Abstract
Objective
the objective of this study was to present an analog method for preoperative planning of primary total hip arthroplasty procedures based on measuring the components by overlaying the transparencies of the prosthesis on the preoperative radiographs and checking the accuracy, both for predicting the size of the acetabular and femoral components used and for restoring the offset and correcting the dysmetria.
Methods
between March 2005 and July 2009, 56 primary total hip arthroplasty procedures performed on 56 patients at the Mario Covas State Hospital in Santo André were analyzed. The measurements on the femoral and acetabular components obtained through planning were compared with those that were used in the surgery. The offsets measured through the preoperative planning were compared with those measured on the postoperative radiographs. Dysmetria was evaluated before and after the operation.
Results
accuracy of 78.6% (p < 0.001) in predicting the size of the acetabular component and 82.2% (p < 0.001) in predicting the femoral nail was observed. The offsets measured through preoperative planning were statistically similar to the offsets measured on the postoperative radiographs. After the operation, we observed absolute equalization in 48.2% of the cases. In 87.5%, the dysmetria was less than or equal to 1 cm and in 69.6%, it was less than or equal to 0.5 cm.
Conclusions
the accuracy was 78.6% and 82.2%, respectively, for the acetabular and femoral components. The offsets that were planned preoperatively were statistically similar to those measured on postoperative radiographs. We found absolute equalization in 48.2% of the cases.
Keywords: Hip arthroplasty, Planning, Hip radiography
Resumo
Objetivos
apresentar um método analógico de planejamento pré‐operatório de artroplastias totais primárias de quadril baseado na medida dos componentes pela sobreposição das transparências da prótese sobre a radiografia pré‐operatória. E verificar a acurácia, tanto na previsão do tamanho do componente acetabular e do componente femoral usado como na restauração do offset e na correção das dismetrias.
Métodos
entre março de 2005 e julho de 2009 foram analisadas 56 artroplastias totais primárias de quadril feitas em 56 pacientes no Hospital Estadual Mário Covas. As medidas dos componentes femorais e acetabulares obtidas no planejamento foram comparadas com as que foram usadas na cirurgia. Os offset medidos no planejamento pré‐operatório foram comparados com os medidos na radiografia pós‐operatória. A dismetria foi avaliada nos momentos pré e pós‐operatórios.
Resultados
foi observada uma acurácia de 78,6% (p < 0,001) na previsão do tamanho do componente acetabular e de 82,2% (p < 0,001) na previsão da haste femoral. Os offset medidos no planejamento pré‐operatório foram estatisticamente semelhantes aos offset medidos na radiografia pós‐operatória. No pós‐operatório observamos a equalização absoluta em 48,2% dos casos. Em 87,5% a dismetria foi igual a ou menor do que 1 cm e em 69,6% foi igual a ou menor do que 0,5 cm.
Conclusões
a acurácia foi de 78,6% e 82,2%, respectivamente, para os componentes acetabulares e femorais. Os offset planejados pré‐operatório foram estaticamente semelhantes aos medidos na radiografia pós‐operatória. Verificamos equalização absoluta em 48,2% dos casos.
Palavras‐chave: Artroplastia de quadril, Planejamento, Quadril/radiografia
Introduction
Preoperative planning for hip arthroplasty procedures was initially poorly understood and used, since the designs and sizes of the prostheses were very limited.1, 2 Today, the variety of designs and the number of sizes of the components have increased considerably, and total hip arthroplasty has been transformed into a more complex procedure.2
Preoperative planning makes it possible to appropriately choose the sizes of the components, equalize the limbs and reduce the duration of the operation.2
Charnley1 demonstrated the importance of preoperative radiographic studies for choosing the correct size of the prosthesis components, and also emphasized the importance of restoring the offset. The latter is directly related to the stability of the arthroplasty.1, 3, 4, 5, 6
Dysmetria is a frequent complication of total hip arthroplasty. It causes lumbalgia, gait disorders and sciatic nerve injuries.7, 8, 9, 10, 11
In this study, using conventional radiographs, we present a preoperative planning method for primary total hip arthroplasty based on measuring the components through overlaying transparencies of the prosthesis on the preoperative radiograph. The study had the following objectives: to assess the accuracy of predicting the sizes of the acetabular and femoral components; to analyze the restoration of the offset; and to correct the dysmetria.
Material and methods
The project for this study was approved by the Ethics Committee of the ABC Medical School, under the number CEP 258/2007.
Between March 2005 and July 2009, 56 primary total hip arthroplasty procedures performed on 56 patients at Hospital Estadual Mário Covas were analyzed.
The mean age was 65 years. In all, 37 patients (66.1%) were female and 19 (33.9%) were male. All the patients had a diagnosis of arthrosis.
The inclusion criterion was the presence of unilateral hip arthrosis. The exclusion criteria were bilateral arthrosis; moderate or severe acetabular protrusion according to the Sotelo‐Garza and Charnley classification;12 acetabular dysplasia greater than Crowe type I;13 femoral neck fracture; and alterations in other joints that caused dysmetria.
All the arthroplasty procedures were total and cemented, and were performed using a posterior approach.
Pelvic radiographs were performed in anteroposterior (AP) view, centered on the pubic symphysis, with the lower limbs rotated internally by 15° and a distance of 1 m between the bulb of the apparatus and the film; and in lateral view covering the proximal one‐third of the femur.
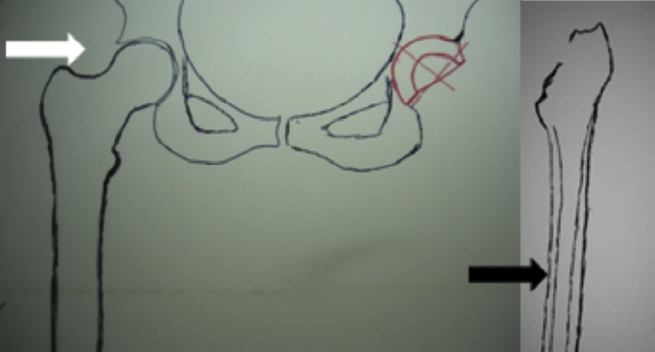
The acetabular component was measured by overlaying the acetabular transparency on the AP radiograph of the normal hip, in order to choose the number that fitted the outline of the acetabulum best. The parameters used were the upper lateral border of the acetabulum, the teardrop and Köhler's iliosciatic line (Fig. 1A and B). The size of the acetabular component was determined such that it would not go beyond the iliosciatic line (Fig. 1B).
Fig. 1.
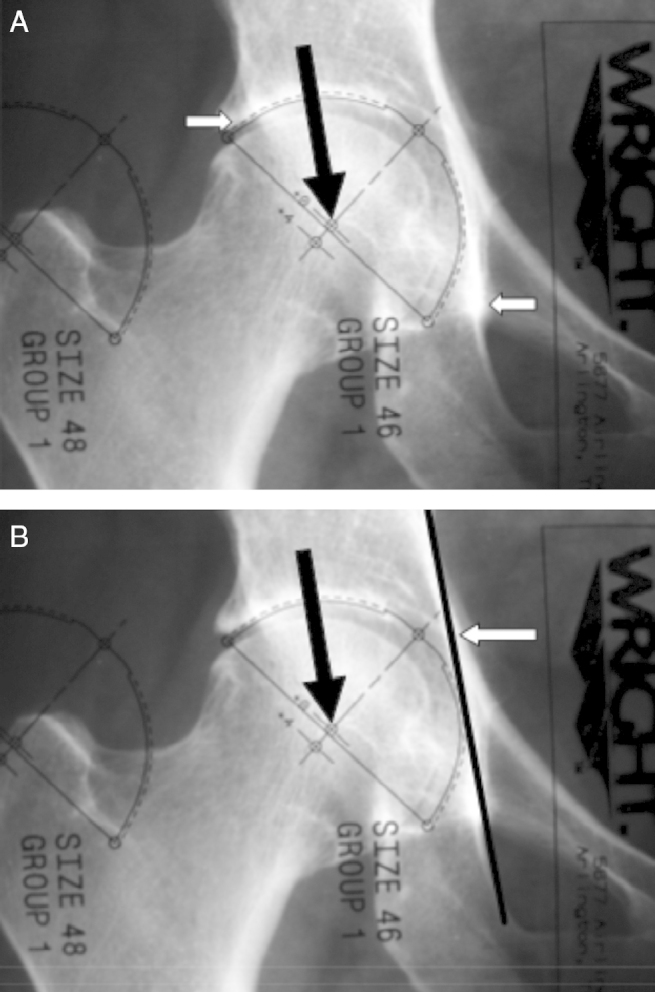
(A) Overlaying the transparency of the acetabular component on the normal side. The white arrow on the left side indicates the upper lateral border of the acetabulum. The white arrow on the right side indicates the teardrop. The center of rotation (CR) of the hip is marked on the transparency and is indicated by the black arrow. (B) Köhler's iliosciatic line. The white arrow indicates Köhler's iliosciatic line. The size of the acetabular component should not go beyond the iliosciatic line. The black arrow indicates the center of rotation.
After the center of rotation (CR) of the normal hip had been marked on the radiograph (Fig. 1A and B), it was transferred to the side to be operated. To transfer it, three reference lines were used as parameters:
Line H: going along the lower limit of the teardrops (Fig. 2A)
Line V1: going along the lateral border of the teardrop on the normal side and perpendicularly to the intersection with line H (Fig. 2A)
Line V2: going along the lateral border of the teardrop on the side to be operated and perpendicularly to the intersection with line H (Fig. 2A)
Fig. 2.
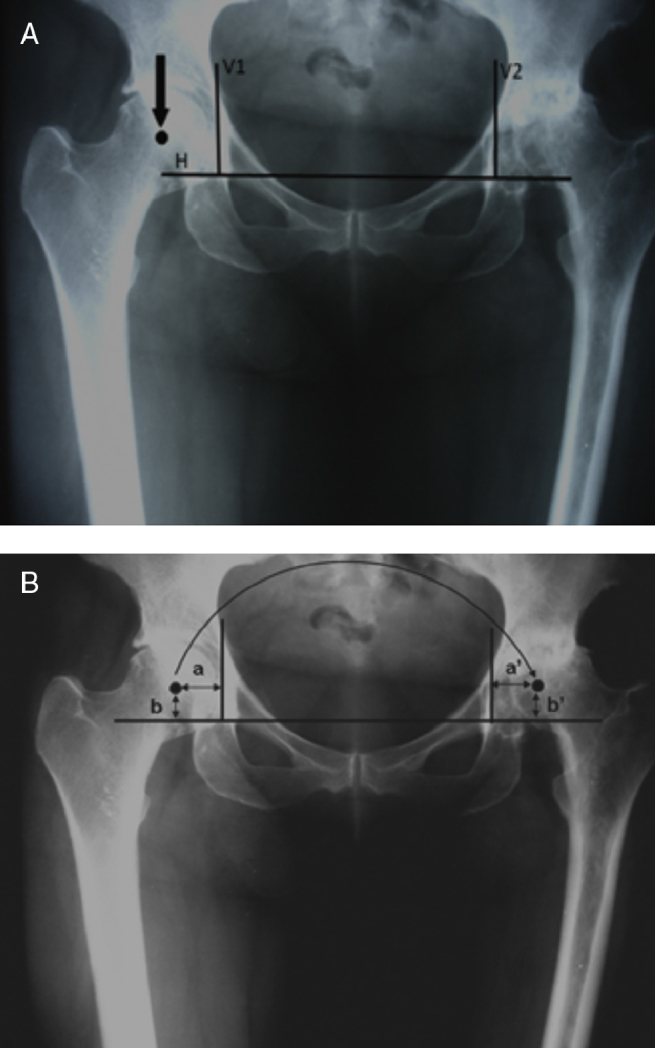
(A) Reference lines H, V1 and V2. The center of rotation is marked on the normal side, indicated by an arrow. Reference lines: the first goes along the lower edge of the teardrops (line H); the second is perpendicular to line H and goes along the lateral edge of the teardrop on the normal side (line V1); the third is also perpendicular to line H and goes along the lateral edge of the teardrop on the side to be operated (line V2). (B) Transfer of the CR from the right side (normal) to the left side. Distance a should be equal to a′ and distance b should be equal to b′.
From the reference lines, the CR was transferred from the normal to the affected side. We then defined four distances measured in millimeters:
Distance a: from the CR of the normal side to line V1 (Fig. 2B);
Distance b: from the CR of the normal side to line H (Fig. 2B);
Distance a′: same length as distance a, starting at line V2 (Fig. 2B);
Distance b′: same length as distance b, starting at line H (Fig. 2B).
The intersection point between the distances a′ and b′ was the CR of the side to be operated.
The femoral offset was the distance along a line going perpendicularly from the center of rotation of the femoral head to the intersection with a line going through the middle of the long axis of the femur.14
The offset of the prosthesis was the distance from a line going perpendicularly from the center of rotation of the prosthesis head to the intersection with a line going through the middle of the major longitudinal axis of the femoral nail (Fig. 3).
Fig. 3.
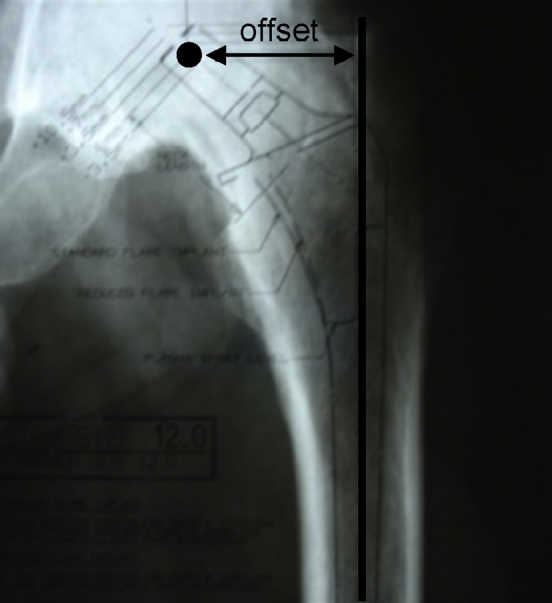
Offset of the prosthesis.
To choose the size of the femoral component, its transparency was overlaid on the AP radiograph on the side to be operated (Fig. 4). The femoral component chosen was determined to be the one with an offset closest to that of the normal side.
Fig. 4.

Measurement using the transparency.
The dysmetria could be one of three types: at the cost of the femur, at the cost of the acetabulum or at the cost of both the femur and the acetabulum (mixed or combined).15 To identify dysmetria, the parameters used were three lines on the AP radiograph of the pelvis, centered on the pubic symphysis:15
Line 1: determined by tracing out a straight line through the most distal points of the sciatic tuberosities;
Line 2: determined by tracing out a straight line along the upper lateral edge of the acetabula;
Line 3: determined by tracing out a straight line through the midpoints of the lesser trochanters.
In normal hips, the three lines are parallel (Fig. 5).
Fig. 5.
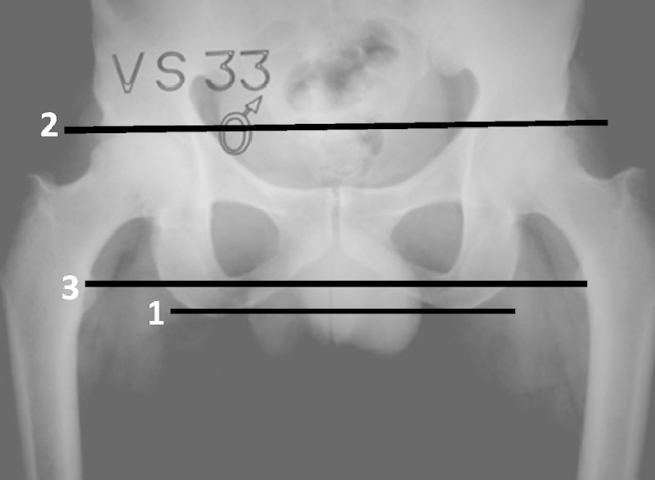
Normal hips. Line 1 goes along the lower limit of the sciatic tuberosities. Line 2 goes along the upper lateral edge of the acetabula. Line 3 goes through the midpoint of the lesser trochanters. The three lines are parallel.
To measure the dysmetria, the parameters used were line H, going along the lower limit of the teardrops, and line 3 (Fig. 6).
Fig. 6.
Calculation of the dysmetria. The dysmetria is obtained as the difference in the distances between line H and line 3 at the level of the lesser trochanters. The difference in measurements between segments “a” and “b” is the amount of the dysmetria. Dysmetria = a − b.
The pelvis with the acetabular component chosen, the calculated CR and the femur to be operated were drawn using tracing paper overlain on the AP radiograph (Fig. 7). The drawing of the pelvis was then overlain on the drawing of the femur, and both of these were placed on the transparency of the femoral component (Fig. 8).
Fig. 7.
The white arrow indicates the drawing of the pelvis with the acetabular component. The black arrow indicates the drawing of the femur.
Fig. 8.
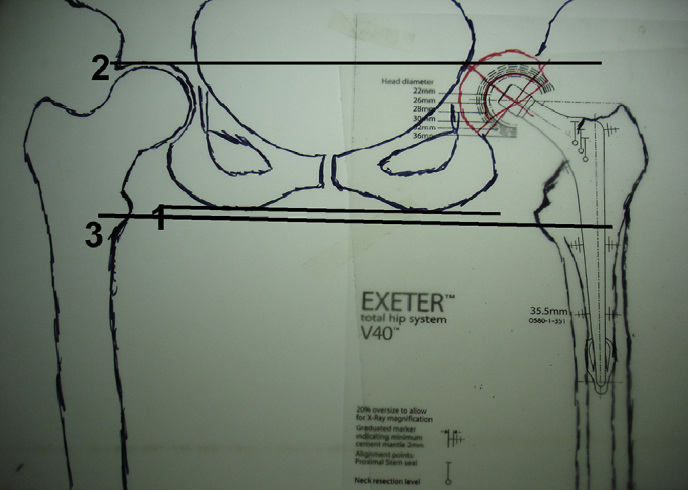
Preoperative planning. Lines 1, 2 and 3 are parallel.
The level of the osteotomy of the femoral neck for equalizing the limbs was defined by sliding the drawings across the femoral transparency. For this, lines 1, 2 and 3 had to be kept parallel (Fig. 8).
The chi‐square test was applied to ascertain the accuracy of the predictions for the acetabular and femoral components. The Mann–Whitney test was applied to compare the planned offset measurements with those obtained on the postoperative radiograph.
Dysmetria was analyzed after the operation.
We used the Statistical Package for the Social Sciences (SPSS), version 17.0, to obtain results of a statistical nature.
Results
Accuracy of 78.6% (p < 0.001) in predicting the size of the acetabular component was observed (Table 1). Accuracy of 82.2% (p < 0.001) in predicting the femoral nail was found (Table 2).
Table 1.
Frequency and percentage distribution of the acetabular components used at the two observation times.
| Acetabular component planned | Acetabular component used |
Total | |||
|---|---|---|---|---|---|
| 44 | 48 | 50 | 52 | ||
| 44 | 18 | 0 | 0 | 0 | 18 |
| 32.10% | 0.00% | 0.00% | 0.00% | 32.10% | |
| 48 | 0 | 20 | 0 | 0 | 20 |
| 0.00% | 35.70% | 0.00% | 0.00% | 35.70% | |
| 50 | 0 | 1 | 3 | 0 | 4 |
| 0.00% | 1.80% | 5.40% | 0.00% | 7.10% | |
| 52 | 0 | 5 | 1 | 3 | 9 |
| 0.00% | 8.90% | 1.80% | 5.40% | 16.10% | |
| 54 | 0 | 0 | 0 | 3 | 3 |
| 0.00% | 0.00% | 0.00% | 5.40% | 5.40% | |
| 56 | 0 | 0 | 1 | 1 | 2 |
| 0.00% | 0.00% | 1.80% | 1.80% | 3.60% | |
| Total | 18 | 26 | 5 | 7 | 56 |
| 32.10% | 46.40% | 8.90% | 12.50% | 100.00% | |
Source: Hospital Estadual Mário Covas.
Table 2.
Frequency and percentage distribution of the femoral nails used at the two observation times.
| Femoral component planned | Femoral component used |
Total | |||||
|---|---|---|---|---|---|---|---|
| 10.5 | 12 | 13.5 | 15 | 35.5 | 37.5 | ||
| 10.5 | 8 | 0 | 0 | 0 | 0 | 0 | 8 |
| 14.30% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 14.30% | |
| 12 | 3 | 15 | 0 | 0 | 0 | 0 | 18 |
| 5.40% | 26.80% | 0.00% | 0.00% | 0.00% | 0.00% | 32.10% | |
| 13.5 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| 0.00% | 0.00% | 1.80% | 0.00% | 0.00% | 0.00% | 1.80% | |
| 15 | 0 | 1 | 1 | 1 | 0 | 0 | 3 |
| 0.00% | 1.80% | 1.80% | 1.80% | 0.00% | 0.00% | 5.40% | |
| 16.5 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| 0.00% | 0.00% | 0.00% | 1.80% | 0.00% | 0.00% | 1.80% | |
| 35.5 | 0 | 0 | 0 | 0 | 15 | 1 | 16 |
| 0.00% | 0.00% | 0.00% | 0.00% | 26.80% | 1.80% | 28.60% | |
| 37.5 | 0 | 0 | 0 | 0 | 2 | 6 | 8 |
| 0.00% | 0.00% | 0.00% | 0.00% | 3.60% | 10.70% | 14.30% | |
| 44 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 1.80% | 1.80% | |
| Total | 11 | 16 | 2 | 2 | 17 | 8 | 56 |
| 19.60% | 28.60% | 3.60% | 3.60% | 30.40% | 14.30% | 100.00% | |
Source: Hospital Estadual Mário Covas.
The offsets measured in the preoperative planning were statistically similar to the offsets measured on postoperative radiographs, with p = 0.630 (Table 3).
Table 3.
Description of and comparison between the offsets planned and used.
| Pair of variables | n | Mean | Standard deviation | Minimum | Maximum | 25th percentile | Median | 75th percentile | Significance (p) |
|---|---|---|---|---|---|---|---|---|---|
| Offset planned (mm) | 56 | 39.7 | 5.4 | 30.0 | 55.0 | 35.0 | 38.5 | 42.0 | 0.630 |
| Offset used (mm) | 56 | 40.3 | 6.4 | 30.0 | 57.0 | 35.0 | 39.0 | 45.0 |
Source: Hospital Estadual Mário Covas.
The mean displacement of the CR was 4 mm in the horizontal axis and 6 mm in the vertical axis.
The mean preoperative dysmetria was 1.6 cm, with a range from 0.0 to 3.9 cm (Table 4). After the operation, we observed that the limbs had been equalized in 27 patients (48.3%), stretched in 18 (32.1%) and shortened in 11 (19.6%). The mean postoperative dysmetria was 0.4 cm, with a range from 0.0 to 2.1 cm (Table 5). We observed that the postoperative dysmetria was less than or equal to 1.0 cm in 87.5% of the patients and less than or equal to 0.5 cm in 69.6%.
Table 4.
Description of the affected lower limb before the operation.
| Length of affected lower limb before the operation (cm) | n | Mean | Standard deviation | Minimum | Maximum | 25th percentile | Median | 75th percentile |
|---|---|---|---|---|---|---|---|---|
| Shortened | 53 | 1.7 | 0.9 | 0.4 | 3.9 | 1.0 | 1.5 | 2.3 |
| Equalized | 3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total | 56 | 1.6 | 0.9 | 0.0 | 3.9 | 0.9 | 1.5 | 2.2 |
Source: Hospital Estadual Mário Covas.
Table 5.
Description of the affected lower limb after the operation.
| Length of affected lower limb before the operation (cm) | n | Mean | Standard deviation | Minimum | Maximum | 25th percentile | Median | 75th percentile |
|---|---|---|---|---|---|---|---|---|
| Shortened | 11 | 0.9 | 0.7 | 0.3 | 2.1 | 0.4 | 0.8 | 1.7 |
| Stretched | 18 | 0.7 | 0.3 | 0.4 | 1.5 | 0.5 | 0.6 | 1.0 |
| Equalized | 27 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total | 56 | 0.4 | 0.5 | 0.0 | 2.1 | 0.0 | 0.3 | 0.6 |
Source: Hospital Estadual Mário Covas.
With regard to the femoral nail, it was observed to be positioned neutrally in 43 hips (76.7%), with valgus rotation in three (5.4%) and with varus rotation in 10 (17.9%).
The analysis of the mean inclination of the acetabular component in the frontal plane showed that this was 42°, with a range from 30° to 58°.
The variations in the offset on postoperative radiographs in relation to what was planned were statistically similar (p = 0.123), with regard to neutral, varus and valgus positions of the femoral nail.
The correlation between variations in the postoperative offset values relative to what was planned and the inclination of the acetabular component was not statistically significant (p = 0.657).
Discussion
During the 1970s, only limited numbers of implants were placed.2, 16 Today, there are several different designs and a large number of sizes available,17 which makes planning essential.2, 16 However, few studies have evaluated the accuracy of component size predictions.2, 6, 16, 18, 19
We began this investigation with the aim of evaluating the method used in our institution.
Today, planning methods using digital radiographs exist. These enable high precision,6, 20 as demonstrated by Eggli et al.,6 who observed accuracy of around 90% in component predictions.
In Brazil, digital radiographs are still not used routinely. The method described in our study was less precise, but can be applied to conventional radiographs without additional cost for the procedure.
In our sample, we observed that the accuracy was 78.6% for the acetabular components and 82.2% for the femoral components. These values were similar to those presented by Paniego et al.,2 who found accuracies of 83% for the acetabular components and 76% for the femoral components; and to those reported by González Della Valle et al.,16 who observed accuracies of 83% and 78%, respectively, for the acetabular and femoral components. Both of the author groups used planning methods with conventional radiographs.
It is difficult to predict the exact magnification in conventional radiographs. For this reason, in order to minimize the possible deviations, we standardized production of the radiographs as described in the methodology.
Arthroplasty procedures aim to restore the hip biomechanics to normal conditions, through choosing appropriate prosthesis sizes, so as to avoid intraoperative and postoperative complications and consequently increase prosthesis longevity.
The importance of the offset is related to the functioning of the abductor musculature:1, 4, 5, 21 through planning, it is possible to restore it.1, 3, 4, 5, 6, 21, 22 Its restoration is related to the stability of the arthroplasty.1, 3, 6, 21 The offsets measured in the preoperative planning in our sample were statistically similar to those measured on postoperative radiographs. This is related to the accuracy of 82.2% in predicting the size of the femoral nails, which had fixed offset values. Therefore, if the size of the femoral component is correct, there is a greater likelihood of achieving the planned offset.
In 1988, Yoder et al.23 observed greater rates of loosening of the femoral component when the acetabular component was placed above and laterally to the center of rotation. In 1996, Pagnano et al.24 observed greater rates of loosening of the acetabular and femoral components when the acetabular component was placed above the center of rotation, even without lateral displacement. In our sample, mean variations from the planned center of rotation were 4 mm in the horizontal axis and 6 mm in the vertical axis. These were close to what was presented by Paniego et al.,2 who observed that 96% of the centers of rotation were placed with displacement of less than 4 mm from the planned center of rotation. It seems to us that the changes in position of the center of rotation are difficult to measure, since they can vary greatly with the magnification of conventional radiographs, given that these changes are measured in millimeters. Yoder et al.23 observed that measurements of 4–5 mm are very imprecise on conventional radiographs, which explains the greater accuracy of planning when digital radiographs are used.
In situations in which the acetabulum presents loss of bone stock or dysplasia, placement of the acetabular component at the center of ideal rotation is more difficult, since in these cases additional coverage with grafts from the femoral head may be needed. These cases were excluded from our study, since they could have led to bias in the analysis on displacement of the center of rotation.
Dysmetria is a common complication following hip arthroplasty.7, 8, 9 Its correction can be envisaged through preoperative planning1, 3, 6, 21 and also during the operation.8 The operated side often becomes stretched.7 Dysmetria greater than 1 cm has been correlated with lumbalgia.9 Our results were inferior to those presented by Eggli et al.,6 who observed dysmetria of less than 5 mm in 94% of the cases. In our sample, we observed absolute equalization in 48.2% of the cases. In 87.5%, the dysmetria was less than or equal to 10 mm and in 69.6% it was less than or equal to 5 mm. However, it needs to be taken into consideration that the study by Eggli et al.6 was conducted using digital radiographs.
Dolhain et al.5 reported that varus or valgus positioning of the femoral and acetabular components influenced the offset of the arthroplasty. In our sample, the relationship between the values of increased, decreased and equalized offset achieved after the operation through putting the femoral component into a varus, valgus or neutral position was analyzed. It was observed that there were no statistically significant differences between the categories of the variable of femoral nail position (p = 0.123). The femoral nail was placed in a neutral position in 76.7% of the cases, in varus in 17.9% and in valgus in 5.4%. However, in the cases in which we observed valgus or varus positioning, these were slight errors that did not give rise to any significant variations in offset.
Going against what was observed by Dolhain et al.,5 we found from our sample that the variations in offset were not related to the variations in inclination of the acetabular component.
Dobzyniac et al.25 determined that the ideal for the femoral component was to position the nail in neutral in the frontal plane, with 20° to 30° of anteversion and neutral position. For the acetabular component, it should be 45° of abduction and 20° to 30° of anteversion. Lewinneck et al.11 defined a safety zone for the acetabular component comprising an inclination of 30° to 50°, in the frontal plane, and anteversion of 5° to 25°. In our sample, the acetabular component was positioned with a mean inclination in the frontal plane of 42°, with a range from 30° to 58°.
To obtain greater precision in positioning prosthesis components, computer‐aided navigation systems were developed, thus enabling lower variation in positioning the acetabular component.26, 27, 28, 29 We did not use these systems, because their cost is still high in Brazil. In our study, the mean inclination of the acetabular component in the frontal plane was 42°, with a range from 32° to 58°. This variation was greater than what has been presented using computer‐aided navigation systems.
The preoperative planning enabled greater precision in choosing the sizes of the acetabular and femoral components and facilitated correction of the dysmetria. It made it possible to predict intraoperative difficulties such as the need for femoral head bone grafting for additional graft coverage in cases of acetabular dysplasia, the need for in situ osteotomy of the femoral neck in cases of severe acetabular protrusion and the need for small components in short patients. It made it possible to choose a femoral component for restoring the offset, and to determine the ideal center of rotation on the affected side.
Conclusions
-
a)
We observed accuracy of 78.5% and 82.2%, respectively, for the acetabular and femoral components;
-
b)
The offsets measured during the preoperative planning were statistically similar to those measured on the postoperative radiographs;
-
c)
There was absolute equalization in 48.2% of the cases. In 87.5%, the dysmetria was less than or equal to 1 cm and in 69.6% it was less than or equal to 0.5 cm.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
We are grateful for collaboration from Professors Giancarlo Polesello, Sérgio Mainine, Alberto Miyazaki and Joel Murachovski, whose opinions were fundamental in drawing up this study.
Footnotes
Please cite this article as: Miashiro EH, Fujikib EN, Yamaguchib EN, Chikudeb T, Rodriguesb LHS, Fontesb GM, et al. Planejamento pré‐operatório de artroplastias totais primárias de quadril com o uso de radiografias convencionais. Rev Bras Ortop. 2014;49:140–148.
Work performed at Hospital Estadual Mário Covas, Faculdade de Medicina do ABC (FMABC), Santo André, SP, Brazil.
References
- 1.Charnley J. Springer‐Verlag; New York: 1979. Low friction arthroplasty of the hip. [Google Scholar]
- 2.Paniego G., Buttaro M., González Della Valle A., Piccaluga F. Utilidad e predictibilidad de um método de planeamiento preoperatorio para la artroplastia total de cadera. Rev Asoc Argent Ortop Traumatol. 2004;69(1):6–12. [Google Scholar]
- 3.Bono J.V. Digital templating in total hip arthroplasty. J Bone Joint Surg Am. 2004;86(Suppl. 2):118–122. doi: 10.2106/00004623-200412002-00016. [DOI] [PubMed] [Google Scholar]
- 4.Charles M.N., Bourne R.B., Davey J.R., Greenwald A.S., Morrey B.F., Rorabeck C.H. Soft‐tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect. 2005;54:131–141. [PubMed] [Google Scholar]
- 5.Dolhain P., Tsigaras H., Bourne R.B., Rorabeck C.H., Mac Donald S., Mc Calden R. The effectiveness of dual offset stems in restoring offset during total hip replacement. Acta Orthop Belg. 2002;68(5):490–499. [PubMed] [Google Scholar]
- 6.Eggli S., Pisan M., Müller M.E. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 1998;80(3):382–390. doi: 10.1302/0301-620x.80b3.7764. [DOI] [PubMed] [Google Scholar]
- 7.Konyves A., Bannister G.C. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):155–157. doi: 10.1302/0301-620x.87b2.14878. [DOI] [PubMed] [Google Scholar]
- 8.McGee H.M., Scott J.H. A simple method of obtaining equal leg length in total hip arthroplasty. Clin Orthop Relat Res. 1985;(194):269–270. [PubMed] [Google Scholar]
- 9.Jasty M., Webster W., Harris W. Management of limb length inequality during total hip replacement. Clin Orthop Relat Res. 1996;(333):165–171. [PubMed] [Google Scholar]
- 10.Turula K.B., Friberg O., Lindholm T.S., Tallroth K., Vankka E. Leg length inequality after total hip arthroplasty. Clin Orthop Relat Res. 1986;(202):163–168. [PubMed] [Google Scholar]
- 11.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip‐replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 12.Sotelo-Garza A., Charnley J. The results of Charnley arthroplasty of the hip performed for protrusio acetabuli. Clin Orthop Relat Res. 1978;(132):12–18. [PubMed] [Google Scholar]
- 13.Crowe J.F., Mani V.J., Ranawat C.S. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23. [PubMed] [Google Scholar]
- 14.Lecerf G., Fessy M.H., Philippot R., Massin P., Giraud F., Flecher X. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Rev Chir Orthop Traumatol. 2009;95(3):210–219. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Cabral F.P., Rondinelli P.C., Côrtes S. Artroplastia total do quadril: planejamento pré‐operatório. In: Rondinelli PC, editor. O quadril do adulto. Medsi; São Paulo: 2001. pp. 1089–1091. [Clínica Ortopédica, v 2, n.°. 4] [Google Scholar]
- 16.González Della Valle A., Slullitel G., Piccaluga F., Salvati E.A. The precision and usefulness of preoperative planning for cemented and hybrid primary total hip arthroplasty. J Arthroplasty. 2005;20(1):51–58. doi: 10.1016/j.arth.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 17.Massin P., Geais L., Astoin E., Simondi M., Lavaste F. The anatomic basis for the concept of lateralized femoral stems: a frontal plane radiographic study of the proximal femur. J Arthroplasty. 2000;15(1):93–101. doi: 10.1016/s0883-5403(00)91337-8. [DOI] [PubMed] [Google Scholar]
- 18.Carter L.W., Stovall D.O., Young T.R. Determination of accuracy of preoperative templating of noncemented femoral prostheses. J Arthroplasty. 1995;10(4):507–513. doi: 10.1016/s0883-5403(05)80153-6. [DOI] [PubMed] [Google Scholar]
- 19.Knight J.L., Atwater R.D. Preoperative planning for total hip arthroplasty. Quantitating its utility and precision. J Arthroplasty. 1992;7(Suppl.):403–409. doi: 10.1016/s0883-5403(07)80031-3. [DOI] [PubMed] [Google Scholar]
- 20.Oddy M.J., Jones M.J., Pendegrass C.J., Pilling J.R., Wimhurst J.A. Assessment of reproducibility and accuracy in templating hybrid total hip arthroplasty using digital radiographs. J Bone Joint Surg Br. 2006;88(5):581–585. doi: 10.1302/0301-620X.88B5.17184. [DOI] [PubMed] [Google Scholar]
- 21.Linclau L., Dokter G., Peene P. Radiological aspects in preoperative planning and postoperative assessment of cementless total hip arthroplasty. Acta Orthop Belg. 1993;59(2):163–167. [PubMed] [Google Scholar]
- 22.Rittmeister M., Callitsis C. Factors influencing cup orientation in 500 consecutive total hip replacements. Clin Orthop Relat Res. 2006;(445):192–196. doi: 10.1097/01.blo.0000194669.77849.3c. [DOI] [PubMed] [Google Scholar]
- 23.Yoder S.A., Brand R.A., Pedersen D.R., O’Gorman T.W. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res. 1988;(228):79–87. [PubMed] [Google Scholar]
- 24.Pagnano W., Hanssen A.D., Lewallen D.G., Shaughnessy W.J. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am. 1996;78(7):1004–1014. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Dobzyniak M., Fehring T.K., Odum S. Early failure in total hip arthroplasty. Clin Orthop Relat Res. 2006;(447):76–78. doi: 10.1097/01.blo.0000203484.90711.52. [DOI] [PubMed] [Google Scholar]
- 26.Nogler M., Kessler O., Prassl A., Donnelly B., Streicher R., Sledge J.B. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;(426):159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 27.Schleicher I., Nogler M., Donnelly W., Sledge J. Acetabular placement using an imageless navigation system, a cadaver trial. J Bone Joint Surg Br. 2004;86(Suppl. 3):474. [Google Scholar]
- 28.Dorr L.D., Malik A., Wan Z., Long W.T., Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;(465):92–99. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 29.Parratte S., Argenson J.N. Validation and usefulness of a computer‐assisted cup‐positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89(3):494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]



