Abstract
This research evaluates condom-use self-efficacy and its increase throughout adolescence. Documentation of the development of condom-use self-efficacy would be important for prevention efforts given the influence of self-efficacy on actual condom-usage. This study assesses a hypothesized mediation mechanism of the development of self-efficacy using a mediation analysis approach. The participants, 497 grade-6 Bahamian students, were randomly assigned to the control condition in a 3-year longitudinal HIV prevention program trial. Condom–use self-efficacy consistently increased and condom-use self-efficacy assessed at earlier periods was positively associated with its values at subsequent periods. Additionally, self-efficacy assessed between two time points one year apart or longer (e.g., 6 months between baseline and 12 months) significantly mediated the impact of its levels at the previous assessment on the level at the subsequent assessment. To sustain program effect, HIV prevention programs should strive to enhance self-efficacy and provide reinforcing “boosters” no later than 12 months post-intervention.
Over the last quarter century, substantial progress has been made in effecting purposeful behavioral change to reduce HIV/AIDS risk behaviors (Uniting the World against AIDS [UNAIDS], 2007). A vast literature describing randomized, controlled trials and meta-analyses clearly demonstrates that interventions designed and executed with attention to specific elements (including sound theoretical grounding, specific skills development, and practice in communication and negotiation) can be successful in reducing and preventing sexual risk behaviors (Auerbach, Hayes, & Kandathil, 2006; Johnson, Carey, Marsh, Levin, & Scott-Sheldon, 2003; Kirby, 2002, 2007; Lyles et al., 2007; Mullen, Ramirez, Strouse, Hedges, & Sogolow, 2002; Robin et al., 2004; Ruiz et al., 2000; UNAIDS, 2007). Despite these advances, specific demographic and socio-geographic sub-groups remain at high risk and substantial challenges in maintaining purposeful behavioral change persist. Among those remaining at high risk are adolescents, young adults (Johnson, et al., 2003; Monasch & Mahy, 2006; Stephenson & Obasi, 2004), and individuals in transitional and developing countries (Beyrer, 2007; UNAIDS, 2007). Challenges that have continued to confront behavioral interventionists include inadequate information regarding long-term intervention effects (Chen et al., 2010; Pedlow & Carey, 2003), waning intervention effects over time (Darbes, Kennedy, Peersman, & Zohrabyan, 2002; DiClemente, Salazar, & Crosby, 2007), lack of attention to sustained behavioral changes (Chen, et al., 2010; Coates, Richter, & Caceres, 2008), and the need for interventions that address the changing environmental exposures and responses thereto that occur as children and adolescents mature (Kirby, Laris, & Rolleri, 2007).
Effective behavioral interventions require a thorough understanding of the mechanisms by which educational efforts lead to anticipated behavior change. Data from diverse sources indicate that self-efficacy is central in purposeful behavior change (Adih & Alexander, 1999; Johnston-Briggs, Liu, Carter-Pokras, & Barnet, 2008; Wang, Cheng, & Chou, 2009). Self-efficacy refers to beliefs a person has regarding his or her capability to perform a specific task or set of tasks (Bandura, 1997; Ormrod, 2000). Intervention studies demonstrate that levels of self-efficacy for HIV prevention can be enhanced through educational programs (Caceres, Rosasco, Mandel, & Hearst, 1994; Kyrychenko, Kohler, & Sathiakumar, 2006). Furthermore, self-efficacy significantly mediates the effect of educational interventions for adolescents to adapt HIV prevention behavior and to avoid HIV risk behavior (Chen et al., 2009; Chen, et al., 2010; Kalichman et al., 2002)
According to Social Cognitive Theory, adolescents with higher levels of self-efficacy regarding an act are more likely to accept challenges and to persevere to overcome difficulties confronted in performing that act (Bandura, Barbaranelli, Caprara, & Pastorelli, 1996, 2001; Bandura, Cioffi, Taylor, & Brouillard, 1988). Further, adolescents with high self-efficacy are also more likely than adolescents with low self-efficacy to devote greater efforts to perform a task for a longer period of time to achieve their goals (Bandura, 1977). In addition, evidence has shown that adolescents with higher levels of self-efficacy are more likely than others to learn and expand their skills, further enhancing their self-efficacy (Schunk, 1990). Indeed, self-efficacy is a prerequisite for the formation of behavioral intentions, the development of action plans, and the initiation of action (Schwarzer, 2008). Data from empirical studies indicate that among adolescents, lower self-efficacy beliefs regarding relevant behaviors significantly predicted a higher number of risk behaviors that are associated with increased likelihood of HIV infection (Holschneider & Alexander, 2003).
Both theory and empirical data support the notion that self-efficacy (including self-efficacy regarding condom-use) develops over the course of adolescence in a self-reinforcing fashion. Self-efficacy as a belief can be affected by many intra-personal and inter-personal factors, such as personal mastery experiences (success raises self-efficacy), modeling effect from vicarious experiences (If others can do it, I can do it as well), and social persuasion (I can do it because my teachers say I can) (Bandura, 1997). Higher levels of self-efficacy in early years may facilitate or self-reinforce the development of self-efficacy in subsequent years throughout adolescence. As an adolescent matures, he or she may become increasingly confident about his or her abilities to perform a specific task, including the use of a condom during sex. However, no reported study has examined whether and how self-efficacy itself at an earlier period affects its levels at subsequent periods. If an effect extends across three time points, in addition to a direct impact, is the relationship between the first and the last point statistically mediated by the level of self-efficacy assessed at the mid-point?
High levels of condom-use self-efficacy have been linked to protective behaviors against HIV infection among older adolescents and young adults (Basen-Engquist & Parcel, 1992; DiIorio et al., 2001; O’Leary, Jemmott, & Jemmott, 2008). For example, greater condom-use self-efficacy was associated with greater intention to use a condom in a sample of first-year college students (Joffe & Radius, 1993) and higher rates of condom-use among high school students aged 15–19 years (Richard & van der Pligt, 1991). Furthermore, research has shown an increase in condom-use self-efficacy over time in older adolescents (St. Lawrence et al., 1995). However, few studies have examined trends in condom-use self-efficacy in young adolescents. This evidence supports the importance of investigating condom-use self-efficacy beliefs and the development of these beliefs especially among preadolescents who are early in the process of sexual initiation.
Using six waves of longitudinal data, in this study, we examine the development of condom-use self-efficacy, including the mediation process of self-efficacy assessed in between two assessments, among an adolescent sample. We hypothesize that (1) condom-use self-efficacy will increase with age; (2) levels of the self-efficacy at an early age (time, e.g., baseline) will be positively associated with levels at subsequent ages (times); (3) furthermore, longitudinal associations across a period 12 months or longer will be mediated through the levels of self-efficacy during the intervening periods. The purpose of the analysis is to document the time course and mediation mechanism of self-efficacy regarding condom-use, and to provide new data enhancing our understanding of the role of self-efficacy and to support HIV prevention interventions for self-efficacy enhancement to increase condom-use.
Methods
Data Sources
Data used for this analysis were collected among pre- and early-adolescents in The Bahamas participating in a randomized controlled trial to assess the effect of an HIV prevention program (Chen, et al., 2009; Chen, et al., 2010; Deveaux et al., 2007; Gong et al., 2009). Six waves of longitudinal data (in 6-month intervals up to 24 months and a 12 month-interval between 24 and 36 months) were used. Participants (45.9% male) were sixth grade students, 10–11 years old (mean = 10.4, SD =.64) at the time of baseline survey.
Follow-up rates were 93% at 6-months, 87% at 12-months, 84% at 18-months, 84% at 24-months, and 81% at 36-months. For variables such as age, gender and all self-efficacy measurement scores, there were no significant baseline differences between students who participated at follow-up assessments compared to students who did not participate in the respective follow-ups. Detailed descriptions of the sample and data collection have been reported elsewhere (Chen, et al., 2009; Deveaux, et al., 2007; Gong, et al., 2009). Briefly, 15 schools were selected from among the 26 government elementary schools located on New Providence, the most populous island of The Bahamas. Participants whose data are included in the analyses were the 497 students attending the five schools, which were randomly assigned to receive the curriculum “Wondrous Wetlands”, an environmental conservation program (containing no information about HIV and condom-use) that served as the control condition. Since the participants in the control group were NOT exposed to educational interventions related to condom-use self-efficacy, data from this group can be used to describe the “natural” trends in self-efficacy. Data were collected using questionnaires in classroom settings. Students completed the surveys while a trained data collector read the survey questions aloud. One hour during class time was required to complete the survey at baseline and each follow-up. The study protocol was approved by the Institutional Review Boards from Wayne State University and the Ministry of Health, The Bahamas.
Measurement of Self-Efficacy
Six items were used to assess condom-use self-efficacy; agreement was measured through a five-point Likert scale (strongly agree = 5 to strongly disagree = 1) for the following statements: (1) I could get condoms; (2) I could put on a condom correctly; (3) I could convince my sexual partner to use a condom; (4) I could ask for condoms in a store; (5) I could ask for condoms in a clinic; and (6) I could refuse to have sex if my partner will not use a condom. This scale has been employed in behavioral intervention research conducted among adolescents in multiple nations, including the United States, Namibia, Vietnam and The Bahamas (Chen, et al., 2009; Kaljee et al., 2005; Stanton et al., 2004; Stanton et al., 1998). Psychometric analyses indicated adequate internal consistency of the scale, with Cronbach α varying from 0.82 to 0.87 for data collected at baseline and follow-up periods. Comparison analysis indicated that levels of self-efficacy assessed at baseline did not differ between those subjects who were retained and those who were lost to follow-up. Consequently, missing data on self-efficacy were imputed using the Markov Chain Monte Carlo (MCMC) method (Schafer, 1997).
Statistical Analysis
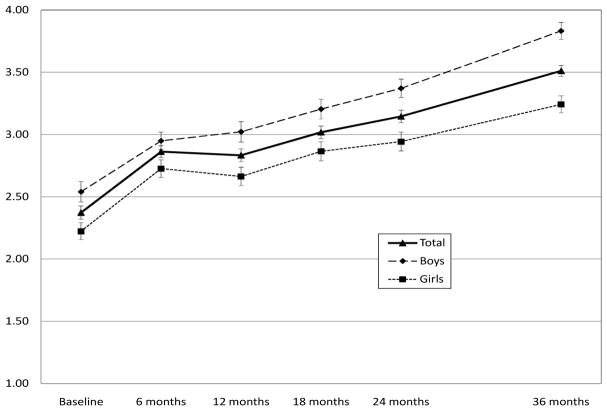
We assessed the levels of condom-use self-efficacy across the 36 months study period to test the first hypothesis, i.e., self-efficacy increases with age. We then constructed 15 regression models to assess levels of condom-use self-efficacy at an earlier time in predicting its levels at all subsequent times as seen in Figure 1(a) to test the second hypothesis, i.e. levels of the self-efficacy at an early age will be positively associated with its levels at subsequent ages. Finally, we constructed five path models to test the third hypothesis that self-efficacy assessed between two time points one-year apart or longer in mediating the effect of self-efficacy in an earlier time on a later time. As an example, Figure 1(b) indicates that the total effect of self-efficacy at baseline on self-efficacy at 12 months can be deconstructed into two components: a direct effect from baseline to 12 months and an indirect effect that is mediated through two consecutive paths (from baseline to 6 months and from 6 months to 12 months). In other words, a direct effect is similar to one individual passing a ball to another individual, while an indirect effect is similar to what occurs when a third person relays the ball between two other persons.
Figure 1.
Hypothesized models characterizing the intrinsic dynamics of self-efficacy among adolescents. Note for part B: The total effect from baseline self-efficacy = the direct effect beta (1) + the indirect effect mediated through beta (2) and beta (3). In addition, beta (2) and beta (3) assess the independent effect on self-efficacy assessed at 12 months from self-efficacy assessed at the baseline and the 6 months respectively.
Likewise, the total effect of baseline self-efficacy on self-efficacy at each subsequent period can be deconstructed by adding all possible direct effects and indirect paths. For example, the total effect of baseline efficacy on self-efficacy at 24 months will consist of four direct effects for self-efficacy assessed at baseline, 6 months, 12 months and 18 months and seven indirect paths, including a) baseline → 6 months → 24 months, b) baseline → 12months → 24 months, c) baseline → 18months → 24 months, d) baseline → 6 months → 12 months → 24 months, e) baseline → 6 months → 18 months → 24 months, f) baseline → 12 months → 18 months → 24 months, and g) baseline → 6 months → 12 months → 18 months → 24 months (see Table 3 for all indirect paths tested). We did not conduct the path model analysis by gender because of sample size limitations.
Table 3.
Indirect Effects for Individual Paths of the Four Different Path Models
| Paths for different models | Effect of a Indirect Path |
|---|---|
| Self-efficacy at 12 months (model 2 total) | .210** |
| 0 → 6 → 12 | .210** |
| Self-efficacy at 18 months (model 3 total) | .263** |
| 0 → 6 → 18 | .084** |
| 0 → 12 → 18 | .075** |
| 0 → 6 → 12 → 18 | .099** |
| Self-efficacy at 24 months (model 4 total) | .232** |
| 0 → 6 → 24 | .010 |
| 0 → 12 → 24 | .032** |
| 0 → 18 → 24 | .021 |
| 0 → 6 → 12 → 24 | .043** |
| 0 → 6 → 18 → 24 | .042** |
| 0 → 12 → 18 → 24 | .035** |
| 0 → 6 → 12 → 18 → 24 | .047** |
| Self-efficacy at 36 months (model 5 total) | .236** |
| 0 → 6 → 36 | .039* |
| 0 → 12 → 36 | .018* |
| 0 → 18 → 36 | .005 |
| 0 → 24 → 36 | .019 |
| 0 → 6 → 12 → 36 | .023* |
| 0 → 6 → 18 → 36 | .010* |
| 0 → 6 → 24 → 36 | .005 |
| 0 → 12 → 24 → 36 | .014* |
| 0 → 12 → 18 → 36 | .009* |
| 0 → 18 → 24 → 36 | .009 |
| 0 → 12 → 18 → 24 → 36 | .016** |
| 0 → 6 → 12 → 18 → 36 | .012* |
| 0 → 6 → 12 → 24 → 36 | .019** |
| 0 → 6 → 18 → 24 → 36 | .019** |
| 0 → 6 → 12 → 18 → 24 → 36 | .021** |
p<0.05,
p<0.01..
In conducting the path model analysis, the goodness-of-fit of a model to the data was assessed using R2. Other goodness-of-fit indices such as the comparative fit index (CFI) were not used because the saturated path models were tested and the levels of self-efficacy assessed at various times were highly correlated (see data in Table 1). We used a within-subject design to guide our statistical analysis to avoid any impact of individual differences in variables that may otherwise affect a youth’s developmental trajectory in a cross-sectional analysis; examples of variables that might impact developmental trajectory include prior sexual experience, condom-use, and gender. In a within subjects design, participants serve as their own controls and potential confounds from individual differences remain constant as the same individuals are followed longitudinally from baseline to 36 months (Tabachnick & Fidell, 2007).
Table 1.
Condom-Use Self-Efficacy at an Early Time Predicted Self-Efficacy at Later Times (Regression Coefficients)
| Self-efficacy at an early time as independent variable | Self-efficacy at a later time as dependent variable
|
||||
|---|---|---|---|---|---|
| 6 months | 12 months | 18 months | 24 months | 36 months | |
| Baseline | .41** | .37** | .31** | .27** | .20** |
| 6 Months | .59** | .52** | .41** | .39** | |
| 12 Months | .61** | .52** | .45** | ||
| 18 Months | .64** | .50** | |||
| 24 Months | .61** | ||||
Note: A total 15 linear regression models were used to assess the association between levels of self-efficacy assessed at an earlier time with its levels at a later time from 6 months up to 36 months. Missing data due to attrition were imputed using the MCMC method (see text for details);
p<0.05 and
p<0.01
The PROC MI from the software SAS (SAS Institute Inc, Cary, NC) was used to impute missing data. The software Mplus (Muthen and Muthen, Los Angeles, CA) was used to conduct all the modeling analyses.
Results
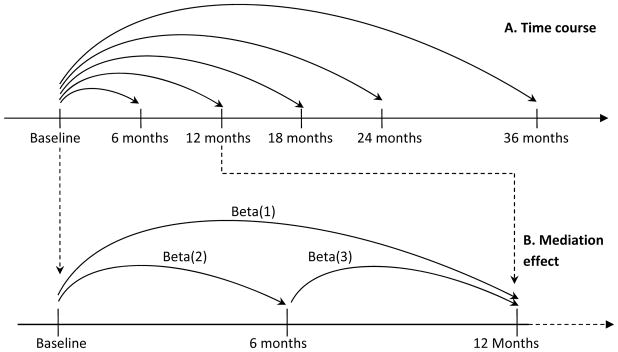
The level and time trend of condom-use self-efficacy are presented in Figure 2. Average self-efficacy scores increased over time from 2.37 (SD = 1.19) at baseline when the average student age was 10 years to 3.50 (SD = 1.02) at 36 months when the average student age was 13 years.
Figure 2.
Developmental trajectories of condom-use self-efficacy beliefs in Bahamian adolescents. Plotted using means and standard errors of condom-use self-efficacy
Results in the first row of Table 1 indicate that baseline condom-use self-efficacy significantly predicted its levels assessed at the five follow-ups from 6 months (b = 0.41, p < 0.01) up to 36 months (b = 0.20, p < 0.01). Data in the table also show that self-efficacy assessed at other times after the baseline significantly predicted its values at subsequent times. For example, self-efficacy assessed at 24 months significantly predicted its value at 36 months (b = 0.61, p < 0.01).
Table 2 contains the results from five path models for condom-use self-efficacy assessed at baseline and subsequent times in predicting its levels across different periods starting at 6 months, and with the inclusion of all mediation paths for assessing the corresponding indirect effects. The R2 for each of the five path models was statistically significant, indicating a good fit of the corresponding models to data. As shown in the table, models 1–5 accounted for 20–47% of the total variance in explaining condom-use self-efficacy. The total effects from baseline to the five corresponding follow-up periods (first row in Table 2) were total effect, and they are identical to those in the first row in Table 1, indicating the effect of baseline self-efficacy on the subsequent assessment of the self-efficacy assessed at the 6-month, 12-month, 18-month, 24-month and 36-month follow-ups respectively. The direct effects from each of the five models were decomposed from these total effects. Results from the first four path models indicate that after adjusting the mediation effects from all mediation paths (Figure 1), self-efficacy assessed at an earlier time was positively associated with its level assessed at subsequent times up to 12 months. For example, results from Model 2 indicate that baseline self-efficacy directly predicted its levels at 12 months (b = 0.16, p < 0.01) after the effect mediated by self-efficacy at 6 months was controlled; likewise, results from Model 3 indicate that self-efficacy at 6 months significantly predicted its level at 18 months (b = 0.22, p < 0.01), allowing for the direct effect of self-efficacy at the baseline and 12 months, and the mediation effect at 12 months.
Table 2.
Results (Regression Coefficients) from Path Models using Baseline Self-Efficacy Predicting its Levels at Subsequent Times
| Predictor variable | Model 1 (6 months) | Model 2 (12 months) | Model 3 (18 months) | Model 4 (24 months) | Model 5 (36 months) |
|---|---|---|---|---|---|
| Total effect | .41** | .37** | .31** | .28** | .20** |
| Direct effect | |||||
| Self efficacy at baseline | a.41** | .16** | .04 | .04 | -.03 |
| Self efficacy at 6 months | .51** | .22** | .03 | .09 | |
| Self efficacy at 12 months | .47** | .21** | .11** | ||
| Self efficacy at 18 months | .48** | .12** | |||
| Self efficacy at 24 months | .44** | ||||
| Model fit | |||||
| R2 | 0.20** | 0.33** | 0.43** | 0.47** | 0.47** |
Note: The five path models were specified using the pattern described in Figure 1. Path Model 1: Self-Efficacy (6months) = Self-efficacy (baseline); Path Model 2: Self-efficacy (12 months) = Self-efficacy (baseline + 6 months); … Path Model 5: Self-efficacy (36 months) = Self-efficacy (Baseline + 6 months + 12 months + 18 months + 24 months). Path models were assessed using Mplus and missing data were imputed using MCMC method (see text for detail). Total effect represents the effect of baseline self-efficacy on the dependent variable without considering the effect from any subsequent assessments, including mediation effects from these assessments; the direct represents the effect of the baseline self-efficacy on its levels at subsequent assessments after considering the effect of all potential mediation steps located between any two assessments.
p<0.05,
p<0.01
In model 1, the total effect is the same as the direct because this is no mediation step.
Results from Model 5 indicate that although baseline self-efficacy no longer directly predicted its level at 36 months significantly (b = −0.03, p > 0.05), self-efficacy assessed at 12 months (when the students advanced from grade six to grade seven) and again at two subsequent periods (18 and 24 months) directly predicted its level at 36 months (when these students advanced to grade nine).
Data in Table 3 summarize the indirect effect of the individual paths for Models 2 through 5 as presented in Table 2. Results in the table indicate that all indirect paths were statistically significant except the ones that contained a path across periods longer than 12 months. For example, the indirect effect for the path “baseline (0) → 6 months → 24 months” and the path “baseline 0 → 18 months → 24 months” were not significant because both contained a period that exceeds 12 months (e.g., 6 months → 24 months and 0 → 18 months).
Discussion and Conclusions
In this study, we examined the developmental process of condom-use self-efficacy among a sample of 497 preadolescents. Longitudinal data were analyzed employing a unique approach of mediation analysis. First, even among a preadolescent sample, findings of this study confirmed results reported in previous studies that the level of condom-use self-efficacy increases with age (Chen, et al., 2009; Chen, et al., 2010; Deveaux, et al., 2007; Foster, 1999; Gong, et al., 2009; St. Lawrence, et al., 1995). Findings from the mediation analysis support our hypothesis that levels of condom-use self-efficacy at an earlier time (age) are positively associated with its levels at subsequent times (ages). Condom-use self-efficacy assessed at an earlier time consistently and positively predicted its level at subsequent times through longitudinal regression modeling analysis. When the mediation effect between two time points is considered, this positive effect of self-efficacy for students in grade six can extend up to 12 months (results from the path Models 1 through 3); if the self-efficacy in grade seven is taken as the “baseline” this effect can extend to 18 months (results from Model 5).
Although it has been documented previously that condom-use self-efficacy may increase with age among adolescents (Chen, et al., 2009; Chen, et al., 2010; Deveaux, et al., 2007; Foster, 1999; Gong, et al., 2009; St. Lawrence, et al., 1995), we believe that this is the first study to document that the development of condom-use self-efficacy in young adolescents is (1) affected directly by its early levels and (2) mediated (or indirectly effected) by its levels during the period in-between. The findings of our analysis indicate that the models we proposed can explain 20–50% of the variance of self-efficacy during a period ranging from 6 months up to 36 months. Additional studies are indicated to examine factors related to this self-reinforcing process such as knowledge, past condom-use experiences, and/or peer influences.
Findings of this study have implications for educational behavior interventions to prevent HIV in which condom-use self-efficacy plays a central role. First, since the level of self-efficacy at an early time is positively associated with its levels at later times, efforts should be directed toward the enhancement of condom-use self-efficacy early in the roll-out of the intervention. In view of our study findings and given the association between condom-use self-efficacy and actual condom-use (Chen, et al., 2009; Deveaux, et al., 2007; Gong, et al., 2009), it is reasonable to hypothesize that higher condom-use self-efficacy immediately post intervention will result in enhanced subsequent self-efficacy development, and higher likelihood of condom-use.
Second, findings from this study also imply the importance of using well-timed boosters to sustain program effect. Data from our analyses indicate that the effect from prior levels of condom-use self-efficacy on subsequent levels decays over time. The direct effect from prior levels appears to extend only through 12 months for adolescents in grade six and through 18 months for adolescents in grade seven. Consequently, boosters with appropriate timing may be important to sustain the self-reinforcing effect of prior condom-use self-efficacy to achieve an ongoing program effect throughout adolescence. Findings from this study suggest that to obtain such sustained effect on condom-use self-efficacy, boosters should be introduced no later than 12 months post intervention when targeting adolescents in grade six. It may be possible to extend this booster interval to 18 months if adolescents in grade seven or later are targeted.
Finally, the observation that the level of condom-use self-efficacy increases over time also has implications for program effect evaluation. Given this information, a pre- post-test design (even with multiple assessments) would not be adequate to assess intervention effect if no control group is included; a randomized controlled trial would be necessary to account for the increase over time.
Limitations
Data used for this analysis were obtained from Bahamian adolescents; caution is needed when generalizing the findings to other populations. Imputed data were employed in the analyses to more effectively use the data collected among all participants, including those who were lost to follow-up. Although the follow-up rates were quite high (over 80% at all periods across the 36-month study period), and our analysis indicated that such attrition was independent from the level of self-efficacy, bias cannot be fully ruled out without complete data. Therefore, caution is needed when the results with imputed data are used. In addition, the relatively small sample size prevented us from conducting the analysis by gender. Further research is needed to demonstrate if the same mediation mechanism is operative for both males and females. Finally, we did not control for the possible clustering effect from the school/class sampling design in the path modeling analysis due to the limited number of schools (only five schools). The path model analysis using the software Mplus requires that the total number of clusters (or in the present analyses, schools) of the sample to be greater than the number of parameters to be estimated for a path model. Our study contains only five schools and thus the sample size is inadequate to control for clustering.
Despite these limitations, in this study we have documented the developmental course of condom-use self-efficacy among a young adolescent sample and demonstrated the importance of prior levels of condom-use self-efficacy on the subsequent development of self-efficacy. The findings of this study provide new data to enhance our understanding of condom-use self-efficacy in particular. Findings from this study also provide evidence useful in the construction of HIV prevention programs targeting adolescents in grade 6 with the expectation of sustaining intervention effects potentially through middle school, especially if boosters are provided periodically after a primary intervention to enhance the mediation effect.
Acknowledgments
Funding Support
This work was supported by the National Institute/National of Mental Health [R01MH069229].
The Bahamas National Trust provided support for training teachers in the Wondrous Wetlands Program and provision of materials for the content of the program. We also thank Glenda Rolle, Director, Health and Family Life Education Unit, Ministry of Education for her tireless support of this research.
Contributor Information
Xinguang Chen, Wayne State University, The Carmen and Ann Adams Department of Pediatrics, Detroit 48201, USA.
Veronica Dinaj-Koci, Wayne State University, Department of Psychology, Detroit 48202, USA.
Nanika Brathwaite, The Bahamas Ministries of Health and Education, Nassau, The Bahamas.
Leslie Cottrell, West Virginia University, Department of Pediatrics, Morganton 26506, USA.
Lynette Deveaux, The Bahamas Ministries of Health and Education, Nassau, The Bahamas.
Perry Gomez, The Bahamas Ministries of Health and Education, Nassau, The Bahamas.
Carole Harris, West Virginia University, Health Research Center, Morgantown 26506, USA.
Xiaoming Li, Wayne State University, The Carmen and Ann Adams Department of Pediatrics, Detroit 48201, USA.
Sonja Lunn, The Bahamas Ministries of Health and Education, Nassau, The Bahamas.
Sharon Marshall, Wayne State University, The Carmen and Ann Adams Department of Pediatrics, Detroit 48201, USA.
Bonita Stanton, Wayne State University, The Carmen and Ann Adams Department of Pediatrics, Detroit 48201, USA.
References
- Adih WK, Alexander CS. Determinants of condom use to prevent HIV infection among youth in Ghana. Journal of Adolescent Health. 1999;24(1):63–72. doi: 10.1016/s1054-139x(98)00062-7. [DOI] [PubMed] [Google Scholar]
- Auerbach JD, Hayes RJ, Kandathil SM. Overview of effective and promisisng interventions to prevent HIV infection. In: Ross D, Dick B, Ferguson J, editors. Preventing HIV/AIDS in young people: A systematic review of the evidence from developing countries World Health Organization techinal report series. Geneva: World Health Organization; 2006. pp. 43–78. [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W.H. Freeman; 1997. [Google Scholar]
- Bandura A, Barbaranelli C, Caprara GV, Pastorelli C. Multifaceted impact of self-efficacy beliefs on academic functioning. Child Development. 1996;67(3):1206–1222. [PubMed] [Google Scholar]
- Bandura A, Barbaranelli C, Caprara GV, Pastorelli C. Self-efficacy beliefs as shapers of children’s aspirations and career trajectories. Child Development. 2001;72(1):187–206. doi: 10.1111/1467-8624.00273. [DOI] [PubMed] [Google Scholar]
- Bandura A, Cioffi D, Taylor CB, Brouillard ME. Perceived self-efficacy in coping with cognitive stressors and opioid activation. Journal of Personality and Social Psychology. 1988;55(3):479–488. doi: 10.1037//0022-3514.55.3.479. [DOI] [PubMed] [Google Scholar]
- Basen-Engquist K, Parcel GS. Attitudes, norms, and self-efficacy: a model of adolescents’ HIV-related sexual risk behavior. Health Eduationc Quarterly. 1992;19(2):263–277. doi: 10.1177/109019819201900209. [DOI] [PubMed] [Google Scholar]
- Beyrer C. HIV epidemiology update and transmission factors: Risks and risk contexts - 16th International AIDS Conference Epidemiology Plenary. Clinical Infectious Diseases. 2007;44(7):981–987. doi: 10.1086/512371. [DOI] [PubMed] [Google Scholar]
- Caceres CF, Rosasco AM, Mandel JS, Hearst N. Evaluating a school-based intervention for STD/AIDS prevention in Peru. Journal of Adolescent Health. 1994;15(7):582–591. doi: 10.1016/1054-139x(94)90143-q. [DOI] [PubMed] [Google Scholar]
- Chen X, Lunn S, Deveaux L, Li X, Brathwaite N, Cottrell L, Stanton B. A cluster randomized controlled trial of an adolescent HIV prevention program among Bahamian youth: Effect at 12 months post-intervention. AIDS and Behavior. 2009;13(3):499–508. doi: 10.1007/s10461-008-9511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Stanton B, Gomez P, Lunn S, Deveaux L, Brathwaite N, Harris C. Effects on condom use of an HIV prevention programme 36 months postintervention: A cluster randomized controlled trial among Bahamian youth. International Journal of STD & AIDS. 2010;21(9):622–630. doi: 10.1258/ijsa.2010.010039. 21/9/622 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates TJ, Richter L, Caceres C. HIV prevention 3 - Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372(9639):669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbes LA, Kennedy GE, Peersman G, Zohrabyan G. System review of HIV behavioral prevention research in African Americans. HIV InSite Knowledge Base Chapter. HIV InSite. 2002 Retrieved from www.hivinsite.org.
- Deveaux L, Stanton B, Lunn S, Cottrell L, Yu SL, Brathwaite N, Harris C. Reduction in human immunodeficiency virus risk among youth in developing countries. Archives of Pediatrics & Adolescent Medicine. 2007;161(12):1130–1139. doi: 10.1001/archpedi.161.12.1130. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventive interventions for adolescents: Sustaining effects using an ecological approach. Journal of Pediatric Psychology. 2007;32(8):888–906. doi: 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- DiIorio C, Dudley WN, Kelly M, Soet JE, Mbwara J, Sharpe Potter J. Social cognitive correlates of sexual experience and condom use among 13- through 15-year-old adolescents. Journal of Adolescent Health. 2001;29(3):208–216. doi: 10.1016/s1054-139x(00)00200-7. S1054-139X(00)00200-7 [pii] [DOI] [PubMed] [Google Scholar]
- Foster EV. Doctoral dissertation. 1999. Social skills training in relation to safer sex behaviors among Mexican-American and European-American adolescents. Retrieved from Proquest Dissertations and Theses (Order number 9905861) [Google Scholar]
- Gong J, Stanton B, Lunn S, Deveaux L, Li XM, Marshall S, Chen XG. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123(5):E917–E928. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holschneider SOM, Alexander CS. Social and psychological influences on HIV preventive behaviors of youth in Haiti. Journal of Adolescent Health. 2003;33(1):31–40. doi: 10.1016/s1054-139x(02)00418-4. [DOI] [PubMed] [Google Scholar]
- Joffe A, Radius SM. Self-efficacy and intent to use condoms among entering college freshmen. Journal of Adolescent Health. 1993;14(4):262–268. doi: 10.1016/1054-139x(93)90172-l. [DOI] [PubMed] [Google Scholar]
- Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LAJ. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985–2000 - A research synthesis. Archives of Pediatrics & Adolescent Medicine. 2003;157(4):381–388. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- Johnston-Briggs BD, Liu JX, Carter-Pokras O, Barnet B. Effect of partner relationship on motivation to use condoms among adolescent mothers. Journal of the National Medical Association. 2008;100(8):929–935. doi: 10.1016/s0027-9684(15)31407-3. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Stein JA, Malow R, Averhart C, Devieux J, Jennings T, Feaster DJ. Predicting protected sexual behaviour using the Information-Motivation-Behaviour skills model among adolescent substance abusers in court-ordered treatment. Psychology Health Medicine. 2002;7(3):327–338. doi: 10.1080/13548500220139368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaljee LM, Genberg B, Riel R, Cole M, Tho LH, Thoa LTK, Minh TT. Effectiveness of a theory-based risk reduction HIV prevention program for rural Vietnamese adolescents. AIDS Education and Prevention. 2005;17(3):185–199. doi: 10.1521/aeap.17.4.185.66534. [DOI] [PubMed] [Google Scholar]
- Kirby D. Effective approaches to reducing adolescent unprotected sex, pregnancy, and childbearing. Journal of Sex Research. 2002;39(1):51–57. doi: 10.1080/00224490209552120. [DOI] [PubMed] [Google Scholar]
- Kirby D. Research finings on programs to reduce teen pregnancy and sexually transmitted diseases. Paper presented at the National Campaign to Prevent Teen and Unplanned Pregnancy.2007. [Google Scholar]
- Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. Journal of Adolescent Health. 2007;40(3):206–217. doi: 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- Kyrychenko P, Kohler C, Sathiakumar N. Evaluation of a school-based HIV/AIDS educational intervention in Ukraine. Journal of Adolescent Health. 2006;39(6):900–907. doi: 10.1016/j.jadohealth.2006.06.006. [DOI] [PubMed] [Google Scholar]
- Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, Kim AS, Team HAPRS. Best-evidence interventions: Findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. American Journal of Public Health. 2007;97(1):133–143. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monasch R, Mahy M. Young people: the centre of the HIV epidemic. In: Ross D, Dick B, Ferguson J, editors. Preventing HIV/AIDS World Health Organization Technical Report Series. Geneva: World Health Organization; 2006. pp. 15–41. [PubMed] [Google Scholar]
- Mullen PD, Ramirez G, Strouse D, Hedges LV, Sogolow E. Meta-analysis of the effects of behavioral HIV prevention interventions on the sexual risk behavior of sexually experienced adolescents in controlled studies in the United States. Journal of Acquired Immune Deficiency Syndromes. 2002;30:S94–S105. [PubMed] [Google Scholar]
- O’Leary A, Jemmott LS, Jemmott JB. Mediation analysis of an effective sexual risk-reduction intervention for women: the importance of self-efficacy. Health Psychology. 2008;27(2):180–184. doi: 10.1037/0278-6133.27.2(Suppl).S180. 2008-03488-011 [pii] [DOI] [PubMed] [Google Scholar]
- Ormrod JE. Educational psychology: Developing learners. 3. Upper Saddle River, NJ: Merrill; 2000. [Google Scholar]
- Pedlow CT, Carey MP. HIV sexual risk-reduction interventions for youth: A review and methodological critique of randomized controlled trials. Behavior Modification. 2003;27(2):135–190. doi: 10.1177/0145445503251562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard R, van der Pligt J. Factors affecting condom use among adolescents. Journal of Community & Applied Social Psychology. 1991;1(2):105–116. [Google Scholar]
- Robin L, Dittus P, Whitaker D, Crosby R, Ethier K, Mezoff J, Pappas-Deluca K. Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: A decade in review. Journal of Adolescent Health. 2004;34(1):3–26. doi: 10.1016/s1054-139x(03)00244-1. [DOI] [PubMed] [Google Scholar]
- Ruiz MS, Gable AR, Kaplan EH, Stoto MA, Fineberg HV, Trussel J, editors. Report Brief No Time to Lose: Getting the most from HIV Prevention. Washington, DC: National Academy Press; 2000. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. London ; New York, NY: Chapman & Hall; 1997. [Google Scholar]
- Schunk DH. Goal-setting and self-efficacy during self-regulated learning. Educational Psychologist. 1990;25(1):71–86. [Google Scholar]
- Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology-an International Review-Psychologie Appliquee-Revue Internationale. 2008;57(1):1–29. [Google Scholar]
- St Lawrence JS, Brasfield TL, Jefferson KW, Alleyne E, Obannon RE, Shirley A. Cognitive-behavioral intervention to reduce African-American adolescents risk for HIV-infection. Journal of Consulting and Clinical Psychology. 1995;63(2):221–237. doi: 10.1037//0022-006x.63.2.221. [DOI] [PubMed] [Google Scholar]
- Stanton B, Cole M, Galbraith J, Li XM, Pendleton S, Cottrel L, Kaljee L. Randomized trial of a parent intervention: Parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics & Adolescent Medicine. 2004;158(10):947–955. doi: 10.1001/archpedi.158.10.947. [DOI] [PubMed] [Google Scholar]
- Stanton B, Li XM, Kahihuata J, Fitzgerald AM, Neumbo S, Kanduuombe G, Zimba RF. Increased protected sex and abstinence among Namibian youth following a HIV risk-reduction intervention: a randomized, longitudinal study. AIDS. 1998;12(18):2473–2480. doi: 10.1097/00002030-199818000-00017. [DOI] [PubMed] [Google Scholar]
- Stephenson J, Obasi A. HIV risk-reduction in adolescents. Lancet. 2004;363(9416):1177–1178. doi: 10.1016/S0140-6736(04)15983-7. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Pearson/Allyn & Bacon; 2007. [Google Scholar]
- Uniting the World Against AIDS [UNAIDS] Bahamas. n.d Retrieved from http://www.unaids.org/en/CountryResponses/Countries/bahamas.asp.
- Wang RH, Cheng CP, Chou FH. Predictors of sexual abstinence behaviour in Taiwanese adolescents: A longitudinal application of the transtheoretical model. Journal of Clinical Nursing. 2009;18(7):1010–1017. doi: 10.1111/j.1365-2702.2008.02509.x. [DOI] [PubMed] [Google Scholar]