Abstract
Objective
The study’s purpose was to test the generalizability of an individualized information prescription model, which has been previously validated for educating patients about hypertension in emergency department and community health center settings. Study investigators assessed the effects of educational materials targeted to health literacy levels and learning styles on patients’ diabetes knowledge in a community clinic setting.
Methods
From May to August 2012, 160 patients were recruited and randomized into intervention (n = 81) and control (n = 79) groups. Inclusion criteria included 18 years or older, English or Spanish speaker, and a type 2 diabetes diagnosis. Measures included modified versions of the Diabetes Knowledge Test and Subjective Numeracy Scale, along with brief health literacy and learning style assessments. Study team members contacted both groups after 2 and 6 weeks to reassess diabetes knowledge.
Results
The control group showed no significant change in diabetes knowledge at both follow-ups. In contrast, the mean number of diabetes knowledge questions answered correctly by the intervention group increased significantly after 2 weeks (Δ = 2.66, P = 0.000), which persisted at 6 weeks (Δ = 2.46, P = 0.00).
Conclusions
This study showed that patients’ knowledge about diabetes increased significantly after exposure to educational materials targeted to their health literacy levels and learning style preferences and that the model is transferrable among health conditions.
Keywords: Health Literacy, Learning, Diabetes, Patient Education, Health Communication, Community Health Centers
INTRODUCTION
More than 9% of the entire US population and 12% of US adults aged 20 and above have diabetes [1]. If current trends persist, 1 in 3 American adults will have diabetes by 2050. The stakes of diabetes care are high: the condition is the 7th highest cause of death in the United States, and people with diabetes are twice as likely to die at any moment than those without the condition [2]. Studies have shown that health literacy—the ability to obtain, understand, and apply medical information—and numeracy—the ability to effectively use numbers in everyday life—are associated with factors affecting diabetes outcomes, such as self-efficacy and glycemic control [3–8].
Diabetes tends to be more prevalent in populations associated with higher levels of inadequate health literacy, such as low-income and minority populations. Diabetes affects 19% of federally qualified community health center patients, the majority of whom live below 200% of the federal poverty level [9]. Minorities have a much higher risk of being diagnosed with diabetes compared to non-Hispanic Whites: the risk is 18% higher for Asian Americans, 66% higher for Hispanics, and 77% higher for non-Hispanic African Americans [1]. It is therefore important to consider health literacy as a factor in the care of highly affected populations, because accounting for health literacy and/or numeracy has been shown to mediate or eliminate the apparent relationship between race and factors such as medication adherence and care preferences in various conditions [10–13].
Due to the national prevalence of diabetes and the demonstrated relationship between health literacy and effective diabetic self-care, the condition was selected to test the reusability of an information prescription model targeted to patients’ health literacy levels and learning styles that was developed by the Eskind Biomedical Library (EBL) Knowledge Management experts at the Vanderbilt University Medical Center (VUMC). The study was the third phase of a research project investigating the impact on health knowledge outcomes of an individualized information prescription model. The model was proved effective in improving patient understanding of hypertension in randomized controlled trials in both emergency department and community health center settings in phase one [14] and phase two [15] of the project. Essential to the generalizability of the model’s approach to other health care settings is an understanding of how best to implement the model for various health conditions.
In phase three of this research project, the EBL Knowledge Management team returned to the same community health center to conduct another randomized controlled trial with English- and Spanish-speaking patients with type 2 diabetes. The goal of the study was to determine if diabetes educational materials tailored to their health literacy levels and learning styles would positively impact participants’ knowledge of their condition.
METHODS
This study was approved by the Institutional Review Board at VUMC.
Setting
The study took place at the Vine Hill Community Clinic (VHCC), which is operated by University Community Health Services (UCHS) and affiliated with the Vanderbilt University School of Nursing. A federally qualified community health center, VHCC serves Nashville’s medically underserved and underinsured population by offering low- or no-cost primary, mental, dental, and prenatal care [16]. In 2012, 90% of UCHS network patients were at or below the 200% poverty level and 34% were uninsured. An additional 36% received benefits through Medicaid. Approximately 9% of UCHS patients had a diabetes diagnosis, and only 57.1% of patients had a glycated hemoglobin (HbA1c) level equal to or below 9%, the treatment goal [17].
Participants
Recruited participants were 18 years or older, spoke English or Spanish, and had a health care provider–confirmed diagnosis of type 2 diabetes. Exclusion criteria were illiteracy, cognitive impairment, and psychiatric reasons for the clinic visit. Baseline data collection included age, gender, race, ethnicity, education level, employment status, household income, and smoking status. Data were also collected on participants’ family history of diabetes and use of diabetes medications. VHCC patients were enrolled in the study from May to August 2012, and all patient follow-up was completed by October 2012. Participants were randomized in a 1:1 ratio to control or intervention groups using a permuted block design with random block sizes.
Measures
Diabetes knowledge
A modified version of the Michigan Research and Training Center’s Diabetes Knowledge Test (DKT) [18] was used to assess patient knowledge of the condition. The study team selected the DKT after performing a comprehensive literature review. An often-used diabetes knowledge assessment, the DKT includes 23 questions that are designed to assess general knowledge of diabetes. Results from the study team’s literature review revealed the DKT has been used in more than 100 studies since its development in 1991.
The team made a few modifications to the DKT to better fit the purposes of the research project. The test includes 9 questions that are specifically focused on insulin use. These questions were not used in the version of the test administered to clinic patients, as the research team wished to focus on patients’ broader understanding of diabetes. Question 5 of the DKT was modified to more closely reflect current practice guidelines, based on feedback from 2 collaborating physicians. The question pertains to the period of time measured by the hemoglobin A1 test, and the correct answer was modified from “6–10 weeks” to “8–12 weeks.” Also 2 questions in the test (questions 8 and 14) are negatively phrased. Though negatively worded statements are a common instrument-development technique, the study team observed patients in the first 2 phases of the research project having difficulty answering those types of questions. Questions 8 and 14 of the original DKT were therefore placed as the last 2 items of the assessment to allow the professionals administering the test the opportunity to notify the patients that these questions were negatively phrased.
Health literacy
To assess participants’ health literacy levels, the three-question subjective assessment developed by Lisa Chew and colleagues at the University of Washington [19] was administered to study participants. The assessment asks patients to indicate, using a four-point Likert scale, how confident they are filling out forms, how often they need help reading hospital materials, and how often they have trouble learning about medical conditions due to reading difficulties. The test is graded on a twelve-point scale, with lower scores indicating more adequate levels of health literacy. Participants scoring zero to four were classified as having adequate health literacy, while those with scores of five to six were classified as marginal and seven to twelve as inadequate. Chew’s research has shown that the three-question assessment has a strong correlation with the commonly used Short Test of Functional Health Literacy in Adults [20], and the study team’s use of both assessments in phase one supported that finding [14]. Using this abbreviated measure helped to reduce patient burden by lowering the time spent on assessing health literacy from seven minutes to less than two minutes.
Learning style preferences
As the goal of the research was to maximize patient compliance through exposure to educational information prescription content, study participants were asked to self-assess their preferences for learning about health information. Data collected in phase one and phase two of the research project [14, 15] demonstrated close alignment of patient subjective responses with results from a formal learning style questionnaire [15]. Additionally, research by other investigators has shown that individual learning preferences evolve over time and that learning via multiple styles may be the most effective method [21–24]. Ultimately, study team members informed patients that the intervention materials were available in multiple formats and allowed participants to choose their preferred formats, as data collected in earlier project phases clearly indicated that learning could be improved by going beyond the traditional written explanation [15]. Patients’ individual preferences for learning format were then used in combination with health literacy level to guide the provision of interventional materials.
Numeracy levels
The final measure used was a modified version of the Subjective Numeracy Scale (SNS). The SNS asks patients to subjectively rate themselves using a six-point Likert scale on how skilled they are in basic math and how useful they find numeric values for understanding information [25]. A condensed, three-item version of the SNS has shown predictive value for the longer, eight-item assessment [26]. To reduce patient burden, the modified, shortened version was used in this study to collect baseline data on patient numeracy. Although intervention materials were not tailored to numeracy levels, the collected data allowed the team to evaluate the potential impact of numeracy on knowledge outcomes and collect such information in a setting where subjective numeracy assessment had not been previously used.
All assessments were translated into Spanish by professional translators in the VUMC Office of Translation Services.
Intervention
Educational materials for the intervention group were developed to reflect the content evaluated in the DKT. From February to April 2012, the team worked to create a tiered set of materials targeted to fifth- and eighth-grade reading levels in each of the four learning styles. Resources consulted during the content development process included the National Institute of Diabetes and Digestive and Kidney Diseases, the American Diabetes Association, the National Diabetes Information Clearinghouse, the Centers for Disease Control and Prevention, and MedlinePlus.
Intervention group members were given the core fifth-grade-level materials for all of their selected learning styles. Participants with adequate health literacy levels also received supplemental information written at the eighth-grade level, which included more in-depth information on diabetes. Patients with marginal health literacy levels were given the option of receiving the more advanced information as well. Patients with inadequate health literacy levels were only offered the core materials that all intervention group members received.
The materials for visual learners made heavy use of images and graphics, while the version for read/write learners was mostly text based. Auditory learners listened to an audio recording of the information. Kinesthetic learners were given a card-sorting activity developed by the study team that asked them to sort cards with facts about diabetes into relevant categories. Spanish-speaking individuals received the versions of the documents that had been translated into Spanish by the VUMC Office of Translation Services. The intervention group patients also took home copies of the information for future reference. Although patients in the control group did not receive the information prescription materials at the time of the clinic visit, they did receive copies once the study was completed so they could still benefit from the information.
Follow-up assessment
At 2 weeks and 6 weeks after the initial assessment, intervention and control group participants were contacted by phone and reassessed with the same modified DKT. With the final assessment, intervention group members were also asked to indicate on a 5-point Likert scale how satisfied they were with the materials and whether they had consulted other resources. Participants who completed the entire study were given a $15 gift card to a local grocery store.
Statistical analysis
The study’s primary outcome, the comparison of the mean difference in diabetes test scores in the control and intervention groups, was evaluated using independent t tests. Differences in test scores were analyzed at 2 weeks and again at 6 weeks. The study sample size was calculated (n = 160) to provide at least 95% power to detect a difference of 2 correctly answered questions on the DKT score before and after intervention at a 2-sided 5% significance level and a standard deviation on the DKT of 2.5 questions. Mixed effects multivariate linear regression analyses were conducted to evaluate the influence of gender, race, level of education, household income, health literacy, study team interviewer, time of posttest administration, and diabetes history on knowledge test scores. The multiple imputation method was used to estimate missing values.
All study data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at VUMC. REDCap is a secure, web-based application designed to support data capture for research studies, providing (1) an intuitive interface for validated data entry, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for importing data from external sources [27].
RESULTS
Study participants
One hundred and sixty patients were enrolled at the beginning of the study. Seventy-nine patients were allocated to the control group and 81 to the intervention group. The team was unable to contact 7 patients from the control group and 6 patients from the intervention group to perform the 2-week follow-up assessment. At the 6-week follow-up, the team was unable to contact an additional 5 patients from the control group and 14 patients from the intervention group. A total of 32 patients did not complete the full study, bringing the total number of participants at completion to 128 (Figure 1).
Figure 1.
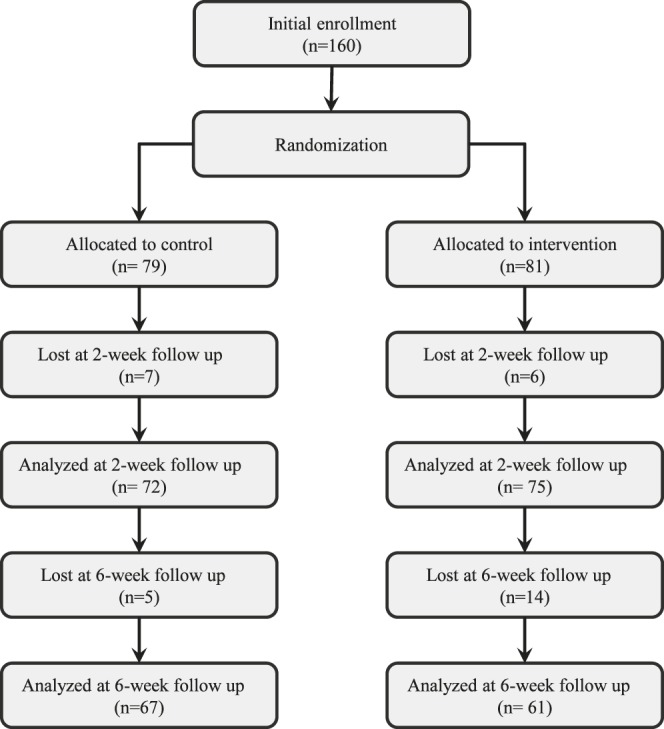
Participant flow chart
Overall, participants were similarly distributed across the control and intervention groups for most characteristics, including age, language, gender, race, ethnicity, household income, family and personal histories of diabetes, and smoking status (Table 1). More participants in the intervention group graduated from high school than in the control group (48% vs. 29%), and more participants in the intervention group reported looking up information on their own at 2-week follow-up (Table 2). Slightly more participants in the intervention group had adequate health literacy levels compared to the control group (79% vs. 66%).
Table 1.
Characteristics of patients recruited from the Vine Hill Community Clinic (VHCC)
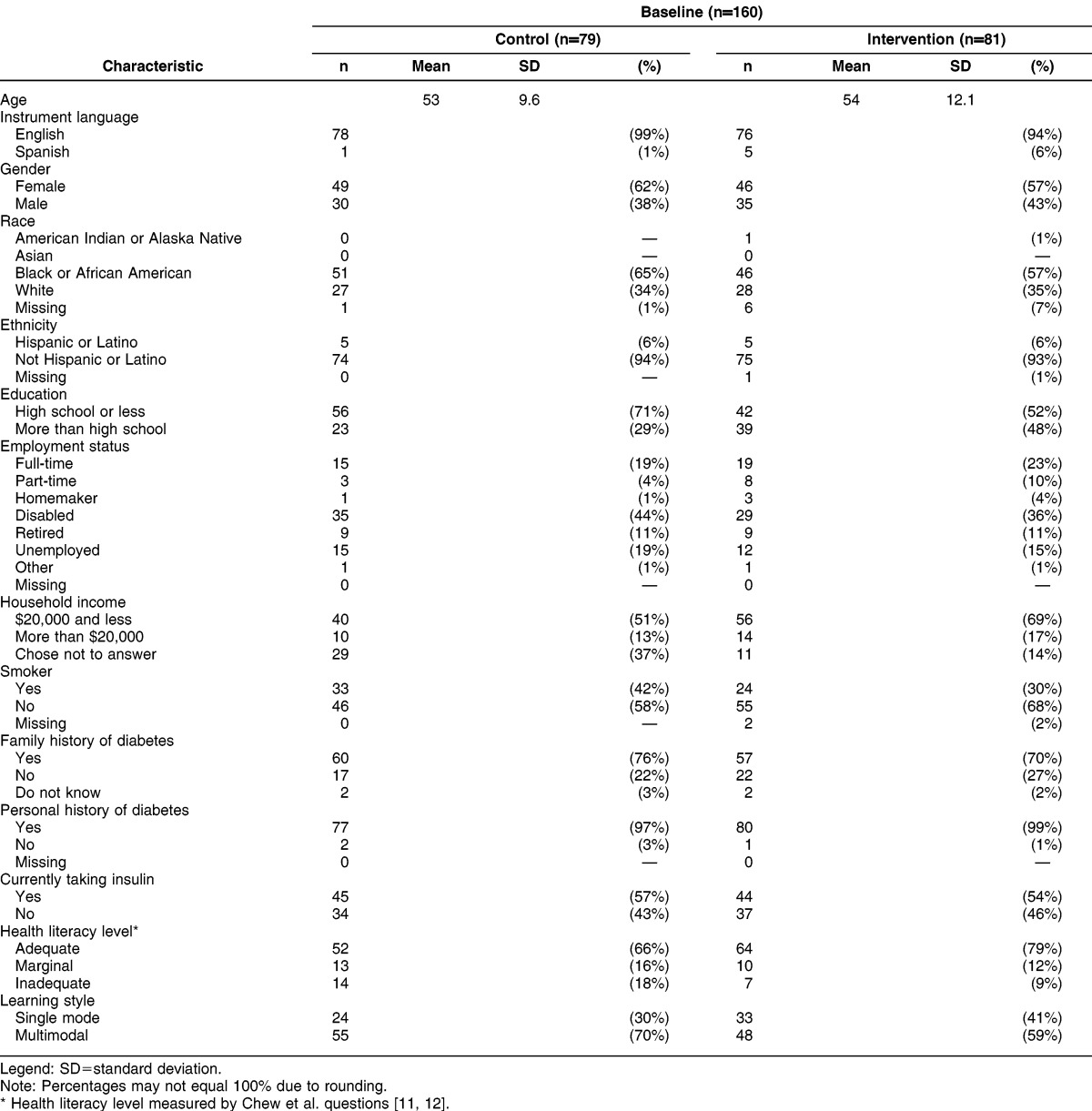
Table 2.
Additional characteristics of VHCC patients
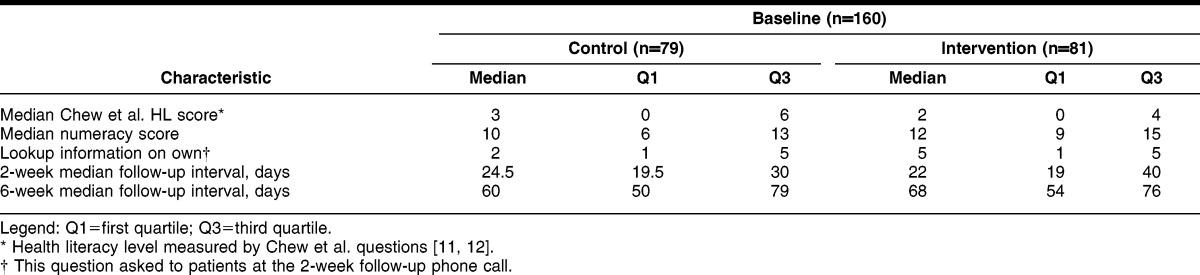
The majority of participants (n = 154, 96%) spoke English, and most (n = 95, 59%) were female. African Americans constituted 61% (n = 97) of the study population. Many participants (n = 98, 61%) had a high school education or less. A similar proportion (n = 96, 60%) had a household income of $20,000 a year or less. While the majority of participants’ health literacy levels were adequate (n = 116, 73%), there was still a significant percentage who did not meet that threshold: 14% (n = 23) of participants had marginal health literacy levels, and 13% (n = 21) of patients’ health literacy levels were inadequate. Two weeks after the baseline clinic visit, participants were asked if they had looked up information on their own. Participants in the intervention group scored higher on a Likert scale of 1–5 (5 indicating the highest score) than those in the control group (median of 5 vs. 2, respectively).
Diabetes Knowledge Test results
An analysis of the DKT results of the 128 individuals who completed the study showed that participants in the intervention group performed better on all questions at the 2-week follow-up compared to the control group (Figure 2). The difference in the number of questions correctly answered by the intervention groups at 2 weeks and 6 weeks were statistically significant (P = 0.00 for both analyses) compared to the control group.
Figure 2.
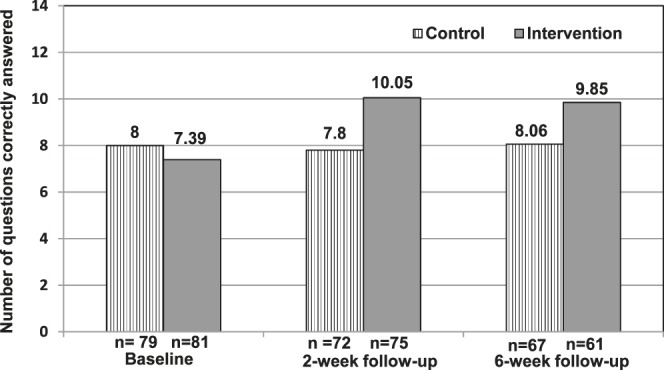
Absolute change in the number of correct responses on the diabetes quiz
Results from the mixed-effect model multivariate linear regression revealed that assignment to the intervention group, pretest score, non-White race, income less than $20,000 annually, and follow-up time period were significant predictors of posttest score after adjusting for gender, race, health literacy level, education, and income.
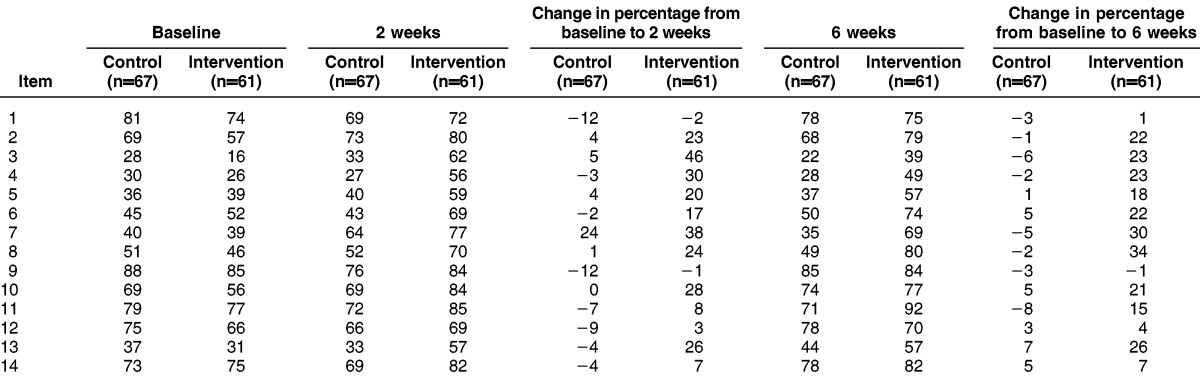
To understand how participants performed on individual quiz items, the study team compiled response data for each question (Table 3). Two weeks after the clinic visit, there were 8 questions that more than 70% of participants in the intervention group answered correctly, in contrast to 3 questions that more than 70% of control group participants answered correctly. At 2-week follow-up, the greatest improvement in the number of correct responses to questions on the diabetes test was observed by intervention group participants for questions 3, 7, and 4 (46%, 38%, and 30%, respectively). These questions asked participants to identify high-fat food items, indicate the effect of unsweetened fruit juice on blood glucose, and define “free food.” At 6-week follow-up, the question with the highest improvement compared to baseline was question 8 (34%), followed by questions 7 and 13. These questions asked participants to demonstrate understanding of numbness or tingling as symptoms of nerve disease, indicate the effect of unsweetened fruit juice on blood glucose levels, and determine which foods should not be used to treat low blood glucose.
Table 3.
Percentage of patients responding correctly to individual Diabetes Knowledge Test items
DISCUSSION
This study supports and validates the usefulness of individualized information prescription materials for multiple health care conditions. The intervention group members’ diabetes knowledge increased significantly on average after exposure to educational materials targeted to their health literacy levels and learning style preferences. The control group, who did not receive individualized materials until after completion of the study, experienced no significant change in test scores during the 6-week trial. These outcomes build on results observed from the team’s earlier studies that demonstrated how this personalized approach to information delivery can improve knowledge outcomes across health care settings [14, 15].
The results presented here confirm the ability of this approach to improve patient knowledge across multiple health care conditions. For a chronic disease like diabetes that has a large public health impact and can be ameliorated through lifestyle modifications, any improvement in patient knowledge could have a significant impact on patient quality of life and could help control the projected exponential growth in prevalence. Interventions attempting to bridge gaps in patient knowledge are particularly important in the community health center setting, where this study has shown that patients tend to have lower health literacy levels and where national data indicate patients have a 50% higher chance of being diagnosed with diabetes than their counterparts [9].
One potential limitation of the study is that the majority of recruited patients tested as having adequate health literacy levels. While the approach was also validated in an emergency department setting in Nashville, it is possible that different results would arise if a similar study were conducted in a different city or clinical setting. Additionally, the study follow-up period of six weeks did not allow for more long-term evaluation of intervention outcomes.
This study demonstrates that health sciences librarians and information scientists can play an important role in providing personalized medicine and thereby influence health outcomes by applying their expert knowledge of health literacy, information provision, and the medical field to the clinical setting. In each of three study phases, patients’ knowledge of their health conditions was significantly improved through exposure to an information prescription targeted to their individual health literacy levels and learning style preferences. Phase three, described here, demonstrates the model’s potential to be scaled to positively impact patient knowledge outcomes for a variety of health conditions.
EBL’s key function is to facilitate the medical center’s transformative vision of personalized medicine through projects that harness the unique expertise of our staff [28]. The study team has implemented the institution’s transformative vision of personalized medicine by taking a highly personalized approach to how health information needs to be delivered to patients. By making visible the value that librarians add through initiatives such as individualized patient education, the health sciences library has the opportunity to solidify its important role in the medical center outside the physical space of the library building and beyond the standard provision of resources.
ACKNOWLEDGMENTS
The authors thank Marcia Epelbaum and Sandra Martin for their contributions to recruiting and interviewing patients in the VHCC and Mallory Blasingame and Annette Williams for editing and bibliographic management assistance during manuscript preparation.
Biography
Taneya Y. Koonce, MSLS, MPH, taneya.koonce@vanderbilt.edu, Deputy Director, Eskind Biomedical Library, Vanderbilt University Medical Center, 2209 Garland Avenue, Nashville, TN 37232; Nunzia B. Giuse, MD, MLS, FMLA, nunzia.giuse@vanderbilt.edu, Assistant Vice Chancellor for Knowledge Management; Director, Eskind Biomedical Library; Professor, Department of Biomedical Informatics; and Professor, Department of Medicine; Vanderbilt University Medical Center, 2209 Garland Avenue, Nashville, TN 37232; Sheila V. Kusnoor, PhD, sheila.v.kusnoor@vanderbilt.edu, Associate Director for Research, Eskind Biomedical Library, Vanderbilt University Medical Center, 2209 Garland Avenue, Nashville, TN 37232; Suzanne Hurley, RN, MSN. APRN-BC, suzanne.hurley@uchshealth.org, Clinical Director for Community Health Services, University Community Health Services, 2410 Franklin Pike, Nashville, TN 37204; Fei Ye, PhD, MSPH, fei.ye@vanderbilt.edu, Assistant Professor of Biostatistics, Division of Cancer Biostatistics, Department of Biostatistics, Vanderbilt University School of Medicine, Vanderbilt Center for Quantitative Sciences, 495 Preston Research Building, Nashville, TN 37232
Footnotes
This research was supported by Institute of Museum and Library Services (IMLS) grant no. IMLS LG-06-10-0186-10.
Based on a presentation at MLA ’14, the 114th Annual Meeting of the Medical Library Association; Chicago, IL; May 18, 2014.
This article has been approved for the Medical Library Association's Independent Reading Program <http://www.mlanet.org/education/irp/>.
REFERENCES
- 1.Centers for Disease Control and Prevention National diabetes statistics report . estimates of diabetes and its burden on the United States [Internet] Atlanta, GA: The Centers, US Department of Health and Human Services; 2014. 2014 [cited 11 Nov 2014]< http://www.cdc.gov./diabetes/data/statistics/2014StatisticsReport.html>. [Google Scholar]
- 2.Centers for Disease Control and Prevention Diabetes: successes and opportunities for population-based prevention and control at a glance. Atlanta: GA: The Centers,US Department of Health and Human Services; 2011. 2011 [Internet] [cited 7 Nov 2014], < http://www.cdc.gov/chronicdisease/resources/publications/aag/ddt.htm>. [Google Scholar]
- 3.Piatt GA, Valerio MA, Nwankwo R, Lucas SM, Funnell MM. Health literacy among insulin-taking African Americans: a need for tailored intervention in clinical practice. Diabetes Educ. 2014 Apr;40(2):240–6. doi: 10.1177/0145721713519292. DOI: http://dx.doi.org/10.1177/0145721713519292. [DOI] [PubMed] [Google Scholar]
- 4.Souza JG, Apolinario D, Magaldi RM, Busse AL, Campora F, Jacob-Filho W. Functional health literacy and glycaemic control in older adults with type 2 diabetes: a cross-sectional study. BMJ Open. 2014;42:e004180. doi: 10.1136/bmjopen-2013-004180. DOI: http://dx.doi.org/10.1136/bmjopen-2013-004180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15(suppl 2):146–58. doi: 10.1080/10810730.2010.499980. DOI: http://dx.doi.org/10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL. Association of numeracy and diabetes control. Ann Intern Med. 2008 May 20;148(10):737–46. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 7.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007 Feb;33(1):144–51. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 8.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002 Jul;24(4):288. 475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 9.Shin P, Alvarez C, Sharac J, Rosenbaum S, Van Vleet A, Paradise J, Garfield R. A profile of community health center patients: implications for policy [Internet] Menlo Park, CA: Kaiser Commission on Medicaid and the Uninsured; 23 Dec 2013 [cited 7 Nov 2014]. < http://kff.org/medicaid/issue-brief/a-profile-of-community-health-center-patients-implications-for-policy/>. [Google Scholar]
- 10.Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, White RO. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(suppl 3):268–78. doi: 10.1080/10810730.2011.604388. DOI: http://dx.doi.org/10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waldrop-Valverde D, Osborn CY, Rodriguez A, Rothman RL, Kumar M, Jones DL. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010 Aug;14(4):799–806. doi: 10.1007/s10461-009-9604-4. DOI: http://dx.doi.org/10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009 Sep;32(9):1614–9. doi: 10.2337/dc09-0425. DOI: http://dx.doi.org/10.2337/dc09-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volandes AE, Paasche-Orlow M, Gillick MR, Cook EF, Shaykevich S, Abbo ED, Lehmann L. Health literacy not race predicts end-of-life care preferences. J Palliat Med. 2008 Jun;11(5) doi: 10.1089/jpm.2007.0224. DOI: http://dx.doi.org/10.1089/jpm.2007.0224. [DOI] [PubMed] [Google Scholar]
- 14.Giuse NB, Koonce TY, Storrow AB, Kusnoor SV, Ye F. Using health literacy and learning style preferences to optimize the delivery of health information. J Health Commun. 2012 Oct;17(suppl 3):122–40. doi: 10.1080/10810730.2012.712610. DOI: http://dx.doi.org/10.1080/10810730.2012.712610. [DOI] [PubMed] [Google Scholar]
- 15.Koonce TY, Giuse NB, Choemprayong S, Hurley S, Martin SL, Epelbaum M, Kusnoor SV. Using personalized education delivery to improve community clinic patients’ knowledge of hypertension [Internet] San Diego, CA: Presented at: Special Libraries Association Annual Meeting. 9–11 Jun 2013 [cited 7 Nov 2014]. < http://dbiosla.org/events/past_sla_conference/San%20Diego/contr_papers2013.html>. [Google Scholar]
- 16.Rivers K. New era dawns at Vine Hill Clinic. VUMC Reporter [Internet] 2007. [cited 7 Nov 2014]. < http://www.mc.vanderbilt.edu/reporter/index.html?ID=5591>. [Google Scholar]
- 17.Health Resources and Services Administration. 2012 health center profile: University Community Health Services, Inc. [Internet] Washington, DC: US Department of Health and Human Services; 2012. [cited 7 Nov 2014]. < http://bphc.hrsa.gov/uds/datacenter.aspx?q=d&bid=0450710&state=TN#fn4>. [Google Scholar]
- 18.Fitzgerald JT, Funnell MM, Hess GE, Barr PA, Anderson RM, Hiss RG, Davis WK. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21(5):706–10. doi: 10.2337/diacare.21.5.706. May 1. [DOI] [PubMed] [Google Scholar]
- 19.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, VanRyn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–6. doi: 10.1007/s11606-008-0520-5. May 1. DOI: http://dx.doi.org/10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004 Sep;36(8):588–94. [PubMed] [Google Scholar]
- 21.Fleming ND, Mills C. Not another inventory, rather a catalyst for reflection. Improve Acad. 1992;11:137–49. [Google Scholar]
- 22.Truluck JE, Courtenay BC. Learning style preferences among older adults. Educ Gerontol. 1999;25(3):221–36. DOI: http://dx.doi.org/10.1080/036012799267846. [Google Scholar]
- 23.Mainemelis C, Boyatzis RE, Kolb DA. Learning styles and adaptive flexibility: testing experiential learning theory. Manag Learn. 2002;33(1):5–33. [Google Scholar]
- 24.Pashler H, McDaniel M, Rohrer D, Bjork R. Learning styles: concepts and evidence. Psychol Sci Public Interest. 2009;9(3):105–19. doi: 10.1111/j.1539-6053.2009.01038.x. DOI: http://dx.doi.org/10.1111/j.1539-6053.2009.01038.x. [DOI] [PubMed] [Google Scholar]
- 25.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Mak Int J Soc Med Decis Mak. 2007 Oct;27(5):672–80. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- 26.McNaughton C, Wallston KA, Rothman RL, Marcovitz DE, Storrow AB. Short, subjective measures of numeracy and general health literacy in an adult emergency department. Acad Emerg Med. 2011;18(11):1148–55. doi: 10.1111/j.1553-2712.2011.01210.x. Nov 1. DOI: http://dx.doi.org/10.1111/j.1553-2712.2011.01210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. DOI: http://dx.doi.org/10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guise NB, Kusnoor SV, Koonce TY, Ryland CR, Walden RR, Naylor HM, Walden RR, Williams AM, Jearome RN. Strategically aligning a mandala of competencies to advance a transformative vision. J Med Lib Assoc. 2013 Oct;101(4):261–7. doi: 10.3163/1536-5050.101.4.007. DOI: http://dx.doi.org/10.3163/1536-5050.101.4.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


