Abstract
Objective
To evaluate the results from proximal fixation of uncemented conical femoral components in patients with a type C proximal femur and compare them with the results obtained from type A and B femurs.
Methods
This was a retrospective study on 87 patients with 90 uncemented total hip arthroplasty procedures. Three patients (three hips) were excluded because their follow-up lasted for less than two years. The follow-up ranged from 2 to 4.3 years and the mean was 2.8 years. The Bicontact femoral implant model was used. The preoperative radiographs were evaluated, the femurs were classified as Dorr types A, B or C and the cortical indices were measured. The patients were evaluated clinically by means of the Harris Hip Score (HHS), before the surgery and at the last follow-up. The sequences of postoperative radiographs were compared regarding stability, complications and any signs of osseointegration of the femoral prosthesis.
Results
Among the 87 hips with follow-up greater than two years, 32 femurs were type A (37%), 37 type B (42%) and 18 type C (21%). Before the operation, the mean HHS was 39.4 for types A and B and 38.8 for type C. At the last follow-up, the mean HHS was 89.8 for types A and B and 86 for type C. None of the 87 femoral components had been revised by the time of the last follow-up; all of them were considered stable. In 86 cases, the radiographs showed signs of osseointegration.
Conclusion
There were no significant differences in the clinical results or in the fixation (and osseointegration) of conical uncemented femoral prostheses with proximal porosity, among femurs with different types of femoral morphology according to the Dorr classification. This conclusion may vary if another implant model were to be used.
Keywords: Arthroplasty, Replacement, Hip; Osseointegration; Femur
Resumo
Objetivo
avaliar os resultados de componentes femorais cônicos não cimentados de fixação proximal em pacientes com fêmur proximal tipo C e compará-los com os resultados obtidos em fêmures tipos A e B.
Métodos
estudo retrospectivo de 87 pacientes com 90 ATQs não cimentadas. Três pacientes (três ATQs) foram excluídos por seguimento menor do que dois anos. Houve seguimento de dois a 4,3 anos e média de 2,8 anos. Foram usados implantes femorais modelo Bicontact. As radiografias pré-operatórias foram avaliadas e classificados os fêmures nos tipos A, B ou C de Dorr, além da aferição dos índices corticais (IC). Clinicamente os pacientes foram avaliados por meio do Harris Hip Score (HHS), antes da cirurgia e no último seguimento. Compararam-se as radiografias pós-operatórias sequenciais quanto a estabilidade, complicações e sinais de osteointegração ou não da prótese femoral.
Resultados
dos 87 quadris com seguimento maior do que dois anos, 32 fêmures eram tipo A (37%), 37 tipo B (42%) e 18 tipo C (21%). No pré-operatório a média do HHS foi de 39,4 nos tipos A e B e 38,8 no tipo C. No último seguimento o HHS em média foi de 89,8 nos tipos A e B e 86 no tipo C. Nenhum dos 87 componentes femorais foi revisado até o último seguimento. Todos foram considerados estáveis. As radiografias de 86 demonstraram sinais de osteointegração.
Conclusão
não houve diferença significativa nos resultados clínicos e na fixação (e osteointegração) de próteses femorais não cimentadas cônicas, com porosidade proximal, em fêmures dos diferentes tipos de morfologia femoral de acordo com a classificação de Dorr. Essa conclusão pode variar em caso de uso de outro modelo de implante.
Palavras-chave: Artroplastia de quadril, Osteointegração, Fêmur
Introduction
Cemented femoral components are the type most used in total hip arthroplasty (THA) in patients with broadened proximal femoral conformation and low bone quality.1
Dorr et al.2 classified proximal femoral conformation into types A, B and C, based on the thickness of the cortical bone and on the shape of the medullary canal. They demonstrated that type C femurs showed structural changes, increased numbers of cells and reduced cell activity. These characteristics indicated an environment that was less favorable to biological fixation of uncemented implants.
Some authors1 have indicated uncemented femoral components for use in young patients with femurs of types A and B. The bone quality of these patients allows greater security in surgical manipulation and better initial stabilization for uncemented femoral prostheses, with the theoretical advantage of better osseointegration.
Use of uncemented implants enables reduction of the duration of surgery and eliminates the time required for preparation and curing of the bone cement. In addition, not using bone cement reduces the risk of fatty embolism.3 The elderly population and individuals with debilitating diseases would be the greatest beneficiaries of these advantages, given their lower physiological reserves. However, these patients frequently have femurs of Dorr type C, which would contraindicate the use of uncemented prostheses.
There is controversy regarding the type of fixation for femoral prostheses that should be used in patients with osteoporosis. Some authors have recommended fixation with acrylic cement, because of fear that there would not be any stability and osseointegration because of the poor bone quality, especially in elderly patients.
Material and methods
Patients who underwent THA using uncemented femoral components at our institution between January 2007 and January 2009 were evaluated. The minimum time interval of the radiological evaluation was two years. Over the period analyzed, 92 THA procedures were performed on 89 patients consecutively. Five patients were excluded: one because of postoperative infection; one because of difficulty in classifying the femoral anatomy due to previous osteomyelitis and three because they did not have a minimum postoperative follow-up of two years. Therefore, 87 THA procedures in 84 patients formed the study group.
Uncemented femoral nails of Bicontact model (Aesculap, Germany) were implanted into the patients of the sample studied here. This prosthesis has a conical shape and is made of titanium alloy. Its cross-sectional format is plane rectangular, with lateral fixation wings and one dorsal anti-rotational wing. It has a microporous circumferential coating of pure titanium, applied as a plasma spray, with pores of 50–200 mcm in diameter. Chrome-cobalt heads of size 28 mm and uncemented acetabular components with a polyethylene liner were used in all the patients. All the THA procedures were performed with a posterolateral approach and with posterior repair of the capsule and external rotator muscles.
The femur was prepared using a sequence of compaction grinders, guided by preoperative planning, until adequate vertical and rotational stability had been attained. After bed preparation, the femoral component was introduced and press-fitted. In the cases in which fractures of the proximal femur were identified, steel wire was wrapped around the femur. The acetabular components were inserted and press-fitted, with additional fixation using two screws.
During the postoperative period, the patients were managed using a standard protocol and weight-bearing was allowed from the second day onwards. The patients used crutches until they were free from pain. The exception was patients with an intraoperative femoral fracture, who were allowed proprioceptive weight-bearing for six to eight weeks, in accordance with radiological controls, and were then released for full weight-bearing after showing signs of consolidation.
The patients were clinically assessed by means of the Harris Hip Score (HHS)4 before the operation and at the final postoperative follow-up consultation.
The morphology of the proximal femur was assessed retrospectively in a qualitative and quantitative manner. Preoperative radiographs in anteroposterior (AP) view of the pelvis and lateral view of the hip were analyzed.
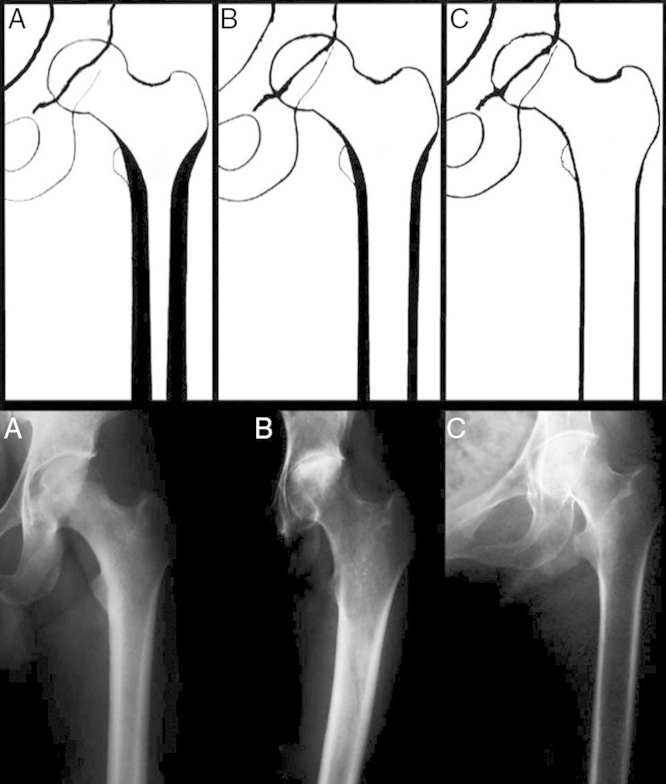
In the qualitative evaluation, which was done by two independent observers, three distinct patterns of femoral bone format and structure that were identified on radiographs between the metaphysis and the diaphyseal isthmus were taken into consideration. If these classifications were different for any given hip, the classification that was taken into consideration came from a third independent observer. As described by Dorr et al.,2 the three morphological patterns were named A, B and C (Fig. 1).
Fig. 1.
Schematic drawings and radiographs of the morphological types described by Dorr.
The femurs were quantitatively evaluated on the preoperative radiographs by means of the cortical index. This index was measured on the anteroposterior and lateral radiographs as illustrated in Fig. 2. Its values were proportional to the thickness of the cortical bone.
Fig. 2.
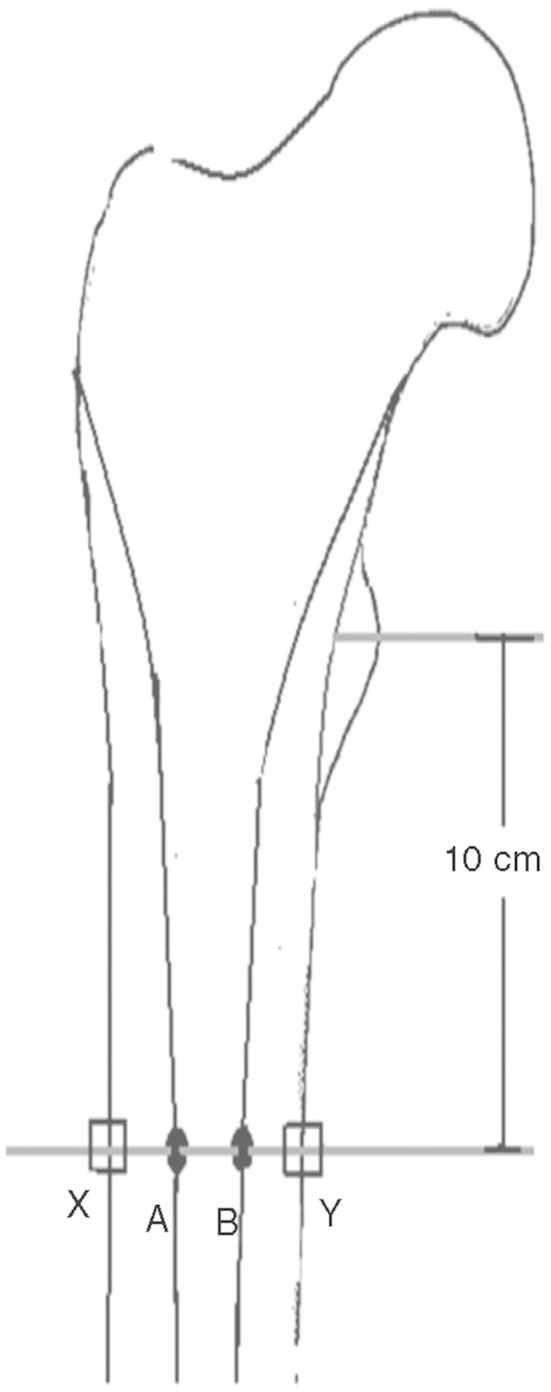
Measurement method for cortical index: CI = (DF-DM)/DF.
To analyze the fixation of the femoral component, radiographs produced in the immediate postoperative period, three months and one year afterwards, and finally after a minimum of two years, were used. On these radiographs, nine parameters were evaluated: (1) the initial position of the components; (2) occurrences of intraoperative fracturing of the femur; (3) cortical hypertrophy; (4) femoral radiolucency lines; (5) reactive lines; (6) remodeling of the calcar; (7) spot welds; (8) pedestal formation; and (9) migration of the femoral component. As described by Engh et al.,5 absence of reactive lines adjacent to the microporous surface of the implant and presence of spot welds were considered to be signs of osseointegration. Components that were not osseointegrated but did not present any progressive radiolucency or change of position were considered to be stable due to fibrosis.5, 6 Components with angular migration or with axial migration greater than 2 mm, three months after the operation, were considered to be unstable.7
Statistical analysis
For the statistical analysis, Student's t test and analysis of variance (ANOVA) were applied to estimate the differences between the radiographic measurements. Fisher's exact test was used to evaluate the frequencies of spot welds on the radiographs and the migration rates.
Results
The mean age at the time of the surgery was 57.8 years (range: 23.4–80.7) and the mean follow-up was 2.8 years (range: 2–4.3). There were 37 male patients and 47 female patients. The diagnosis for 41 patients (45 hips) was primary osteoarthrosis; 19 patients, osteonecrosis of the femoral head; nine patients, developmental dysplasia; seven patients, rheumatoid arthritis; and the remaining seven, post-traumatic coxarthrosis, septic post-arthritis coxarthrosis, femoral neck fracture, Perthes disease and ankylosing spondylitis (Table 1).
Table 1.
Demographic information.
| Patients (hips) | 84 (87) |
| Mean age (years) | 57.8 |
| Female sex | 47 (56%) |
| Primary osteoarthrosis | 45 (52%) |
| Osteonecrosis of the femoral head | 19 (22%) |
| Hip dysplasia | 9 (10%) |
| Rheumatoid arthritis | 7 (8%) |
| Other diagnoses | 7 (8%) |
Analysis on the radiographs regarding the morphological type of the proximal femur among the 87 hips showed that there were 32 type A femurs (37%), 37 type B (42%) and 18 type C (21%). The mean cortical indexes found on the anteroposterior radiographs of the femurs of types A, B and C were respectively 0.58, 0.49 and 0.38, and these were considered to be statistically different (p < 0.001). On lateral-view radiographs, the mean cortical indexes were 0.48, 0.41 and 0.28, which were also considered to be statistically different (p < 0.001) (Table 2).
Table 2.
Radiographic measurements of the cortical indexes (CI) in the different morphological types.
| Type A | Type B | Type C | |
|---|---|---|---|
| CI from anteroposterior radiographs | 0.57 (± 0.04) | 0.49 (± 0.05) | 0.38 (± 0.06) |
| CI from lateral radiographs | 0.48 (± 0.06) | 0.41 (± 0.06) | 0.28 (± 0.06) |
Results shown as mean ± standard deviation
The mean preoperative clinical score was 39.5 points (range: 22–55) and the postoperative score was 89.2 (range: 64–100). The mean preoperative score among patients with femurs of types A and B was 39.4 and in those with type C it was 38.8. At the last follow-up visit, the mean HHS was 89.8 for types A and B and 86 for type C. There were no statistically significant differences in the clinical results among the patients with different types of femoral morphology.
None of the 87 femoral components required revision up to the time of the last follow-up and all of them were considered stable. The radiographs on 86 of the femurs showed signs of osseointegration: 81% presented spot welds and 91% presented remodeling and rounding of the calcar. One femoral component with reactive lines in the microporous region was considered to be stable though fibrous fixation. This case migrated 2 mm distally over the first three postoperative months and then remained stable. In this case, the patient suffered from rheumatoid arthritis and presented type 3 morphology. Since this was the only case of its kind, it cannot be stated that there was any significant difference in the osseointegration rate between the type C femurs and the types A and B femurs.
In 16 femoral prostheses that were considered to be osseointegrated, no spot welds were seen on radiographs and, in these cases, absence of reactive lines adjacent to the microporous surface and modeling of the calcar were the criteria used to define osseointegration. Eight (47%) of the 17 osseointegrated components in the type C femurs did not show signs of welds, compared with 12% in types A/B. Thus, in the osseointegrated components, the presence of spot welds on radiographs was significantly lower (p < 0.01) in type C femurs (Table 3).
Table 3.
Frequency of spot welds on radiographs of the osseointegrated components.
| Types A/B | Type C | |
|---|---|---|
| Without spot welds on radiograph | 8 (12%) | 8 (47%) |
| With spot welds on radiograph | 61 (88%) | 9 (53%) |
| Total | 32 | 17 |
Radiographic reactive lines in the nonporous portion of the osseointegrated femoral implants were present in 62 cases, or 72% of the total. Using the zone classification proposed by Gruen et al.,8 the reactive lines occurred in zones 3 and 5 in 57 femurs (66%), in zone 4 (36%) and in zones 2 and 6 (21%). Cortical hypertrophy in the nonporous region of the nail was noted in 46% of the osseointegrated cases.
Distal migration of the femoral prosthesis greater than 2 mm was observed in 10 cases (11%), always in the first three postoperative months, and remained stable thereafter. With the exception of one case, cited earlier, all of them evolved with radiographic signs of osseointegration. Among the components that migrated more than 2 mm, six were of types A and B and four were of type C. This frequency tended to be greater in type C, although its statistical significance level was p = 0.2).
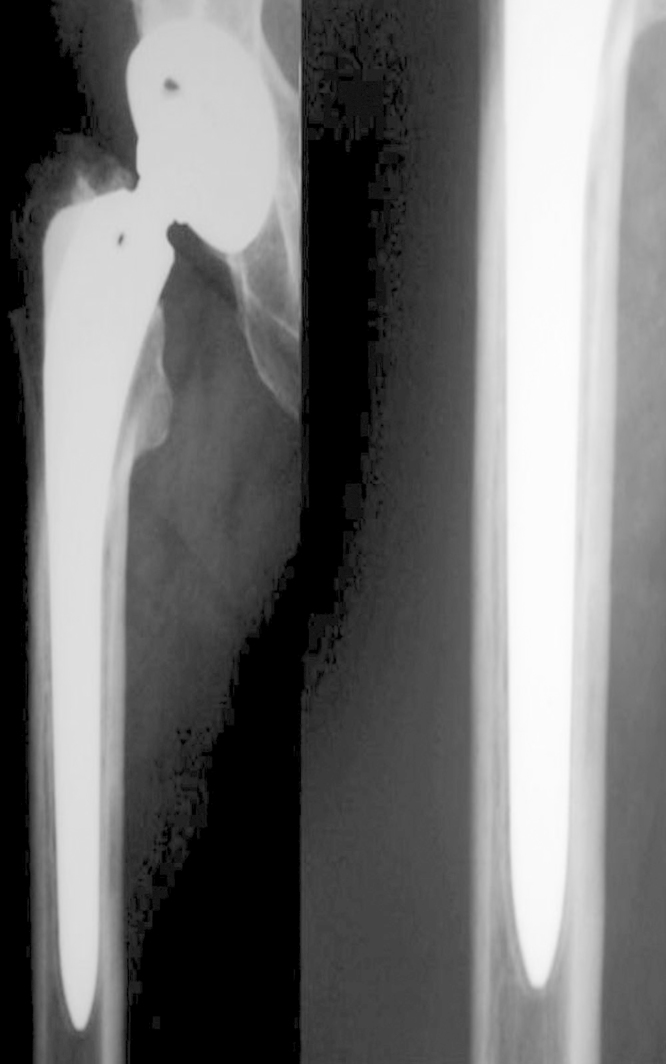
Intraoperative femoral fractures occurred in eight cases (9%), of which four were limited to the calcar region and underwent wire binding. In three cases, the fracture extended as far as the distal third of the femoral component. Only one of these underwent wire binding, while the other two were only noted during postoperative controls (Fig. 3). Despite the fractures, osseointegration of the femoral components occurred in these cases (Fig. 4).
Fig. 3.
Intraoperative femoral fracture identified on control radiographs: early postoperative period on the left and after 2.5 years on the left.
Fig. 4.
Reactive lines in the smooth portion of the osseointegrated femoral implant.
Discussion
With increasing life expectancy among the population and higher activity levels among patients with systemic diseases and elderly people, the number of hip arthroplasty procedures performed has been progressively increasing9 and is including patients with poor bone quality.
In our study, the means for the cortical index found in types A and B on anteroposterior radiographs were not considered to be different from those described by Dorr (Table 4). There was a significant difference (p = 0.01) between our mean and the mean demonstrated by Dorr only in relation to the cortical index of the anteroposterior view in type C. In the lateral radiographic view, the cortical index values were not considered to be statistically distinct from Dorr's values. This seems to us to be objective data that could be used in the future to compare results between different studies, given the possible subjectivity of the qualitative classification into types A, B and C.
Table 4.
Comparison between mean cortical indexes (CI) of the present study and those described by Dorr.
| Munif 2011 | Dorr 1993 | p | |
|---|---|---|---|
| CI | CI | ||
| Anteroposterior | |||
| Type A | 0.58 | 0.58 | 1 |
| Type B | 0.49 | 0.5 | 0.42 |
| Type C | 0.38 | 0.42 | 0.01 |
| Lateral | |||
| Type A | 0.48 | 0.48 | 1 |
| Type B | 0.41 | 0.39 | 0.18 |
| Type C | 0.28 | 0.3 | 0.21 |
Student's t test.
From a study on 90 THA procedures performed on patients over the age of 80 years, with between two and eleven years of follow-up, Keisu et al.6 reported that there were signs of osseointegration in all the patients. They did not note any difference between the 23 femurs classified as type C and the 67 type A or B.
Berend et al.10 evaluated 49 THA procedures in patients over the age of 75 years, with a mean follow-up of five years, and demonstrated comparable clinical and radiographic results for Dorr types A, B and C. In those results, cortical index measurements and the rates of osseointegrated components and components that were stable because of fibrous fixation were not taken into consideration.
Reitman et al.11 reported the results from 72 THA procedures performed on 62 patients aged over 65 years, with a mean follow-up of 13.2 years. They demonstrated that the results from osseointegration of the femoral nail in 33 femurs classified as Dorr type C did not differ from the results relating to types A and B. However, the authors reported that 19 patients were lost from the follow-up.
Kelly et al.12 demonstrated good results over nine to 14 years of postoperative follow-up on 15 patients with Dorr type C femoral morphology. These authors used an uncemented femoral component coated with hydroxyapatite.
Like the abovementioned studies, the present study did not show any difference in clinical results between the different femoral morphological types and was also not capable of proving any significant difference in the osseointegration rates seen through radiography, between the different Dorr types.
Our study was conducted on 87 consecutive THA procedures, without age limitations, which thus differed from the other studies cited. In our practice, there were non-elderly patients who presented type C morphology or low cortical index values. Eleven of the 18 type C femurs (61%) were in patients under the age of 60 years at the time of the surgery.
We did not find any difference in osseointegration rate between femurs that became fractured during the operation and those that did not become fractured. This finding corroborates the study by Badhe et al.,13 in which the rate of intraoperative fractures without displacement that were treated by means of cerclage was 13.7% and, likewise, no difference in osseointegration rate between femurs that became fractured during the operation and those that did not become fractured was found.
The survival results found for the femoral prostheses in the present study, with a mean follow-up of 2.8 years, may become modified over the long term. Kobayashi et al.7 studied 527 THA procedures to determine whether radiological evaluation performed two years after the operation could have predicted the long-term survival of the femoral component. These authors took the view that femoral components that did not present radiolucency lines of thickness greater than 2 mm or distal migration greater than 2 mm had a 6% possibility of aseptic loosening over a period of five to ten years.
Engh et al.5 reported that there was greater difficulty in radiologically identifying osseointegration in components with proximal porosity. They considered that presence of spot welds and absence of reactive lines in the porous region were the greatest signs of osseointegration. They also highlighted that implants with solely proximal porosity made it difficult to identify spot welds on radiographs.
Among the 86 femoral implants that were considered to have achieved osseointegration in our study, 16 did not present spot welds. In the type C femurs, 47% of the osseointegrated implants did not present spot welds on radiographs, which was a significantly higher rate than among the types A and B, which was 12%. We believe that the reduced bone density and lower osteoblastic activity found in type C may explain the lower frequency of bone bridges between the cortical bone and the implant that was seen on radiographs.
Eingartner et al.14 studied the Bicontact prosthesis and observed that migration greater than 2 mm in the first months did not impede osseointegration. In our study, the initial migration of the femoral component greater than 2 mm that was observed in 10 cases did not impede osseointegration of the femoral components. One of the femoral nails migrated 13 mm over the first three months, and thereafter stabilized. Over the sequential follow-up until 42 months after the operation, there was no additional change in position. At the last radiographic evaluation, there were signs of osseointegration, such as spot welds. The only component that did not osseointegrate underwent initial migration of 2 mm over the first three months, with subsequent fibrous stabilization.
The presence of reactive lines in femoral implants with proximal porosity has already been described in the literature15, 16 and is not a sign of loosening of the prosthesis (Fig. 4). These lines occur because there is a minimum degree of movement between the distal uncoated part of the prosthesis and the endosteum, as well as the difference in the modulus of elasticity between the prosthetic component and the femoral axis.17
Despite the short mean length of follow-up of our study (2.8 years), we consider that the limited number of patients lost from the follow-up (three patients; three hips; representing 3% of the THA procedures) was a positive factor. Moreover, none of the patients who were lost presented type C femoral morphology.
Conclusion
There were no significant differences in the results relating to conical uncemented femoral prostheses with proximal porosity, between femurs of different morphological type according to the Dorr classification. This conclusion might vary if another implant model were to be used and also over the course of postoperative follow-up on THA.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Ahmad Hatem A, Ferreira da Luz B, Nishimoto Nishi R, Gilberto Cimbalista de Alencar P. Avaliação dos resultados de componente femoral cônico de fixação proximal não cimentado em fêmur tipo C de Dorr. Rev Bras Ortop. 2014;49:260–266.
Work performed at Hospital de Clínicas, Universidade Federal do Paraná, Curitiba, PR, Brazil.
References
- 1.Lachiewicz P.F. Cement fixation of the femoral component in older patients. Instr Course Lect. 2008;57:261–265. [PubMed] [Google Scholar]
- 2.Dorr L.D., Faugere M.C., Mackel A.M., Gruen T.A., Bognar B., Malluche H.H. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231–242. doi: 10.1016/8756-3282(93)90146-2. [DOI] [PubMed] [Google Scholar]
- 3.Hagio K., Sugano N., Takashina M., Nishii T., Yoshikawa H., Ochi T. Embolic events during total hip arthroplasty an echocardiographic study. J Arthroplasty. 2003;18(2):186–192. doi: 10.1054/arth.2003.50027. [DOI] [PubMed] [Google Scholar]
- 4.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 5.Engh C.A., Massin P., Suthers K.E. Roentgenographic assessment of biological fixation of porous surfaced femoral components. Clin Orthop Relat Res. 1990;(257):107–128. [PubMed] [Google Scholar]
- 6.Keisu K.S., Orozco F., Sharkey P.F., Hozack W.J., Rothman R.H., McGuigan F.X. Primary cementless total hip arthroplasty in octogenarians. J Bone Joint Surg Am. 2001;83(3):359–363. doi: 10.2106/00004623-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi A., Donnelley W.J., Scott G., Freeman M.A. Early radiological observations may predict the long term survival of femoral hip prosthesis. J Bone Joint Surg Br. 1997;79(4):583–589. doi: 10.1302/0301-620x.79b4.7210. [DOI] [PubMed] [Google Scholar]
- 8.Gruen T.A., McNieice G.M., Amstutz H.C. Modes of failure of cemented stem type femoral component: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;(141):17–27. [PubMed] [Google Scholar]
- 9.Ostendorf M., Johnell O., Malchau H., Dhert W.J., Schrijvers A.J., Verbout A.J. The epidemiology of total hip replacement in the Netherlands and Sweden: present status and future needs. Acta Orthop Scand. 2002;73(3):282–286. doi: 10.1080/000164702320155257. [DOI] [PubMed] [Google Scholar]
- 10.Berend K.R., Lombardi A.V., Mallory T.H., Dodds K.L., Adams J.B. Cementless double-tapered total hip arthroplasty in patients 75 years of age and older. J Arthroplasty. 2004;19(3):288–295. doi: 10.1016/j.arth.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Reitman R.D., Emerson R., Higgins L., Head W. Thirteen year results of total hip arthroplasty using a tapered titanium femoral component inserted without cement in patients with type c bone. J Arthroplasty. 2003;18(7):116–121. doi: 10.1016/s0883-5403(03)00344-9. [DOI] [PubMed] [Google Scholar]
- 12.Kelly S.J., Robbins C.E., Bierbaum B.E., Bono J.V., Ward D.M. Use of a hydroxyapatite-coated stem in patients with Dorr Type C femoral bone. Clin Orthop Relat Res. 2007;(465):112–116. doi: 10.1097/BLO.0b013e318156bf96. [DOI] [PubMed] [Google Scholar]
- 13.Badhe N.P., Quinnell R.C., Howard P.W. The uncemented bi-contact total hip arthroplasty. J Arthroplasty. 2002;17(7):896–901. doi: 10.1054/arth.2002.34523. [DOI] [PubMed] [Google Scholar]
- 14.Eingartner C., Volkmann R., Heigele D., Weise K. Long-term results of an uncemented straight femoral shaft prosthesis. Hip Int. 2006;16(1):23–32. doi: 10.5301/hip.2008.5638. [DOI] [PubMed] [Google Scholar]
- 15.Mulliken B.D., Bourne R.B., Rorabeck C.H., Nayak N. Hip arthroplasty radiographic evaluation and stability a tapered titanium femoral stem inserted without cement in a total hip arthroplasty radiographic evaluation and stability. J Bone Joint Surg Am. 1996;78(8):1214–1225. doi: 10.2106/00004623-199608000-00012. [DOI] [PubMed] [Google Scholar]
- 16.McLaughlin J.R., Lee K.R. Total hip arthroplasty with an uncemented femoral component. Excellent results at ten-year follow-up. J Bone Joint Surg Br. 1997;79(6):900–907. doi: 10.1302/0301-620x.79b6.7482. [DOI] [PubMed] [Google Scholar]
- 17.Keisu K.S., Mathiesen E.B., Lindgren J.U. The uncemented fully textured Lord hip prosthesis: a 10- to 15-year followup study. Clin Orthop Relat Res. 2001;(382):133–142. doi: 10.1097/00003086-200101000-00020. [DOI] [PubMed] [Google Scholar]