Abstract
Objective
this was an epidemiological study on trochanteric bursitis at the time of performing total hip arthroplasty.
Methods
sixty-two sequential patients who underwent total hip arthroplasty due to osteoarthrosis, without any previous history of trochanteric bursitis, were evaluated. The bursas were collected and evaluated histologically.
Results
there were 35 female patients (56.5%) and 27 male patients (43.5%), with a mean age of 65 years (±11). Trochanteric bursitis was conformed histologically in nine patients (14.5%), of whom six were female (66.7%) and three were male (33.3%).
Conclusions
14.5% of the bursas analyzed presented inflammation at the time that the primary total hip arthroplasty due to osteoarthrosis was performed, and the majority of the cases of bursitis were detected in female patients.
Keywords: Hip arthroplasty, Osteoarthritis, Bursitis, Epidemiology
Resumo
Objetivo
fazer um estudo epidemiológico da bursite trocantérica no momento da feitura da artroplastia total do quadril (ATQ).
Métodos
foram avaliados 62 pacientes, sequenciais, submetidos à ATQ por osteoartrose, sem história prévia de bursite trocantérica. As bursas foram coletadas e avaliadas histologicamente.
Resultados
foram observados 35 pacientes do sexo feminino (56,5%) e 27 do masculino (43,5%), com média de 65 anos (+/−11). A bursite trocantérica foi confirmada histologicamente em nove (14,5%), seis do sexo feminino (66,7%) e três (33,3%) do masculino.
Conclusões
das bursas analisadas, 14,5% apresentaram inflamação no momento da feitura da ATQ primária por osteoartrose. A maioria das bursites foi detectada nas pacientes femininas.
Palavras-chave: Artroplastia de quadril, Osteoartrite, Bursite, Epidemiolgia
Introduction
Trochanteric bursitis is the term used to describe intermittent chronic pain accompanied by discomfort on palpation of the lateral region of the hip caused by an inflammatory process in the bursas.1 The bursas are pouches coated with synovial membranes, with fluids inside them, which are responsible for diminishing the friction of tendons and muscles over bone prominences.2 Among all the bursas of the hip that have been described, the trochanteric bursa is the one most frequently affected by inflammation. The most frequent cause of trochanteric bursitis is repetitive microtrauma due to active use of the muscles that are inserted into the greater trochanter, thereby resulting in degenerative changes to the tendons, muscles or fibrous tissues.3
Hip arthrosis is one of the musculoskeletal diseases that may be associated with trochanteric bursitis. Both in young and in old patients, the indications for total hip arthroplasty (THA) involve progressive worsening of pain with loss of function and worsening of quality of life consequent to osteoarthrosis.4 THA is the elective orthopedic procedure most performed worldwide, with the highest success rate.5 Nonetheless, there are no relevant data in the current literature regarding the incidence of trochanteric bursitis among patients undergoing THA. Silva et al.6 presented the only study on preoperative bursitis, but with few bursas collected and with patients presenting rheumatoid arthritis and osteoarthrosis.6 However, the incidence of trochanteric bursitis following THA procedures is approximately 4.6%.7 The gold-standard diagnosis for defining trochanteric bursitis is made through anatomopathological assessment of the bursa. Ferrala et al.8 and Nikolajsen et al.9 reported that, 12–18 months after the THA procedure, around 12% of their patients still presented chronic pain in performing their daily activities.8, 9
The present study aimed to evaluate the association between trochanteric bursitis and osteoarthrosis at the time of performing primary THA.
Materials and methods
This was a prospective study on 62 sequential patients who presented primary hip osteoarthrosis and underwent a THA procedure. Bursectomy is a routine procedure performed with THA at our service.
The bursas were collected during the surgery and were sent to the institution's pathology laboratory. An experienced pathologist analyzed the bursas and identified whether bursitis was present. Slides were prepared at section thicknesses of 2.0–3.0 μm and were stained using the hematoxylin-eosin technique. An Olympus optical microscope (model BX40) was used. The criterion used for diagnosing bursitis was the presence of capsule thickening, with fibroblastic proliferation and lymphocytic, histiocytic or neutrocytic inflammatory infiltrate, and with synovial hyperplasia.
Patients with rheumatoid arthritis, proximal epiphysiolysis of the femur, local tumors, developmental dysplasia of the hip, Legg–Calvé–Perthes disease, previous hip fractures, hemophilia, osteonecrosis, sequelae from septic arthritis and tuberculosis and previous procedures or radiotherapy on the hip that was to be operated. All the information was gathered from the medical files and also included demographic, epidemiological and clinical data such as age, sex and clinical presentations.
The statistical analysis on the data was performed using the Excel for Windows software, and it consisted of descriptive statistics and frequency distributions.
Results
There were 35 female patients (56.5%) and 27 male patients (43.5%). The mean age was 65 years (standard deviation ±11), with a range from 41 to 85.
The diagnosis of trochanteric bursitis was confirmed in nine of the patients analyzed (14.5%). Among these, six (66.7%) were female and three (33.3%) were male. Fig. 1 presents the histology of a normal bursa, at magnifications of 100× (A) and 200× (B). A thin fibrous membrane coated with synovial cells can be seen. Fig. 2 presents the histology of a bursa with an inflammatory process (chronic bursitis), at magnifications of 100× (A) and 200× (B), respectively. Fibrous thickening of the capsule can be seen, with a predominantly lymphocytic inflammatory infiltrate and synovial hyperplasia.
Fig. 1.
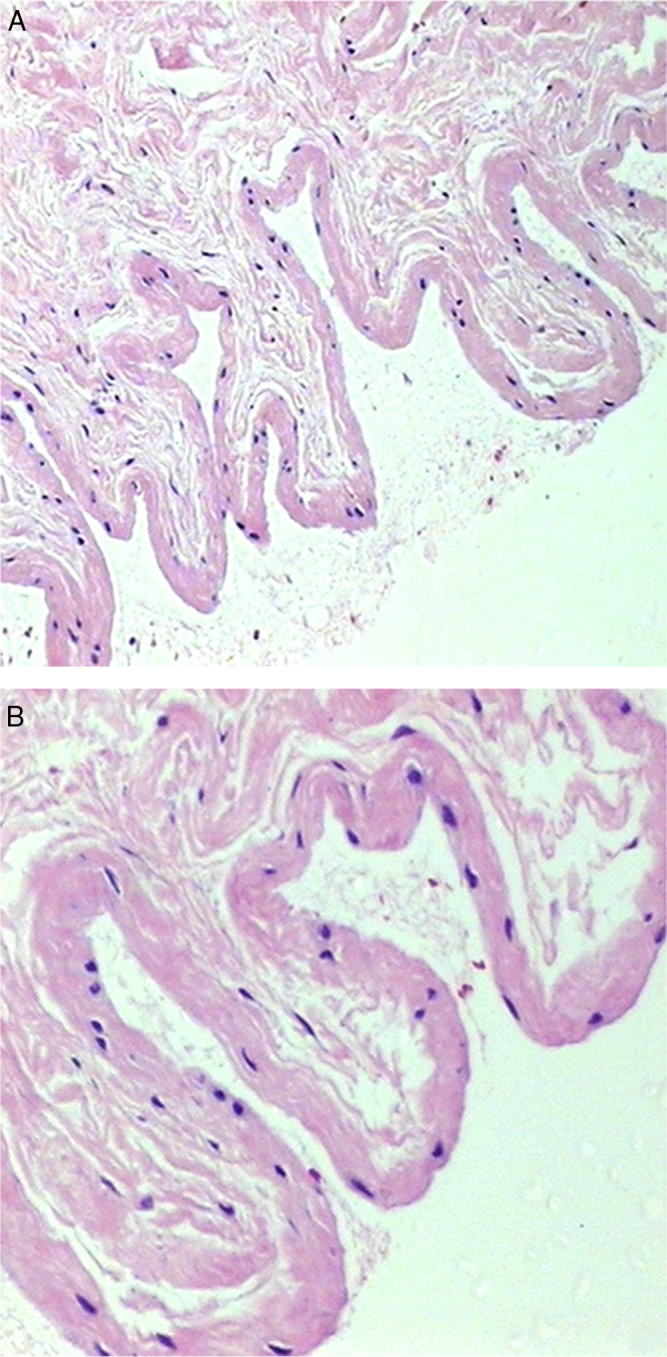
Normal trochanteric bursa stained using the hematoxylin-eosin technique: (A) magnification of 100× and (B) magnification of 200×.
Fig. 2.
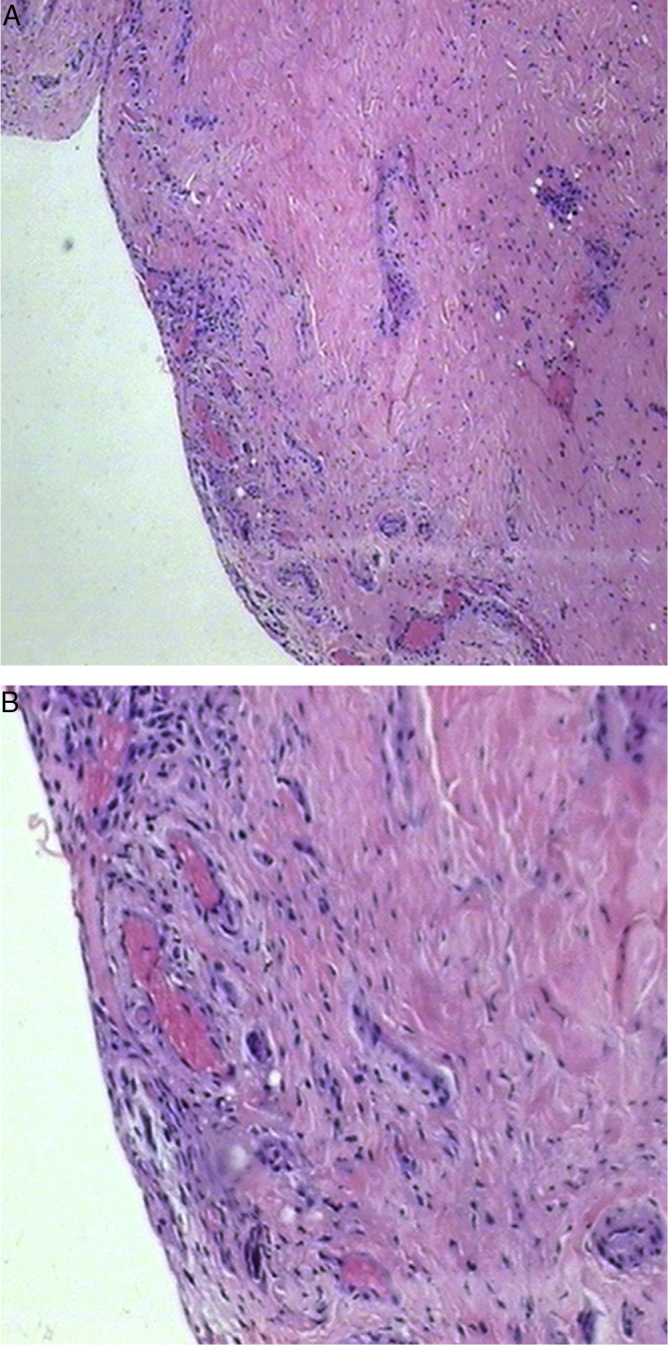
Chronic bursitis stained using the hematoxylin-eosin technique: (A) magnification of 100× and (B) magnification of 200×.
Discussion
The treatment for trochanteric bursitis is generally conservative and includes non-steroidal anti-inflammatory medications for up to six to eight weeks, along with ice. Infiltrations, thermal contrasts (ice and heat), rest and physiotherapy can also be used, with ultrasound at the level of the greater trochanter and femoral triangle, in association with muscle stretching for the iliotibial band and the iliopsoas tendon.3, 10 In the present study, no conservative treatment for bursitis had been administered prior to the surgical procedure, given that the patients presented symptomatic hip osteoarthrosis and THA was indicated. Thus, we aimed to study the epidemiology of the trochanteric bursitis at the time of performing the hip surgery.
Trochanteric bursitis may be a manifestation of a secondary disease such as hip osteoarthrosis. In the cases of the present study, we found that nine patients (14.5%) presented silent trochanteric bursitis at the time of their hip arthroplasty procedures, and that most of these patients were female (six; 66.7%). Thus, the great majority of the patients did not present trochanteric bursitis at the time of performing the primary THA.
Some hip surgeons do not perform resection of the bursa during the THA procedure. This might be reflected in the postoperative bursitis rates observed in the literature. Farmer et al. evaluated bursitis treatment consisting of use of injectable corticosteroids, after performing arthroplasty. They analyzed 689 primary arthroplasty procedures during the postoperative period and observed that the incidence was 4.6%.7
The present study investigated the incidence of trochanteric bursitis at the time of THA in patients with specific conditions, i.e. primary arthrosis. Although this does not portray the general condition of the population that undergoes arthroplasty, given that many patients present secondary arthrosis (rheumatoid arthritis, proximal epiphysiolysis of the femur, dysplasia, osteonecrosis, etc.), the data found in this study justify resection of the bursas during the arthroplasty procedure.
Conclusions
Among the patients who underwent THA due to osteoarthrosis (9/62), 14.5% presented silent trochanteric bursitis at the time of the hip surgery. Two thirds were female (66.7%).
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Schwartsmann CR, Loss F, de Freitas Spinelli L, Furian R, Silva MF, Zanatta JM, et al. Associação entre bursite trocantérica, osteoartrose e artroplastia total do quadril. Rev Bras Ortop. 2014;49:267–270.
Work performed in the Santa Casa de Porto Alegre Hospital Complex, Porto Alegre, RS, Brazil.
References
- 1.Alvarez-Nemegyei J., Canoso J.J. Evidence-based soft tissue rheumatology: III: Trochanteric bursitis. J Clin Rheumatol. 2004;10(3):123–124. doi: 10.1097/01.rhu.0000129089.57719.16. [DOI] [PubMed] [Google Scholar]
- 2.Stedman T.L., editor. Stedman: Dicionário médico. Tradução de Cláudia Lúcia Caetano de Araújo. 25th ed. Guanabara Koogan; Rio de Janeiro: 1996. [Google Scholar]
- 3.Dani W.S., Azevedo E. Bursite trocantérica. Rev Bras Med. 2006;7(1):2–5. [Google Scholar]
- 4.Shrader M.W. Total hip arthroplasty and hip resurfacing arthroplasty in the very young patient. Orthop Clin North Am. 2012;43(3):359–367. doi: 10.1016/j.ocl.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Pivec R., Johnson A.J., Mears S.C., Mont M.A. Hip arthroplasty. Lancet. 2012;380(9855):1768–1777. doi: 10.1016/S0140-6736(12)60607-2. [DOI] [PubMed] [Google Scholar]
- 6.Silva F., Adams T., Feinstein J., Arroyo R.A. Trochanteric bursitis: refuting the myth of inflammation. J Clin Rheumatol. 2008;14(2):82–86. doi: 10.1097/RHU.0b013e31816b4471. [DOI] [PubMed] [Google Scholar]
- 7.Farmer K.W., Jones L.C., Brownson K.E., Khanuja H.S., Hungerford M.W. Trochanteric bursitis after total hip arthroplasty: incidence and evaluation of response to treatment. J Arthroplasty. 2010;25(2):208–212. doi: 10.1016/j.arth.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Ferrala P., Carla S., Fortina M., Scipio D., Riva A., Di Giacinlo S. Painful hip arthroplasty: definition. Clin Cases Miner Bone Metab. 2011;8(2):19–22. [PMC free article] [PubMed] [Google Scholar]
- 9.Nikolajsen L., Brandsborg B., Lucht U., Jensen T.S., Kehlet H. Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand. 2006;50(4):495–500. doi: 10.1111/j.1399-6576.2006.00976.x. [DOI] [PubMed] [Google Scholar]
- 10.Huber T.A., Ortiz J. Bursite trocantérica. Rev Bras Ortop. 1992;27:723–728. [Google Scholar]


