Abstract
Objective
To quantify progress with the initiation of salt reduction strategies around the world in the context of the global target to reduce population salt intake by 30% by 2025.
Methods
A systematic review of the published and grey literature was supplemented by questionnaires sent to country program leaders. Core characteristics of strategies were extracted and categorised according to a pre-defined framework.
Results
A total of 75 countries now have a national salt reduction strategy, more than double the number reported in a similar review done in 2010. The majority of programs are multifaceted and include industry engagement to reformulate products (n = 61), establishment of sodium content targets for foods (39), consumer education (71), front-of-pack labelling schemes (31), taxation on high-salt foods (3) and interventions in public institutions (54). Legislative action related to salt reduction such as mandatory targets, front of pack labelling, food procurement policies and taxation have been implemented in 33 countries. 12 countries have reported reductions in population salt intake, 19 reduced salt content in foods and 6 improvements in consumer knowledge, attitudes or behaviours relating to salt.
Conclusion
The large and increasing number of countries with salt reduction strategies in place is encouraging although activity remains limited in low- and middle-income regions. The absence of a consistent approach to implementation highlights uncertainty about the elements most important to success. Rigorous evaluation of ongoing programs and initiation of salt reduction programs, particularly in low- and middle- income countries, will be vital to achieving the targeted 30% reduction in salt intake.
Introduction
Cardiovascular disease (CVD), the leading cause of death worldwide, kills 17 million people each year which represents 30% of all global deaths [1]. The major risk factor for cardiovascular disease is high blood pressure [1, 2], and excessive sodium intake is an important cause [3]. Sodium consumption of more than 2g/d is estimated to cause 1.65 million cardiovascular related deaths each year, representing around 1 of every 10 deaths from cardiovascular causes [4]. The World Health Organization (WHO) has recommended salt reduction as a ‘best buy’, recognising it as one of the most cost effective and feasible approaches to prevent non-communicable diseases (NCDs) [1].
A review of salt reduction strategies undertaken in 2010 identified 32 national salt reduction strategies worldwide [5]. Most were in Europe, followed by the Western Pacific Region and the Americas. Since the last review, a series of recent research reports have provided further support for salt reduction [3, 6–9] and while several widely critiqued observational analyses have contested the nature of the association between salt and vascular outcomes [10–13] the totality of the evidence supports efforts to achieve population-wide lowering of salt intake. Furthermore, the evaluation of the United Kingdom’s (UK) salt reduction strategy has highlighted feasibility, demonstrating a 15% reduction in population salt intake between 2003 and 2011 [14] with average blood pressure in the adult population falling by 3/1.4mm Hg over the same period [15].
In 2011, the United Nations (UN) General Assembly convened a High-Level Meeting to address the Prevention and Control of NCDs worldwide [16]. The General Assembly adopted the Political Declaration of the meeting, which committed all 193 member countries and states to the prevention and control of NCDs [17]. Subsequently, at the 66th World Health Assembly, WHO Member States adopted the global target of a 30% reduction in mean population intake of salt/sodium by 2025. This was one of nine voluntary global targets set to achieve an overarching 25% reduction in premature mortality from CVDs, cancer, diabetes and chronic respiratory diseases by 2025 [18]. Subsequently the WHO has supported Member States by identifying how best to develop, implement and monitor salt reduction strategies [19, 20] including consideration of how salt reduction and iodine deficiency elimination programs can be integrated [21]. A range of resources have been made available [22, 23]. Within this context we sought to systematically document existing national salt reduction strategies and provide an overview of initiatives in place to reduce population salt intake in line with the new global target.
Methods
Search Strategy
Salt reduction initiatives were identified from a search of peer-reviewed and grey literature published up to May 2014 as well as from salt reduction experts and country program leaders.
The retrieval and summary process was divided into 5 steps:
Conduct a systematic search of peer-reviewed and grey literature
Establish a database to systematically record initiatives according to a pre-defined framework
Consult with international salt reduction experts
Supplement and verify information through questionnaires sent to country program leaders
Analyse and compare the findings with a similar review that was conducted in 2010.
We searched the following databases: Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Public Health Group Specialized Register, MEDLINE, EMBASE, Effective Public Health Practice Project Database, Web of Science, TRoPHI databases and LILACS database [24]. A comprehensive list of search terms (S1 Annex) was used including ‘salt’, ‘sodium’, ‘government programs’ or ‘nutrition policy’. Titles and abstracts were screened independently by two reviewers and inconsistencies (few) were resolved via discussion.
In parallel, a search for pertinent grey literature using these terms was conducted in OpenGrey, Google, WHO and regional office databases and websites, governmental websites (e.g., Food Standards Agency, Public Health Agency of Canada, Centers for Disease Control and Prevention), scientific or non-governmental organization (NGO) websites (e.g., Institute of Medicine, Food Safety Authority of Ireland, Heart Foundation) and international or national salt reduction associations (e.g., World Action on Salt and Health).
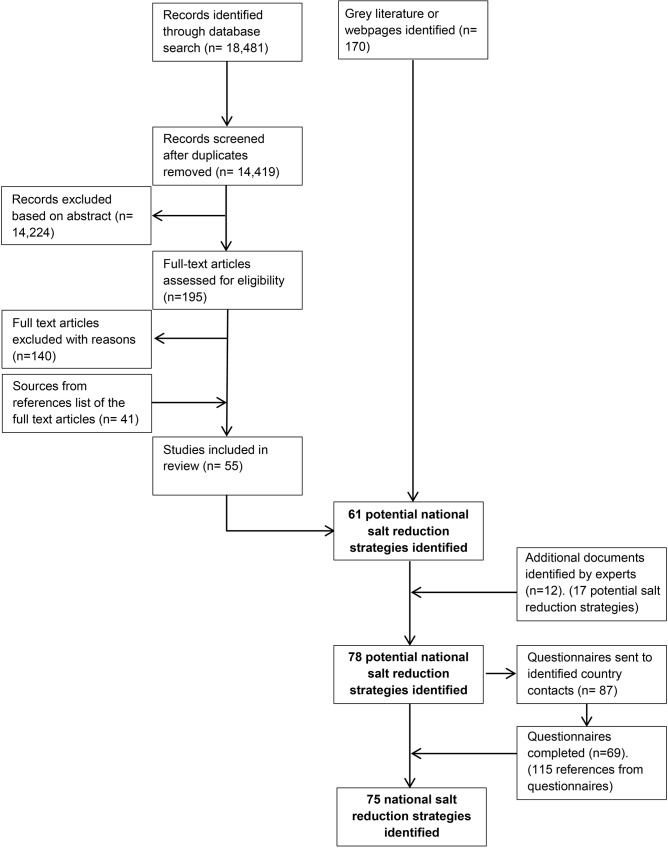
A database of initiatives was established based on this information. A list of countries identified as having salt reduction strategies was sent to international experts and WHO representatives to identify whether any other countries with strategies had been missed. The database was continuously updated with the information being received. A questionnaire for each national country program was prepared (S2 Annex) by pre-filling each questionnaire based on existing country information. The questionnaire was sent to 86 country program leaders identified through the expert review. Additional information gathered from the responses was used to update the database. Queries were followed up with country program leaders, the relevant WHO regional expert or a targeted search (Fig 1).
Fig 1. Identification process of national salt reduction strategies around the world.
Ethics Statement
Program leaders were informed of the purpose of the study through an introductory email sent with the questionnaire and consented to the information being used as part of the study through return of the questionnaire. University of Sydney Human Research Ethics Committee approval was granted for the questionnaire portion of this work (#14923).
Inclusion/Exclusion criteria
National strategies aiming to achieve population-wide reduction in salt intake were included. A national salt reduction strategy was defined as having government involvement with at least one of the following; a document and/or statement highlighting their commitment to population-level salt reduction OR a program of work to engage the industry to reduce salt in foods OR a campaign to change consumer knowledge, attitude & behaviour (KAB) specifically related to salt OR work aiming to reduce salt intake in public institution settings (e.g. government-funded schools, hospitals or workplaces). Initiatives that just provided information to consumers about salt as a part of a broader nutrition or health promotion campaign were excluded. National strategies were considered to be in their planning stages if initiatives were still being developed or if the strategic action plan had been developed but there was no evidence of program implementation.
Data extraction
For each country, standard information relating to the characteristics of the national salt reduction strategy was extracted based on a previous review [5]. However, to improve the understanding of how national salt reduction strategies have progressed, additional information was extracted regarding targets for salt levels within specific food types, salt taxes and work in public institution settings. Information on reported program impact based on population-level salt intake, salt levels in foods and consumer KAB outcome measures was also gathered (S3 Annex).
Analysis
Key characteristics for each national salt reduction strategy were entered in a database and examined in relation to: regional distribution as categorised by the WHO regions; income level classified by The World Bank; leadership and strategic approach; baseline monitoring data; types of implementation strategies; and evaluation of program impact. National strategies were classified as ‘strategy developed’, ‘strategy planned’ or ‘no strategy developed’ based on the strategies implemented and the country contact’s opinion. Where there were multiple sources of varying information, data was extracted from the source likely to be the most accurate or recent. A quantitative assessment of the percentage of countries reporting each characteristic was undertaken.
Where characteristics and information about the strategy were collected in both the current and previous 2010 review, there was a comparison to determine if there had been any changes.
Results
Sources of information
A total of 55 peer-reviewed articles and 170 grey literature documents and websites were retrieved from the literature search. An additional 115 documents were referenced in the completed questionnaires or obtained from a targeted search for more information to support questionnaire responses (Fig 1).
From the initial literature search, 61 countries with national salt reduction strategies were identified. International experts and WHO regional representatives provided 12 additional documents, which identified a further 17 potential national strategies. 87 questionnaires were sent to country program leaders and of these, 69 countries completed the questionnaire or provided relevant information. National salt reduction strategies were confirmed through 62 returned questionnaires and 7 confirmed there was no strategy or the strategy was still being planned. An additional 13 countries were considered to have a national salt reduction strategy based on information from peer-reviewed and grey literature despite not providing completed questionnaires.
Countries with national salt reduction strategies by WHO region
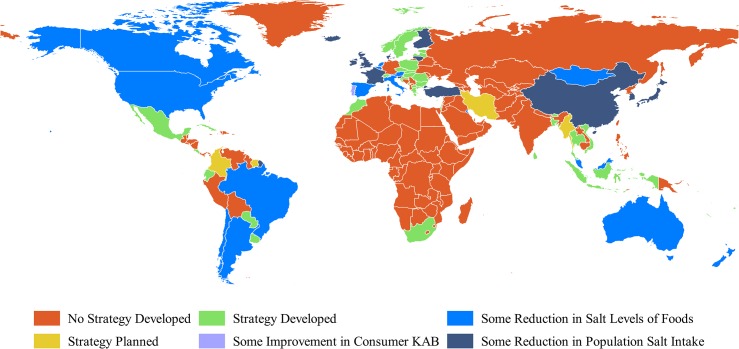
In all, 75 countries (includes territories and areas) with national salt reduction strategies were identified in 2014, which is more than double the 32 reported in 2010. An additional nine countries are currently in their planning stages. National salt reduction strategies are now being implemented in countries across all six WHO regions and there are one or more strategies in the South-East Asia, Eastern Mediterranean and African region, where there were none previously (Fig 2).
Fig 2. Countries’ reported progress towards reduction in population salt intake.
Made with Natural Earth. Free vector and raster map data @ naturalearthdata.com.
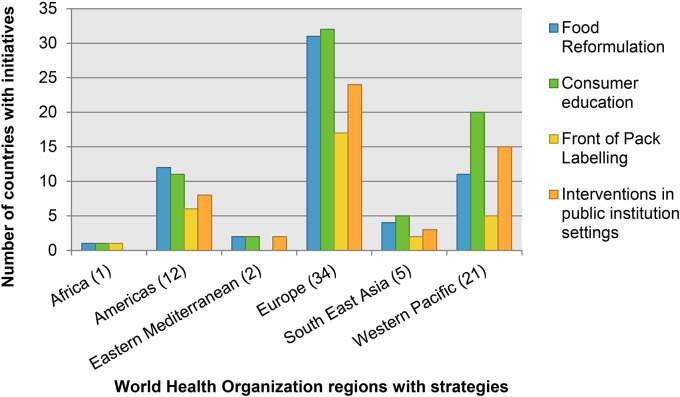
In all regions, consumer education was the most commonly used strategy followed by food industry engagement to reformulate products and FoPL schemes, except in the WHO Region of the Americas where industry engagement is the most commonly used strategy (Fig 3). The WHO South-East Asia Region is the only region where countries have not reported using voluntary or mandatory salt level targets to encourage reformulation (Fig 3).
Fig 3. Types of salt reduction initiatives adopted by countries.
Countries with national salt reduction strategies by income level
National salt reduction strategies are now implemented in countries at all income levels as classified by the World Bank [25]. National salt reduction strategies identified previously [5] were limited to high income (25) and upper middle income countries (7). However strategies now exist in 41 high income countries, 21 upper middle income countries, 11 lower middle income countries, and 1 low income country (as well as 1 country that is not classified).
Leadership and strategic approach
All strategies identified include some form of government involvement. However, 45 countries also report NGO, industry or other advocacy organization activity of which 9 acknowledged NGO or industry leadership. Three-quarters (57/75) of strategies have an established target for population salt intake, ranging from 5 to 8 grams per day. 38 countries have a target of 5 grams of salt per day, as recommended by WHO, 16 countries have a target of 6 grams per day and 3 have targets of more than 6 grams per day. The majority (72%) of national salt reduction strategies are linked to a broader initiative such as non-communicable disease or nutrition programs. There have been no significant changes in the leadership and strategic approach of national salt reduction strategies since the previous review in 2010.
Baseline assessment and monitoring
With regards to establishing a baseline, 60 countries have one or more estimates of population-level salt intake, approximately double the number of countries compared to 2010. 24-hour urine collection, regarded as the gold standard for assessing salt intake, has been carried out in 32 countries, while 42 have used dietary surveys including 24-hour dietary recall or food frequency questionnaires. 7 have used household budget surveys to estimate salt intake. Whilst dietary surveys are still the most common method of estimating population salt intake, there has been an increase from 7/32 (22%) to 32/75 (43%) in the use of 24-hour urine samples since the previous review. The most current reported salt intakes ranged from 5 grams in Cyprus measured by dietary survey in 2005–08 [26] to 15.3 grams in a province of Vietnam, measured by spot urine in 2012. Out of the 60 countries with data available, 27 reported mean salt intake levels equal to or greater than 10 grams (double the WHO recommended daily salt intake).
Data regarding the sodium content level of some foods or meals has been collected in 52 countries, an increase from 56% to 69% since the 2010 review. Sodium content data is collected through food composition databases, food analysis, industry self-reporting or shop surveys.
Of the 75 strategies identified, the proportion measuring KAB in relation to salt at baseline, increased substantially to 60% (45/75), compared to 13% (4/32) in the 2010 review. Most surveys included questions relating to knowledge of the adverse health effects of excessive salt intake, attitudes towards the importance of reducing salt or behaviour such as adding salt to food without tasting or cooking with low-salt products.
Implementation strategies
The main implementation strategies for salt reduction are food reformulation, consumer education, front of pack labelling, interventions in public institution settings (such as schools, hospitals and the workplace) and taxation (Table 1). Almost all countries are multifaceted in their approach, with 70/75 (93%) countries implementing or planning to implement more than one type of strategy. Additionally more countries are incorporating legislative initiatives (33/75) such as establishing maximum sodium content limits in foods, taxing high-sodium content products, mandatory FoPL schemes or warning labels for high salt foods and sodium content standards for publicly procured foods and meals (Table 2). So far, only two countries, South Africa and Argentina, have adopted comprehensive legislative schemes to limit salt levels in foods [27, 28].
Table 1. Baseline assessments and implementation strategies by WHO Region.
| Country | Monitoring | Implementation Strategies | ||||
|---|---|---|---|---|---|---|
| Baseline assessment | Salt intake (g/person/day) | Food reformulation | Consumer education | Front of Pack Labelling | Interventions in public institution settings | |
| World Health Organization African Region | ||||||
| Mauritius (P) [47] | SI/SL | 7.9 (2012 24h) | P | P | P | E/VG (sch/wk/ hosp) |
| South Africa [27, 48, 49] | SI/SL/KAB | 8.1 (2005 24h & DS) | T (M) | NGO | Logo (vol) | P |
| World Health Organization Region of the Americas[50, 51] | ||||||
| Argentina [52] | SI/SL/KAB | 11.2 (2011 24h) | T (vol/M) | Gov | No | E/PP/VG (sch/wk) |
| Barbados [20] | SI/SL/KAB | 12–15 (2010 unknown) | IM | Gov/ NGO | No | E/VG (sch/wk) |
| Brazil [53] | SI/SL/KAB | 11.8 (2002–3 & 2008–9 HS) | T (vol) | Gov | No | E/PP/VG (sch) |
| Canada [54] | SI/SL/KAB | 8.5 (2004 DS) a | T (vol) | Gov/ NGO | Logo (vol) | No |
| Chile [55] | SI/SL/KAB | 9.8 (2009–10 spot) | T (vol) | Gov | W (man) | E (sch) |
| Colombia (P) [56, 57] | SI b # | 11.8 (1988 24h) b | P | P | No | - |
| Costa Rica [58] | SI/SL/KAB | 9.3 (2004–5 HS) | IM | Gov | %DI (vol) | PP (sch) |
| Cuba | KAB | - | IM | Gov | - | PP (sch) |
| Ecuador [59] | SI/SL/KAB | 10 (DS) | T (vol) | - | TL (man) | - |
| Mexico | No | P | T (vol) | Gov | %DI (man) | PP (sch) |
| Paraguay [60] | SL/KAB | P | T (M) | Gov | No | E (sch/wk) |
| Suriname (P) [61] | No | P | - | Gov | P | - |
| United States [62–64] | SI/SL/KAB | 8.8 (2009–10 DS) | T (vol) | Gov/ NGO | % DI (vol) | E/PP/VG (sch/wk/ hosp) |
| Uruguay | SI/SL/KAB | 9.5 (2005–6 HS) | T (vol) | Gov | P | No |
| World Health Organization Eastern Mediterranean Region | ||||||
| Iran (P) [65] | SI b | 10.6 (2007 24h) b | P | Gov | No | E (sch) |
| Kuwait | SI/SL | 8.8 (m) 6.9 (w) (2010 DS) | T (Vol) | Gov | P | E/PP (sch/ wk/ hosp) |
| Morocco | SI/SL/KAB | Yes TBA (2013–14 24h & DS) | IM | NGO | P | No |
| World Health Organization European Region [26, 29] | ||||||
| Austria [66] | SI/SL/KAB | 8.7 (m) 7.6 (w) (2012 24h & DS) | T (vol) | Gov | No | VG (sch) |
| Belgium [67] | SI/SL/KAB | 10.45 (2009 24h) | T (vol/M) | Gov | Logo (vol) | No |
| Bulgaria | SI/SL/KAB | 13.8 (2004 DS) | T (vol/M) | Gov | %DI (vol) | PP (sch) |
| Croatia [68] | SI/SL | 12 (2010 DS) | T(vol)(bread) | Gov/ NGO | No | VG (sch) |
| Cyprus | SI | 5 (2005–8 DS) | IM | Gov | Yes (vol) | E (sch) |
| Czech Republic | SI/SL | 13.6 (2003–4 DS) | T (vol) | Gov | Logo (vol) | - |
| Denmark | SI/SL | 9.88 (m) 7.02 (w) (2010 median spot) | T (vol) | Gov | Logo (vol) | - |
| Estonia | SI/KAB | 10 (1997 DS) | P IM | Gov | %DI (vol) | PP (sch/ hosp) |
| Finland [69, 70] | SI/SL/KAB | 9 (m) 6.5 (w) (2012 DS) | T (vol) | Gov/ NGO | W (man) Logo (vol) | E/PP/VG (sch/ wk/hosp) |
| France [33] | SI/SL/KAB | 8.4 (2006–7 DS) | T (vol) | Gov | No | PP (sch) |
| Greece | SL/KAB | No | T (vol/M) | Gov | No | E/PP (sch) |
| Hungary [71] | SI/SL/KAB | 11.2 (m) 9.6 (w) (2010 24h) | T (vol/M) (bread) | Gov | Logo (vol) | PP (sch) |
| Iceland | SI | 9.5 (m) 6.5 (w) (2010–11 DS) | IM (bread) | Gov | - | - |
| Ireland [72] | SI/SL/KAB | 11.1 (m) 8.5 (w) (2008–10 DS & spot) a | T (vol) | Gov | %DI (vol) | E (sch) |
| Israel | SI/SL/KAB | 7 (1999–2001 DS) | T (vol) | Gov | P | E/PP (sch/ wk/ hosp) |
| Italy [73] | SI/SL/KAB | 10.6 (m) 8.2 (w) (2009–11 24h) | T (vol) | Gov/ NGO | No | P |
| Latvia [74] | SI/SL/KAB | 7.1 (2007 DS) | IM | Gov | %DI (vol) | PP (sch/ hosp) |
| Lithuania [75] | SI/SL/KAB | 8.75 (2007 DS) | T (vol) | Gov/ NGO | Logo (vol) | E/PP (sch) |
| Luxembourg | SI/SL | 9.1 (2007–8 DS) | IM | Gov | - | E (sch) |
| Macedonia | SI | 14 (2011 IE) | No | P | No | P |
| Malta [57] | SI b /KAB | 9.7 (1988 24h) b | P IM | Gov | No | P |
| Montenegro | No | P | IM | - | - | - |
| Netherlands | SI/SL/KAB | 10.7 (m) 7.8 (w) (2010 24h) | T (vol)/ T(M) (bread) | NGO/ Industry | Logo (vol) / %DI (vol) | VG (sch/ wk) |
| Norway | SI/SL/KAB | 10 (2010–11 DS) | IM | Gov | Logo (vol) | P |
| Poland | SI/SL/KAB | 10.9 (2009 IE) | T (vol) | Gov/ NGO | Logo (vol)/ GDA (vol) | E/VG (sch/ hosp) |
| Portugal [76] | SI/KAB/SL (bread) | 10.7 (2012 24h) | T (vol/M) (bread) | Gov | TL (M) | E/VG (sch/ wk) |
| Romania | SI | 11.25 (2010 DS) | IM | Gov | - | PP (sch) |
| Slovakia | SI | 9.5 (m) 6.5 (w) (2011 DS) | IM | NGO | No | - |
| Slovenia [77] | SI/SL/KAB | 11.3 (2012 24h) | T (vol) | Gov | - | E/PP (sch/ wk/ hosp) |
| Spain [78] | SI/SL | 9.7 (2009 24h) | T (vol) | Gov | No | PP (sch) |
| Sweden | SI/SL | 10–12 (2011 DS) | T (vol) | Gov | Logo (vol) | PP/VG (sch/ wk) |
| Switzerland [79] | SI/SL | 9.1 (2011 24h) | IM | Gov/ NGO | No | VG (sch/ wk/ hosp) |
| Turkey [31] | SI/SL | 15 (2012 24h) | T (vol) | Gov | Logo (P) | E/VG (sch/ wk/ hosp) |
| United Kingdom [80–82] | SI/SL/KAB | 8.1 (2011 24h) | T (vol) | Gov | TL (vol) /%DI (vol) | E/PP (sch) |
| World Health Organization South East Asia Region [83, 84] | ||||||
| Bangladesh | SI b /KAB | 10–11 (2012 24h) b | IM (NGO) | NGO | No | No |
| Bhutan (short term strategies) | No | No | No | Gov | No | E (sch) |
| Indonesia (P) | SI | 15 (2012 unknown) | IM | Gov/ NGO | %DI (vol)/ W (man) | P |
| Myanmar (Burma) (P) | SI | 6–8 (2012 unknown) | No | Gov | No | - |
| Sri Lanka | SI b /SL | 8.3; 8.9 (urban; rural 2012 24h) b | IM/ P T (M) | Gov | TL (P) | VG (wk/ hosp) |
| Thailand [85] | SI/SL | 10.8 (2009 DS) | IM | Gov | %DI (man) | E (sch/ hosp) |
| World Health Organization Western Pacific Region [86] | ||||||
| Australia [87, 88] | SI/SL/KAB | 8.9 (2011 24h) b | T (vol) | NGO | %DI/Logo (vol) | VG (sch/ wk/ hosp) |
| China [44] | SI/SL/KAB | 12 (2009 DS) | No | Gov | %DI (vol) | - |
| Confederation of Northern Mariana Islands (P) | No | No | No | Gov/ NGO | No | E/PP/VG (sch) |
| Cook Islands | SI/SL/KAB | Yes (2013–14 24h) | T (vol) | Gov | No | E/PP (sch/wk) |
| FSM | No | No | IM | Gov | No | E (sch/ wk/ hosp) |
| Fiji | SI/KAB | 9.4 (2012–13 24h) | T (vol) | Gov | P | E/VG (sch/ wk/ hosp) |
| French Polynesia | No | No | P | Gov | No | E (sch/ wk) |
| Guam (P) | No | P | P | Gov | P | P |
| Japan [43] | SI | 10.4 (2012 DS) | IM | Gov/ NGO | No | No |
| Kiribati (P) | SL | No | No | Gov | No | No |
| Korea [89] | SI/SL/KAB | 11.6 (2012 DS) | T (vol) | Gov | %DI (vol)/ TL (man) | E/PP (sch/wk) |
| Malaysia | SI/SL | 6.4 (2003 DS) | IM | Gov/ NGO | P | E/PP (sch/ hosp) |
| Marshall Islands | No | No | No | Gov | P | E/VG (sch) |
| Mongolia [90] | SI/SL/KAB | 11 (2011 24h) | T (vol) | Gov | - | E/VG (wk) |
| Nauru | No | No | No | Gov | No | E (sch) |
| New Caledonia | KAB | No | IM | Gov | No | E (sch/ hosp) |
| New Zealand [91] | SI/SL/KAB | 8.57 (2012 24h) | T(vol) (NGO) | Gov/ NGO | %DI/Logo (vol) | No |
| Palau | No | P | No | P | No | P |
| Samoa (P) | SI/SL/KAB | 6.9 (2013 24h) | P | Gov | P | P |
| Singapore [83, 92] | SI/SL/KAB | 8.3 (2010 24h) | IM | Gov/ NGO | Logo (vol) | E/VG (sch) |
| Solomon Islands | No | No | P | Gov | No | P |
| Tonga | No | No | P | Gov | No | E (sch) |
| Tuvalu | SL | P | No | Gov | No | E (sch) |
| Vanuatu (P) | SL | No | P | P | No | E (sch) |
| Vietnam | SI b /SL/KAB | 15.3 (2012 spot) b | P | Gov | No | E (sch) |
P–Planned; SI-population salt intakes; SL–salt level in foods; DS–dietary survey; HS–household survey; 24h–24 hour urines; spot—spot urines; IE–indirect estimate of salt intake; KAB—consumer knowledge, attitude or behaviour; m–men; w—women
a includes discretionary salt
b not nationally representative
T—sodium content targets for foods; IM—industry meetings; Vol—voluntary; M–mandatory; NGO—non-governmental organization; Gov–government; %DI—percentage daily intake labelling (or Guideline daily amount in some countries); TL—traffic light labelling; W—high salt warning labels; E—education; PP—food procurement policy with sodium standards; VG—voluntary guidelines for sodium in foods; Sch—school settings; Wk—workplace settings; Hosp—hospital settings.
Dashes (-) indicate not aware of program. Each country’s population salt intake listed is based on the most current nationally representative assessment where available.
Table 2. Countries with legislative action on salt reduction.
| Mandatory Salt Targets | Argentina (most foods) [28], Belgium (bread) [29], Bulgaria (bread, milk products, meat products & lutenica) [29], Greece (bread, tomato products) [29], Hungary (bread) [29], Netherlands (bread) [29], Paraguay (bread) [60], Portugal (bread) [29], South Africa (most foods) [27] |
| Taxation on high salt foods | Fiji (tax on MSG), Hungary [29], Portugal [29] |
| Regulation on Front of Pack Labelling | Chile [51], Ecuador [51], Finland [29], Indonesia [93], Korea (on children’s foods) [94], Mexico [51], Portugal [76],Thailand (on 5 snack food categories) [94] |
| Standards for salt as part of procurement policies in public institution settings | Argentina, Brazil, Bulgaria [95], Cook Islands, Costa Rica [58], Estonia [95], Finland, France, Greece, Hungary, Israel, Korea, Kuwait, Latvia [95], Lithuania, Malaysia, Mexico, Romania, Slovenia, Spain [96], Sweden, USA [97], UK [98] |
Food Reformulation
Like the previous review, a high majority (81%) of national salt reduction strategies include industry engagement to reduce the salt content of products. Globally, bread is the most targeted food for reformulation followed by foods such as bakery products, processed meats, dairy products, sauces and convenience meals. 36 countries have taken the next step to establish voluntary sodium content targets for foods and meals. Furthermore, nine countries have mandated maximum sodium content limits for products. Whilst these are mostly for bread, Argentina, Bulgaria, Greece and South Africa have additional limits for other foods.
Consumer education
Raising consumer awareness and education in relation to salt is still part of most strategies. All except four countries have consumer education campaigns, 50 of which are led solely by government, 16 by both government and NGO or industry and 5 led solely by NGOs. In almost all cases, consumer awareness and education activities are used in conjunction with other salt reduction intervention strategies.
Front of Pack Labelling
A total of 31 countries (compared to 10 in 2010) have voluntary or mandatory FoPL schemes related to salt or sodium. Of those, eight countries have mandatory FoPL schemes. The most frequently used FoPL scheme are logos and symbols (19), which also includes traffic light labels (4), to indicate that the product meets established nutrient criteria. The second most commonly used FoPL scheme is the percentage daily intake (%DI) or guideline daily amount (%GDA), adopted by 16 countries. Three countries have warning labels on high salt foods. FoPL schemes have been introduced by government, NGO and industry.
Interventions in public institution settings
National salt reduction strategies involving activities that target public institution settings such as schools, workplaces, public hospitals and other public institutions were identified in 43 countries. This information was not previously reported in 2010 and does not take into account the fact that in some countries, state or local governments would have jurisdiction over this. Many of these activities are education programs; however a high proportion of countries (37/43) have nutrition guidelines for foods and meals sold and served in public settings, particularly schools and hospitals. 19 countries have voluntary nutrition guidelines and 23 have mandatory nutrition standards (including sodium) for foods and meals procured in public settings.
Taxation. Three countries; Fiji, Hungary and Portugal have adopted a tax related to salt. Two have a specific sodium tax and the third has a general tax. Fiji has a tax on monosodium glutamate (MSG) which it increased from 5% to 32% in 2012 [29]. Similarly, Hungary introduced a public health product tax on an extensive range of pre-packaged foods with high salt and sugar contents in 2011. The tax applies to products such as salty snacks with salt content above 1 gram per 100 grams, condiments with more than 5 grams per 100 grams and flavourings above 15 grams per 100 grams [29]. Portugal has a valued-added tax (VAT) on processed or packaged foods in general which covers foods high in salt, compared to a reduced VAT for non-processed foods [29].
Reported Program impact
Change in population salt intake
12 countries have reported a reduction in population salt intake (Table 3). This is an increase from four countries identified in 2010. Moreover, three of the four countries (Finland, Japan and UK) that reported reductions in 2010 are reporting further reductions [14, 30]. Countries reported using different methods to monitor changes in sodium intake which may affect the strength of the evidence for reductions. Slovenia, Turkey and the UK reported salt intake reductions of 9%, 16% and 15% respectively, based on 24 hour urinary excretion measurements [14, 31]. Finland monitored population salt intake through both 24 hour urine collection (FINRISK) and dietary surveys (FINDIET surveys) [30]. Denmark monitored population salt intake from spot urine sodium to predict 24 hour sodium excretion [32]. The remaining countries used comparative dietary surveys to estimate change in salt intake. Reductions ranged from approximately 5% in France between 1999 and 2007 to 36% in Finland between 1979 and 2007 [30, 33]. For some countries such as China, Turkey and Lithuania, the baseline and follow-up data points do not align closely with the salt reduction implementation dates and therefore it is difficult to conclude that reductions were due to the interventions.
Table 3. Countries that have reported a reduction in population salt intake.
| Country | Measurement tool | Reduction in population salt intake | Timescale |
|---|---|---|---|
| China[45] | Dietary survey | 28.8% (16.8g to 12g) | 1991–2009 |
| Denmark | Spot urine | 7% (10.68g(m),7.51g(w) to 9.88g(m), 7.02g(w)) (Median salt intake) | 2006–2010 |
| Finland[30] | Mixed (dietary survey & 24hr urine) | 36% (13g(m),11g(w) to 8.3g(m),7g(w)) | 1979–2007 |
| France[33] | Dietary survey | 4.9% (8.1g to 7.7g) | 1999–2007 |
| Iceland[26] | Dietary survey | 6.0% (8.4g to 7.9g) | 2002–2010 |
| Ireland[99] | Dietary survey | 13.6% (8.1g to 7g) | 2001–2011 |
| Japan | Dietary survey | 23.0% (13.5g to 10.4g) | 1997–2012 |
| Korea | Dietary survey | 13.6% (13.37g to 11.55g) | 2005–2012 |
| Lithuania [75] | Dietary survey | 18.6% (10.75g to 8.75g) | 1997–2007 |
| Slovenia | 24hr urine | 8.9% (12.4g to 11.3g) | 2007–2012 |
| Turkey [31] | 24hr urine | 16.7% (18.01g to 15g) | 2008–2012 |
| UK [14] | 24hr urine | 14.7% (9.5g to 8.1g) | 2001–2011 |
Change in sodium content of foods
19 countries reported a change in salt levels in foods and meals in 2014 compared to 4 in 2010. Brazil and Kuwait have recently reported reductions in addition to the 17 countries previously recorded [34]. Changes in sodium content were measured by laboratory analyses in 12 countries, product label survey in two, industry self-report in three and both industry self-report and label survey in two countries. All countries except Malaysia reported that sodium content had declined in bread, with reductions ranging from 6% to 38%. 11 countries also reported that sodium content had declined in other foods such as processed meats, cheese, breakfast cereals, sauces, convenience and ready meals.
Change in consumer knowledge, attitudes and behaviour in relation to salt
Improvement in consumer KAB in relation to salt was reported in seven countries compared to two in 2010 (Table 4). All countries measured changes based on surveys either self- completed or in an interview.
Table 4. Examples of changes in consumer knowledge, attitudes and behaviour in relation to salt.
| Country | Method of assessment | Improvements in consumer KAB |
|---|---|---|
| Ireland[100] | Consumer Survey | Behaviour- 37% of adults claimed they had changed behaviour as a result of the Salt Heart Campaign. 25% of adults claimed they changed their behaviour as a result of the ‘Already salted campaign'. |
| Korea | National Health and Nutrition Survey | Attitude- reported an increased interest in sodium in consecutive years based on the NHNS |
| Netherlands | Consumer Survey | Attitude- an increased number of people reported paying attention to the salt content of foods between 2008 and 2011 |
| Portugal[101] | Survey | Knowledge & behaviour- the number of people who were aware of the risks of excessive salt intake increased from 29% in 2007 to 72% in 2009 |
| Singapore[102] | Survey | Behaviour- the number of people NOT adding salt or sauce to food at the table increased from 39.8% in 1998 to 72.4% in 2010. |
| Slovenia | Computer Assisted Telephone Interviewing | Knowledge- the proportion of respondents who believe their daily consumption of salt is too high raised between April 2010 and February 2011 |
| United Kingdom[81] | Survey | Behaviour- the number of adults claiming to make a special effort to reduce salt increased from 34% in 2004 to 43% in 2009 |
Discussion
The number of countries with national salt reduction strategies has more than doubled since the previous review in 2010 with programs now implemented in countries across all WHO regions and across countries with a broad range of income levels. Whilst some of the additional 44 countries identified by this review may have commenced planning and activities prior to 2010, the majority (33/44) report start dates from 2010 onwards. This suggests significant impact has accrued through the recent efforts to expand the programs, driven by the World Health Organisation.
However, whilst the range of countries with programs in place has increased there remains marked variation in penetration across WHO regions with almost two-thirds of the European Region, but only 10% and 2% of the Eastern Mediterranean and African Region active. The coordinated actions of regional agencies such as the European Salt Action Network (ESAN) and the Pan American Health Organization (PAHO) were a likely key factor in the 80% increase and doubling of strategies in the European and Americas regions, respectively. Likewise the tripling of activity in the WHO Western Pacific Region reflects concerted WHO efforts. Additional support is now most urgently required in the Eastern Mediterranean and African regions where country engagement remains very low.
At present 33 low- and middle-income countries have a national salt reduction strategy in place, an increase from 7 in the previous report. The promotion of salt reduction as a ‘best buy’—an intervention that is not only cost-effective but also affordable, feasible and culturally acceptable to implement in any resource setting [1]–makes it a particularly compelling proposal for lower income settings. There is also potentially enormous impact of salt reduction in countries where there is a high salt intake combined with a very large population such as China and India.
Increased legislative initiatives
There has been a shift from solely voluntary initiatives to incorporating a legislative or fiscal component (Table 2). In 2010, very few countries had mandatory levels for salt and only in a limited number of food products. South Africa and Argentina have led with the development of much more extensive schemes [27, 28]. Three salt-related taxes and six (of eight) mandatory FoPL schemes that include labelling of salt have also been recently implemented. Direct evaluation of the efficacy of these schemes is awaited but modelling studies consistently suggest that legislative action will be much more effective [35]. Robust monitoring and evaluation plans built into these programs from the start will be key to determining their utility and making the case for their more widespread use [34, 36].
Many countries are now reporting food procurement policies which incorporate salt standards for foods in public institution settings such as public schools and hospitals, as part of their national salt reduction strategies. A separate review of healthy food procurement policies has demonstrated positive impact in relation to availability and selection of healthy food [37] but further research is required to understand how such policies can be best used to lower population salt intake. This should include examination of the extent to which they can be used, not only to improve the nutritional composition of foods served but also in terms of the potential to generate an increased demand for healthier (low-sodium) foods.
Approaches to monitoring
Implementing clear monitoring approaches is vital to demonstrate program effectiveness, but it also encourages greater change, particularly for voluntary strategies [34]. More countries have established mechanisms for monitoring of population salt intake levels, sodium content in foods and salt-related KAB but the quality of approaches vary.
Comparative dietary surveys were used in over half of the countries that reported reductions in population salt intake. Whilst this approach is likely to underestimate salt intake, if the method of measurement is consistent, it is still a useful measure of change over time [38, 39]. Additionally it can provide information about sources of sodium in the diet. Although 24 hour urine sodium excretion is considered the gold standard, it can be costly and a high burden on participants, which is challenging for many countries to adopt [20]. The use of spot urine measurements to estimate 24 hour urinary sodium excretion may therefore be more appropriate for large population surveys [39] and WHO has produced guidance for monitoring salt intake as part of STEPS that countries should follow [20]. This includes undertaking spot urine samples for the whole sample and 24 hour urine samples for a sub-sample of the population where possible, as well as standard questions for assessing and monitoring changes in KAB [40].
Standardised comparable approaches to measuring salt levels in foods are also vital. Almost two-thirds of countries monitoring change in salt levels in one or more food categories are using laboratory analysis which is likely to be very accurate but often covers a limited range of products rather than reflecting the whole food supply. Comprehensive surveys of salt levels in foods based on reported product label data should be considered in parallel to ensure that progress is made across a larger scale [34].
Countries reporting an impact
Whilst 29 countries have reported an impact in relation to one or more of the outcome measurements, the different monitoring approaches means that the strength of the evidence varies. All but one of the programs reporting an impact to date are voluntary, however this is likely due to the fact that most legislative approaches to salt reduction are relatively new and there has been insufficient time to measure an impact. The exception is Finland, where the 36% reduction in population salt intake is partially attributed to its mandatory warning labels on high salt foods established in 1993, which led to significant reformulation of foods [26, 41].
Engagement with food industry including the establishment of specific salt targets for a range of foods is a key element of 10 out of the 12 countries that have reported a reduction in population salt intake.
The two countries which did not prioritise engagement with the food industry were Japan and China, where processed foods are not the major source of sodium in the diet. In Japan, most of the sodium in the diet comes from soy sauce added during cooking or eating, followed by salted vegetables and miso soup [42]. Therefore salt reduction efforts have been focused on improving people’s understanding of salt and health through public education and consumer awareness campaigns [43]. Likewise in China, the main approach has been through national and regional educational campaigns [44]. However, it is unlikely that these educational programs are the major cause of reduction in salt intake in China. Changes in the diet and food environment associated with modernization during this period, such as refrigeration and advancements in transport has led to a reduction in preservation and pickled food consumption, which is more likely to contribute to the reduction in salt intakes [45]. Research currently underway to look at the potential use of salt substitutes in China [46] is likely to provide a more viable approach to salt reduction in China, as well as being more effective in countries where the main source of sodium in the diet is salt added during cooking and at the table including Vietnam, Thailand and India.
The use of education campaigns is a key element of almost every salt reduction strategy and common to all strategies reporting a reduction in salt intake to date. Whilst the quality of the before and after surveys used in the seven countries reporting improved consumer KAB is not clear and likely to be subject to self-report bias, if the surveys are consistent, it can be a useful measure for change [39].
Strengths and Limitations
This is the first comprehensive review of countries’ progress towards achieving the new global target for salt reduction. Questionnaires were sent to countries identified as having salt reduction initiatives and/or a country salt reduction contact person through a literature search and regional WHO representatives and experts. Although not all country contacts could be identified and there were some non-respondents, it is unlikely any major salt reduction initiatives were missed. The comprehensive database of national salt reduction initiatives and country contacts established as a result of this review will enable us to regularly update the information in future.
Much of the information was obtained from country questionnaires which relied on the knowledge and potentially subjective opinion of one country representative, usually from a government agency. Other stakeholders that often play an important role in salt reduction efforts, such as NGOs and industry organisations, were not requested to complete the questionnaire. Subsequent reviews of this kind might consider consulting with a wider range of stakeholders. However, in many cases, the questionnaire respondent acknowledged consulting other relevant people therefore initiatives are not likely to have been overlooked.
Similarly, whilst it is recognised that sub-national governments are implementing salt reduction strategies in their local jurisdiction, particularly healthy food procurement policies in public institution settings, this was not included as the review focused on national strategies. A review of sub-national salt reduction efforts and their impact would be useful to understand their contribution.
A key strength of this review is the systematic and comprehensive method of data collection. Although some salt reduction activities may have been missed in the previous review as it was not as comprehensive, an assessment of available start dates shows this did not affect the comparison of salt reduction strategies over time. The questionnaire was based on pre-defined categories from a previous review but expanded to encompass new elements of salt reduction strategies reflecting advancements on this issue. Future reviews should also include questions about national strategies to reduce iodine deficiency in view of the need to ensure that the two programs are effectively co-ordinated.
Whilst a key strength of the review is the fact that it encompasses a comprehensive search of the grey literature including government reports, presentations or questionnaires completed by country program officers, a parallel limitation of this is that the methodological rigor behind some of the reports is unknown. In particular, the robustness of the studies used as the basis for reported reductions in salt intake, salt levels in foods or changes in consumer KAB were not assessed and therefore should be interpreted with caution. The primary objective of this study was to provide a comprehensive overview of reported activity. A parallel Cochrane review of national salt reduction interventions currently underway will focus on the impact of the interventions [24]. The two studies taken together will add considerably to the body of evidence on the effectiveness and characteristics of national salt reduction programs.
Conclusion
Population salt reduction is considered as a ‘best buy’ intervention for the prevention of NCDs [1] and this review exemplifies that countries of all regions and income levels are able to implement such programs. The significant increase in number of national salt reduction strategies and countries reporting an impact in relation to one or more outcome measures represents some progress towards the global salt target. However the scope of some existing salt reduction initiatives need expanding and more robust monitoring is required to ensure strategies are having optimal impact. Rigorous evaluation will also explain which elements are important to the success of programs as currently the implementation of initiatives is varied.
Our results also highlight less than half of the programs are implemented in LMICs. Urgent action is required to address this given that 80% of NCD deaths occur in LMICs [1]. Furthermore, it is projected that the greatest increases in NCDs will be in the WHO regions of Africa, South-East Asia and the Eastern Mediterranean [1]—the three regions currently with the least salt reduction activity. Increased support to implement salt reduction strategies in LMICs and robust evaluations of ongoing programs is imperative to ensure the targeted 30% reduction in mean population salt intake is achieved by 2025, which in turn will prevent millions of deaths worldwide.
Supporting Information
(DOC)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The authors would like to thank national country contacts who responded to the questionnaires and provided additional information. We would also like to thank the World Health Organization staff and international experts who helped to identify initiatives and facilitate introductions to country contacts including Godfrey Xuereb, Peter Hoejskov, Temo Waqanivalu, Cherian Varghese, Chandralall Sookram, Fabienne Meier, Feisul Mustapha, Graham McGreggor, Claire Farrand, Kat Jenner and Victoria Targett. Jennifer McCrea-Logie and Sheila Penney from the Public Health Agency of Canada provided a very useful initial database which informed this work.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
BN is supported by an Australian Research Council Future Fellowship (DP100100295) and a National Health and Medical Research Council of Australia Senior Research Fellowship (APP100311). BN works within a NHMRC Centre for Research Excellence (APP1041020) and holds an NHMRC Program Grant (APP1052555). ED is supported by a NHMRC Sidney-Sax Overseas Fellowship. NC is supported by the Heart and Stroke Foundation of Canada, Canadian Institute for Health Research Chair in Hypertension Prevention and Control. LM is supported by a Population Health Investigator Award from Alberta Innovates—Health Solutions (until June 2014) and an Applied Public Health Chair from the Canadian Institutes of Health Research, the Public Health Agency of Canada, and Alberta Innovates—Health Solutions (starting October 2014). LM's work on this project was supported in part by an operating grant from the Canadian Institutes of Health Research, Ref # SOK-116970. JW is supported in her work on salt reduction through a National Health and Medical Research Council (NHMRC) and National Heart Foundation Career Development Fellowship. JW also gratefully acknowledges additional funding for work on salt reduction from the World Health Organization, the NHMRC and the Victorian Health Promotion Foundation throughout the period of this study.
References
- 1.World Health Organization. Global status report on noncommunicable diseases 2010. 2010 [cited 2014 30 September]. Available: http://whqlibdoc.who.int/publications/2011/9789240686458_eng.pdf?ua=1.
- 2. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2013;4:CD004937 10.1002/14651858.CD004937.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global Sodium Consumption and Death from Cardiovascular Causes. New Engl J Med. 2014;371(7):624–34. 10.1056/NEJMoa1304127 [DOI] [PubMed] [Google Scholar]
- 5. Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. J Hypertens. 2011;29(6):1043–50. 10.1097/HJH.0b013e328345ed83 [DOI] [PubMed] [Google Scholar]
- 6. Suckling R, He F, Markandu N, MacGregor G. Modest Salt Reduction Lowers Blood Pressure and Urinary Albumin Excretion In Impaired Glucose Tolerance and Type 2 Diabetes. J Hypertens. 2010;28:e219 10.1097/01.hjh.0000378867.74072.1c [DOI] [PubMed] [Google Scholar]
- 7. Weir MR, Yadao AM, Purkayastha D, Charney AN. Effects of High- and Low-Sodium Diets on Ambulatory Blood Pressure in Patients With Hypertension Receiving Aliskiren. J Cardiovasc Pharm T. 2010. December 1, 2010;15(4):356–63. 10.1177/1074248410377173 [DOI] [PubMed] [Google Scholar]
- 8. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. [Journal Article]. 2013. 2013-04-04 22:56:59;346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. He FJ, MacGregor GA. Reducing Population Salt Intake Worldwide: From Evidence to Implementation. Prog Cardiovasc Dis. 2010;52(5):363–82. 10.1016/j.pcad.2009.12.006 [DOI] [PubMed] [Google Scholar]
- 10. Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of Urinary Sodium and Potassium Excretion with Blood Pressure. New Engl J Med. 2014;371(7):601–11. 10.1056/NEJMoa1311989 [DOI] [PubMed] [Google Scholar]
- 11. O'Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, et al. Urinary Sodium and Potassium Excretion, Mortality, and Cardiovascular Events. New Engl J Med. 2014;371(7):612–23. 10.1056/NEJMoa1311889 [DOI] [PubMed] [Google Scholar]
- 12.Campbell NRC, Lackland DT, Niebylski ML, Nilsson PM. Is Reducing Dietary Sodium Controversial? Is It the Conduct of Studies With Flawed Research Methods That Is Controversial? A Perspective From the World Hypertension League Executive. The Journal of Clinical Hypertension. 2014. [DOI] [PMC free article] [PubMed]
- 13. Sodium and Cardiovascular Disease. New England Journal of Medicine. [Correspondence]. 2014;371(22):2134–9. [DOI] [PubMed] [Google Scholar]
- 14. Sadler K, Nicholson S, Steer T, Gill V, Bates B, Tipping S, et al. National Diet & Nutrition Survey—Assessment of dietary sodium in adults (aged 19 to 64 years) in England, 2011 Department of Health; 2011. [cited 2014 29 October]. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213420/Sodium-Survey-England-2011_Text_to-DH_FINAL1.pdf. [Google Scholar]
- 15. He FJ, Pombo-Rodrigues S, MacGregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014. April 1, 2014;4(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Health Organization. United Nations high-level meeting on noncommunicable disease prevention and control: NCD summit to shape the international agenda World Health Organization; 2011. [cited 2014 21 August]. Available: http://www.who.int/nmh/events/un_ncd_summit2011/en/. [Google Scholar]
- 17.United Nations, General Assembly. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases, A/66/L.1 (16 September 2011). 2012 [cited 2014 21 August]. Available: http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf?ua=1.
- 18.Sixty-sixth World Health Assembly. Follow-up to the Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases WHA 66.10. 2013 [cited 2014 21 August]. Available: http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_R10-en.pdf.
- 19.World Health Organization. Creating an enabling environment for population-based salt reduction strategies. Switzerland2010 [cited 2014 30 October]. Available: http://whqlibdoc.who.int/publications/2010/9789241500777_eng.pdf.
- 20. World Health Organization. Strategies to monitor and evaluate population sodium consumption and sources of sodium in the diet- report of a joint technical meeting convened by WHO and the Government of Canada Canada, October 2010. Canada: World Health Organization,; 2011. [cited 2014 30 October]. Available: http://whqlibdoc.who.int/publications/2011/9789241501699_eng.pdf. [Google Scholar]
- 21.World Health Organization. Salt reduction and iodine fortification strategies in public health: report of a joint technical meeting convened by the World Health Organization and The George Institute for Global Health in collaboraton with the International Council for the Control of Iodine Deficiency Disorders Global Network. Sydney, Australia: World Health Organization; 2013 [cited 2014 29 October]. Available: http://apps.who.int/iris/bitstream/10665/101509/1/9789241506694_eng.pdf?ua=1.
- 22. World Health Organization, The George Institute for Global Health. Salt matters for Pacific Island countries- Mobilizing for effective action to reduce population salt intake in Pacific island countries World Health Organization; 2014. [cited 2014 28 November]. Available: http://www.wpro.who.int/southpacific/entity/publications/salt-matters-publication.pdf?ua=1. [Google Scholar]
- 23. World Health Organization. Population sodium reduction strategies Geneva: World Health Organization; 2014. [cited 2014 30 October]. Available: http://www.who.int/dietphysicalactivity/reducingsalt/en/index1.html. [Google Scholar]
- 24. Mclaren L, Sumar N, Lorenzetti DL, Campbell N, McIntyre L, V. T. Population-level interventions in government jurisdictions for dietary sodium reduction (Protocol). Cochrane Database Syst Rev. 2012(10): doi: 1002/14651858.CD010166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The World Bank Group. Country and Lending Groups. The World Bank Group,; 2014 [cited 2014 23 September]. Available: http://data.worldbank.org/about/country-and-lending-groups#High_income.
- 26. World Health Organization. Mapping salt reduction initiatives in the WHO European Region Copenhagen: WHO Regional Office for Europe; 2013. [cited 2013 29 October]. Available: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/publications/2013/mapping-salt-reduction-initiatives-in-the-who-european-region. [Google Scholar]
- 27.South Africa Government. Government Gazette: NO. R. 214 Foodstuffs, Cosmetics and Disinfectants Act, 1972 (Act 54 of 1972) Regulations Relating to the Reduction of Sodium in Certain Foodstuffs and Related Matters. Heart Foundation; 2013 [cited 2014 7 April]. Available: http://www.heartfoundation.co.za/sites/default/files/articles/South%20Africa%20salt%20legislation.pdf.
- 28.Ministerio de Salud. ALIMENTOS Ley 26.905 Consumo de sodio. Valores Máximos.: Ministerio de Salud,; 2014 [cited 2014 8 May]. Available: http://www.msal.gov.ar/ent/images/stories/programas/pdf/2014-08_Ley26905-Ley-Sodio.pdf.
- 29.European Commission. Survey on Members States'- Implementation of the EU Salt Reduction Framework. 2013 [cited 2013 21 October]. Available: http://ec.europa.eu/health/nutrition_physical_activity/docs/salt_report1_en.pdf.
- 30. Pietinen P, Paturi M, Reinivuo H, Tapanainen H, Valsta LM. FINDIET 2007 Survey: energy and nutrient intakes. Public Health Nutr. 2010. June;13(6A):920–4. 10.1017/S1368980010001102 [DOI] [PubMed] [Google Scholar]
- 31. World Health Organization. Progress in reducing salt consumption in Turkey World Health Organization; 2013. [cited 2014 13 January]. Available: http://www.euro.who.int/en/countries/turkey/news/news/2013/04/progress-in-reducing-salt-consumption-in-turkey. [Google Scholar]
- 32. European Commission. National Salt Initiatives: Implementing the EU Framework for Salt Reduction Activities European Commission,; 2009. [cited 2014 21 October]. Available: http://ec.europa.eu/health/ph_determinants/life_style/nutrition/documents/national_salt_en.pdf. [Google Scholar]
- 33. European Commission. Collated information on salt reduction in the EU European Commission,; 2008. [cited 2014 21 October]. Available: http://ec.europa.eu/health/ph_determinants/life_style/nutrition/documents/compilation_salt_en.pdf. [Google Scholar]
- 34. Webster J, Trieu K, Dunford E, Hawkes C. Target Salt 2025: A Global Overview of National Programs to Encourage the Food Industry to Reduce Salt in Foods. Nutrients. 2014;6(8):3274–87. 10.3390/nu6083274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cobiac LJ, Vos T, Veerman JL. Cost-effectiveness of interventions to reduce dietary salt intake. Heart. [Research Support, Non-U.S. Gov't]. 2010. December;96(23):1920–5. [DOI] [PubMed] [Google Scholar]
- 36. Charlton K, Webster J, Kowal P. To Legislate or Not to Legislate? A Comparison of the UK and South African Approaches to the Development and Implementation of Salt Reduction Programs. Nutrients. 2014;6(9):3672–95. 10.3390/nu6093672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Niebylski M, Lu T, Campbell N, Arcand J, Schermel A, Hua D, et al. Healthy Food Procurement Policies and Their Impact. Int J Environ Res Public Health. 2014;11(3):2608–27. 10.3390/ijerph110302608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization. Reducing salt intake in populations: report of a WHO Forum and Technical Meeting. Geneva, Switzerland: World Health Organization; 2007 [cited 2014 30 October]; 1–56]. Available from: http://www.who.int/dietphysicalactivity/Salt_Report_VC_april07.pdf.
- 39. McLean RM. Measuring population sodium intake: a review of methods. nutrients. 2014;6(11):4651–62. 10.3390/nu6114651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. The World Health Organization. STEPwise approach to surveillance (STEPS) The World Health Organization,; 2014. [cited 2014 23 September]. Available: http://www.who.int/chp/steps/en/. [Google Scholar]
- 41. Pietinen P, Valsta LM, Hirvonen T, Sinkko H. Labelling the salt content in foods: a useful tool in reducing sodium intake in Finland. Public Health Nutr. 2008. April;11(4):335–40. [DOI] [PubMed] [Google Scholar]
- 42. Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010;110(5):736–45. 10.1016/j.jada.2010.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Udagawa K, Miyoshi M, Yoshiike N. Mid-term evaluation of "Health Japan 21": focus area for the nutrition and diet. Asia Pac J Clin Nutr. 2008;2:445–52. [PubMed] [Google Scholar]
- 44. Xi B, Hao Y, Liu F. Salt reduction strategies in China. Lancet. 2014;383(9923):1128 10.1016/S0140-6736(14)60567-5 [DOI] [PubMed] [Google Scholar]
- 45. Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014. February;99(2):334–43. 10.3945/ajcn.113.059121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The George Institute for Global Health. China Salt Substitute and Stroke Study (SSaSS). [Internet]: ClinicalTrials.gov; 2014 [cited 2014 20 November]. Available: http://clinicaltrials.gov/show/NCT02092090.
- 47.Republic of Mauritius Ministry of Health and Quality of Life. National Plan of Action for Nutrition 2009–2010. 2009 [cited 2014 16 June]. Available: http://health.gov.mu/English/Documents/nut1-8.pdf.
- 48. Charlton K, Steyn K, Levitt D. Dietary Intervention Lowers Blood Pressure In South Africans with Hypertension South African Medical Research Council; 2007. [cited 2013 24 October]. Available: http://www.mrc.ac.za/policybriefs/saltpolicy.pdf. [Google Scholar]
- 49. Hofman K, Tollman S. Population health in South Africa: a view from salt mines. Lancet Glob Health. 2013;1(2). [DOI] [PubMed] [Google Scholar]
- 50. Pan American Health Organisation. Salt-Smart Americas: A Guide for Country-Level Action Washington, DC: PAHO; 2013. [cited 2013 30 October]. Available: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=21554&Itemid. [Google Scholar]
- 51.Pan American Health Organization. Report for the Technical Meeting on Setting Targets and Timelines to Reduce the Salt Content of Food. Mexico: Pan American Health Organization,; 2013 [cited 2014 3 March]. Available: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=25646+&Itemid=999999&lang=en.
- 52. Ministry of Health NCD health promotion and control department. "Menos SAL, Mas VIDA" initiative—Experience in Argentina. [PowerPoint slides]: Pan American Health Organization; 2011. [cited 2014 25 June 2014]. Available: http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&gid=15753&Itemid=. [Google Scholar]
- 53. Nilson EA, Jaime PC, Resende Dde O. Initiatives developed in Brazil to reduce sodium content of processed foods. Rev Panam Salud Publica. 2012. October;32(4):287–92. [DOI] [PubMed] [Google Scholar]
- 54. Campbell NR, Willis KJ, L'Abbe M, Strang R, Young E. Canadian initiatives to prevent hypertension by reducing dietary sodium. Nutrients. 2011. August;3(8):756–64. 10.3390/nu3080756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Charry D. Strategy to reduce sodium/salt intake in Chile Ministry of Health; 2011. [cited 2013 19 November]. Available: http://www.paho.org/hq/index.php?option=com_content&view=article&id=6227&Itemid=4330&lang=en. [Google Scholar]
- 56. Allemandi L, Tiscornia V, Castronuovo L, Schoj V, Champagne B. Mapping of civil society organizations in Latin America and the Caribbean working on initiatives to reduce salt intake in the population InterAmerican Heart Foundation,; 2013. [cited 2014 24 March]. Available: http://www.healthycaribbean.org/newsletters/march-2014/Mapping-of-civil-society-organizations.pdf. [Google Scholar]
- 57. Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988. July 30;297(6644):319–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Blanco-Metzler A, Montero-Campos Mde L, Nunez-Rivas H, Gamboa-Cerda C, Sanchez G. Advances in reducing salt and sodium intake in Costa Rica. Rev Panam Salud Publica. 2012. October;32(4):316–20. [DOI] [PubMed] [Google Scholar]
- 59. Penney S. Dropping the Salt. Practical steps countries are taking to prevent chronic non-communicable diseases through population-wide dietary salt reduction Canada: Public Health Agency of Canada; 2009. [cited 2013 23 October]. Available: http://www.salux-project.eu/docpublic/download/name/Dropping%20the%20salt%20-%20Sheila%20Penney.pdf-179. [Google Scholar]
- 60. Ministry of Health Paraguay. Advances & Challenges Paraguay Pan American Health Organization,; 2011. [cited 2014 31 October]. Available: http://www.paho.org/hq/index.php?option=com_content&view=article&id=6227&Itemid=4330&lang=en. [Google Scholar]
- 61. He FJ, Campbell NR, MacGregor GA. Reducing salt intake to prevent hypertension and cardiovascular disease. Rev Panam Salud Publica. 2012. October;32(4):293–300. [DOI] [PubMed] [Google Scholar]
- 62. Levings J, Cogswell M, Curtis CJ, Gunn J, Neiman A, Angell SY. Progress toward sodium reduction in the United States. Rev Panam Salud Publica. 2012. October;32(4):301–6. [DOI] [PubMed] [Google Scholar]
- 63. Institute of Medicine (U.S.). Committee on Strategies to Reduce Sodium Intake. Strategies to Reduce Sodium Intake in the United States Henney J, Taylor C, Boon C, editors. Washington DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 64. New York City Department of Health and Mental Hygiene. National Salt Reduction Initiative 2008. [cited 2014 25 November]. Available: http://www.nyc.gov/html/doh/html/diseases/salt.shtml. [Google Scholar]
- 65. World Health Organization; Consultation on developing strategic directions for salt and fat reduction in the Eastern Mediterranean Region Cairo, Egypt: World Health Organization; 2013. [cited 2014 11 June]. Available: http://www.emro.who.int/nutrition/nutrition-events/salt-fat-reduction.html. [Google Scholar]
- 66.Bundesministerium Fur Gesundheit. Austrian National Salt Reduction Initiative. 2013 [cited 2014 30 April]. Available: http://www.bmg.gv.at/cms/home/attachments/4/9/8/CH1046/CMS1373970659184/who_conference_austrian_salt_initiative.pptx.
- 67. Federal Public Service Health. Food Chain Safety and Environment Salt in Bread: Technical, Taste and other Parameters for Healthy Eating. The Belgian Approach. Belgium: European Commission; 2009. [cited 2014 26 June]. Available: http://ec.europa.eu/health/nutrition_physical_activity/docs/ev20091021_valkenborg_en.pdf. [Google Scholar]
- 68. Jelakovic B, Kaic-Rak A, Milicic D, Premuzic V, Skupnjak B, Reiner Z. Less salt—more health. Croatian action on salt and health (CRASH). Lijec Vjesn. 2009. Mar-Apr;131(3–4):87–92. [PubMed] [Google Scholar]
- 69. Pietinen P. Finland's experiences in salt reduction Brussels: National Institute for Health and Welfare,; 2009. [cited 2014 13 June]. Available: http://ec.europa.eu/health/nutrition_physical_activity/docs/ev20091021_pietinen_en.pdf. [Google Scholar]
- 70. Pietinen P, Mannisto S, Valsta LM, Sarlio-Lahteenkorva S. Nutrition policy in Finland. Public Health Nutr. 2010. June;13(6A):901–6. 10.1017/S1368980010001072 [DOI] [PubMed] [Google Scholar]
- 71.National Institute for Food and Nutrition Science. Implementation of the "Spot Salt!" Hungarian Salt Reduction Program. 2011 [cited 2014 8 November]. Available: http://www.oeti.hu/download/national_salt_reduction_programme_-_english_summary.pdf.
- 72. Food Safety Authority of Ireland. Salt and Health Food Safety Authority of Ireland,; 2014. [cited 2014 4 November]. Available: http://www.fsai.ie/science_and_health/salt_and_health.html. [Google Scholar]
- 73. Strazzullo P, Cairella G, Campanozzi A, Carcea M, Galeone D, Galletti F, et al. Population based strategy for dietary salt intake reduction: Italian initiatives in the European framework. Nutr Metab Cardiovasc Dis. 2012;22(3):161–6. 10.1016/j.numecd.2011.10.004 [DOI] [PubMed] [Google Scholar]
- 74. Šmate I, Straume I, Skrule J. The National Policy of Public Health and Nutrition in Latvia. prolas. 2012;66(3):128. [Google Scholar]
- 75.National Food and Veterinary Risk Assessment Institute. Promotion of the reduced salt consumption—Lithuania. [cited 2013 8 November]. Available: http://www.nmvrvi.lt/uploads/File/Strukturos/Salt%20project.pdf.
- 76. Polonia J, Martins L. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009. November 2009;23(11):771–2. 10.1038/jhh.2009.64 [DOI] [PubMed] [Google Scholar]
- 77. Ribic CH, Zakotnik JM, Vertnik L, Vegnuti M, Cappuccio FP. Salt intake of the Slovene population assessed by 24 h urinary sodium excretion. Public Health Nutr. 2010. November;13(11):1803–9. 10.1017/S136898001000025X [DOI] [PubMed] [Google Scholar]
- 78.Ballesteros J. Workshop on salt reduction in bread. [PowerPoint Slides]: European Commission; 2009 [cited 2014 25 June 2014]. Available: http://ec.europa.eu/health/nutrition_physical_activity/docs/ev20091021_ballesteros_en.pdf.
- 79. Bundesamt für Gesundheit. Salt Strategy for 2013–16 Paper on a Strategy for reducing Salt Consumption Bundesamt für Gesundheit,; 2013. [cited 2014 23 April]. Available: http://www.blv.admin.ch/themen/04679/05055/05060/05115/index.html?lang=en&download=NHzLpZeg7t,lnp6I0NTU042l2Z6ln1ad1IZn4Z2qZpnO2Yuq2Z6gpJCFfYN5fWym162epYbg2c_JjKbNoKSn6A—. [Google Scholar]
- 80. He FJ, Brinsden HC, MacGregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens. 2014. June;28(6):345–52. 10.1038/jhh.2013.105 [DOI] [PubMed] [Google Scholar]
- 81. Wyness LA, Butriss JL, Stanner SA. Reducing the population's sodium intake: the UK Food Standards Agency's salt reduction programme. Public Health Nutr. 2012. February;15(2):254–61. 10.1017/S1368980011000966 [DOI] [PubMed] [Google Scholar]
- 82. Food Standards Agency. UK Salt Reduction Initiatives Department of Health,; 2009. [cited 2014 23 October]. Available: http://www.food.gov.uk/sites/default/files/multimedia/pdfs/saltreductioninitiatives.pdf. [Google Scholar]
- 83.World Health Organisation. Expert Meeting on Population Sodium Reduction Strategies for Prevention and Control of Noncommunicable Diseases in the South-East Asia Region. New Delhi: World Health Organization; 2013 [cited 2014 5 November]. Available: http://www.searo.who.int/entity/noncommunicable_diseases/documents/sea_ncd_86/en/.
- 84. World Health Organization. Regional Health Forum, WHO South-East Asia Region Special issue on blood pressure—take control. World Health Organization,; 2013. [cited 2014 5 November]. Available: http://www.searo.who.int/publications/journals/regional_health_forum/en/. [Google Scholar]
- 85. Hawkes C, Jewell J, Allen K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING framework. Obes Rev. 2013;14:159–68. 10.1111/obr.12098 [DOI] [PubMed] [Google Scholar]
- 86. World Health Organisation Regional Office for the Western Pacific. Regional Consultation On Strategies to Reduce Salt Intake Singapore: World Health Organization; 2010. [cited 2014 13 November]. Available: http://www.wpro.who.int/noncommunicable_diseases/documents/RCStratReduce_Salt_Intake/en/. [Google Scholar]
- 87. Department of Health Australia. Food and Health Dialogue website Australian Government Department of Health; 2009. [cited 2014 5 November]. Available: http://www.foodhealthdialogue.gov.au/internet/foodandhealth/publishing.nsf/Content/Home. [Google Scholar]
- 88. Land M-A, Webster J, Christoforou A, Praveen D, Jeffery P, Chalmers J, et al. Salt intake assessed by 24 h urinary sodium excretion in a random and opportunistic sample in Australia. BMJ Open. 2014. January 1, 2014;4(1). 10.1136/bmjopen-2013-003720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. World Cancer Research Fund International. WCRF International Food Policy Framework for Healthy Diets: NOURISHING World Cancer Research Fund International,; 2014. [cited 2014 28 April]. Available: http://www.wcrf.org/policy_public_affairs/nourishing_framework/nutrition_labelling_claims.php. [Google Scholar]
- 90. World Health Organization. Salt reduction in Mongolia World Health Organization; 2013. [cited 2014 13 November]. Available: http://www.wpro.who.int/world_health_day/2013/measuring_and_reducing_salt_MNG.pdf. [Google Scholar]
- 91. Gorton D, Jayasinha N, Monro D. Salt reduction in New Zealand: are we keeping up with Australia? N Z Med J. 2010. April 30;123(1313):102–4. [PubMed] [Google Scholar]
- 92. Health Promotion Board. HBP Declares War on Salt: Singapore Residents Exceed Daily Recommended Salt Consumption by 60% Singapore: Health Promotion Board,; 2011. [cited 2014 9 July]. Available: http://www.news.gov.sg/public/sgpc/en/media_releases/agencies/hpb/press_release/P-20111003-1/AttachmentPar/0/file/Salt%20and%20FINEST%20Press%20release%20(FINAL).pdf. [Google Scholar]
- 93. Global Agricultural Information Network. Indonesia Food and Agricultural Import Regulations and Standards USDA Foreign Agricultural Service; 2013. [cited 11 September 2014]. Available: http://www.puntofocal.gov.ar/notific_otros_miembros/idn84_t.pdf. [Google Scholar]
- 94. European Food Information Council. Global Update on Nutrition Labelling Brussels, Belgium: European Food Information Council,; 2014. [cited 2014 27 May]. Available: http://www.eufic.org/upl/1/default/doc/GlobalUpdateExecSumJan2014%2013%20Jan%202014_FINALwebSummary.pdf. [Google Scholar]
- 95. World Cancer Research Fund International. WCRF Nourishing Framework: Offer healthy foods London: World Cancer Research Fund International,; 2014. [cited 2014 16 September]. Available: http://www.wcrf.org/int/policy/nourishing-framework/offer-healthy-foods. [Google Scholar]
- 96. de Lago M. Spain bans sale of unhealthy food in schools in bid to tackle obesity. BMJ. [Journal Article]. 2011. 2011-06-28 15:03:41;342:d4073. [DOI] [PubMed] [Google Scholar]
- 97. United States Department of Agriculture. Nutrition Standards for School Meals [Webpage]: United States Department of Agriculture Food and Nutrition Service,; 2014. [cited 2014 4 September]. Available: http://www.fns.usda.gov/school-meals/nutrition-standards-school-meals. [Google Scholar]
- 98. Department of Environment Food and Rural Affairs; The Government Buying Standards for Food and Catering Services,. UK: UK Government Department for Environment Food & Rural Affairs,; 2014. [cited 2014 8 August]. Available: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/347129/GBS_for_Food_and_catering_services.pdf. [Google Scholar]
- 99.Walton J. Salt Intakes in the Irish Population: Estimates and Trends. 2013 [cited 2013 11 December]. Available: https://www.fsai.ie/uploadedFiles/Science_and_Health/Salt_and_Health/SRP_2013_Janette%20Walton_IUNA.pdf.
- 100.Safefood. Amarach Safetrak Wave 7. Ireland: Safefood; 2006 [cited 2014 19 February]. Available: http://www.safefood.eu/Publications/Market-research/Safetrak.aspx.
- 101.Nainggolan L. A Portugese Success Story: One Nation Begins to Curb Its Salt Intake. Medscape; 2009 [cited 2014 11 November]. Available: http://www.medscape.com/viewarticle/704589.
- 102. Health Promotion Board. Report of the National Nutrition Survey 2010 Singapore Singapore: Health Promotion Board, Singapore; 2010. [cited 2014 9 July]. Available: http://www.hpb.gov.sg/HOPPortal/content/conn/HOPUCM/path/Contribution%20Folders/uploadedFiles/HPB_Online/Publications/NNS-2010.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.