Abstract
Objective
to test the null hypothesis that patients with the terrible triad of the elbow (dislocation together with fractures of the radial head and coronoid process) who are treated with open reduction and internal fixation of the radial head have final results that are comparable with those of patients treated with arthroplasty or partial resection of the radial head.
Methods
twenty-six patients with the terrible triad of the elbow who were operated by a single surgeon were evaluated on average 23 months after the surgery (range: 16–36 months). There were 17 men and nine women of mean age 41 ± 13.4 years. The fractures of the radial head were treated by means of osteosynthesis (12 patients), arthroplasty (nine) or resection of a small fragment or no treatment (five). Fixation of the coronoid process/anterior capsule was performed in 21 patients. The lateral ligament complex (LLC) was repaired in all the patients, while the medial ligament complex (MLC) was repaired in three patients whose elbows remained unstable after treatment for the radial head and LLC, but without fixation of the coronoid process.
Results
the mean final range of flexion and extension was 112°. The mean pronation was 70° and supination, 6°. The mean DASH score (Disabilities of the Arm, Shoulder & Hand) was 12 and mean MEPI (Mayo Elbow Performance Index) was 87. According to the MEPI scores, 21 patients (80%) had good and excellent results. There was no statistically significant difference in the results between the patients who underwent fixation of the radial head and those who underwent arthroplasty or resection of a small fragment.
Conclusion
there was no difference between the patients treated with arthroplasty of the radial head and those treated with other techniques.
Keywords: Dislocations, Elbow joint, Radial fractures
Resumo
Objetivo
testar a hipótese nula de que os pacientes com a tríade terrível do cotovelo (luxação associada a fraturas da cabeça do rádio e do processo coronoide) tratados com redução aberta e fixação interna da cabeça do rádio têm resultado final comparável aos pacientes tratados com artroplastia ou ressecção parcial da cabeça do rádio.
Métodos
foram avaliados, em média aos 23 meses (16 a 36) após a cirurgia, 26 pacientes com a tríade terrível do cotovelo operados por um único cirurgião. Eram 17 homens e nove mulheres, com média de idade de 41 anos (± 13,4). As fraturas da cabeça do rádio foram tratadas com osteossíntese (12 pacientes), ou artroplastia (nove), ou ressecção de um fragmento pequeno ou nenhum tratamento (cinco). Fixação do processo coronoide/cápsula anterior foi feita em 21 pacientes. O complexo ligamentar lateral (LCL) foi reparado em todos os pacientes, enquanto que o complexo ligamentar medial (LCM) foi reparado em três pacientes cujos cotovelos persistiam instáveis após o tratamento da cabeça do rádio e do LCL, mas sem fixação do processo coronoide.
Resultados
o arco final médio de flexão e extensão foi de 112°. A pronação média foi de 70° e a supinação, de 6°. O escore Dash (Disabilities of Arm, Shoulder & Hand) médio foi de 12 e o Mepi (Mayo Elbow Performance Index) médio foi de 87. De acordo com o Mepi, 21 pacientes (80%) tiveram bons e excelentes resultados. Não houve diferença estatisticamente significativa entre os resultados dos pacientes submetidos a fixação da cabeça do rádio e aqueles submetidos a artroplastia ou ressecção de um fragmento pequeno.
Conclusão
não há diferença entre os pacientes tratados com a artroplastia da cabeça do rádio daqueles tratados com outras técnicas.
Palavras-chave: Luxações, Articulação do cotovelo, Fraturas do rádio
Introduction
Injuries that involve dislocation of the elbow in association with fracturing of the radial head and fracturing of the coronoid process are referred to as the terrible triad of the elbow.1 Historically, these injuries have been difficult to deal with and the results from treatment have been unsatisfactory due to instability, arthrosis and/or stiffness of the elbow.2, 3 The difficulty in treating this injury pattern has been ascribed to lack of knowledge regarding the anatomical factors involved in elbow stabilization and the appropriate surgical techniques. Pugh and McKee4, 5 described a systematized approach for surgical treatment of the terrible triad of the elbow, which included osteosynthesis or arthroplasty of the radial head, repair of the coronoid when possible and/or repair of the joint capsule, and repair of the lateral ligament complex (LLC) of the elbow. They reported that 80% of their patients presented good or excellent results and also that the revision rate was 15–25%. Since then, several authors have presented good and excellent results (77–100%) from surgical treatment of the terrible triad of the elbow, in accordance with the protocol presented by Pugh et al.6, 7, 8, 9, 10, 11, 12, 13, 14
This study had the objective of evaluating the clinical and radiographic results from patients with the terrible triad of the elbow who were operated in accordance with this protocol. Our hypothesis was that the patients who underwent arthroplasty of the radial head would have results that were comparable to those of the other patients.
Methods
Between March 2007 and December 2009, 32 patients with the terrible triad of the elbow were diagnosed and underwent surgical treatment performed by the same surgeon (LBJG) at Hospital Madre Teresa (HMT) and “Risoleta Tolentino Neves” University Hospital (HURTN). Six patients were excluded: four who could not be found and two who did not adhere to the postoperative follow-up. Thus, 26 patients remained for evaluation (17 men and nine women), with a mean age of 41 years (±13.4). Three were left-handed and 23 were right-handed. The injury mechanisms were falls from a height in 13 cases, motorcycle accidents in 10 cases and being run over, falling off a bicycle and being in a car accident in one case each. The elbows were operated, on average, nine days (±5.93) after the initial trauma. The left side was affected in 17 patients (65%) and right side in seven (35%).
The fractures of the radial head were classified as type 4, in accordance with Mason's classification as modified by Johnston.15 In six fractures, only one fragment was identified and, in four of these, there was an anterior fragment accounting for less than 20% of the joint surface, which was extremely comminuted, without the possibility of fixation. Five fractures had two fragments, seven fractures had three and eight fractures had more than three.
The fractures of the coronoid process were classified in accordance with O’Driscoll,16 who divided such fractures, as seen on a coronal slice from a computed tomography scan, into three main types. Type 1 consists of fractures of the top of the coronoid process: 1A with fragments up to 2 mm and 1B with fragments larger than 2 mm. Type 2 fractures are anteromedial and type 3 are at the base of the coronoid process. Type 1A fractures of the coronoid process were identified in 19 patients, and type 1B fractures in the remaining seven patients.
In all the patients, injuries to the lateral ligament complex die to avulsion at its origin in the lateral condyle were identified. Reinsertion was performed by means of a transosseous suture or a 4.0 metal anchor (Hexagon Ind. e Com. de Aparelhos Ortopédicos Ltda., Campinas, SP) using Ethibond no. 2 thread (Johnson & Johnson do Brasil Ltda., São José dos Campos, SP). Reinsertion of the medial ligament complex was performed in only three patients, by means of 4.0 metal anchors and Ethibond no. 2 thread. These patients presented residual instability after treatment of the fracture of the radial head and the lateral ligament complex. In these three cases, the coronoid process/anterior capsule was not fixed because, during the preoperative assessment, the surgeon considered these to be separate injuries that did not contribute toward the elbow instability.
Seven patients presented other fractures in the ipsilateral upper limb: two fractures in the distal radius, one fracture in the ulnar styloid, one fracture in the lateral condyle, one Stenner injury in the thumb, one fracture of the metacarpal and one rotator cuff injury in the shoulder. With the exception of the rotator cuff injury, all the others were fixed during the same operation, in order to accelerate elbow rehabilitation during the postoperative period.
In all the patients, a universal posterior incision in the elbow was made, with lateral subcutaneous pushback until the elbow was completely exposed laterally. The Kocher interval was explored using the spacing already defined by the lateral ligament injury, in order to obtain access to the elbow joint. After the joint had been exposed, the coronoid process was dealt with first. In 12 patients, transosseous suturing of pull-out type was performed, which included the anterior joint capsule and the fragment of the coronoid process. In one patient, the suturing was performed by means of a 4.0 metal anchor that was inserted into the proximal ulna. In eight patients who all had type 1B fractures of the coronoid process, osteosynthesis of the fractured bone fragment of the coronoid process was performed using a cannulated screw alone in two cases, cannulated screw and Kirschner wires in two cases, cannulated screw and transosseous suturing of the capsule in one case, Kirschner wires and transosseous suturing in two cases and Kirschner wires alone in one case. In five patients, no repair to the coronoid process was performed, because during the preoperative assessment, the surgeon considered that these were separate injuries that did not contribute toward the elbow instability.
The radial head was dealt with next. For four patients who presented an anterior fragment accounting for less than 20% of the joint surface, which was comminuted and did not present any possibility of reconstruction, it was decided to perform simple resection of the fragments, since there was no impairment of elbow stabilization (Fig. 1). In six fractures, osteosynthesis using Herbert screws was performed. In four cases, Kirschner wires were used in addition to Herbert screws. In two patients, screws and plates were used. In eight patients, uncemented arthroplasty of the radial head was performed using a monoblock prosthesis (Meta Bio Industrial Ltda., Rio Claro, SP), with three possible sizes, relating to neck lengths of 9, 12 and 19 mm. In one patient, arthroplasty was performed using a methyl methacrylate molded prosthesis, which was removed eight weeks later. In one patient who presented only slight displacement, the fracture was not subjected to osteosynthesis.
Fig. 1.

A 56-year-old woman who suffered a fall from a standing position. (A) Lateral and anteroposterior radiographs prior to reduction, showing posterior dislocation of the elbow and type 2 fracturing of the radial head, with a comminuted anterior fragment. (B) Lateral and anteroposterior radiographs after surgical treatment, showing concentric reduction of the elbow, despite resection of the anterior fragment of the radial head.
Lastly, the lateral ligament complex of the elbow was reinserted at its isometric point, either by means of metal anchors or by means of transosseous suturing. The stability of the elbow was tested through full passive extension of the elbow in neutral orientation. Following this, assisted passive flexion of the elbow was performed, with the aim of testing concentric stability over the entire range of motion (ROM). In three patients, residual posterior subluxation was observed: in these cases, the medial ligament complex was repaired using a 4.0 anchor and Ethibond no. 2 thread, and joint stability was reestablished over the entire ROM. There was no need for an articulated external fixator in any patient.
After the surgery, the elbow was immobilized for one week at 90° of flexion and in pronation, using a plaster-cast splint. After the immobilization had been removed, the patients were advised to start a home-based program for early gains in ROM, which consisted of active flexion and extension of the elbow (extension with the elbow pronated), along with passive pronation-supination of the elbow while flexed at 90°. This program was continued for six weeks and, during this period, the patients were instructed not to perform abduction of the shoulder greater than 60°, or abduction with the shoulder flexed at 90°, in order to avoid varus stress on the ligament reconstruction, as recommended by Duckworth et al.17 Six weeks later, the patients were referred for physiotherapy and rehabilitation of the operated limb was started under supervision.
Postoperative controls were conducted in the 1st, 2nd and 6th weeks and in the 3rd, 6th and 12th months. Pain was assessed using a visual analog scale, ROM by means of a goniometer and stability through clinical tests (pivot shift and drawer) and radiograph imaging, in terms of concentric reductions observed in anteroposterior (AP) and lateral views. The consolidation of the fractures and presence of heterotopic ossification and degenerative alterations were also assessed.
The final evaluation on the patients was made by a properly trained shoulder and elbow surgery specialist and consisted of application of the DASH18 and MEPI19 questionnaires, measurement of the ROM, assessment of joint stability, investigation of complications and other surgical procedures in the same elbow, and evaluation of AP and lateral-view radiographs in order to investigate calcification around the ligament insertions, heterotopic ossification and degenerative alterations of the elbow. These alterations were classified in accordance with the criteria of Broberg and Morrey19: grade 0 (absence; i.e. normal elbow); grade 1 (mild; joint narrowing alone and minimal formation of osteophytes); grade 2 (moderate; moderate joint narrowing and moderate formation of osteophytes); grade 3 (severe; severe narrowing and joint destruction).
The variables were analyzed using Fisher's test and values were considered to be significant when p < 0.05.
Results
The final evaluation was made after an average postoperative period of 23 months (range: 12–36). The final mean flexed contracture was 20° (±13.70°), with a range from 0° to 40° (Fig. 2). The final mean flexion was 132° (±13.20°), with a range from 90° to 150°. The final mean ROM was 112° (±24.29°). The mean pronation was 70° (±18.34°), with a range from 0° to 80°. The mean supination was 63° (±19.92°), with a range from 0° to 80°.
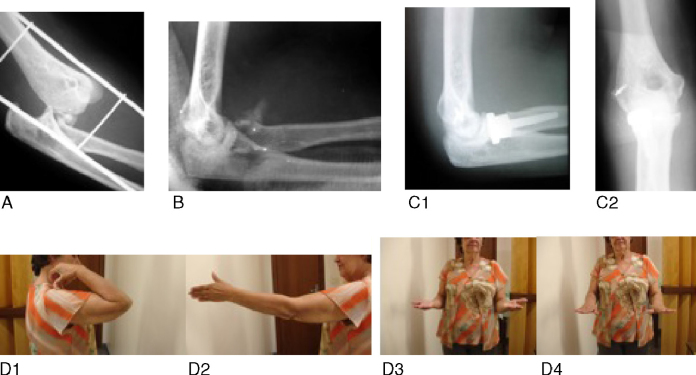
Fig. 2.
A 54-year-old woman who suffered a fall from a standing position. (A) Lateral radiograph prior to reduction, showing posterior dislocation of the elbow and fracturing of the radial head. (B) Lateral radiograph after reduction, showing comminutive fracturing of the radial head and fracturing of the coronoid. C1 and C2: lateral and anteroposterior radiographs showing concentric reduction of the elbow, the radial head prosthesis and the lateral metal anchor. D1, D2, D3 and D4: clinical results from final follow-up.
The mean DASH was 12 (±15.36), with a range from 0 to 44. The mean MEPI was 87 (±14.34), with a range from 50 to 100. The individual MEPI analysis showed that there were 12 excellent, nine good, four fair and one poor result, i.e. 80% of the patients presented satisfactory results. The radiographic evaluation showed that there were no degenerative alterations in 14 patients (54%), while nine patients presented grade 1 alterations, one grade 2 and none grade 3. In the cases of two patients, no updated radiographic assessment was possible.
Among the eight patients who received a radial head prosthesis, four (50%) presented a flexion-extension range of less than 100°. In the group of 17 patients whose radial heads were reconstructed, only three (17%) had a flexion-extension range of less than 100°. However, these values were not statistically significant (p = 0.159). The MEPI in the arthroplasty group was less than 75 in three patients (37%), and it was also less than 75 in three patients (17%) in the group that underwent osteosynthesis. However, these values were not statistically significant (p = 0.208). In this evaluation, the patient who underwent arthroplasty of the radial head using a methyl methacrylate molded prosthesis, which was subsequently removed, was excluded from the comparative analysis, despite presenting MEPI of 85° and a flexion-extension range of 150°.
Complications
None of the patients presented any infections, dehiscence of the operative wound or neurovascular lesions. Five patients had complications that required surgical treatment. One presented avascular necrosis and pseudarthrosis of the radial head and underwent removal of the synthesis material together with the bone fragments from the radial head, three months after the index surgery. Four patients developed elbow joint stiffness. Of these, two presented anterior heterotopic ossification and three had undergone radial head arthroplasty. All of them underwent surgical release of the elbow in association with removal of the radial head prosthesis and the heterotopic ossification, in the cases in which these were present. In one patient, two osteocapsular releases of the elbow were performed. One of the patients developed proximal radioulnar synostosis after removal of the prosthesis, and subsequently underwent the Kaminemi–Morrey procedure,20 but there was no gain in pronation-supination, because of the neoformation of synostosis. This patient refused new surgery.
Discussion
Historically, published papers on treatment of the terrible triad were sparse, presented small case series and had different surgical or conservative approaches. All of them presented poor results from treatments for this type of injury.2, 3, 19
Recently, several studies and investigations have provided better understanding of the biomechanics and stability of the elbow and of the interactions between these factors21, 22, 23, 24, 25, 26, 27, 28 and have contributed toward publication of better surgical results from this injury. Pugh et al.4, 5 described a systematized approach for surgical treatment of the terrible triad of the elbow, which included osteosynthesis or arthroplasty of the radial head, repair of the coronoid if possible and/or the joint capsule, and repair of the lateral ligament complex of the elbow, along with making repairs to the medial collateral ligament and using external fixators for the elbow in selected cases. These authors demonstrated good and excellent results in most of their patients and also presented a revision rate of 15–25%. Subsequently, several studies presented consistent and reproducible results through using the same systematized approach, with proportions of good and excellent results of 77–84%.6, 9, 13
Our study confirms the results from these more recent studies and reinforces the reproducibility of satisfactory results among patients who undergo the approach proposed by Pugh et al. Among our patients, 80% presented good and excellent results, with a mean MEPI of 87 points and a mean DASH of 12. Nonetheless, 38% presented some degree of degenerative alterations, even though most of these were mild, which supports the notion that a subtle degree of joint instability persists. This would give rise to poor functioning of the joint, with a consequent early start to degenerative alterations in some of these elbows. A longer follow-up period would be needed to evaluate the progression of these degenerative alterations and their possible clinical repercussions.
Our null hypothesis was corroborated. Although several papers have emphasized the importance of trying to constitute the radiocapitellar joint anatomically or as close to this as possible, there are no studies that have compared the results from arthroplasty of the radial head with other techniques for treating the terrible triad. Van Glabbeeket et al.29 described the importance of restoring the length of the radius after arthroplasty of the radial head, in elbows with injuries to the medial collateral ligament. These authors recommended that replacement of the radial head should be done with the same accuracy and reproducibility regarding the positions of the components as in any other arthroplasty. Charalambouset et al.30 suggested that osteosynthesis of the radial head in patients with medial collateral ligament injuries presented results that were superior to those of arthroplasty and excision of the radial head, with regard to the varus stability of the elbow. The radial head prosthesis that we had available to us was modular, with just three size possibilities, all related to the neck length: 9 mm, 12 mm and 19 mm. There were no variations in the size of the radial head, the nail or the bipolarity. Thus, this prosthesis has the primary function of acting as a spacer and enabling adequate healing of the soft tissues after the operation. We imagined that although this prosthesis would be unable to reestablish the radiocapitellar and proximal radioulnar joints more precisely, patients undergoing arthroplasty of the radial head would have results similar to those who underwent other treatments. In comparing these groups, we did not find any statistically significant results. Thus, we believe that if treatment of the radial head is chosen, the resected radial head should be replaced by a rigid spacer, which could be a metal prosthesis or a radial head molded from methyl methacrylate, as was done in one of our patients, until adequate healing of the soft tissues has been achieved. Clearly, this is a conclusion from a short follow-up and with a small group of patients, which weakens the statistical analysis. A longer follow-up is necessary in order demonstrate whether the “non-anatomical” reconstruction of the radial head might have consequences for the elbow.
This study presents some limitations. It was a retrospective observational study with a short average follow-up (23 months). This short follow-up made it impossible to correctly assess the incidence, progression and clinical repercussions of secondary degenerative osteoarthrosis, which is one of the most feared and difficult-to-treat late complications. The small number of patients in each group evaluated also weakened the final analysis of our hypothesis.
Conclusion
Surgical treatment of the terrible triad of the elbow provided satisfactory and reproducible results for most patients, independent of the method of treating the fracture of the radial head. There were no differences between the patients treated with osteosynthesis of the radial head and those treated with arthroplasty of the radial head or resection of a fragment.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Gonçalves LBJ, Neto JAS, Correa Filho MRC, de Andrade RP, de Andrade MAP, Gomes AH, et al. Tríade terrível do cotovelo: a influência do tratamento da cabeça do rádio. Rev Bras Ortop. 2014;49:328–333.
Work performed at Hospital Madre Teresa and Hospital Unimed, Belo Horizonte, MG, Brazil.
References
- 1.Hotchkiss R.N. Fractures and dislocations of the elbow. In: Rockwood C.A., Green D.P., Bucholz R.W., Heckman J.D., editors. 4th ed. Vol. 1. Lippincott-Raven; Philadelphia: 1996. pp. 929–1024. (Rockwood and Green's fractures in adults). [Google Scholar]
- 2.Josefsson P.O., Gentz C.F., Johnell O., Wendeberg B. Dislocations of the elbow and intraarticular fractures. Clin Orthop Relat Res. 1989;(246):126–130. [PubMed] [Google Scholar]
- 3.Ring D., Jupiter J.B., Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84A:547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Pugh D.M., McKee M.D. The “terrible triad” of the elbow. Tech Hand Up Extrem Surg. 2002;6(1):21–29. doi: 10.1097/00130911-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Pugh D.M., Wild L.M., Schemitsch E.H., King G.J., McKee M.D. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg. 2004;86A:1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Forthman C., Henket M., Ring D.C. Elbow dislocation with intra-articular fracture: the results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am. 2007;32(8):1200–1209. doi: 10.1016/j.jhsa.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Lindenhovius A.L., Jupiter J.B., Ring D. Comparasion of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg Am. 2008;33(6):920–926. doi: 10.1016/j.jhsa.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Zeiders G.J., Patel M.K. Management of unstable elbows following complex fracture-dislocations – the “terrible triad” injury. J Bone Joint Surg Am. 2008;90(Suppl. 4):75–84. doi: 10.2106/JBJS.H.00893. [DOI] [PubMed] [Google Scholar]
- 9.Winter M., Chuinard C., Cikes A., Pelegri C., Bronsard N., de Peretti F. Surgical management of the elbow dislocation associated with non-reparable fractures of the radial head. Chir Main. 2009;28(3):158–167. doi: 10.1016/j.main.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Seijas R., Ares-Rodriguez O., Orellana A., Albareda D., Collado D., Llusa M. Terrible triad of the elbow. J Orthop Surg (Hong Kong) 2009;17(3):335–339. doi: 10.1177/230949900901700319. [DOI] [PubMed] [Google Scholar]
- 11.Guitton T.G., Ring D. Nonsurgically treated terrible triad injuries of the elbow: report of four cases. J Hand Surg Am. 2010;35(3):464–467. doi: 10.1016/j.jhsa.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 12.Chemama B., Bonnevialle N., Peter O., Mansat P., Bonnevialle P. Terrible triad injury of the elbow: how to improve outcomes? Orthop Traumatol Surg Res. 2010;96(2):147–154. doi: 10.1016/j.rcot.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Martin J., Pretell-Mazzini J., Andres-Esteban E.M., Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols: a review. Int Orthop. 2011;35(6):851–860. doi: 10.1007/s00264-010-1024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeong W.K., Oh J.K., Hwang J.H., Hwang S.M., Lee W.S. Results of terrible triads in the elbow: the advantage of primary restoration of medial structure. J Orthop Sci. 2010;15(5):612–619. doi: 10.1007/s00776-010-1515-8. [DOI] [PubMed] [Google Scholar]
- 15.Johnston G.W. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J. 1962;31:51–56. [PMC free article] [PubMed] [Google Scholar]
- 16.O’Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 17.Duckworth A.D., Kulijdian A., McKee M.D., Ring D. Residual subluxation of the elbow after dislocation or fracture-dislocation: treatment with active elbow exercises and avoidance of varus stress. J Shoulder Elbow Surg. 2008;17(2):276–280. doi: 10.1016/j.jse.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 18.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the Dash (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 19.Broberg M.A., Morrey B.F. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68(5):669–674. [PubMed] [Google Scholar]
- 20.Kamineni S., Maritz N.G., Morrey B.F. Proximal radial resection for posttraumatic radioulnar synostosis: a new technique to improve forearm rotation. J Bone Joint Surg Am. 2002;84-A(5):745–751. doi: 10.2106/00004623-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Morrey B.F., An K.N. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11(5):315–319. doi: 10.1177/036354658301100506. [DOI] [PubMed] [Google Scholar]
- 22.O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73(3):440–446. [PubMed] [Google Scholar]
- 23.Dunning C.E., Zarzour Z.D., Patterson S.D., Johnson J.A., King G.J. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 2001;83-A(12):1823–1828. doi: 10.2106/00004623-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 24.McKee M.D., Schemitsch E.H., Sala M.J., O’Driscoll S.W. Thepathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003;12(4):391–396. doi: 10.1016/s1058-2746(03)00027-2. [DOI] [PubMed] [Google Scholar]
- 25.Schneeberger A.G., Sadowski M.M., Jacob H.A. Coronoid process and radial head as posterolateral rotatory stabilizer of the elbow. J Bone Joint Surg Am. 2004;86-A(5):975–982. doi: 10.2106/00004623-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Okazaki M., Takayama S., Seki A., Ikegami H., Nakamura T. Posterolateral rotatory instability of the elbow with insufficient coronoid process of the ulna: a report of 3 patients. J Hand Surg Am. 2007;32(2):236–239. doi: 10.1016/j.jhsa.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Hull J.R., Owen J.R., Fern S.E., Wayne J.S., Boardman N.D., III Role of the coronoid process in varus osteoarticular stability of the elbow. J Shoulder Elbow Surg. 2005;14(4):441–446. doi: 10.1016/j.jse.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 28.Terada N., Yamada H., Seki T., Urabe M.D., Takayama T.S. The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J Shoulder Elbow Surg. 2000;9(4):344–346. doi: 10.1067/mse.2000.106082. [DOI] [PubMed] [Google Scholar]
- 29.Van Glabbeek F., Van Rie R.P., Bumfeld J.A., Neale P.G., O’Driscol S.W., Morrey B.F. Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am. 2004;86-A(12):2629–2635. doi: 10.2106/00004623-200412000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Charalambous C.P., Stanley J.K., Siddique I., Powell E., Ramamurthy C., Gagey O. Radial head fracture in the medial collateral ligament deficient elbow; biomechanical comparison of fixation, replacement, and excision in human cadavers. Injury. 2006;37(9):849–853. doi: 10.1016/j.injury.2006.04.125. [DOI] [PubMed] [Google Scholar]