Abstract
Background
Drivers of heavy and tractor-trailer trucks accounted for 56% of all production and nonsupervisory employees in the truck transportation industry in 2011. There are limited data for illness and injury in long-haul truck drivers, which prompted a targeted national survey.
Methods
Interviewers collected data during 2010 from 1,670 long-haul truck drivers at 32 truck stops across the 48 contiguous United States that were used to compute prevalence estimates for self-reported health conditions and risk factors.
Results
Obesity (69% vs. 31%, P <0.01) and current smoking (51% vs. 19%, P <0.01) were twice as prevalent in long-haul truck drivers as in the 2010 U.S. adult working population. Sixty-one percent reported having two or more of the risk factors: hypertension, obesity, smoking, high cholesterol, no physical activity, 6 or fewer hours of sleep per 24-hr period.
Conclusion
Survey findings suggest a need for targeted interventions and continued surveillance for long-haul truck drivers.
Keywords: survey, truck driver, health, intervention, risk factor, surveillance, work practices
INTRODUCTION
The U.S. Transportation and Warehousing sector (North American Industrial Classification System [NAICS] codes 48–49) employed 4.4 million workers in 2011 [BLS, 2013]. Of the 11 industries making up this sector, truck transportation providing over-the-road transportation of cargo (NAICS 484) was the largest with 31% of total workers. Truck drivers move goods for a customer (for-hire carriage) or for their employer (private carriage) locally within a metropolitan area, or longer distances within or between geographical regions and may be employed in any NAICS sector requiring freight transport. They drive different types of trucks depending on the size and type of shipment. Drivers of heavy and tractor-trailer trucks made up the largest percentage (56%) of production and nonsupervisory workers in NAICS 484, and accounted for 1.6 million workers (19%) of all transportation and material moving occupations in 2011. Truck drivers’ health requirements for fitness for duty and work schedules are regulated by the Federal Motor Carrier Safety Administration (FMCSA) of the U.S. Department of Transportation (DOT).
The need for better health and injury baseline data for truck drivers has been well documented [TRB, 2006, 2007; Saltzman and Belzer, 2007; Krueger, 2012]. Truck drivers have been reported to be at increased risk for a number of chronic diseases and health conditions such as heart disease, diabetes mellitus, hypertension, and obesity [Roberts and York, 1997; Laden et al., 2007; TRB, 2007; Apostolopoulos et al., 2010]. Drivers of heavy and tractor-trailer trucks experience high rates of injury. In 2009, the incidence rate for nonfatal injury involving days away from work among these truck drivers was 327.6 injuries per 10,000 full-time workers, three times that of the general worker population [BLS, 2010a]. However, the causes and extent of high rates of injury and illness in truck drivers are not well known.
Truck drivers are a mobile and difficult to study population because of their long hours and unpredictable schedules. A number of methods have been used to evaluate the health and injury of truck drivers. Some studies have been conducted using administrative records such as death certificates and union records [Leigh and Miller, 1998; Koda et al., 2000; Robinson and Burnett, 2005; Jain et al., 2006; Laden et al., 2007; Garshick et al., 2008; Dahl et al., 2009; Martin et al., 2009; Birdsey et al., 2010; Helmkamp et al., 2013]. Health studies of commercial truck drivers have been conducted at trade shows or other gatherings [Korelitz et al., 1993; Wood et al., 2012]. Intercept studies have been conducted when drivers stopped at truck stops, rest stops, or weigh stations [Williamson et al., 1992, 2001; FHWA, 1999; McCartt et al., 2000; Solomon et al., 2004; Belman et al., 2005; Williamson, 2006; Bigelow et al., 2012; Angeles et al., 2013]. Studies using data from administrative records or through intercept methods, however, are often generated from a convenience sample and may not be nationally representative. They may also include regional or local drivers in addition to long-haul truck drivers. For example, participants in the Fatigue Management Survey [FMCSA, 2006] were unionized drivers and were not long-haul drivers.
Due to limitations in the studies described above and the need for a population based study of long-haul truck drivers, the National Institute for Occupational Safety and Health (NIOSH) initiated the National Survey of Long-Haul Truck Driver Health and Injury (LHTDS). Long-haul truck drivers (LHTD) are those drivers of heavy and tractor-trailer trucks whose freight delivery routes require sleep periods away from home. The LHTDS was developed with the goal of producing a nationally representative sample from which estimates of the prevalence of health conditions, injuries, and risk factors associated with long-haul truck driving could be determined. Findings from the LHTDS provide baseline health and injury data that can be used: (1) to suggest areas where intervention is needed, (2) to identify benchmarks against which injury or illness reductions can be evaluated after interventions are implemented, and (3) to guide the development of LHTD health and safety policy.
This paper presents an overview of the LHTDS and describes important findings related to truck driver demographics, working conditions, health risks, and lifestyle-related chronic diseases. Subsequent reports will produce additional analyses of health behavior, fatigue, crashes, and injuries among LHTD.
MATERIALS AND METHODS
Sampling Strategy and Design
The LHTDS weighted the sampling process in three stages to approximate a nationally representative probability sample of LHTDs. First, sections of interstate or other limited-access highways were selected, followed by selection of individual truck stops along the selected highway sections, and finally selection of drivers for interview at the selected truck stops.
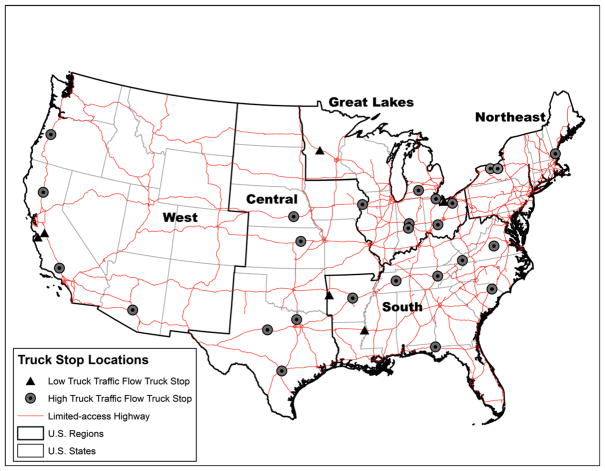
In stage one, limited-access highway segments were stratified by geographic region and truck traffic volume. States comprising each of the five geographic regions are shown in Figure 1. State-highway segments in each region were stratified by truck traffic volume using results from the 2002 Freight Analysis Framework modeling system [FHWA, 2007]. This ensured that drivers traveling along both high- and low-flow traffic routes were included in the survey. High-flow routes were those with a traffic flow over 12,500 trucks per day; all other routes were considered low-flow. The number of high-flow state-highway segments in each region was selected to be proportional to the mileage length of limited-access highway within that region. Low-flow state-highway segments were selected with probability proportional to that state’s population.
FIGURE 1.
Locations of 32 truck stops where long-haul truck drivers were surveyed, Survey of U.S. Long-Haul Truck Drivers, Fall 2010.
In stage two, individual truck stops were selected along state-highway segments. Truck stops with a restaurant and paved overnight parking lot with at least five parking spaces were identified using a national listing of truck stops [Brice, 2008]. Thirty-two truck stops were selected with probability proportional to the number of parking spaces at the truck stop. Truck stop locations where LHTD were surveyed are shown in Figure 1.
In stage three, truck drivers entering truck stops during a 3-day interview period were recruited by the interview team. Drivers were recruited during different 8-hr shifts between 7 AM and 10 PM. One team member approached truck drivers as they entered the truck stop and attempted to recruit them, while the other two interviewers administered interviews. The number recruited at each truck stop varied and depended on the amount of foot traffic at the truck stop and the availability of interviewers. Recruiters were instructed to approach all individuals entering when interviewers were available, so each truck driver who entered during a recruitment period had an equal chance of selection. Interviewers collected data from 1,670 currently employed LHTD during the period October–December 2010.
The number of truck drivers to be interviewed was determined based on the number needed in a simple random sample to obtain 95% confidence intervals of ±2.5% about an estimated percentage of 50% of the drivers responding to a survey question. The time to administer the survey, cost, and expected numbers of drivers at each truck stop were also considered. An intra-truck stop correlation between responses rho = 0.01 was assumed [calculation based on Belman et al., 2005].
Survey Questionnaire
The LHTDS questionnaire was designed to focus on factors which may account for a significant burden of occupational ill health and injury among LHTD. Topics included: the work environment, work history and driving practices [Belman et al., 2005], health conditions and risk factors [NCHS, 2006; CDC, 2007a], health insurance coverage [NCHS, 2006], sleep [NCHS, 2006] and demographics. Height and weight were measured. Anthropometric measurements followed standard protocols [CDC, 2007b].
Survey Administration
After recruiting drivers and obtaining informed consent to participate in the survey, a screening interview was administered to determine eligibility. Truck drivers were eligible for the survey if they: (1) had driven a truck with three or more axles as their main job for 12 months or more, and (2) took at least one mandatory 10-hr rest period away from home during each delivery run. Eligible drivers were administered the personal interview and anthropometric measurements were taken. If drivers were not willing to participate in the full-length interview due to time or other constraints, interviewers administered a short non-respondent interview collecting eligibility and basic demographic information (gender, age, perceived health status, type of driver, smoking status, self-reported height, and weight). Drivers completing the personal interview were slightly younger than those completing only the non-respondent interview (47 years vs. 50 years), and perceived themselves in worse health (81% indicated good or better health vs. 85% from non-respondent interviews). A $25 gift card for use at the truck stop chain was offered for participating in the personal interview and associated components. A $2 gift card was offered for answering the non-respondent interview.
Probability Weighting for National Estimates
Each completed personal interview had an associated probability weight, which represented the inverse of the product of probabilities of selection of the highway segment in stage 1, the truck stop in stage 2, and the truck driver in stage 3:
The probability of selection of individual drivers at each truck stop was estimated as: (number of eligible drivers interviewed at the truck stop)/(estimated total number of eligible drivers at the truck stop). The total number of eligible drivers at a truck stop was estimated from foot counts taken during random 15-min periods multiplied by an eligibility rate, which was based on the percentage of eligible drivers out of all drivers receiving screening or non-respondent interviews at that truck stop. Since some individuals ignored interviewers when approached for survey participation, it could not be determined whether these individuals were eligible LHTD, non-eligible truck drivers, passengers, or others who used the truck stop. We assumed that the eligibility rate and demographics for these individuals was the same as for those drivers whose eligibility was known from the screening and non-respondent interviews. The final driver weight included a non-response adjustment to account for drivers who refused participation and a raking adjustment on six dimensions (traffic flow stratum, truck driver status, age, gender, health status, and BMI) [Rizzo et al., 1996].
Statistical Analysis
Descriptive statistics including national estimates of the total number of LHTD and percentages of drivers responding to individual interview questions were determined as the sum of the weights for responding truck drivers. Variances of the national estimates were calculated using the jackknife replication method for complex survey data [Rust and Rao, 1996].
Prevalence of self-reported health conditions and risk factors among LHTD and in the 2010 National Health Interview Survey (NHIS) adult working population were compared. Age- and sex- adjustment of the LHTDS and 2010 NHIS populations was required to meaningfully compare the two, because of the different age and sex distributions in each. Estimates were age-and sex-adjusted to the U.S. year 2010 employed population using employment data from the 2010 Current Population Survey (CPS) [BLS, 2011]. Age groups 16–19, 20–29, 30–39, 40–49, 50–59, and 60–69 and 70 years and older were used. t-Tests of statistical significance were performed to compare self-reported health conditions and risk factors from the LHTDS with those from the NHIS [Korn and Graubard, 1999]. Variance estimates needed to compare the LHTDS and NHIS estimates were calculated using the Taylor series method [Rust and Rao, 1996].
The CPS is a household, multistage probability sample survey conducted monthly by the Bureau of the Census for the Bureau of Labor Statistics to provide data on employment and unemployment in the nation’s population. Data are collected on the non-institutionalized U.S. civilian population ages 16 and above [BLS, 2006]. The NHIS is a household, multistage probability sample survey conducted annually by the National Center for Health Statistics [NCHS, 2006]. Data were available for 15,323 currently employed adults between the ages of 20 and 80 in 2010.
Body mass index (BMI)
BMI was calculated as [weight (kg)]/[height (m)]2: weight categories were defined as: underweight, BMI <20; normal weight, 20 ≤ BMI <25; overweight, 25 ≤ BMI <30; obese, BMI ≥ 30; and morbid obesity, BMI ≥ 40 kg/m2 [CDC, 2012a]. When anthropometric measurements were not obtained (305 individuals), values for height and weight were imputed using a hot deck statistical procedure based on self-reported values of height and weight obtained during the personal interviews [Rubin, 2008]. Imputed and measured height and weight values were used to calculate BMI.
Age- and sex- adjusted estimates were calculated using SUDAAN V. 10.0 [Research Triangle Institute, 2008]. All other estimates were calculated using SAS V. 9.3 [SAS Institute, 2011]. Further details on the survey procedures and sample selection are available from the lead author (WKS). The survey was approved by the Office of Management and Budget (OMB no. 0920–0865) and NIOSH Human Subjects Review Board. A waiver of documentation of informed consent was requested since no personal identifying information was collected.
RESULTS
Table I shows that of the total 5,514 individuals approached by interviewers for participation in the LHTDS, 3,759 were estimated to be long-haul drivers meeting eligibility criteria for it. One thousand six hundred seventy drivers (44% of the 3,759 estimated total eligible drivers) participated in at least one component of the survey: 1,265 (76%) completed the personal interview, 960 (58%) had height and weight measurements taken and 405 (24%) completed the non-respondent interview only. Two thousand eighty-nine drivers (56% of the estimated eligible drivers) refused interviewer efforts to recruit them. When screening or non-respondent interview respondents indicated reasons for non-participation, reasons given were time constraints (N = 403), language barriers (N = 7), lack of interest (N = 4), and privacy concerns and governmental interference (N = 3).
TABLE I.
Number and Geographic Region of Respondents, Survey of U.S. Long-Haul Truck Drivers, Fall 2010
| Description | Number | Percent of respondents |
|---|---|---|
| Total number of individuals approached to participate | 5,514 | N.A. |
| Total number of eligible drivers approached (estimated)a | 3,759 | N.A. |
| Total eligible drivers participating in survey | 1,670 | 100.0 |
| Survey component completed | ||
| Personal interview | 1,265 | 75.7 |
| Anthropometric measurements takenb | 960 | 57.5 |
| Non-respondent interview only | 405 | 24.3 |
| Geographic regionc where personal interview completed (number of truck stops) | ||
| Northeast (3) | 91 | 7.2 |
| Great Lakes (8) | 326 | 25.8 |
| South (9) | 369 | 29.2 |
| Central (6) | 257 | 20.3 |
| West (6) | 222 | 17.6 |
N.A., not applicable.
Based on responses to screening questionnaire.
Anthropometric measurements were offered only if a personal interview was given. All drivers self-reported height and weight as part of the personal interview.
- Northeast: New Hampshire, New York.
- Great Lakes: Ohio, Michigan, Indiana, Minnesota.
- South: Virginia, South Carolina, Tennessee, Florida, Arkansas, Louisiana.
- Central: Iowa, Nebraska, Kansas, Texas.
- West: Oregon, California, Arizona.
Findings from the personal interview and anthropometric components of the LHTDS are presented in Tables II–IV. Ninety-four percent of the participants were male (Table II). Ages of drivers in this study were between 20 and 80 years with a mean age of 48. Seventy-four percent of drivers were white, 17% were Black or African-American, and 7% reported other or multiple races. Nine percent were of Hispanic ethnicity.
TABLE II.
Demographic Characteristics, Survey of U.S. Long-Haul Truck Drivers, Fall 2010
| Description | Weighted national estimate (percent)a | 95% Confidence interval | Number of drivers observed (out of N =1,265) |
|---|---|---|---|
| Gender | |||
| Male | 93.5 | (91.3, 95.6) | 1,184 |
| Female | 6.5 | (4.4, 8.7) | 81 |
| Age range (years) | |||
| 20–29 | 5.1 | (3.1, 7.1) | 69 |
| 30–39 | 16.9 | (12.6, 21.3) | 254 |
| 40–49 | 32.9 | (29.8, 36.0) | 401 |
| 50–59 | 29.2 | (24.9, 33.5) | 386 |
| 60–69 | 14.8 | (8.4, 21.2) | 142 |
| 70–80 | 1.1 | (0.1, 2.1) | 13 |
| Hispanic or Latinob | 8.6 | (5.2, 12.1) | 106 |
| Race | |||
| White | 73.5 | (69.9, 77.2) | 923 |
| African American | 17.1 | (10.6, 23.6) | 196 |
| Other or multiple racec | 6.9 | (3.4,10.4) | 106 |
| Unknown | 2.5 | (0.5,4.5) | 40 |
| Marital status | |||
| Married | 58.0 | (51.3, 64.6) | 676 |
| Not married | 41.9 | (35.4, 48.4) | 586 |
| Refused/missing | 0.1 | (0.0, 0.4) | 3 |
| Education | |||
| High school or less | 55.5 | (52.0, 59.0) | 686 |
| College or above | 44.4 | (41.0, 47.8) | 577 |
| Refused/missing | 0.1 | (0.0, 0.3) | 2 |
| Employment | |||
| Company employee | 64.5 | (59.7, 69.4) | 816 |
| Owner-operator | 35.5 | (30.6, 40.3) | 449 |
| Type of company working or contracting for | |||
| For hire | 90.0 | (86.2, 93.7) | 1,142 |
| Private carriage | 8.3 | (4.4, 12.2) | 103 |
| Both for hire and private carriage | 1.2 | (0.0, 2.6) | 15 |
| Don’t know/refused/missing | 0.5 | (0.0, 1.1) | 5 |
Weighted national estimates using 1,265 survey responses.
Hispanic ethnicity includes Spanish, Mexican, Mexican-American, Chicano, Puerto-Rican, Cuban, Dominican(Republic), Central or South American, Other Latin American, or other Hispanic/Latino.
Other race includes Asian, Native American, Native Hawaiian or Pacific Islander, and unknown.
TABLE IV.
Prevalence of Self-reported Health Conditions, Risk Factors, and Health Care Coverage, Fall 2010 Survey of U.S. Long-Haul Truck Drivers, Compared to Prevalence Reported by Working Adults in the 2010 National Health Interview Survey (NHIS)
| Self-reported health condition/risk factor | Survey of U.S. Long-Haul Truck Drivers
|
2010 NHIS
|
|||
|---|---|---|---|---|---|
| Weighted national prevalence estimate (percent)a | 95% Confidence interval | Number of drivers observed (out of N = 1,265) | Weighted national prevalence estimate (percent)a | 95% Confidence interval | |
| Heart diseaseb | 4.4** | (3.1, 6.2) | 98 | 6.7 | (6.3, 7.2) |
| Diabetesc | 14.4* | (9.4, 21.6) | 180 | 6.8 | (6.3, 7.2) |
| Hypertensiond | 26.3 | (20.6, 33.0) | 421 | 24.1 | (23.3, 24.9) |
| High cholesterole,h | 21.7 | (16.4, 28.2) | 341 | No data | |
| Body mass index (BMI)f | |||||
| Underweight (BMI <20) | 0.4** | (0.1, 1.9) | 6 | 4.6 | (4.2, 5.0) |
| Normal (20 ≤ BMI <25) | 7.9** | (5.5, 11.2) | 132 | 30.0 | (29.1, 30.9) |
| Overweight (25 ≤ BMI <30) | 22.8** | (17.0, 29.8) | 312 | 34.9 | (34.0, 35.9) |
| Obese (BMI ≥ 30) | 68.9** | (61.7, 75.3) | 815 | 30.5 | (29.6, 31.4) |
| Morbid obesity (BMI ≥ 40) | 17.4** | (11.6, 25.3) | 210 | 7.3 | (6.8, 7.8) |
| No moderate or vigorous physical activity for 30 min in past 7 daysh | 27.1 | (19.8, 35.8) | 383 | No data | |
| Perceived health status | |||||
| Excellent, very good, or good | 83.5** | (75.6, 89.2) | 1,035 | 93.9 | (93.5, 94.4) |
| Fair or poor | 16.5** | (10.8, 24.4) | 230 | 6.1 | (5.6, 6.5) |
| Current cigarette smokerg | 50.7** | (41.7, 59.7) | 586 | 18.9 | (18.1, 19.7) |
| Does not drink alcohol | 38.9** | (30.8, 47.5) | 484 | 10.9 | (10.3, 11.5) |
| Average hours of sleep in a 24-hr period | |||||
| 6 hr or less | 26.5 | (19.5, 35.4) | 319 | 30.0 | (29.2, 30.8) |
| Between 6 and 8 | 51.4** | (42.1, 60.5) | 651 | 63.9 | (63.1, 64.8) |
| Greater than 8 | 22.1** | (17.0, 27.9) | 292 | 5.0 | (4.8, 5.4) |
| Not covered by health insurance or health care plan | 38.1** | (30.7, 46.2) | 414 | 17.2 | (16.5, 18.0) |
| Delayed or did not receive needed health care in past 12 months | 18.3* | (11.5, 27.7) | 217 | 9.7 | (9.1, 10.2) |
| Did not receive flu shot in last 12 months | 80.2** | (73.1, 85.9) | 1,007 | 67.0 | (66.1, 67.9) |
P <0.05 compared to NHIS.
P <0.01 compared to NHIS.
Weighted national prevalence estimates. Estimates are sex- and age-adjusted to the year 2010 working population using age groups 16–19, 20–29, 30–39, 40–49, 50–59, 60–69, and 70 years or older.
Heart disease was defined as ever having been told by a health professional of having coronary heart disease, angina, or any other heart condition.
Diabetes was defined as ever having been told by a health professional of having diabetes.
Hypertension in the LHTDS was defined as currently taking medicine to lower blood pressure, or ever having been told by a health professional that of having high blood pressure. It was defined in the NHIS as ever having been told by a health professional of having high blood pressure.
High cholesterol was defined as currently taking medicine to lower cholesterol, or ever having been told by a health professional of having high cholesterol.
Body mass index (BMI) is defined as: BMI = ((weight [lbs] × 703)/(height [in.])2). Imputed and measured values of height and weight were used to calculate BMI.
Current cigarette smoking is defined as ever having smoked at least 100 cigarettes and currently smoking every day or some days.
This question was not included in the NHIS.
Work history and driving practices are described in Table III. Participating drivers had worked an average of 16 years as a LHTD (range: 1–54 years). During the previous 7-day period, drivers had worked an average 60 hr. Those tasks which respondents indicated they spent an average of 2 or more hours per week are shown in Table III and include driving (46.2 hr), waiting for the dispatcher or completing paperwork (7.3 hr), loading/unloading/securing the load (2.9 hr), and truck maintenance or repair (1.8 hr). Other tasks included waiting (other than for the dispatcher) (1.5 hr), other work at the terminal (0.4 hr), and other jobs to get the load (0.2 hr), training (0.1 hr), and inspection/fueling (0.1 hr). Nearly 45% had spent only 1–6 days sleeping at home in the past 30 days, while 18% had not slept at home in the past 30 days.
TABLE III.
Work History and Driving Practices, Survey of U.S. Long-Haul Truck Drivers, Fall 2010
| Description | Weighted national estimatea | 95% Confidence interval | Number of drivers observed (out of N = 1,265) |
|---|---|---|---|
| Mean number of years worked as a long-haul truck driver | 16.4 | (14.4, 18.5) | 1,265 |
| Mean miles driven in past 12 months | 107,668 | (101,407, 113,929) | 1,262 |
| Mean total number of hours worked in last 7 days | 60.4 | (56.3, 64.5) | 1,265 |
| Average hours on task | |||
| Driving | 46.2 | (44.2, 48.2) | 1,259 |
| Waiting for dispatcher, completing paperwork | 7.3 | (6.0, 8.6) | 968 |
| Loading/unloading/securing the load | 2.9 | (1.8, 3.9) | 592 |
| Truck maintenance or repair | 1.8 | (0.7, 2.8) | 553 |
| Driving practice on current trip | |||
| Driving alone | 78.2% | (70.4, 86.0) | 1,003 |
| Driving with others | 21.8% | (14.0, 29.6) | 262 |
| Type of freight shipment on current trip | |||
| Less than truckload freightb | 16.1% | (11.5, 20.7) | 212 |
| Truckload freightc | 74.6% | (68.0, 81.1) | 942 |
| Don’t know/refused/missing | 9.4% | (5.9, 12.9) | 111 |
| Drivers with a second job | 2.2% | (0.9, 3.4) | 37 |
| Union membership | 2.6% | (1.1, 4.1) | 39 |
| Number of days sleeping at home in past 30 days | |||
| 0 days | 18.3% | (14.1, 22.5) | 250 |
| 1–6 days | 44.6% | (39.8, 49.5) | 558 |
| 7 or more days | 37.1% | (30.3, 43.9) | 456 |
| Don’t know/refused/missing | 0.02% | (0.0,0.07) | 1 |
| Hours usually driven before stopping for a break or fuel | |||
| 4 hr or less | 49.3% | (45.9, 52.6) | 594 |
| Between 5 and 8 hr | 42.0% | (39.6, 44.4) | 545 |
| More than 8 hr | 7.2% | (5.2, 9.3) | 109 |
| Don’t know/refused/missing | 1.5% | (0.2, 2.8) | 17 |
Weighted national estimates using 1,265 survey responses.
Less than truckload (LTL) freight is defined as carrying multiple shipments each under 10,000 lbs to be delivered to one or more terminals or receivers [Burks et al., 2010].
Truckload (TL) freight is defined as carrying one or more shipments each over 10,000 lbs to be delivered directly to one or more receivers [Burks et al., 2010].
BMI of drivers in this study ranged from 17.2 to 61.7. Over two-thirds of respondents were obese while 17% were morbidly obese (BMI ≥ 40 kg/m2) (Table IV). In comparison, only one-third of U.S. working adults were reported to be obese and 7% morbidly obese by the 2010 NHIS (P <0.01).
We calculated the self-reported prevalence of chronic conditions based on whether drivers had ever been told by a health care professional that they had the condition. The reported prevalence of health professional-diagnosed heart disease in LHTD was significantly lower from that in the U.S. adult NHIS working population (4.4% vs. 6.7%, P <0.01), while diabetes mellitus was significantly elevated (14.4% vs. 6.8%, P <0.05). However, the prevalence of hypertension was not different from that reported by the NHIS (26.3% vs. 24.1%). Twenty-two percent were either taking medicine for, or had been told they had, high cholesterol. Twenty-seven percent of drivers reported no moderate or vigorous physical activity of at least 30 min duration during the previous 7 days. There were no comparable questions on high cholesterol or physical activity in the NHIS.
Almost 51% of LHTD were current cigarette smokers, compared to 19% current smokers in the 2010 NHIS (P <0.01). Although most drivers averaged >6 hr of sleep per 24-hr period, 27% of drivers averaged 6 hr or less of sleep compared to 30% of working adults. Eighty-four percent of drivers perceived their health status to be excellent, very good, or good, compared to 94% in the NHIS (P <0.01).
Twice as many (38%) drivers were not covered by health insurance or a health care plan compared to 17% of all working adults (P <0.01). Eighteen percent had delayed, or had not received, needed health care in the previous 12 months, twice that in the 2010 NHIS, while 80% had not received a flu shot in the previous 12 months. Sixty-seven percent of the adult working population had not received a flu shot in the previous 12 months.
DISCUSSION
Our population-based survey is the first to provide national estimates of health conditions, risk factors, and work practices for U.S. Long-Haul Truck Drivers. We found obesity to be twice as prevalent in long haul truck drivers as reported in the 2010 adult working population in the NHIS. Although the prevalence of overweight workers in the U.S. adult working population (35%) was higher than in LHTD (23%), 69% of LHTD were obese compared to 31% in the U.S. adult working population. We also found a high prevalence of current smoking among LHTD (51%), over twice the percentage reported in the U.S. adult working population (19%).
LHTD face a constellation of interrelated risk factors for chronic disease. Obesity has been associated with numerous health conditions, including heart disease, diabetes mellitus, hypertension, high cholesterol, and sleep apnea [NIH, 1998; Thompson et al., 1999]. Smoking is a strong risk factor for lung cancer, heart, and other disease. Eighty-eight percent of LHTD reported at least one of three risk factors: hypertension, smoking, or obesity, and 9% reported all three conditions, compared to 54% of the NHIS adult working population reporting 1 or more of these risk factors and 2% indicating all three. Additional risk factors are high cholesterol, physical inactivity, and short and long sleep duration [Sabanayagam and Shankar, 2010]. Four percent of our drivers did not report any of the risk factors hypertension, obesity, smoking, high cholesterol, no moderate or vigorous physical activity for at least 30 min duration during the previous week, or 6 or fewer hours of sleep per 24-hr period; 61% reported having 2 or more, and 1% indicated all six risk factors.
Moderate to vigorous physical activity of 30–60 min per day for 5 or more days per week is recommended for adults for health benefits [Physical Activity Guidelines Advisory Committee, 2008; CDC, 2012b]. Only 24% of drivers in our study met these guidelines. Increased physical activity alone may have limited impact on levels of obesity, however. In this study, approximately 60% of the drivers who met physical guidelines were obese. Sixty percent of those drivers who did not meet guidelines were also obese. Lack of correlation between physical activity and obesity has been found in other studies [NIH, 1998; Petersen et al., 2004; Dwyer-Lindgren et al., 2013]. Dietary treatment, communication of health benefits of physical activity and increased physical activity are recommended as part of treatment for weight loss and weight maintenance in adults [NIH, 1998].
Truck drivers may not be able to obtain a commercial driving license (CDL) if they have any medical condition that is likely to interfere with the ability to control and drive a commercial motor vehicle safely. To meet medical certification, they must undergo at least biennial physical examinations as part of a medical screening process. Disqualifying conditions include diabetes mellitus, a history of heart disease severe enough to cause syncope or other serious symptoms, epilepsy, uncontrolled high blood pressure, and addiction to illicit drugs or alcohol. [Qualifications of drivers and longer combination vehicles (LCV) driver instructors, 2013]. Health conditions in both the LHTDS and NHIS were self-reported based only on whether the respondent had ever been told of the condition by a health care professional. Diabetes mellitus prevalence was found to be 14% in the LHTDS. Diabetes mellitus is a disqualifying condition for a CDL if the driver has experienced a severe hypoglycemic reaction in the past 12 months or twice in the past 5 years, but is not a disqualifying condition if the driver meets CDL physical qualification standards and has a treatment plan that does not include the use of insulin. Insulin-using drivers with diabetes mellitus may, however, qualify for a CDL under the Federal Diabetes Exemption program which requires annual evaluation by an endocrinologist and ophthalmologist/optometrist [Grandfathering for certain drivers participating in vision and diabetes waiver study programs, 2013]. Control of diabetes mellitus was not asked in the LHTDS, which may account for the high prevalence of diabetes in the LHTDS compared to the NHIS adult working population (14.4% vs. 6.8%, P <0.05). Use of medication to control blood pressure and high cholesterol levels was asked during the LHTDS (but not in the NHIS).
Even with a preponderance of health risk factors, fully 83% of LHTD perceived their health to be excellent, very good, or good. Perceived health status has been shown to be inversely related to the number of physician contacts per year [Miilunpalo et al., 1997]; many drivers may feel that their mandatory medical examinations at least every 2 years are sufficient and, therefore, do not seek other medical care. We found that twice as many drivers (18%) had delayed or did not receive needed health care in the previous 12 months compared to the NHIS adult working population. Eighty percent of LHTD had not received a flu shot in the previous 12 months compared to 67% in the NHIS workers.
Lack of health insurance may be reflected in this low utilization of medical resources among LHTD. Twice as many LHTD (38%) were not covered by health insurance or any health care plan as in the U.S. adult working population (17%). The percentage of drivers not covered is similar to the 31% uninsured long-distance drivers reported by Solomon et al. [2004]. Health coverage has been associated with education level and socioeconomic class. Thirty-four percent of workers in the U.S. adult working population have high school or less education, compared to 56% of the drivers in the LHTDS. Almost half of truck drivers have been reported not to have a regular health provider due to factors such as irregular schedules or inconvenient locations, lack of insurance, or high cost [Solomon et al., 2004; Stasko and Neale, 2007; Angeles et al., 2013]. Others have reported that working conditions such as time pressure, hours worked on the job, drivers’ degree of control over their work schedule, type of compensation, time spent at home, and other characteristics of work schedules may negatively impact health and safety, stress, and levels of fatigue and sleepiness [Orris et al., 1997; McCartt et al., 2000; Freund, 2006; Taylor and Dorn, 2006; Stasko and Neale, 2007; Friswell and Williamson, 2010; Van der Beek, 2012].
The overweight and obesity issues of LHTD in our study are not unique to this survey population. Guan found a mean BMI for U.S. truck drivers of 33.2 [Guan et al., 2012], almost the same as the mean BMI in the LHTDS (33.4). However, studies in other countries have found long-distance truck drivers to have lower mean BMI than in the LHTDS. Long-distance truck drivers were found to have an average BMI of 24 in Japan [Koda et al., 2000]; an average BMI of 28.6 in England and Scotland [Robb and Mansfield, 2007]; average BMI of 29.7 in Australia [Howard et al., 2004]; and average BMI of 29 in Argentina [Perez-Chada et al., 2005]. Fifteen percent of 160 Israeli port drivers were obese and 38% overweight [Sabbagh-Ehrlich et al., 2005]; while 53% of 406 Canadian drivers perceived themselves to be overweight [Angeles et al., 2013].
Strengths and Limitations
Based on our weighted sample size, LHTD eligible for this study represented an estimated 857,600 truck drivers nationally, or about 60% of the total number (1.5 million) drivers of heavy and tractor-trailer trucks shown by the BLS in 2010 [BLS, 2010b].
Current health and injury surveillance systems are limited in that they often do not distinguish between the types of drivers who are represented. For example, occupational data for long-haul drivers as a single group are not available in the CPS because the CPS currently combines drivers of heavy and tractor trailer trucks with driver-sales workers. Additionally, work characteristics and illness and injury patterns vary between regional or drivers-sales workers, who may drive shorter routes and return home each day, and long-haul drivers, who drive longer routes and may be away from home for days at a time.
Since this is a cross-sectional study, causality cannot be determined. Results can best be used to examine associations between risk factors, health and chronic disease. Respondents to this cross-sectional survey were drivers on the road who visited truck stops during the fall of 2010. Missing from the sample were current drivers who were on vacation or scheduled breaks, seasonal drivers, and part-time drivers, those who did not patronize truck stops or any of the participating truck stops; and drivers who may have been ill or injured and not driving at the time. Ideally, a survey of LHTD should be repeated at different times of the year to reflect trucking activity throughout the year. Many individuals did not wish to participate or ignored interviewers, often because of limited time at the truck stop or possibly because they felt they were already in good health. Slightly more respondents to the non-respondent interview perceived their health to be good or better compared to drivers completing the personal interview (89% vs. 81%), so it is possible that prevalence estimates based on personal interviews may slightly over-estimate ill health and risk factors among LHTD. It was assumed that eligible drivers who patronized nonparticipating truck stops had similar demographic characteristics to drivers completing the non-respondent and personal interviews at participating truck stops.
Self-reported data collected in this study were subject to recall and interviewer bias. Bias was limited by the use of standard interview protocols and survey-specific training, including use of probes. It is also possible that the financial incentives provided for participation could have biased driver responses if respondents thought that questions were based on maintaining one’s job. To minimize possible bias in self-reported anthropometric data, only measured or imputed height and weight values were used to calculate BMI.
In this study, the number of truck stops in each geographical region was selected to be proportional to the length in miles of selected highways in that region. This selection scheme accounts for the lack of truck stops in the eastern part of the West region, and low number of truck stops in the Northeast region. The Northeast region participation rate was significantly higher than in other regions. This could have been due to shorter distances travelled by LHTD in the Northeast region (allowing more time to participate) or more interest in the LHTDS. Respondents in the Northeast region had a higher level of education than respondents in other regions. There were no statistical differences by region between proportions of respondents by gender, marital status, age, and years worked.
CONCLUSION
Our survey is one of the largest in-depth health Survey of U.S. Long-Haul Truck Drivers to be conducted in the U.S. It is the first to document LHTD work practices, health risks, and chronic diseases and provide nationally representative estimates. Our survey found a constellation of chronic disease risk factors to be present among LHTD. These included hypertension, high cholesterol, obesity, smoking, physical inactivity, and sleep duration. The high prevalence of obesity and smoking, prevalence of self-reported health conditions, and low utilization of health resources by truck drivers are primary findings from the survey. This study suggests a need for targeted interventions to meet the health needs of LHTD and surveillance through repeated data collections to track progress in meeting these health needs. Such surveys may be used to guide development of trucking policy and health programs.
Acknowledgments
This work was supported by the National Institute for Occupational Safety and Health with partial funding from the Federal Motor Carrier Safety Administration, U.S. Department of Transportation. We wish to thank Albert Alvarez, Rebecca Brewster, Dale Belman, Michael Belzer, LaMont Byrd, Gerald Donaldson, Eric Garshick, Jim Helmkamp, Gerald Krueger, Scott Madar, Anne McCartt, Stephanie Pratt, Roger Rosa, Andy Schaudt, John Sestito, Aaron Sussell, Thomas Weakley, Martin Walker, Ann Williamson, and Eric Wood for their helpful comments and/or guidance in development of our survey and questionnaire. Teri Jacobs, Hovi Nguyen and Matthew Groenewold prepared maps. We in particular wish to thank the participating truck stops and drivers without whom this data collection would not have been possible. Westat Inc. provided data collection and statistical support. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Footnotes
Disclosure Statement: The authors report no conflicts of interests.
References
- Angeles R, McDonough B, Howard M, Dolovich L, Marzanek-Lefebvre F, Qian H, Riva JJ. Work. 2013. 00. IOS Press; 2013. Primary health care needs for a priority population: A survey of professional truck drivers; pp. 1–7. [DOI] [PubMed] [Google Scholar]
- Apostolopoulos Y, Sonmez S, Shattell M, Belzer M. Worksite-induced morbidities among truck drivers in the United States. AAOHN J. 2010;58(7):285–296. doi: 10.3928/08910162-20100625-01. [DOI] [PubMed] [Google Scholar]
- Belman DL, Monaco AK, Brooks TJ. Sailors on the concrete sea: A portrait of truck drivers’ work and lives. East. Lansing, Michigan: Michigan State University Press; 2005. p. 207. [Google Scholar]
- Bigelow PI, Betts D, Hogg-Johnson S, Amick BC, Sieber WK, Skinner M, Jakubicek M. Health, safety, and wellness of truck drivers in Canada: Results of a pilot study. In: Krueger GP, editor. Research on the health and wellness of commercial truck and bus drivers: Summary of an international conference. Washington DC: Transportation Research Board; 2012. pp. 95–105. Available at: http://onlinepubs.trb.org/onlinepubs/conf/cpw5.pdf. [Google Scholar]
- Birdsey J, Alterman T, Li J, Petersen MR, Sestito J. Mortality among members of a truck driver trade association. AAOHN J. 2010;58(11):473–480. doi: 10.3928/08910162-20101018-01. [DOI] [PubMed] [Google Scholar]
- BLS. Design and methodology: Current population survey. Technical paper 66. 2006 Oct; 2006. Available at: http://www.census.gov/prod/2006pubs/tp-66.pdf.
- BLS. Nonfatal occupational injuries and illness requiring days away from work, 2010. 2010a Available at: http://www.bls.gov/news/release/osh2.nr0.htm.
- BLS. National occupational employment and wage estimates, United States, May 2011. 2010b Available at: http://www.bls.gov/oes/2011/may/oes_nat.htm.
- BLS. Employment status of the civilian noninstitutional population by age, sex, and race. 2011 Available at: http://www.bls.gov/cps/cpsaat03.pdf.
- BLS. Industries at a glance: Transportation and warehousing: NAICS 48–49. 2013 Available at: http://www.bls.gov/iag/tgs/iag48-49.htm.
- Brice TA. The trucker’s friend and national truck stop directory 2008. Clearwater, FL: TR Publications; 2008. [Google Scholar]
- Burks SV, Belzer M, Kwan Q, Pratt S, Shackelford S. Trucking 101: An industry primer. Transportation research circular E-C146. 2010 Available at: http://onlinepubs.trb.org/onlinepubs/circulars/ed146.pdf.
- CDC. Behavioral risk factor surveillance system survey questionnaire. 2007a Available at: http://www.cdc.gov/BRFSS/questionnaires/english.htm.
- CDC. National Health and Nutrition Examination Survey (NHANES): Anthropometry procedures manual. 2007b Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf.
- CDC. Healthy weight. 2012a Available at: http://www.cdc.gov/healthyweight/assessng/bmi.
- CDC. How much physical activity does an adult need? 2012b Available at: http://www.cdc.gov/physicalactivity/everyone/guidelines/adults.html.
- Dahl S, Kaerlev L, Jensen A, Tuchsen F, Hannerz H, Nielsen PS, Olsen J. Hospitalization for lifestyle related diseases in long haul drivers compared with other truck drivers and the working population at large. Work. 2009;33:345–353. doi: 10.3233/WOR-2009-0882. [DOI] [PubMed] [Google Scholar]
- Dwyer-Lindgren L, Freedman G, Engell RE, Fleming TD, Lim SS, Murray CJL, Mokdad AH. Prevalence of physical activity and obesity in US counties, 2001–2011: A road map for action. Population Health Metrics. 2013;11:7. doi: 10.1186/1478-7954-11-7. Available at: http://www.pophealthmetrics.com/content/11/1/7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FHWA. DOT Publication No. FHWA-MCRT-99-006. Washington, DC: Department of Transportation; 1999. Commercial truck driver fatigue, alertness, and countermeasures survey. Available at: http://www.fmcsa.dot.gov/documents/tb.99-006.pdf. [Google Scholar]
- FHWA. Freight analysis framework V. 2. Estimated daily long-haul traffic on the National Traffic System within geographic regions, 2002. 2007 Available at: http://ops.fhwha.dot.gov/freight/freight_analysis/faf/index.htm.
- FMCSA. Truck driver fatigue management survey, 2006. 2006 Available at: http://www.fmcsa.dot.gov/facts-research/research-technology/report/Truck-Driver-Fatigue-Management-Survey-Report.pdf.
- Freund DM. CMV safety: A new focus on the driver. National Occupational Research Agenda (NORA) symposium 2006: Research Makes a difference; April 18–20, 2006; Washington, DC: U.S. DHHS, CDC, NIOSH; 2006. pp. 358–359. Available at: http://www.cdc.gov/niosh/nora/symp06/pdfs/norasymposium2006book.pdf. [Google Scholar]
- Friswell R, Williamson A. Work characteristics associated with injury among light/short-haul transport drivers. Accid Anal Prev. 2010;42:2068–2074. doi: 10.1016/j.aap.2010.06.019. [DOI] [PubMed] [Google Scholar]
- Garshick E, Laden F, Hart JE, Rosner B, Davis ME, Eisen EA, Smith TJ. Lung cancer and vehicle exhaust in trucking industry workers. Environ Health Perspect. 2008;116(10):1327–1332. doi: 10.1289/ehp.11293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandfathering for certain drivers participating in vision and diabetes waver study programs. 49CFR Part 391.6, 2013.
- Guan J, Hsiao H, Bradtmiller B, Kau T-Y, Reed MR, Jahns S, Loczi J, Hardee HL, Piamonte D. U.S. truck driver anthropometric study and multivariate anthropometric models for cab designs. Hum Factors. 2012;54(5):859–870. doi: 10.1177/0018720812442685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmkamp JC, Lincoln JE, Sestito J, Wood E, Birdsey J, Kiefer M. Risk factors, health behaviors and injury among adults employed in the transportation, warehousing, and utilities super sector. Am J Ind Med. 2013;56(5):556–568. doi: 10.1002/ajim.22148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard ME, Desai A, Grunstein R, Hulkins C, Armstrong JG, Joffe D, Swann P, Campbell DA, Pierce RJ. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–1021. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- Jain NB, Hart JE, Smith TJ, Garshick E, Laden F. Smoking behavior in trucking industry workers. Am J Ind Med. 2006;49:1013–1020. doi: 10.1002/ajim.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koda S, Yasuda N, Sugihara Y, Ohara H, Udo H, Otani T. Analyses of work-relatedness of health problems among truck drivers by questionnaire survey. Sangyo Eiseigaku Zasshi. 2000;42(1):6–16. doi: 10.1539/sangyoeisei.kj00002552185. [DOI] [PubMed] [Google Scholar]
- Korelitz JJ, Fernandez AA, Uyeda VJ, Spivey GH, Browdy BL, Schmidt RT. Health habits and risk factors among truck drivers visiting a health booth during a trucker trade show. Am J Health Promot. 1993;8(2):117–123. doi: 10.4278/0890-1171-8.2.117. [DOI] [PubMed] [Google Scholar]
- Korn EL, Graubard BI. Analysis of health surveys. New York, NY: John Wiley & Sons, Inc; 1999. p. 436. [Google Scholar]
- Krueger GP, editor. Research on the health and wellness of commercial truck and bus drivers: Summary of an international conference. Washington DC: Transportation Research Board; 2012. Available at: http://onlinepubs.trb.org/onlinepubs/conf/cpw5.pdf. [Google Scholar]
- Laden F, Hart JE, Smith TJ, Davis ME, Garshick E. Cause-specific mortality in the unionized U.S. trucking industry. Environ Health Perspect. 2007;115(8):1192–1196. doi: 10.1289/ehp.10027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh JP, Miller TR. Job-related diseases and occupations within a large workers’ compensation data set. Am J Ind Med. 1998;33(3):197–211. doi: 10.1002/(sici)1097-0274(199803)33:3<197::aid-ajim1>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Martin BC, Church TS, Bonnell R, Ben-Joseph R, Borgstadt T. The impact of overweight and obesity on the direct medical costs of truck drivers. J Occup Environ Med. 2009;51:180–184. doi: 10.1097/JOM.0b013e3181965d6e. [DOI] [PubMed] [Google Scholar]
- McCartt AT, Rohrbaugh JW, Hammer MC, Fuller SZ. Factors associated with falling asleep at the wheel among long-distance truck drivers. Accid Anal Prev. 2000;32:493–504. doi: 10.1016/s0001-4575(99)00067-6. [DOI] [PubMed] [Google Scholar]
- Miilunpalo S, Vuori I, Oja P, Pasanen M, Urpoen H. Self-rated health status as a health measure: The predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50(5):517–528. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- NCHS. National Health Interview Survey, 2006. 2006 Available at: http://www.cdc.gov/nchs/quest_data_related_1997_forward.htm.
- NIH. NIH publication number 94-4083. Bethesda, MD: U.S. DHHS, NIH, NHLBI; 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Available at: http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. [Google Scholar]
- Orris P, Hartman DE, Strauss P, Anderson RJ, Collins J, Knopp C, Xu Y, Melius J. Stress among package truck drivers. Am J Ind Med. 1997;31:202–210. doi: 10.1002/(sici)1097-0274(199702)31:2<202::aid-ajim10>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Perez-Chada D, Videla AJ, O’Flaherty ME, Palermo P, Meoni J, Sarchi MI, Khouory M, Duran-Cantollla J. Sleep habits and accident risk among truck drivers: A cross-sectional study in Argentina. Sleep. 2005;28(9):1103–1108. doi: 10.1093/sleep/28.9.1103. [DOI] [PubMed] [Google Scholar]
- Petersen L, Schnohr P, Sorensen TIA. Longitudinal study of the long-term relation between physical activity and obesity in adults. Int J Obesity. 2004;28:105–112. doi: 10.1038/sj.ijo.0802548. [DOI] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. Physical activity guidelines advisory committee report, 2008. Washington, DC: U.S. DHHS; 2008. Available at: http://www.health.gov/paguidelines/report/pdf/committeereport.pdf. [Google Scholar]
- Qualifications of driver and longer combination vehicles (LCV) driver instructors. 49 CFR Part 391 (2013).
- Research Triangle Institute. SUDAAN language manual, release 10.0. Research Triangle Park, NC: Research Triangle Institute; 2008. [Google Scholar]
- Rizzo L, Kalton G, Brick JM. A comparison of some weighting adjusting methods for panel nonresponse. Surv Methodol. 1996;22:43–53. [Google Scholar]
- Robb MJM, Mansfield NJ. Self-reported musculoskeletal problems amongst professional truck drivers. Ergonomics. 2007;50(6):814–827. doi: 10.1080/00140130701220341. [DOI] [PubMed] [Google Scholar]
- Roberts S, York J. Design, development and evaluation of driver wellness programs. Technical memorandum number one: Wellness literature and programs review. 1997 Available at: http://www.fmcsa.dot.gov/documents/wellness-2.pdf.
- Robinson CF, Burnett CA. Truck drivers and heart disease in the United States, 1979–1990. Am J Ind Med. 2005;47(2):113–119. doi: 10.1002/ajim.20126. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. Hoboken, NJ: John Wiley and Sons, Inc; 2008. p. 288. [Google Scholar]
- Rust KF, Rao JNK. Variance estimation for complex surveys using replication techniques. Stat Methods Med Res. 1996;5(3):283–310. doi: 10.1177/096228029600500305. [DOI] [PubMed] [Google Scholar]
- Sabbagh-Ehrlich S, Friedman L, Richter ED. Working conditions and fatigue in professional truck drivers at Israeli ports. Inj Prev. 2005;11:110–114. doi: 10.1136/ip.2004.007682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: Results from the National Health Interview Survey. Sleep. 2010;33(8):1037–1042. doi: 10.1093/sleep/33.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saltzman GM, Belzer MH. Truck driver occupational safety and health: 2003 conference report and selective literature review. Proceedings of truck driver occupational safety and health conference; April 24–25, 2003; Detroit, MI. Cincinnati, OH: U.S. DHHS, CDC, NIOSH; 2007. NIOSH document # 2007-120. [Google Scholar]
- SAS Institute Inc. Statistical analysis system V. 9.3. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- Solomon AJ, Doucette JT, Garland E, McGinn T. Healthcare and the long haul: Long distance truck drivers—A medically underserved population. Am J Ind Med. 2004;46:463–471. doi: 10.1002/ajim.20072. [DOI] [PubMed] [Google Scholar]
- Stasko JC, Neale AV. Health care risks and access within the community of Michigan over-the-road truckers. Work. 2007;29:205–211. [PubMed] [Google Scholar]
- Taylor AH, Dorn L. Stress, fatigue, health, and risk of road traffic accidents among professional drivers: The contribution of physical inactivity. Ann Rev Public Health. 2006;27:371–391. doi: 10.1146/annurev.publhealth.27.021405.102117. [DOI] [PubMed] [Google Scholar]
- Thompson D, Edelsberg J, Colditz G, Bird AP, Oster G. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159:2177–2183. doi: 10.1001/archinte.159.18.2177. [DOI] [PubMed] [Google Scholar]
- TRB. Future truck and bus safety research opportunities. Conference proceedings; Summary of conference; March 23–24, 2005; Arlington, Virginia. 2006. Available at: http://onlinepubs.trb.org/onlinepubs/conf/cp38.pdf. [Google Scholar]
- TRB. The domain of truck and bus safety research. Transportation Research Circular E-C117. 2007 Available at: http://onlinepubs.trb.org/onlinepubs/circulars/ec117.pdf.
- Van der Beek AJ. World at work: Truck drivers. Occup Environ Med. 2012;69:291–295. doi: 10.1136/oemed-2011-100342. [DOI] [PubMed] [Google Scholar]
- Williamson AM, Feyer AM, Coumarelos C, Jenkins T. Paper CR 190. Canberra ACT: Australian Transport Safety Bureau; 1992. Strategies to combat fatigue in the long-distance and transport industry. Stage 1: The industry perspective. [Google Scholar]
- Williamson A, Sadural S, Feyer AM, Friswell R. Driver fatigue: A survey of professional long distance heavy vehicle drivers in Australia Information Paper CR 198. Canberra ACT: Australian Transport Safety Bureau; 2001. [Google Scholar]
- Williamson A. Final report of stimulant use by long distance road transport drivers project. New South Wales Injury Risk Management Research Centre, University of New South Wales; 2006. A survey of stimulant drug use in long distance truck drivers in NSW; pp. 55–103. [Google Scholar]
- Wood E, Kinney A, Murtaugh M, Thiese MS, Hegmann KT. Health profile of commercial drivers. In: Krueger GP, editor. Research on the health and wellness of commercial truck and bus drivers: Summary of an international conference. Washington DC: Transportation Research Board; 2012. pp. 28–30. Available at: http://onlinepubs.trb.org/onlinepubs/conf/cpw5.pdf. [Google Scholar]