Abstract
Background
Pressure ulcers are frequent complications for long term hospitalized bed-ridden patients which are not able to move or move very little. In fact, the lesion forms in a skin and muscle region which undergoes a constant pressure between an underlying bone protrusion and a support structure such as a bed or a wheelchair. Initially only the outer layers are involved but in time, the ulcer can spread to the deeper structures and reach the bone.
Patients and methods
In our work we described the anatomical areas that are most often subject to developing a pressure ulcer and we considered the surgical treatment and reconstructive procedures which are applied using a logical and rigorous sequence.
Results
We considered 4 clinical cases (2 ischiatic sores, 1 sacral sore and 1 gluteal-trochanteric sore) which demonstrate the surgical treatment and the reconstructive pro-cedures.
Conclusions
It is crucial to cover the defects with a thick flap to give more support and protection to the areas which undergo pressure and to lower the incidence of recurrences.
Keywords: Pressure ulcers, Pressure sores, Reconstruction, Flaps
Introduction
A pressure ulcer is a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear (1). The continuous pressure leads initially to ischemia and subsequently to the necrosis of the interested area. Pressure ulcers of the ischial, sacral and trochanteric region are the most frequent sores, accounting for 62%.
According to the NPUAP classification, the pressure ulcers that have to be surgically treated are those in Stage 3 and Stage 4 (2). Ulcers comprised in lower stages will be kept under observation and all measures of prevention will be applied. Nonetheless, these ulcers evolve into more serious forms that will eventually need surgery. Stage 2 ulcers can be repaired with skin grafts.
Sacral, ischial and trochanteric ulcers are the most difficult to treat (3, 4). These pressure sores mostly occur in wheel-chair bound patients, due to their impossibility to actively change position, exposing the patients to several recurrences also after successful surgery. In addition, the general conditions of the patients are often complicated by bad nutrition and local and systemic infections. All of these factors make challenging to achieve a successful surgical treatment without long term recurrences (5–7).
In this paper we described the surgical techniques and reconstructive procedures of four cases of pressure ulcers and discussed the surgical options based on the anatomical regions involved.
Patients and methods
Ischial ulcers
Surgical treatment: the procedure will start by marking on the skin the true margins of the ulcer. An elliptical incision, which runs parallel to the gluteal fold, is practiced around the ulcer with a margin of 0.5–1 cm. Healthy skin must be totally preserved. Sharp excision is used to remove completely, in full thickness, the bursa and scar tissue. The incision is extended in depth up to the periosteum of the ischial tuberosity. Using a mallet and a curved osteotome introduced through the upper margin of the wound, the ischial prominence and the ulcer are removed as a whole (“en bloc excision”). The wound is then washed with a 10% betadine solution and a sodium chloride solution and checked for eventually spotting of bleeding points.
Reconstructive procedures: if the ulcer is promptly treated and/or sufficiently shallow, a direct closure can be performed. Direct closure can also be performed in the case of a deep but small ulcer with sufficient whole adjacent tissue without causing excessive tension on the skin. A flap is needed for reconstruction after en bloc excision with partial or total ostectomy. The elective technique is a skin flap with interposition of muscle. The semitendinous, semimembranous, biceps femoris and gluteus maximus are the muscles most frequently used for reconstruction and a big thigh skin flap is lifted in order to expose the muscles to be used. According to the dimension of the defect that has to be repaired, one or more muscles are distally detached being careful to maintain intact blood supply. Therefore, the muscles are lifted and/or rotated and/or folded to repair the ulcer. The skin flap will derive from the medial or lateral thigh. A Blake drainage is placed and the skin flap is superiorly rotated to close the defect. The subcutaneous layer is sutured with a 4/0 resorbable suture and the skin with a 4/0 non resorbable half buried horizontal mattress suture. The donor site is covered with a split thickness skin graft.
Sacral ulcers
Surgical treatment: the incision is performed along the ulcer margins. Total coccygectomy, partial sacrectomy and, if necessary, ostectomy of vertebral spinal processes are performed. The coccyx is removed by performing a periostal incision and by using a curved 1.5–2 cm osteotome. The sacral ligaments are incised and the sacral tuberosity is excised.
Reconstructive procedures: if the ulcer is treated in early onset, a debridement can be performed and it can be covered a split thickness skin graft. If the lesion is in a more advanced stage a rotation inferiorly based pedicled musculocutaneous flap is used to repair the defect. This flap is wide, thick and well vascularized and it can be harvested later for other procedures. Moreover, the wound does not lie in the gluteal fold so it does not undergo compression. The musculocutaneous flap from the great gluteus has to be planned and designed for the greatest extension possible. While harvesting the flap, great care has to be posed in preserving the vascular pedicle and the most possible perforating vessels, in order to guarantee an adequate blood supply. After rotation, the flap is fixed and the subcutaneous layer is reconstructed with 2/0 resorbable suture, while the skin is sutured with 4/0 non resorbable half buried horizontal mattress suture. The donor site is grafted.
Trochanteric ulcers
Surgical treatment: the trochanteric prominence must be removed. After excision, ostectomy and hemostasis, the area is irrigated, the margins are widened with retractors and deep structures are inspected, especially the fascia lata. It is important to locate eventual fistulas and/or tunnels that will be readily removed. If the fascia lata presents signs of infection or necrosis, all of the necrotic tissue has to be completely excised.
Reconstructive procedures: when the ulcer is superficial a split thickness skin graft can be used after debridement. The bipedicled advancement flap has particular use in trochanteric ulcers. A deep, convex incision, that runs parallel to the margin of the ulcer, is made so to reach the fascia lata. The skin and the subcutaneous between the incision and the ulcer are lifted from the fascia lata with its double pedicle. The flap is advanced so it covers the ulcer without tending excessively the pedicle and two drainages are placed. The lower margin of the flap is closed in two layers while the upper margin is sutured to the fascia lata. The donor site will be closed with a skin graft.
The anteriorly based fasciocutaneous transposition flap extends posteriorly passing the farthest excision margin of the ulcer on the postero-lateral side of the thigh. The fascia lata is lifted with the skin and subcutaneous tissue. After rotation, a drainage is placed and the flap is fixed in two layers: the subcutaneous with 2/0 resorbable suture and the skin with 4/0 non resorbable half buried mattress suture.
The musculocutaneous flap guarantees an adequate protection of the area and an abundant blood supply. It is harvested on the lateral side of the thigh and when it is designed, the point of entry of the circumflex femoral artery within the muscle must be signaled. When the flap is lifted, great attention must be paid on the vascular pedicle that assures adequate blood supply. In order to secure the perforating arteries, the fascia lata and the subcutaneous tissue are sutured together with a 4/0 resorbable suture. The flap is transposed onto its final trochanteric site and the donor site is covered with a split thickness skin graft.
Results
We considered 4 clinical cases (2 ischiatic sores, 1 sacral sore and 1 gluteal-trochanteric sore) which demonstrate the surgical treatment and the reconstructive procedures that we adopted.
Case 1
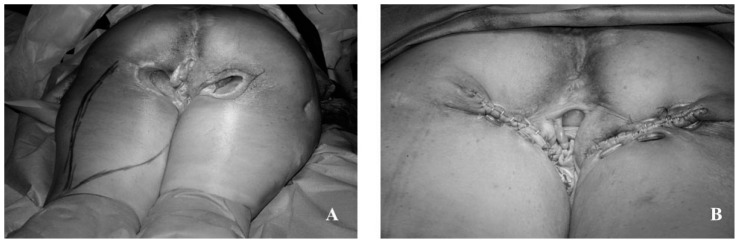
Bilateral ischial pressure ulcer in a female paraplegic patient. NPUAP Stage 4 pressure ulcer. During surgical debridement, extreme care was paid in preserving the lateral walls of the vagina because of the depth of the ulcer. The reconstruction was then performed with a bilateral posterior thigh advancement flap (Figure 1).
Fig. 1.
Bilateral ischial pressure ulcers in a female paraplegic patient. A) pre-operative view. B) post-operative result.
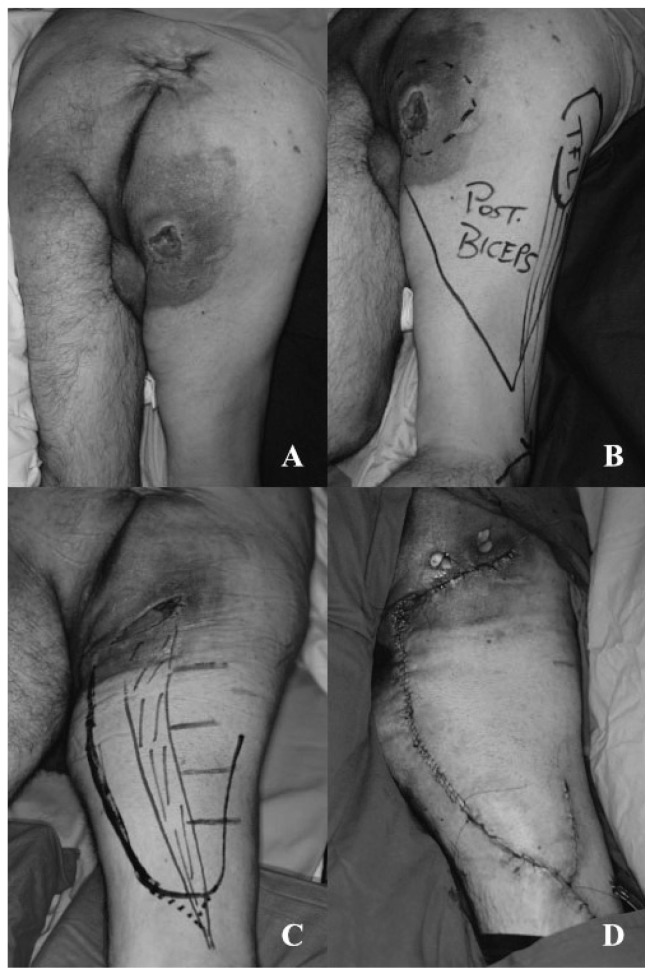
Case 2
Right ischial ulcer in paraplegic patient. NPUAP Stage 3 pressure ulcer. The ulcer presented large subcutaneous extent, without involving the ischiatic bone. The margins of the ulcer were elevated and there was an acute inflammation of the adjacent tissues.
The reconstruction was performed with a posterior thigh skin flap with interposition of biceps femoris muscle (Figure 2).
Fig. 2.
Right ischial ulcer in paraplegic patient. A) pre-operative view. B) design and planning of reconstruction. C) debridement. D) post-operative result.
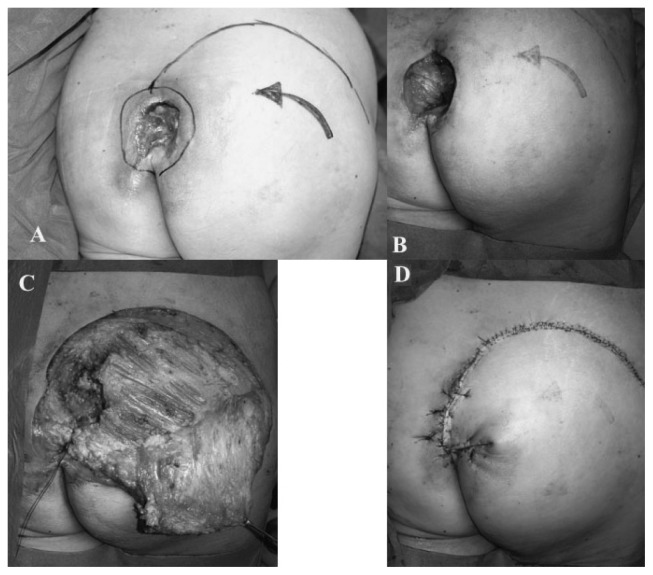
Case 3
Sacral ulcer in tetraplegic patient. NPUAP Stage 4 pressure ulcer. The ulcer presented great extent of local infection, pre-operatively treated with antibiotics. Partial sacrectomy and large debridement were necessary. The reconstruction was performed with a fasciocutaneous flap and interposition of gluteus maximus muscle (Figure 3).
Fig. 3.
Sacral ulcer in tetraplegic patient. A) pre-operative view, design and planning of the reconstruction. B) debridement. C) harvesting of fasciocutaneous gluteal flap and interposition of gluteus maximus muscle.
Case 4
Right gluteal-trochanteric ulcer in paraplegic patient. NPUAP Stage 3 pressure ulcer. The ulcer involved the gluteus maximus ulcer. Large debridement was necessary. The reconstruction was performed with a muscolocutaneous rotation flap of the right tensor fascia lata muscle (Figure 4).
Fig. 4.
Right gluteal-trochanteric ulcer in paraplegic patient. A) pre-operative view. B) harvesting and rotation of myocutaneous tensor fascia lata flap. C) post-operative result. D) one year follow-up.
Discussion
Pressure ulcers are defined as being lesions of the soft tissues due to continuously applied pressure in correspondence of a bony prominence. Wheelchair-bound patients are most frequently affected by pressure sores. Moreover, they also tend to develop pressure ulcers in more than one region at the same time or during their lifetime. The frequency of pressure ulcers according to the anatomic position moving downwards in a head to toe direction are: occiput 1%, chin 0.5%, scapula 0.5%, elbow 3%, spinous process of the vertebrae 1%, iliac spine 4%, sacrum 23%, femoral trochanter 15%, ischium 24%, knee 6%, pretibial spine 2%, malleolus 7%, heel 8% (8).
The continuous pressure leads initially to ischemia and subsequently to the necrosis of the interested area (9). Sacral, ischial and trochanteric regions are subjected to more pressure, having large bony prominence under the soft tissues. The necrosis, the emaceration and the bacterial infection all work together at widening the lesion and the formation of a subcutaneous abscess (9). This process causes a thrombosis of the adjacent deep vascular region, which brings about the spreading of necrosis and further tissue damage. The lesion margins thicken and tend to roll onto themselves deepening and forming a pocket or bursa.
Initial signs of pressure sores are represented by erythema, edema and a fine hemorrhagic purpura. Subsequently the skin sags in the middle and forms a reddened halo all around. Within 3 to 5 days a point of necrosis forms and in time, its color changes from reddish-gray to yellowish-gray to grayish-black typical of necrotic eschar. After color mutation, the edema widens and the skin becomes translucid. Margins can often bleed.
If the ulcer deepens, it can involve underlying bones and articulations, causing osteomyelitis and inflammatory arthritis.
Therapeutic options for pressure ulcers are medical and surgical treatment. The conservative or medical treatment consists of bedside debridement and a wet to dry medication. The wet to dry medication is very useful and it is performed cleansing the sore every 8 hours with 10% betadine solution. The ulcer will be covered with gauze moistened with sodium chloride solution. This gauze will be moistened every 4 hours and changed every 8 hours without ever closing the medication so it will adhere to the necrotic tissue, therefore tearing away the dead tissue away at the removal of the gauze. This type of medication will be repeated for 7 to 10 days until granulation tissue appears at the bottom of the ulcer which will then heal. Pressure ulcers have better healing when treated with local application of platelet growth factor (PDFG) and of fibroblast growth factor (FGF) (10). Recent use of VAC (Vacuum Assisted Closure device), which removes oxygen and thus infections therefore facilitating the healing process of pressure sores, seems promising, but the irregular margins presented by the ulcers makes VAC hard to apply in most cases (11).
The surgical treatment consists of surgical debridement and ostectomy of the bony prominence (if needed), followed by reconstruction of the area involved. Performing a correct surgical procedure does not assure the patient of not going thorough recurrences or complications. Thus several flap surgeries are often needed. For this reason, during surgery procedures it is crucial to preserve the tissues and vessels of the anatomic regions involved, so to eventually perform flaps to treat recurrences. The surgical techniques that we described, allow to adequately cover the sacral, ischial and trochanteric sores by using muscle rotation or folding to fill the defect created after debridement. Performing a myocutaneous flap or a cutaneous flap with muscle interposition reduces long term recurrences and allows the patient to continue to use wheel-chairs in his daily life.
Conclusion
In conclusion, surgical treatment represents the only therapeutic option that could prevent recurrences of pressure ulcers. When the sores are located in sacral, ischial or trochanteric regions, it is important to cover the defects with a thick flap to give more support and protection to the areas which undergo pressure. The best results could be accomplished, as reported in this paper, by performing myocutaneous flaps or cutaneous flaps with muscle interposition, which might guarantee a successful repair and a good long term recurrence free survival.
References
- 1.National Pressure Ulcers Advisory Panel. Updated staging system. 2007. [Google Scholar]
- 2.National Pressure Ulcers Advisory Panel. New 2014 Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. 2014. [Google Scholar]
- 3.Hurbungs A, Ramkalawan H. Sacral pressure sore reconstruction: the pedicled superior gluteal artery perforator flap. Afr J Surg. 2012;50(1):6–8. [PubMed] [Google Scholar]
- 4.Ahmadzadeh R, Bergeron L, Tang M, et al. The superior and inferior gluteal artery perforator flaps. Plast Reconstr Surg. 2007;120:1551–1556. doi: 10.1097/01.prs.0000282098.61498.ee. [DOI] [PubMed] [Google Scholar]
- 5.Kim CM, Yun IS, Lee DW, Lew DY, Rah DK, Lee WJ. Treatment of Ischial Pressure Sores with Both Profunda Femoris Artery Perforator Flaps and Muscle Flaps. Arch Plast Surg. 2014;41(4):387–393. doi: 10.5999/aps.2014.41.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berlowitz DR, Wilking SVB. The short-term outcome of pressure sores. J Am Geriatr Soc. 1990;38:748–752. doi: 10.1111/j.1532-5415.1990.tb01464.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee SS, Huang SH, Chen MC, Chang KP, Lai CS, Lin SD. Management of re-current ischial pressure sore with gracilis muscle flap and V-Y profunda femoris artery perforator-based flap. J Plast Reconstr Aesthet Surg. 2009;62(10):1339–46. doi: 10.1016/j.bjps.2007.12.092. Epub 2008 Jul 2. [DOI] [PubMed] [Google Scholar]
- 8.Agris J, Spira M. Pressure Ulcers: Prevention and treatment. Clinical Symposia. 1979;31(5) [PubMed] [Google Scholar]
- 9.Dinsdale SM. Decubitus ulcers: role of pressure and friction in causation. Arch Phys Med Rehabil. 1974;55:147. [PubMed] [Google Scholar]
- 10.Phillips LG, Robson MC. Pathobiology and treatment of pressure ulcerations. In: Jurkiewicz MJ, editor. Plastic Surgery, Principles and Practice. St. Louis, Mo: Mosby; 1990. [Google Scholar]
- 11.Thorne CH, Bartlett SP, Beasley RW, Aston SJ, Gurtner GC, Spear SL. Grabb and Smith’s Plastic Surgery. 2006. [Google Scholar]