Abstract
Surgical approach of single parathyroid adenoma treatment is turning to a less invasive surgery, allowing us to obtain better aesthetic results, reduction of duration of surgical operation, reduction of post-operative morbidity and hospital stay. Tc99m-sestaMIBI scintigraphy is mainly performed for preoperative localization of parathyroid adenomas. Our technique is instead based on the possibility to inhibit the interference of Tc99m-sestaMIBI uptake of the thyroid gland by means of the administration of Lugol’s solution. Indeed, to confirm the identification and removal of the hyperfunctional parathyroid, it is accepted as adequate an ex vivo radioactivity count of the adenoma 20% or 40% greater than the value of the post-excisional background radioactivity, in association or not with intraoperative measurement of PTH. This method allows us to perform surgery with no timetable restriction, and to clearly distinguish the radioactivity of parathyroid adenoma from that of the surrounding tissues and thyroid gland.
Keywords: Radioguided surgery, Tc99m-sestaMIBI scintigraphy, Single parathyroid adenoma
Introduction
Gamma detection probe is more frequently indicated for two surgical procedures: sentinel lymph nodes (SLN) sampling (for breast cancer and melanomas) and minimally-invasive radioguided surgery (MIRS) of parathyroid adenomas (1). While SLN biopsy is a well-defined procedure and there are no technical problems for the identification of SLN, intraoperative identification of parathyroid adenomas can be difficult to perform due to organization issues and coordination between different departments (2, 3). Technetium (Tc99m)-sestaMIBI is used as radiotracer for intraoperative localization of adenomatous parathyroid glands and the injection is usually performed 2–3 hours before surgery, since it is exploited the characteristic of Tc99m-sestaMIBI to wash out more quickly from thyroid than from the parathyroid glands (4). The lapse of time useful to perform surgery is therefore narrow or strict, and sometimes the organization of operating rooms can be difficult. Furthermore, sometimes in our experience the thyroid uptake of radiotracer made problematic the identification of parathyroid adenoma, despite our observance of technical lapse of time. Trying to elaborate a “less strict” procedure for rapid and sure intraoperative localization of parathyroid adenomas and for minimally-invasive and safe surgery, several protocols have been proposed. Some authors described a protocol consisting in the execution of scintigraphy the same day of surgery (5). In that case patients are intravenously injected with 740 to 925 megabecquerel (MBq) of Tc99m-sestaMIBI for the scintigraphic location of adenoma, and the surgery is performed between 2.5 and 3 hours after injection. Other authors described a separate day protocol whereas pre-operative double-tracer (Tc99m-pertechnetate and Tc99m-sestaMIBI) subtraction scintigrafy is performed several days before the surgery to identify the adenoma (4). On the day of the surgery, some minutes before the beginning of the operation, patients are injected with low dose of Tc99m-sestaMIBI (37 MBq) (6). The undoubted effectiveness of those protocols is limited by the strict window of time for surgery and by the background radiation due to radiotracer uptake of the surrounding tissues, above all thyroid parenchyma.
Looking for a solution to perform an accurate and safe radioguided parathyroidectomy to overcome those problems, we studied and developed an original method, as described below.
Method
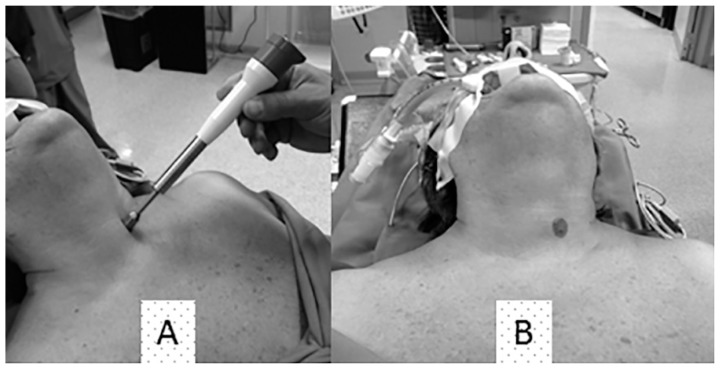
Our protocol is based on the preoperative diagnosis by scintigraphy of the parathyroid gland, with dual tracer method and subsequently on the original preparation of the patient, before administration of a single dose of Tc99m-sestaMIBI, in view of the intraoperative identification of the adenoma. Patient preparation is done by administration of 5 drops every 12 hours of 10% Lugol’s solution, four days before the surgery and on the day of the operation, in order to totally inhibit the thyroid function. Lugol’s iodine is a solution of elemental iodine and potassium iodide in water, that causes a decrease of thyroid gland vascularity, a decrease in thyroidal iodide uptake, a decrease in iodide oxidation and organification, and a block in the release of thyroid hormones (7). On the day of the surgery, patient undergoes scintigraphy of parathyroid glands, 10 minutes after the intravenously administration of 111 MBq of 99mTc-sestaMIBI. After localization of previously diagnosed adenoma, its cutaneous projection area is detected by hand-held -probe and is marked with indelible ink, as a guide for surgical access (Figure 1). We have chosen to inhibit thyroid because the radiotracer absorbed by the thyroid parenchyma sometimes had interfered with uptake of hyperfunctional parathyroid gland during surgery, and that happened even when preoperative adenoma uptake of radiotracer was clearly greater than thyroid uptake; this was most likely due to both the surgical preparation of surrounding structures that can facilitate diffusion of radiotracer in thyroid parenchyma, and to Technetium instability. Therefore, thanks to the preoperative administration of Lugol’s solution, we temporarily inhibited thyroid function and we facilitated the Tc99m-sestaMIBI concentration only in the parathyroid adenoma.
Fig. 1.
Hand-held γ-probe detection of adenoma (A): its cutaneous projection area is marked with indelible ink (B).
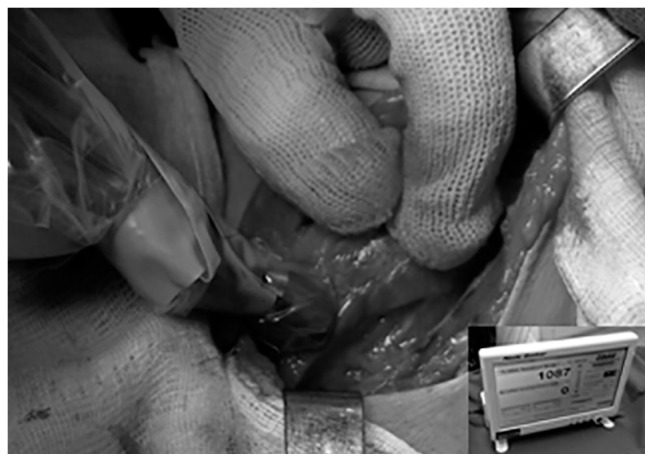
In our experience, even if we did not follow the timetable indicated in the previous protocols (5, 6), radiotracer was totally absorbed in parathyroid adenoma that was easily located by means of traditional hand-held probe, with no interference by the thyroid gland. Previously we made several attempts using timetables from different protocols with the aim of finding unequivocally the adenomatous parathyroid gland but only now we were able to totally eliminate the interference due to thyroid gland uptake. Intact parathyroid hormone (PTH) test performed before the surgery and thirty minutes after the removal of the adenoma confirmed the accuracy of surgery. PTH test was performed just for the purpose of the study given that as well lower left parathyroid adenoma, our patient also had some thyroid nodules with a small papillary thyroid carcinoma (0.6 cm) of the left thyroid lobe (just histologically identified incidentaloma). Therefore, forced to perform total thyroidectomy too, we unequivocally verified the validity of this method even on the surgical specimens. After preoperative inhibition of thyroid function, radioactivity was totally concentrated on hyperfunctional parathyroid adenoma (Figure 2).
Fig. 2.
Intraoperative radioactivity of parathyroid adenoma.
Discussion
For several years, surgical approach of parathyroid adenomas treatment is turning to a less invasive surgery, allowing us to obtain better aesthetic results, reduction of duration of surgical operation, reduction of post-operative morbidity and hospital stay, with a consequent reduction of costs. Fundamental indications for minimally invasive surgery are the presence of a single adenoma and the precise preoperative and intraoperative localization. Most of the patients (80% to 90%) are affected by single parathyroid adenoma, so theoretically candidable to this procedure, but we must consider that there may be some contraindications, such as obesity or the presence of an enlarged thyroid (8). Tc-99m-sestaMIBI scintigraphy is mainly performed for preoperative localization of parathyroid adenomas and it can be performed in combination with ultrasound or CT. Rubello et al. (9) have suggested to perform a dual tracer scintigraphy combined with ultrasound of the neck, which allowed the identification of preoperative parathyroid adenomas, and they assigned to minimally invasive surgery only patients with normal thyroid. Thanks to this procedure, associated with the surgical protocol developed by the authors and previously reported (6), 97% of patients who underwent MIRS have been successfully treated (9).
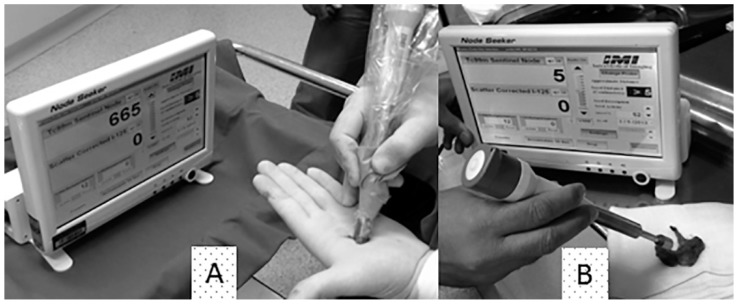
Our technique is instead based on the possibility to inhibit the interference of Tc99m-sestaMIBI uptake of the thyroid gland by means of the administration of 10% Lugol’s solution, which is useful both to the certain identification and intraoperative localization of the adenoma by gamma probe, and to subsequently verify the operation outcome. Indeed, to confirm the identification and removal of the hyperfunctional parathyroid it is accepted as adequate an ex vivo radioactivity count of the adenoma 20% or 40% greater than the value of the post-excisional background radioactivity, in association or not with intraoperative measurement of PTH, depending on the protocols (10, 11). Furthermore, according to some authors, the count of radioactivity is so reliable as to make unnecessary the intraoperative PTH assay or other confirmatory examinations (12, 13). In our experience, the thyroid parenchyma and surrounding tissues did not show a significant radioactivity count, either before surgery or after removal (Figure 3).
Fig. 3.
The radioactivity of the surgical specimen, although reduced as compared to intraoperative detection, remains totally concentrated on the adenoma (A), with no interference of the thyroid parenchyma (B).
Conclusion
In conclusion, this method allows us to perform surgery with no timetable restriction and to clearly distinguish the radioactivity of parathyroid adenoma from that of the surrounding tissues, including the thyroid radioactivity. We think that this protocol will allow us to reduce the time of hospitalization and costs. It will allow us to technically improve the treatment of parathyroid adenomas and organization of operating theatres.
Acknowledgements
We would like to thank the patients who participated in this study. No financial support was received for this study.
Footnotes
Consent
Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflict of interest statement
The authors declare that they have no competing interests.
Author’s contributions
VP, LDV and VD designed and wrote the paper; VP, PU and VD performed the surgery; FM and SI performed lymphoscintigraphic mapping; PU, LDV and VD performed the literature search and supported the writing of the paper. All authors read and approved the final manuscript.
References
- 1.Povoski SP, Neff RL, Mojzisik CM, O’Malley DM, Hinkle GH, Hall NC, et al. A comprehensive overview of radioguided surgery using gamma detection probe technology. World J Surg Oncol. 2009;7:11. doi: 10.1186/1477-7819-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soluri A, Massari R, Trotta C, Stella S, Cavaiola S, Capriotti G, Di Santo GP, Di Paolo ML, Mangano AM, Liberatore M, Micarelli A, Bruzzese A, Pasta V. High resolution mini-gammaca-mera and 99mTc [HMPAO]-leukocytes for diagnosis of infection and radioguided surgery in diabetic foot. G Chir. 2005 Jun-Jul;(6–7):246–50. [PubMed] [Google Scholar]
- 3.Soluri A, Trotta C, Scopinaro F, Tofani A, D’Alessandria C, Pasta V. Radioisotope guided surgery with imaging probe, a hand-held high-resolution gamma camera. Nuclear Instruments and Methods in Physics Research A. 2007;583:366–371. [Google Scholar]
- 4.Mariani G, Gulec SA, Rubello D, Boni G, Puccini M, Pelizzo MR, et al. Preoperative localization and radioguided parathyroid surgery. J Nucl Med. 2003;44(9):1443–58. [PubMed] [Google Scholar]
- 5.Norman J, Chheda H. Minimally invasive parathyroidectomy facilitated by intraoperative nuclear mapping. Surgery. 1997;122(6):998–1003. doi: 10.1016/s0039-6060(97)90201-4. [DOI] [PubMed] [Google Scholar]
- 6.Rubello D, Piotto A, Casara D, Muzzio PC, Shapiro B, Pelizzo MR. Role of gamma probes in performing minimally invasive parathyroidectomy in patients with primary hyperparathyroidism: optimization of preoperative and intraoperative procedures. Eur J Endocrinol. 2003;149(1):7–15. doi: 10.1530/eje.0.1490007. [DOI] [PubMed] [Google Scholar]
- 7.Erbil Y, Ozluk Y, Giriş M, Salmaslioglu A, Issever H, Barbaros U, et al. Effect of Lugol Solution on Thyroid Gland Blood Flow and Microvessel Density in the Patients with Graves’ Disease. J Clin Endocrinol Metab. 2007 Jun;92(6):2182–9. doi: 10.1210/jc.2007-0229. [DOI] [PubMed] [Google Scholar]
- 8.Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol. 2012;33(4):457–68. doi: 10.1016/j.amjoto.2011.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubello D, Casara D, Giannini S, Piotto A, De Carlo E, Muzzio PC, et al. Importance of radio-guided minimally invasive parathyroidectomy using hand-held gamma probe and low (99m)Tc-MIBI dose. Technical considerations and long-term clinical results. Q J Nucl Med. 2003;47(2):129–38. [PubMed] [Google Scholar]
- 10.Murphy C, Norman J. The 20% rule: a simple, instantaneous radioactivity measurement defines cure and allows elimination of frozen sections and hormone assays during parathyroidectomy. Surgery. 1999;126(6):1023–8. doi: 10.1067/msy.2099.101578. [DOI] [PubMed] [Google Scholar]
- 11.Rubello D, Piotto A, Casara D, Muzzio PC, Shapiro B, Pelizzo MR. Role of gamma probes in performing minimally invasive parathyroidectomy in patients with primary hyperparathyroidism: optimization of preoperative and intraoperative procedures. Eur J Endocrinol. 2003;149(1):7–15. doi: 10.1530/eje.0.1490007. [DOI] [PubMed] [Google Scholar]
- 12.Norman J, Politz D. Measuring individual parathyroid gland hormone production in real-time during radioguided parathyroidectomy. Experience in over 8,000 operations. Minerva Endocrinol. 2008;33(3):147–57. [PubMed] [Google Scholar]
- 13.Quillo AR, Bumpous JM, Goldstein RE, Fleming MM, Flynn MB. Minimally invasive parathyroid surgery, the Norman 20% rule: is it valid? Am Surg. 2011;77(4):484–7. [PubMed] [Google Scholar]