach. Thereafter, comparative studies of the different endoscopic approaches to the anterior and middle cranial fossa should follow.
Conclusions
In selected cases, the possibility of minimally invasive skull base surgery can be provided with a transorbital transnasal endoscopic combined approach. Wide range of exposure from posterior wall of frontal sinus to the retrosellar area can be demonstrated. Direct trajectory, clear visualisation and synchronous dissection between the two surgeons are a fruitful aspect of this approach. Multidisciplinary work and careful orbital manipulation will minimise the risk of orbital complications. Clinical applications and limitations can be verified clearly with further clinical review.
References
- 1.Rachinger W, Grau S, Tonn JC. Different microsurgical approaches to meningiomas of the anterior cranial base. Acta Neurochir (Wien) 2010;152:931–939. doi: 10.1007/s00701-010-0646-1. [DOI] [PubMed] [Google Scholar]
- 2.Castelnuovo P, Dallan I, Battaglia P, et al. Endoscopic endonasal skull base surgery: past, present and future. Eur Arch Otorhinolaryngol. 2010;267:649–663. doi: 10.1007/s00405-009-1196-0. [DOI] [PubMed] [Google Scholar]
- 3.Nicolai P, Battaglia P, Bignami M, et al. Endoscopic surgery for malignant tumors of the sinonasal tract and adiacent skull base: a 10-year experience. Am J Rhinol. 2008;222:308–316. doi: 10.2500/ajr.2008.22.3170. [DOI] [PubMed] [Google Scholar]
- 4.Castelnuovo P, Belli E, Bignami M, et al. Endoscopic nasal and anterior craniotomy resection for malignant nasoethmoid tumors involving the anterior skull base. Skull Base. 2006;16:15–18. doi: 10.1055/s-2005-922095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snyderman CH, Carrau RL, Kassam AB, et al. Endoscopic skull base surgery: principles of endonasal oncological surgery. J Surg Oncol. 2008;97:658–664. doi: 10.1002/jso.21020. [DOI] [PubMed] [Google Scholar]
- 6.Chu EA, Quinones-Hinojosa A, Boahene KD. Trans- blepharoplasty orbitofrontal craniotomy for repair of lateral and posterior frontal sinus cerebrospinal fluid leak. Otolaryngol Head Neck Surg. 2010;142:906–908. doi: 10.1016/j.otohns.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Raza SM, Conway JE, Li KW, et al. A modified frontal-nasal- orbital approach to midline lesions of the anterior cranial fossa and skull base: technical note with case illustrations. Neurosurg Rev. 2010;33:63–70. doi: 10.1007/s10143-009-0222-4. [DOI] [PubMed] [Google Scholar]
- 8.Raza SM, Quinones-Hinojosa A, Lim M, et al. The transconjunctival transorbital approach: a keyhole approach to the midline anterior skull base. World Neurosurg. 2013;80:864–871. doi: 10.1016/j.wneu.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciporen JN, Moe KS, Ramanathan D, et al. Multiportal endoscopic approaches to the central skull base: a cadaveric study. World Neurosurg. 2010;73:705–712. doi: 10.1016/j.wneu.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 10.Moe KS, Bergeron CM, Ellenbogen RG. Transorbital neuroendoscopic surgery. Neurosurgery. 2010;67(3 Suppl Operative):16–28. doi: 10.1227/01.NEU.0000373431.08464.43. [DOI] [PubMed] [Google Scholar]
- 11.Locatelli D, Rampa F, Acchiardi I, et al. Endoscopic endonasal approaches for repair of cerebrospinal fluid leaks: nineyear experience. Neurosurgery. 2006;58(Suppl 2):246–256. doi: 10.1227/01.NEU.0000193924.65297.3F. discussion 256-7. [DOI] [PubMed] [Google Scholar]
- 12.AlQahtani A, Turri-Zanoni M, Dallan I, et al. Endoscopic endonasal resection of sinonasal and skull base malignancies in children: feasibility and outcomes. Childs Nerv Syst. 2012;28:1905–1910. doi: 10.1007/s00381-012-1866-x. [DOI] [PubMed] [Google Scholar]
- 13.AlWeri A, Jho HD. Endoscopic endonasal approaches to the cavernous sinus: surgical approaches. Neurosurgery. 2001;49:354–360. doi: 10.1097/00006123-200108000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Dave S, Bared A, Casiano RR. Surgical outcomes and safety of transnasal endoscopic resection for anterior skull tumors. Otolaryngol Head Neck Surg. 2007;136:920–927. doi: 10.1016/j.otohns.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Lund VJ, Stammberger H, Nicolai P, et al. European Rhinologic Society Advisory Board on endoscopic techniques in the management of nose, paranasal sinus and skull base tumors: European position paper on endoscopic management of tumors of the nose, paranasal sinuses and skull base. Rhinol Suppl. 2010;22:1–143. [PubMed] [Google Scholar]
- 16.Nicolai P, Castelnuovo P, Lombardi D, et al. Role of endoscopic surgery in the management of selected malignant epithelial neoplasms of the naso-ethmoidal complex. Head Neck. 2007;29:1075–1082. doi: 10.1002/hed.20636. [DOI] [PubMed] [Google Scholar]
- 17.Berhouma M, Jacquesson T, Jouanneau E. The fully endoscopic supraorbital trans-eyebrow keyhole approach to the anterior and middle skull base. Acta Neurochir (Wien) 2011;153:1949–1954. doi: 10.1007/s00701-011-1089-z. [DOI] [PubMed] [Google Scholar]
- 18.Dehdashti AR, Ganna A, Witterick I, et al. Expanded endoscopic endonasal approach for anterior cranial base and suprasellar lesions: indications and limitations. Neurosurgery. 2009;64:677–687. doi: 10.1227/01.NEU.0000339121.20101.85. [DOI] [PubMed] [Google Scholar]
- 19.Divitiis E, Cavallo LM, Esposito F, et al. Extended endoscopic transsphenoidal approach for tuberculum sellae meningiomas. Neurosurgery. 2008;62(Suppl 3):1192–1201. doi: 10.1227/01.neu.0000333785.04435.2c. [DOI] [PubMed] [Google Scholar]
- 20.Kasemsiri P, Carrau RL, Prevedello DM, et al. Indications and limitations of endoscopic skull base surgery. Future Neurology. 2012;7:263–277. [Google Scholar]
- 21.Snyderman CH, Pant H, Carrau RL, et al. What are the limits of endoscopic sinus surgery? The expanded endonasal approach to the skull base. Keio J Med. 2009;58:152–160. doi: 10.2302/kjm.58.152. [DOI] [PubMed] [Google Scholar]
- 22.Batra PS, Citardi MJ, Worley S, et al. Resection of anterior skull base tumors: Comparison of combined traditional and endoscopic techniques. Am J Rhinol. 2005;19:521–528. [PubMed] [Google Scholar]
- 23.Al-Mefty O. Supraorbital-pterional approach to skull base lesions. Neurosurgery. 1987;21:474–477. doi: 10.1227/00006123-198710000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Burduk PK, Kaźmierczak W, Dalke K, et al. Craniofacial resection for tumors of paranasal sinuses involving the anterior skull base. Otolaryngol Pol. 2012;66:96–101. doi: 10.1016/S0030-6657(12)70755-2. [DOI] [PubMed] [Google Scholar]
- 25.Elbabaa SK, Al-Mefty O. Craniofacial approach for anterior skull-base lesions. Atlas Oral Maxillofac Surg Clin North Am. 2010;18:151–160. doi: 10.1016/j.cxom.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Wang T, Wang X, Li M, et al. Surgical approaches of anterior skull base tumors. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007;21:50–51. [PubMed] [Google Scholar]
- 27.Ganly I, Patel SG, Singh B, et al. Complications of craniofacial resection for malignant tumors of the skull base: Report of an International Collaborative Study. Head Neck. 2005;27:445–451. doi: 10.1002/hed.20166. [DOI] [PubMed] [Google Scholar]
- 28.Melamed I, Merkin V, Korn A, et al. The supraorbital approach: an alternative to traditional exposure for the surgical management of anterior fossa and parasellar pathology. Minim Invasive Neurosurg. 2005;48:259–263. doi: 10.1055/s-2005-915603. [DOI] [PubMed] [Google Scholar]
- 29.Obeid F, Al-Mefty O, et al. Recurrence of olfactory groove meningiomas. Neurosurgery. 2003;53:534–542. doi: 10.1227/01.neu.0000079484.19821.4a. [DOI] [PubMed] [Google Scholar]
- 30.Kabil MS, Shahinian HK. Application of the supraorbital endoscopic approach to tumors of the anterior cranial base. J Craniofac Surg. 2005;16:1070–1074. doi: 10.1097/01.scs.0000198624.46501.e0. [DOI] [PubMed] [Google Scholar]
- 31.Andaluz N, Romano A, Reddy LV, et al. Eyelid approach to the anterior cranial base. J Neurosurg. 2008;109:341–346. doi: 10.3171/JNS/2008/109/8/0341. [DOI] [PubMed] [Google Scholar]
- 32.Feiz-Erfan I, Spetzler RF, Horn EM, et al. Proposed classification for the transbasal approach and its modifications. Skull Base. 2008;18:29–47. doi: 10.1055/s-2007-994292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jallo GI, Bognar L. Eyebrow surgery: the supraciliary craniotomy: technical note. Neurosurgery. 2006;59:E157–E158. doi: 10.1227/01.NEU.0000220045.23743.80. [DOI] [PubMed] [Google Scholar]
- 34.Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005;57:242–255. doi: 10.1227/01.neu.0000178353.42777.2c. [DOI] [PubMed] [Google Scholar]
- 35.Owusu Boahene KD, Lim M, Chu E, et al. Transpalpebral orbitofrontal craniotomy: a minimally invasive approach to anterior cranial vault lesions. Skull Base. 2010;20:237–244. doi: 10.1055/s-0030-1249247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sellari-Franceschini S, Lenzi R, Santoro A, et al. Lateral wall orbital decompression in Graves' orbitopathy. Int J Oral Maxillofac Surg. 2010;39:16–20. doi: 10.1016/j.ijom.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Gardner PA, Kassam AB, Rothfus WE, et al. Preoperative and intraoperative imaging for endoscopic endonasal approaches to the skull base. Otolaryngol Clin N Am. 2008;41:215–230. doi: 10.1016/j.otc.2007.10.010. 915-8. [DOI] [PubMed] [Google Scholar]