Abstract
Objective
To examine the relationship between sleep disordered breathing (SDB) and adverse pregnancy outcomes in a high-risk cohort
Study Design
This was a planned analysis of a prospective cohort designed to estimate the prevalence and trends of SDB in a high-risk pregnant women. We recruited women with a BMI ≥ 30 kg/m2, chronic hypertension, pre-gestational diabetes, prior preeclampsia, and/or a twin gestation. Objective assessment of SDB was completed between 6–20 weeks and again in the third trimester. SDB was defined as an apnea hypopnea index ≥5, and further grouped into severity categories: mild SDB (5–14.9), moderate SDB (15–29.9) and severe SDB (≥30). Pregnancy outcomes (preeclampsia, gestational diabetes, preterm birth, infant weight) were abstracted by physicians blinded to the SDB results.
Results
Of the 188 women with a valid early pregnancy sleep study, 182 had complete delivery records. There was no relationship demonstrated between SDB exposure in early or late pregnancy and preeclampsia, preterm birth < 34 weeks, and small for gestational age (<5%) or large for gestational age (>95%) neonates. Conversely, SDB severity in early pregnancy was associated with the risk of developing gestational diabetes (no SDB 25%, mild SDB 43%, moderate/severe SDB 63%, p=.03). The adjusted OR for developing gestational diabetes for moderate/severe SDB was 3.6 (0.6, 21.8).
Conclusions
This study suggests a dose-dependent relationship between SDB in early pregnancy and the subsequent development of gestational diabetes. In contrast, no relationships between SDB during pregnancy and preeclampsia, preterm birth, and extremes of birthweight were demonstrated.
Keywords: sleep disordered breathing, sleep apnea, pregnancy, gestational diabetes, adverse pregnancy outcomes
Introduction
Sleep disordered breathing (SDB) refers to a group of disorders characterized by abnormal respiratory patterns (e.g., apneas, hypopneas) or abnormal gas exchange (e.g., hypoxia) during sleep.1,2 Obstructive sleep apnea (OSA), the most common type of SDB, is characterized by airway narrowing during sleep that leads to respiratory disruption, hypoxia, and sleep fragmentation.
Pregnancy has been associated with several alterations in sleep and a high frequency of sleep disturbances.3 Many studies have demonstrated that SDB symptoms (snoring, excessive daytime sleepiness) are common in pregnancy and that the prevalence of SDB symptoms increases as pregnancy progresses.3–6 This progression is at least partly related to the weight gain, edema and hyperemia of pregnancy that lead to upper airway narrowing and increased airway resistance.
In non-pregnant populations, SDB has been linked not only to poor sleep and impaired daytime function, but also to adverse health outcomes, such as cardiovascular and metabolic disease.7–13 Recent data also have suggested a potential link between SDB and adverse pregnancy outcomes such as hypertensive disorders of pregnancy, gestational diabetes and preterm birth.14–20 In a retrospective study, Chen at al15 reported that SDB was associated with an increased risk of preeclampsia (aOR 1.6, 95% CI 2.16, 11.26), gestational diabetes (aOR 1.63, 95% CI 1.07, 2.48) and preterm birth (aOR 2.31, 95% CI 1.77, 3.01). Such data underscore the potential association between SDB and adverse pregnancy outcomes, and the importance of gaining a better understanding of this link. However, most of the research regarding the epidemiology of SDB in pregnancy is retrospective or cross-sectional, and the majority of studies have relied on self-reported symptom assessments. The objective of this study was to examine the relationship between objectively-assessed SDB during pregnancy and the risk of adverse pregnancy outcomes.
Methods
This was a planned secondary analysis of a study that was designed to evaluate the prevalence of and trends in SDB across pregnancy among women at high risk for developing preeclampsia.21,22 We recruited women with pre-pregnancy BMI ≥ 30 kg/m2, chronic hypertension, pregestational diabetes (type 1 or type 2), prior history of preeclampsia, and/or a twin gestation. The study subjects were recruited as a convenience sample from ambulatory care practices at two University centers serving women with both private and public insurance.
After signing informed consent, women completed an at-home, overnight sleep evaluation with the Watch-PAT100 (Itamar medical Ltd., Israel) during early pregnancy (between 6–20 weeks of gestation) and were asked to repeat the study in late pregnancy (between 28–37 weeks of gestation). The Watch-PAT 100, which has a peripheral arterial tonometry (PAT) finger plethysmograph and standard oxygen saturation (SpO2) probe, allows the recording of the PAT signal, heart rate, and oxyhemoglobin saturation. Sleep time is estimated using an inbuilt actigraph.23 Analysis of these signals allows for the determination of an apnea hypopnea index (AHI) which is a sum of the number of apneas (breathing pauses) and hypopneas (shallow breathing) that occur per hour of sleep. In adults an AHI of 0–4.9 is considered normal and an AHI ≥ 5 defines SDB. An AHI of 5–14.9 is typically considered mild SDB, 15–29.9 moderate SDB, and ≥30 severe SDB.1,2,24,25
The Watch-PAT proprietary software algorithm was used to analyze the PAT signal amplitude along with the heart rate and SpO2 to estimate the AHI. An AHI event was scored if either a PAT amplitude reduction occurred with ≥ 3% oxyhemoglobin desaturation or ≥ 4% oxyhemoglobin desaturation occurred.26 Studies in non-pregnant populations have shown that respiratory indices, such as the AHI, derived from the Watch-PAT are strongly correlated (r=0.90) with those obtained from in-laboratory polysomnography (PSG), and also have demonstrated that the Watch-PAT is an accurate and reliable ambulatory method for the detection of SDB.23,26–28. O’Brien et al recently presented data comparing the Watch-PAT to full PSG in third trimester pregnant subjects. Their results indicate that among pregnant women, the Watch-PAT AHI correlated very well with PSG AHI(r=0.76, p<.0001) and that the Watch-PAT demonstrated excellent sensitivity (88%) and specificity (86%) for identification of SDB in pregnancy.29
All participants received obstetrical care by their physicians who were unaware of the sleep study results. However, women were informed if their AHI was ≥ 10 and given contact information for sleep specialists in the area if they were interested in further evaluation. Given that there are currently no sanctioned pregnancy-specific guidelines for SDB treatment or evidence that treatment in the short term impacts maternal, obstetric or neonatal outcomes, no alteration of care was recommended or mandated for study participants, regardless of AHI.
Pregnancy outcomes were abstracted from the medical record by physicians unaware of the SDB status of the study subjects. Outcomes of interest included preeclampsia, gestational diabetes, preterm birth (<34 weeks gestation) and birth weight. Preeclampsia was divided into the following categories in concordance with ACOG guidelines:1) mild preeclampsia: new-onset systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg on two occasions 6 hours apart on or after 20 weeks 0/7 days of gestation and within 72 hours of a diagnosis of proteinuria (≥300 mg in a 24-hour urine collection, a spot protein creatinine (PC) ratio of 0.2, or the finding of ≥ 2+ on dipstick if a 24-hour urine or PC ratio was not available);30,31 2) severe preeclampsia: criteria for mild preeclampsia are met plus one or more of the following: blood pressure of 160 mmHg systolic or higher or 110 mmHg diastolic or higher on two occasions at least 6 hours apart, proteinuria ≥5 g, cerebral or visual disturbances, pulmonary edema or cyanosis, epigastric or right upper-quadrant pain, impaired liver function, thrombocytopenia, and/or fetal growth restriction; 3) superimposed preeclampsia: in a woman with hypertension before 20 weeks of gestation, a sudden increase in proteinuria if already present in early gestation, a sudden increase in hypertension, or the development of HELLP syndrome. All diagnoses of preeclampsia were confirmed by a second physician.27,28 Gestational diabetes was diagnosed according to glucose tolerance test standards (either a 100 gram, 3-hour glucose tolerance test or a 75 gram, 2 hour glucose tolerance test). Women with pregestational diabetes were excluded from the gestational diabetes analyses.
Associations were explored between SDB presence/severity and our outcomes of interest through the use of the χ2, Fischer exact, and χ2 test for trend for categorical variables. Multivariable logistic regression was used to adjust for potential confounders. All tests were two-tailed and a P < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS 19.0 statistical software (SPSS Inc., Chicago, IL).
For the primary study, designed to detected changes in SDB across pregnancy, we established that that a sample size of 180 women would be required to complete the baseline study.22 We enrolled 233 women, 182 had valid sleep study data and delivered at the study sites. The incidence of early pregnancy SDB in this high-risk population was 30%. Assuming a 15% risk of preeclampsia in our non-SDB subjects and an α of 0.05, we had 80% power to detect an increase to 34% (crude odds ratio 2.9) among women with SDB. This magnitude of association is consistent with that which has been observed between SDB and cardiovascular and metabolic diseases in non-pregnant individuals.10,32 This study was approved by the Institutional Review Board of Northwestern University and NorthShore University HealthSystem.
Results
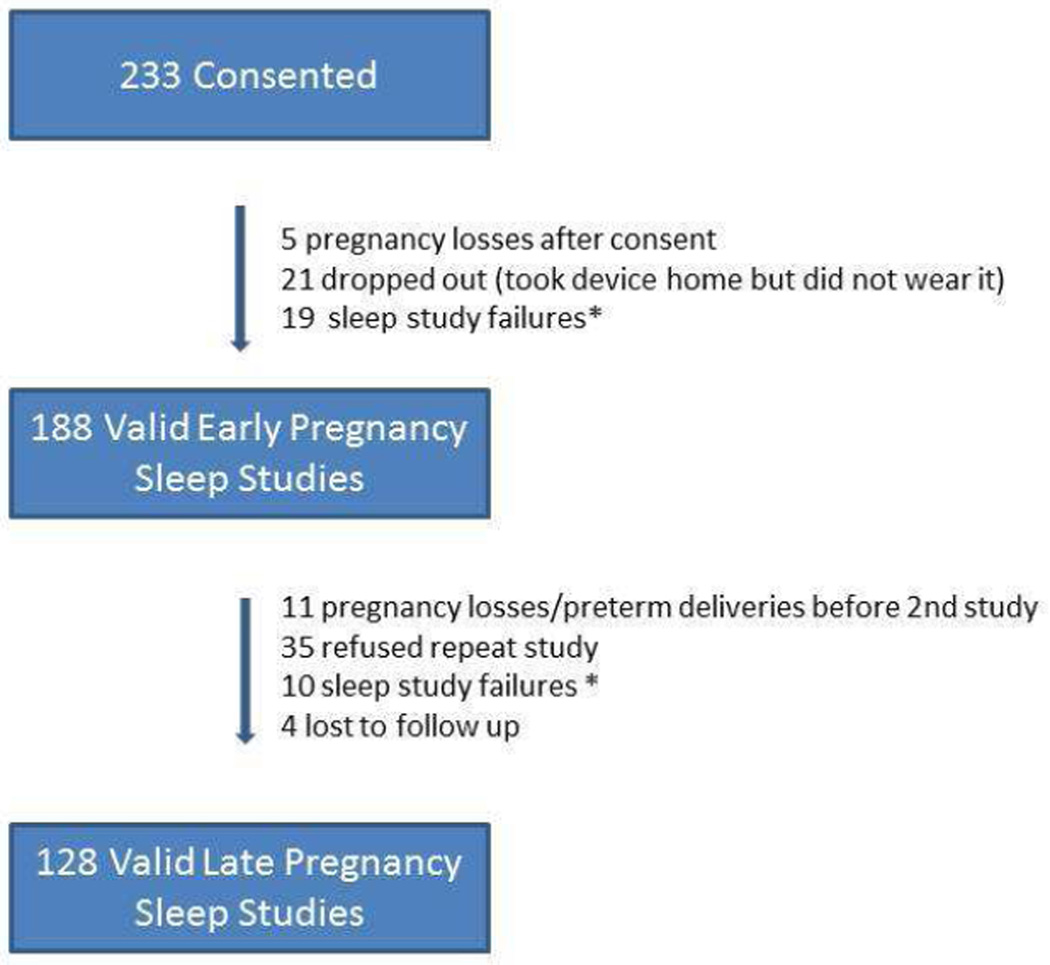
Two hundred and thirty-three women consented to participate in the primary study. One hundred and eighty-eight and 128 of these women had a valid early and late pregnancy sleep study respectively. The reasons for incomplete sleep data are presented in Figure 1. The mean gestational age (± standard deviation) was 16.7 ± 3.5 and 32.6 ± 2.4 weeks at the first and second sleep study, respectively. Demographic characteristics of the study population are provided in Table 1. Sixty-two percent of subjects were obese, 30% had chronic hypertension, 57% had pregestational diabetes, 15% had prior preeclampsia, and 6% had a twin gestation. Fifty-four percent of women had more than one qualifying risk factor. In early pregnancy 21%, 6% and 3% of women had mild, moderate or severe SDB, respectively. These frequencies increased to 35%, 7% and 5 % in the third trimester. Twenty-seven percent of participants (n=34) experienced a worsening of SDB during pregnancy; 26 were cases of new-onset SDB, while the other 8 had SDB in early pregnancy that worsened in severity.22 Because of the small number of cases of moderate and severe SDB, we combined these two groups for further analysis. Pregnancy outcomes were available for 182 of the 188 women with a valid early pregnancy sleep study. Two women had first trimester miscarriages, and 4 women were lost to follow-up.
Figure 1.
Study recruitment
* 24% of study failures were due to participant errors/non-compliance
Table 1.
Characteristics of study participants
| Entire cohort (N=188) |
Participants with an AHI ≤ 5 in early pregnancy (N=132) |
Participants with an AHI ≥ 5 in early pregnancy (N=56) |
P value | |
|---|---|---|---|---|
| Age (years) | 33.0 ± 5.9 | 32.4 ± 6.1 | 34.4 ± 5.2 | .04 |
| Ethno-racial status | ||||
| White | 39.2% | 40.2% | 37.5% | .8 |
| Black | 25.5% | 26.5% | 23.2% | |
| Hispanic | 20.2% | 18.2% | 25.0% | |
| Other | 14.9% | 15.1% | 14.3% | |
| Pre-pregnancy BMI (kg/m2) | 32.8 ± 8.7 | 30.8 ± 8.2 | 37.2 ±8.3 | <.001 |
| Maternal history | ||||
| Chronic hypertension | 29.8% | 23.5% | 44.6% | .004 |
| Pre-gestational diabetes | 57.4% | 62.1% | 46.4% | .05 |
| Twins | 5.9% | 7.6% | 1.8% | .2 |
| Nulliparous | 29.3% | 28.8% | 30.4% | .8 |
| Prior preeclampsia | 16.5% | 14.4% | 21.4% | .2 |
The rates of adverse pregnancy outcomes stratified by SDB status are presented in tables 2 and 3. Preeclampsia occurred in 17.6% of women (14 cases of mild preeclampsia, 6 cases of severe preeclampsia and 12 cases of superimposed preeclampsia). There was no relationship demonstrated between SDB in early or late pregnancy and preeclampsia. The rate of preterm birth < 34 weeks was 9%, of which half were iatrogenic. There was no relationship demonstrated between SDB exposure in early or late pregnancy and either preterm birth < 34 weeks or iatrogenic preterm birth < 34 weeks. Similarly, there was no association between SDB and extremes of birthweight (<5% or >95% for gestational age).33
Table 2.
SDB in Early Pregnancy and Adverse Pregnancy Outcomes
| No SDB | Mild SDB (AHI 5–14.9) |
Moderate/Severe SDB (AHI ≥15) |
P value* | |
|---|---|---|---|---|
| Any Preeclampsia | 24/127 (18.9) | 5/40 (12.5) | 3/15(20) | .7 |
| Preeclampsia among women without CHTN | 17/99 (17.2) | 1/23(4.3) | 2/8(25) | .7 |
| Superimposed preeclampsia among women with CHTN | 7/28 (25) | 4/17(23.5) | 1/7(14.3) | .6 |
| Gestational diabetes | 13/49 (26.5) | 9/21 (42.9) | 5/8(62.5) | .03 |
| Preterm birth < 34 weeks | 12/127 (9.4) | 3/40 (7.5) | 2/15(13.3) | .8 |
| Iatrogenic preterm birth < 34 weeks | 6/127 (4.7) | 2/40(5) | 1/15 (6.7) | .7 |
| Birth weight* | ||||
| <5% | 1/125 (0.8) | 1/40 (2.5) | 0/15 (0) | .8 |
| >95% | 27/125(21.6) | 7/40 (17.5) | 1/15 (6.7) | .2 |
chi-square for trend
CHTN=chronic hypertension
Data are n/N(%)
Birth weight was not available for 2 subjects
Table 3.
SDB in Late Pregnancy and Adverse Pregnancy Outcomes
| No SDB | Mild SDB AHI 5–14.9 |
Moderate/Severe SDB AHI ≥15 |
P value* |
|
|---|---|---|---|---|
| Any Preeclampsia | 13/67 (19.4) | 4/45 (8.9) | 2/16 (12.5) | .2 |
| Preeclampsia among women without CHTN | 10/50 (20) | 3/33 (9.1) | 1/7 (14.3) | .3 |
| Superimposed preeclampsia among women with CHTN | 3/17 (17.6) | 1/12 (8.3) | 1/9 (11.1) | .6 |
| Gestational diabetes | 4/25 (16) | 5/14 (35.7) | 5/11 (45.5) | .05 |
| Preterm birth < 34 weeks | 5/67 (7.5) | 1/45 (2.2) | 0/16 (0) | .1 |
| Iatrogenic preterm birth < 34 weeks | 4/67 (6) | 1/45 (2.2) | 0/16 (0) | .2 |
| Birth weight | ||||
| <5% | 1/67 (1.5) | 0/44 (0) | 0/16 (0) | .4 |
| >95% | 13/67 (19.4) | 1/44 (25) | 2/16 (12.5) | .9 |
chi-square for trend
CHTN=chronic hypertension
Data are n/N (%)
In contrast, increasing SDB severity in early pregnancy was associated with an increased risk of developing gestational diabetes (P=.03). This trend also was observed for SDB in late pregnancy, although the difference did not reach statistical significance. The unadjusted odds ratio for developing gestational diabetes was 2.1 (95%CI 0.7, 6.1) for women with mild SDB in early pregnancy and 4.6 (1.0–22.1) for women with moderate/severe SDB. Controlling for age, pre-pregnancy BMI, race/ethnicity, parity, chronic hypertension and twin gestation, the adjusted OR for developing gestational diabetes for mild SDB in early pregnancy was 1.5 (0.4, 6.0), and 3.6 (0.6, 21.8) for moderate/severe SDB. While the adjusted OR estimates derived from this modest sample size did not achieve statistical significance, they demonstrate the potential independent impact of SDB on glucose control during pregnancy.
Conclusions
This study suggests a dose-dependent relationship between SDB exposure in early pregnancy and the subsequent development of gestational diabetes. In contrast, no relationships were demonstrated between SDB during pregnancy and preeclampsia, preterm birth, and extremes of birth weight.
Data from symptom-based studies and retrospective chart reviews have demonstrated a link between SDB and gestational diabetes. In a recent metaanalysis, Pamidi et al demonstrated a pooled, adjusted OR of 1.86 (95% CI 1.30, 2.42) for gestational diabetes when SDB is suspected during pregnancy.34 A second, contemporaneous metaanalysis corroborate this data.35 Our findings confirm this relationship, and in addition demonstrate a dose-response relationship between severity of SDB in early pregnancy and the subsequent development of gestational diabetes.
In contrast to prior reports, our study did not demonstrate a relationship between SDB and preeclampsia. Louis et al recently published a study similar in design and size (N = 175) to this study. They demonstrated that women with SDB (AHI ≥ 5) were more likely to develop preeclampsia (adjusted OR 3.5, 95% CI 1.3, 9.9).18 It is important to note that the Louis et al cohort had a higher mean pre-pregnancy BMI and a higher percentage of Black participants than the population in our study. Subjects in their study also suffered from more severe SDB compared to our cohort (i.e., a median AHI in early pregnancy 12.9 vs. 9.8, respectively). Furthermore, prior studies, may not have adequately distinguished between chronic hypertension and superimposed preeclampsia. Given the association between chronic hypertension and SDB, misclassification of the former as superimposed preeclampsia would bias the results towards a positive association. In the present study, we attempted to lessen the chance of this bias by having any case of preeclampsia confirmed by a second abstractor. While our sample size was modest, we had 80% power to detect an increase to 34% (crude odds ratio of 2.9) in the rate of preeclampsia in subjects with SDB. This magnitude of association is in the range of what has been reported by Pamidi et al in their metaanalysis (crude OR 2.86, 95% CI 2.17, 3.78) and by Louis et al in their cohort study.18,34
Our study had several strengths. We used objective assessments of SDB in pregnancy, and our SDB data were ascertained prior to the adverse pregnancy outcomes. All chart abstraction was conducted by obstetricians who were unaware of the SDB exposure. Moreover, all preeclampsia cases were reviewed by a second abstractor and all gestational diabetes cases were confirmed by review of glucose tolerance testing results.
Our study has several limitations that require consideration as well. First, our study population was a high-risk, heterogeneous cohort and we recognize that the results of our study may not be generalizable to all pregnant women. Healthier women may have greater consequences from SDB exposure; however, their likelihood of having SDB would be significantly less. Secondly, while all chart abstractors were blinded to the SDB exposure, participants with an AHI of ≥ 10 were notified of their sleep study findings (14.9% and 30.5% of participants in early and late pregnancy, respectively). As part of our medical records review, we asked chart abstractors to search the record of all subjects for evidence that a clinical sleep study was performed, that a formal diagnosis of SDB was made or that a subject was on CPAP. To our knowledge, no participant received care for SDB during pregnancy. Lastly, the majority of our SDB cases, as expected in a young female cohort, were mild. Larger sample sizes are needed to more precisely ascertain how more severe SDB may impact pregnancy.
Our study findings underscore the importance of systematically gathering further evidence on the impact of SDB on pregnancy. Studies addressing SDB’s impact on pregnancy are heterogeneous in regards to study design and SDB definition. Furthermore, as we have illustrated, finding in these studies are inconsistent. Consequently, it is premature to suggest that obstetrical care providers should systematically screen for SDB in pregnancy. Such a change in care would require a massive education effort, as most obstetrical providers have not been trained to screen for sleep disorders, and would lead to increased healthcare costs.
Moreover, at this time there is no evidence that treatment of SDB in the short term improves maternal or neonatal outcomes. Continuous positive airway pressure (CPAP) has been used to improve pathophysiologic derangements related to SDB. For example, CPAP improves biomarkers of inflammation and oxidative stress.36–41 It improves nocturnal respiratory indices, and in patients with significant symptoms of SDB, it can improve sleep and daytime function.42 A recent study of middle aged, predominately male adults demonstrated that 3 months of CPAP therapy in individuals with at least moderate SDB was associated with a decrease in blood pressure, lipid levels, glycated hemoglobin levels, BMI and abdominal fat content.40 Yet, in non-pregnant adults, the role of CPAP in reversing or preventing long-term cardiovascular and metabolic morbidity remains unanswered, especially for patients with only mild SDB.43–46 Similarly, the role of CPAP in preventing maternal/fetal morbidity during pregnancy has yet to be determined. Large, prospective cohorts that use objective SDB assessments across pregnancy are needed to accurately define the impact of SDB on pregnancy outcomes. Secondly, clinical trials of CPAP use in pregnancy are needed to determine if short term treatment of SDB in pregnancy can improve maternal and neonatal health.
In summary, our study suggests a relationship between SDB and gestational diabetes, but not with preeclampsia, preterm birth or fetal growth. Future studies are needed to further and precisely determine the implications of SDB on pregnancy, and to evaluate the impact of treatment of this sleep disorder during pregnancy on maternal and perinatal health.
CLINICAL IMPLICATIONS.
Our findings suggest a relationship between sleep-disordered breathing (SDB) and gestational diabetes but not preeclampsia, preterm birth, or fetal growth.
There is clinical equipoise about how SDB affects pregnancy and whether screening for and treating this disorder in pregnancy can improve outcomes.
Studies are needed to determine the implications of SDB on pregnancy and to evaluate the impact of SDB treatment during pregnancy on maternal and perinatal health.
Acknowledgments
Financial Support: NIH/NICHD 1K12HD050121, Preeclampsia Foundation Vision Grant, Northwestern Memorial Foundation Dixon Translational Research Initiative
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE: The authors report no conflict of interest
Meeting presentations:
Presented at the 32nd Annual Meeting for the Society of Maternal-Fetal Medicine, San Francisco, CA; February 2013. Abstract 256.
References
- 1.Hauri P, editor. The International Classification of Sleep Disorders, Diagnostic and Coding Manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 2.Iber C, Ancoli-Israel S, Chesson A, Quan S. The American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Vol. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 3.Pien GW, Schwab RJ. Sleep disorders during pregnancy. Sleep. 2004 Nov 1;27(7):1405–1417. doi: 10.1093/sleep/27.7.1405. [DOI] [PubMed] [Google Scholar]
- 4.Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. Jan;115(1):77–83. doi: 10.1097/AOG.0b013e3181c4f8ec. [DOI] [PubMed] [Google Scholar]
- 5.Sahota PK, Jain SS, Dhand R. Sleep disorders in pregnancy. Curr Opin Pulm Med. 2003 Nov;9(6):477–483. doi: 10.1097/00063198-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Santiago JR, Nolledo MS, Kinzler W, Santiago TV. Sleep and sleep disorders in pregnancy. Ann Intern Med. 2001 Mar 6;134(5):396–408. doi: 10.7326/0003-4819-134-5-200103060-00012. [DOI] [PubMed] [Google Scholar]
- 7.Marshall NS, Wong KK, Phillips CL, Liu PY, Knuiman MW, Grunstein RR. Is sleep apnea an independent risk factor for prevalent and incident diabetes in the Busselton Health Study? J Clin Sleep Med. 2009 Feb 15;5(1):15–20. [PMC free article] [PubMed] [Google Scholar]
- 8.Newman AB, Nieto FJ, Guidry U, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol. 2001 Jul 1;154(1):50–59. doi: 10.1093/aje/154.1.50. [DOI] [PubMed] [Google Scholar]
- 9.Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000 Apr 12;283(14):1829–1836. doi: 10.1001/jama.283.14.1829. [DOI] [PubMed] [Google Scholar]
- 10.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000 May 11;342(19):1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 11.Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005 Dec 15;172(12):1590–1595. doi: 10.1164/rccm.200504-637OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young T, Peppard P. Sleep-disordered breathing and cardiovascular disease: epidemiologic evidence for a relationship. Sleep. 2000 Jun 15;23(Suppl 4):S122–S126. [PubMed] [Google Scholar]
- 13.Young T, Peppard P, Palta M, et al. Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med. 1997 Aug 11–25;157(15):1746–1752. [PubMed] [Google Scholar]
- 14.Bourjeily G, Raker CA, Chalhoub M, Miller MA. Pregnancy and fetal outcomes of symptoms of sleep-disordered breathing. Eur Respir J. 2010 Oct;36(4):849–855. doi: 10.1183/09031936.00021810. [DOI] [PubMed] [Google Scholar]
- 15.Chen YH, Kang JH, Lin CC, Wang IT, Keller JJ, Lin HC. Obstructive sleep apnea and the risk of adverse pregnancy outcomes. Am J Obstet Gynecol. 2011 Sep 16; doi: 10.1016/j.ajog.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Facco FL, Grobman WA, Kramer J, Ho KH, Zee PC. Self-reported short sleep duration and frequent snoring in pregnancy: impact on glucose metabolism. Am J Obstet Gynecol. 2010 May 25; doi: 10.1016/j.ajog.2010.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Facco FL, Liu CS, Cabello AA, Kick A, Grobman WA, Zee PC. Sleep-disordered breathing: a risk factor for adverse pregnancy outcomes? Am J Perinatol. 2012 Apr;29(4):277–282. doi: 10.1055/s-0031-1295658. [DOI] [PubMed] [Google Scholar]
- 18.Louis J, Auckley D, Miladinovic B, et al. Perinatal Outcomes Associated With Obstructive Sleep Apnea in Obese Pregnant Women. Obstet Gynecol. 2012 Nov;120(5):1085–1092. doi: 10.1097/AOG.0b013e31826eb9d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Louis JM, Auckley D, Sokol RJ, Mercer BM. Maternal and neonatal morbidities associated with obstructive sleep apnea complicating pregnancy. Am J Obstet Gynecol. 2010 Mar;202(3):261 e261–265 e261. doi: 10.1016/j.ajog.2009.10.867. [DOI] [PubMed] [Google Scholar]
- 20.Reutrakul S, Zaidi N, Wroblewski K, et al. Interactions between pregnancy, obstructive sleep apnea, and gestational diabetes mellitus. The Journal of clinical endocrinology and metabolism. 2013 Oct;98(10):4195–4202. doi: 10.1210/jc.2013-2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Facco FL, Ouyang DW, Zee PC, Grobman WA. Development of a pregnancy-specific screening tool for sleep apnea. J Clin Sleep Med. 2012;8(4):389–394. doi: 10.5664/jcsm.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Facco FL, Ouyang DW, Zee PC, Grobman WA. Sleep Disordered Breathing in a High Risk Cohort-Prevalence and Severity across Pregnancy. Am J Perinatol. 2013 doi: 10.1055/s-0033-1363768. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hedner J, Pillar G, Pittman SD, Zou D, Grote L, White DP. A novel adaptive wrist actigraphy algorithm for sleep-wake assessment in sleep apnea patients. Sleep. 2004 Dec 15;27(8):1560–1566. doi: 10.1093/sleep/27.8.1560. [DOI] [PubMed] [Google Scholar]
- 24.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012 Oct 15;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clinic proceedings. Mayo Clinic. 2011 Jun;86(6):549–554. doi: 10.4065/mcp.2010.0810. quiz 554-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pittman SD, Ayas NT, MacDonald MM, Malhotra A, Fogel RB, White DP. Using a wrist-worn device based on peripheral arterial tonometry to diagnose obstructive sleep apnea: in-laboratory and ambulatory validation. Sleep. 2004 Aug 1;27(5):923–933. doi: 10.1093/sleep/27.5.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zou D, Grote L, Peker Y, Lindblad U, Hedner J. Validation a portable monitoring device for sleep apnea diagnosis in a population based cohort using synchronized home polysomnography. Sleep. 2006 Mar 1;29(3):367–374. doi: 10.1093/sleep/29.3.367. [DOI] [PubMed] [Google Scholar]
- 28.Ayas NT, Pittman S, MacDonald M, White DP. Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med. 2003 Sep;4(5):435–442. doi: 10.1016/s1389-9457(03)00111-4. [DOI] [PubMed] [Google Scholar]
- 29.O'Brien LM, Bullough AS, Shelgikar AV, Chames MC, Armitage R, Chervin RD. Validation of Watch-PAT-200 against polysomnography during pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2012 Jun 15;8(3):287–294. doi: 10.5664/jcsm.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol. 2002 Jan;99(1):159–167. doi: 10.1016/s0029-7844(01)01747-1. [DOI] [PubMed] [Google Scholar]
- 31.Caritis S, Sibai B, Hauth J, et al. Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998 Mar 12;338(11):701–705. doi: 10.1056/NEJM199803123381101. [DOI] [PubMed] [Google Scholar]
- 32.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009 Jan 3;373(9657):82–93. doi: 10.1016/S0140-6736(08)61622-0. [DOI] [PubMed] [Google Scholar]
- 33.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstetrics and gynecology. 1996 Feb;87(2):163–168. doi: 10.1016/0029-7844(95)00386-X. [DOI] [PubMed] [Google Scholar]
- 34.Pamidi S, Pinto LM, Marc I, Benedetti A, Schwartzman K, Kimoff RJ. Maternal sleep-disordered breathing and adverse pregnancy outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol. 2013 Aug 2; doi: 10.1016/j.ajog.2013.07.033. [DOI] [PubMed] [Google Scholar]
- 35.Luque-Fernandez MA, Bain PA, Gelaye B, Redline S, Williams MA. Sleep-disordered breathing and gestational diabetes mellitus: a meta-analysis of 9,795 participants enrolled in epidemiological observational studies. Diabetes care. 2013 Oct;36(10):3353–3360. doi: 10.2337/dc13-0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bayram NA, Ciftci B, Keles T, et al. Endothelial function in normotensive men with obstructive sleep apnea before and 6 months after CPAP treatment. Sleep. 2009 Oct;32(10):1257–1263. doi: 10.1093/sleep/32.10.1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ciccone MM, Favale S, Scicchitano P, et al. Reversibility of the endothelial dysfunction after CPAP therapy in OSAS patients. Int J Cardiol. 2012 Jul 26;158(3):383–386. doi: 10.1016/j.ijcard.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 38.Kohler M, Stoewhas AC, Ayers L, et al. Effects of continuous positive airway pressure therapy withdrawal in patients with obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med. 2011 Nov 15;184(10):1192–1199. doi: 10.1164/rccm.201106-0964OC. [DOI] [PubMed] [Google Scholar]
- 39.Ohike Y, Kozaki K, Iijima K, et al. Amelioration of vascular endothelial dysfunction in obstructive sleep apnea syndrome by nasal continuous positive airway pressure--possible involvement of nitric oxide and asymmetric NG, NG-dimethylarginine. Circ J. 2005 Feb;69(2):221–226. doi: 10.1253/circj.69.221. [DOI] [PubMed] [Google Scholar]
- 40.Sharma SK, Agrawal S, Damodaran D, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med. 2011 Dec 15;365(24):2277–2286. doi: 10.1056/NEJMoa1103944. [DOI] [PubMed] [Google Scholar]
- 41.Zamarron C, Riveiro A, Gude F. Circulating levels of vascular endothelial markers in obstructive sleep apnoea syndrome. Effects of nasal continuous positive airway pressure. Arch Med Sci. 2011 Dec 31;7(6):1023–1028. doi: 10.5114/aoms.2011.26615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2010 Oct;33(10):1373–1380. doi: 10.1093/sleep/33.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barbe F, Duran-Cantolla J, Capote F, et al. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010 Apr 1;181(7):718–726. doi: 10.1164/rccm.200901-0050OC. [DOI] [PubMed] [Google Scholar]
- 44.Duran-Cantolla J, Aizpuru F, Montserrat JM, et al. Continuous positive airway pressure as treatment for systemic hypertension in people with obstructive sleep apnoea: randomised controlled trial. BMJ. 2010;341:c5991. doi: 10.1136/bmj.c5991. [DOI] [PubMed] [Google Scholar]
- 45.Haentjens P, Van Meerhaeghe A, Moscariello A, et al. The impact of continuous positive airway pressure on blood pressure in patients with obstructive sleep apnea syndrome: evidence from a meta-analysis of placebo-controlled randomized trials. Arch Intern Med. 2007 Apr 23;167(8):757–764. doi: 10.1001/archinte.167.8.757. [DOI] [PubMed] [Google Scholar]
- 46.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005 Mar 19–25;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]