Abstract
Objectives
The burden of disease in patients with ankylosing spondylitis (AS) can be considerable. However, no agreement has been reached among expert members of Assessment of SpondyloArthritis International Society (ASAS) to define severity of AS. Based on the International Classification of Functioning, Disability and Health (ICF), a core set of items for AS has been selected to represent the entire spectrum of possible problems in functioning. Based on this, the objective of this study was to develop a tool to quantify health in AS, the ASAS Health Index.
Methods
First, based on a literature search, experts’ and patients’ opinion, a large item pool covering the categories of the ICF core set was generated. In several steps this item pool was reduced based on reliability, Rasch analysis and consensus building after two cross-sectional surveys to come up with the best fitting items representing most categories of the ICF core set for AS.
Results
After the first survey with 1754 patients, the item pool of 251 items was reduced to 82. After selection by an expert committee, 50 items remained which were tested in a second cross-sectional survey. The results were used to reduce the number of items to a final set of 17 items. This selection showed the best reliability and fit to the Rasch model, no residual correlation, and absence of consistent differential item function and a Person Separation Index of 0.82.
Conclusions
In this long sequential study, 17 items which cover most of the ICF core set were identified that showed the best representation of the health status of patients with AS. The ASAS Health Index is a linear composite measure which differs from other measures in the public domain.
INTRODUCTION
Ankylosing spondylitis (AS), is the prototype of spondyloarthritis (SpA), and is characterised by inflammation and new bone formation in the axial skeleton, enthesitis and peripheral arthritis.1 Since AS usually starts in early adulthood, the lifetime impact of the disease can be considerable resulting in pain, stiffness, fatigue, limitation in activities and social participation.2–4 However, no agreement has been reached among expert members of Assessment of SpondyloArthritis international Society (ASAS) to define severity of AS. Since severity contains different aspects of the disease (disease activity, damage, reduced mobility, reduced physical function, reduced social participation), it comes close to the meaning of impact of the disease. The impact of the disease might be related to quality of life, but is even a bit broader than the subjective experience of those problems.
This broader concept is included in the International Classification of Functioning, Disability and Health (ICF) which has been published by WHO more than a decade ago. The ICF represents an universally accepted model that classifies and describes functioning, disability and health in individuals with a wide spectrum of diseases or conditions in a systematic way.5 The term ‘functioning’ in the context of the ICF is equated more with ‘health’ than ‘function’ as the latter term is limited to physical function and ignores the complexity of global functioning. The ASAS has applied the ICF as a basis to define a core set of items relevant for patients with AS.6 Within the Comprehensive ICF Core Set for AS, 80 categories have been selected describing the typical spectrum of problems related to the functioning of patients with AS in a multidis-ciplinary assessment. Sixty-six items relate to functioning and 14 to environmental factors (EFs). There is an increasing awareness that some functional restrictions are influenced by contextual factors related to personal and EFs.7 EFs are defined as elements external to the individual that can influence functioning either as a facilitator or as a barrier. More recently, the role of contextual factors has also been recognised by Outcome Measures in Rheumatology (OMERACT).8
Instruments currently available for the assessment of patients with AS focus predominantly on specific aspects of health such as pain, disease activity and physical function. The overall picture of impairments, limitations and restrictions in activities or social participation of patients with AS are not adequately assessed in freely available disease-specific questionnaires. Moreover, most of the available questionnaires have not conceptualised their underlying construct. Although the ICF could possibly serve as an appropriate model, no ICF based self-reported measure has been published to date.
If such a tool is intended for measurement purposes, it is necessary that the items representing the ICF categories are unidimensional. The unidimensionality of the functioning categories of the ICF has already been confirmed.9,10 Therefore, the ICF Core Set for AS may serve as the underlying construct to develop an appropriate tool since the whole range of functioning and disability of patients with AS is captured.
The objective of this paper is to describe the development of an instrument aimed at assessing health in patients with AS as operationalised by the ICF according to ICF categories of functioning. This disease-specific questionnaire is based on the Comprehensive ICF Core Set for AS which we have named the ASAS Health Index (ASAS HI).
METHODS
The development of this health index represents a combined effort of ASAS and the ICF Research Branch in cooperation with the WHO Collaboration Centre of the Family of International Classifications in Germany (at Deutsches Institut für Medizinische Dokumentation und Information (DIMDI)). The intention of the project and the underlying methodology has been described elsewhere.11 In brief, the aim was to develop an index for functioning and health to be used in patients with AS that is easy to administer, easy to fill in and applicable to patients worldwide. Five phases were considered necessary to achieve this goal (see table 1). The selection of items related to contextual factors was ignored here since a different methodological approach would have been required for the selection of EF.
Table 1.
Phases of development for the ASAS Health Index
| Phase | Aims | Methods |
|---|---|---|
| Ia Preparatory | Development of a pool of items representing the categories of the Comprehensive ICF Core Set for AS | Linkage of various assessment tools for functioning and health to ICF categories |
| Ib Patient meeting | Patient preference and weighting of the items per ICF category | Relative weight to each item, patient-distributed 100 points per ICF category. |
| II 1st international cross-sectional survey | Item reduction (within and across ICF categories) | Rasch analysis, Spearman’s rank correlation coefficient |
| III Expert consultation | Agreement on item reduction | Nominal consensus process |
| IV 2nd international cross-sectional survey | Validation of the draft version and further item reduction | Testing psychometric properties Rasch analysis |
| V Consensus Meeting | Agreement on a final version | Nominal consensus process |
AS, ankylosing spondylitis; ASAS, Assessment of SpondyloArthritis international Society; ICF, International Classification of Functioning, Disability and Health.
Preparatory phase: The item pool was developed by linking items from existing questionnaires to the Comprehensive ICF Core Set for AS related to the components of body functions, activities and participation. It was decided not to link items to the component of body structure because involvement of body structures is not easily assessed by patients, and, if structures are affected, they should be captured by the component body functions. The origins of the items were: (a) from existing questionnaires currently available in the field of AS (identified by a systematic literature search) and (b) from additional instruments that are not commonly used in patients with AS but which have already been linked to the ICF (data from ICF Research Branch). This implies that items not commonly contained in AS specific measures which, however, covered categories of the ICF Core Set for AS, were also represented in the item pool. Examples of such items were motivation and depth of respiration (eg, “I have been less motivated to do anything that requires physical effort” from the Multiple Sclerosis Quality of Life Inventory). All items were linked separately by two trained health professionals (UK and AB) according to established linking rules.12,13 Consensus between the two health professionals was required for inclusion of an item. Disagreement was resolved by one of the developers of the ICF linking rules (AC). To be eligible, items had to be short, comprehensible and should only address a single concept. Where possible, potential items were quoted directly from the original instruments. However, to guarantee a consistent item structure some items had to be reworded. For example, they were transformed into the first person and into the present tense. The response option was dichotomised to ‘I agree’ and ‘I do not agree’.
Patient meeting: Face-to-face meetings were conducted with patients to ascertain which items currently included in the item pool were considered important and preferable by the patients. The patients were asked to give a relative weight to each item (patient distributed 100 points per category). In addition, patients were allowed to propose new items if they felt that the proposed concept was not adequately covered in the existing questionnaires.
First international cross-sectional survey: The objective of the survey was to reduce the item pool by identifying the best candidate items. A cross-sectional international web-based survey was undertaken to test the item pool in the following English-speaking countries: UK, USA, Canada, Australia and New Zealand. Due to the size of the item pool, the questionnaires were split into five subsets linked by a common set of 20 items. These common items reflected basic aspects of the disease such as pain or impaired mobility. The difficulty level of these common items served as a comparator in the selection process. The patients were invited to participate through their national patient organisations. The patients could enter the survey only if they stated that a diagnosis of AS had been made by a physician. The patients responded to the items of one of the five subsets (random selection) of the ASAS HI and provided information on sociodemographic (age, symptom and disease duration) and disease characteristics (Bath AS Disease Activity Index (BASDAI), Bath AS Functional Index, nocturnal back pain, total back pain and Bath AS Patient Global Score last week and 6 months, all on a 0–10 numerical rating scale).14–16
Expert consultation: After presentation of the results of the first postal survey, the steering committee experts reduced the item pool by deleting items which did not fulfil predefined criteria by a nominal consensus process. The selected items needed to fit the Rasch model, and they should not show differential item function (DIF) for age, gender and disease activity. Furthermore, items needed to represent the whole range and variety of the ICF Core Set for AS.
Second international cross-sectional survey: A cross-sectional international study was undertaken in English-speaking countries to investigate the reduced item pool. Patients were invited to participate in this web-based survey either through their national patient organisations or by their local rheumatologists. The methodology used in this survey was the same as described in the first postal survey–except for the reliability part that was included (T1, T2, time frame 2 weeks) in a subset of patients.
Consensus meeting: Based on the results of reliability assessments and Rasch analysis, the steering committee selected the best fitting items to create the final version. For items assessing functioning, emphasis was put on optimal targeting, the ability of items to differentiate between different levels of health, and optimal coverage of items to the variety of ICF categories of the Comprehensive ICF Core Set for AS. Agreement was achieved by a nominal consensus process.
The final version has been field tested in English-speaking countries to test for content validity, applicability and feasibility.
Statistics
Descriptive data are presented as mean±SD for quantitative variables and as absolute frequencies and percentages for qualitative variables. Rasch analyses were conducted after each survey to assess the overall fit of the model, individual item fit, the response scale used and presence of DIF in those items which belong to the functioning categories of the ICF. A DIF problem may be present when the response to an item worked differently in patient groups. In this study DIF was studied for person factors age, gender, disease activity, extraspinal manifestations, country and being employed. Rasch analyses were conducted in two random samples of the whole data set, resulting in an ‘evaluation’ and a ‘validation’ sample. The test-retest reliability of the items of the ASAS HI was analysed using κ statistics. Data analysis was performed with SPSS V.20.0 and RUMM2030.
RESULTS
This paper will deal only with the analysis of the categories representing a whole range of functioning of patients with AS. The results of the analysis of the EF item set will be described elsewhere.
Preparatory phase: 251 items which had been linked to 44 categories of the Comprehensive ICF Core Set for AS constituted the final item pool. The items were derived from 60 different questionnaires. A total of 76 items covered the 23 ICF categories from the component body functions, 122 items covered the 24 categories from the component activities and participation, and 53 items covered 14 categories of the EF.
Patient meeting: In August 2008, 13 patients with AS who were fluent in English originating from seven different countries (Canada (two), Germany (three), the Netherlands (two), Switzerland (one), Turkey (one), UK (two), USA (two)) discussed and weighted the item pool. The items were presented to the patients in blocks with one block representing one ICF category. The characteristics of the patients participating are given in table 2. Three of the patients were working as physicians. Ten items proposed by the patients were added to the item pool.
First international cross-sectional survey: A total of 1915 patients responded to the web survey, but 161 patients were excluded because of incomplete data. The characteristics of the remaining 1754 patients included in the analysis are shown in table 2. Rasch analyses were conducted in seven iteration cycles in which 62 items were removed because of misfit and 54 items because of DIF. Detailed results of the Rasch analysis will be published elsewhere.
Expert consultation: After careful consideration and discussion of the results of the first postal survey, the expert committee including one patient with AS decided to remove another 41 items. This was based on the following inclusion criteria for items of the draft version: a high χ2 probability value, representation of major ICF categories (eg, pain, maintain body position, sleep functions) and representation of the whole range of difficulty levels. Finally, the experts agreed on 50 remaining items representing a whole range of functioning abilities of patients with AS in the draft version.
Second international cross-sectional survey: A total of 705 patients responded to the second postal survey, 628 of which (89.1%) were invited by the patient organisations. Complete data sets of 611 patients were available for further analysis (table 2). Data from an additional 77 patients provided by rheumatologists from Canada, New Zealand, the UK and the USA also took part in the reliability study when they were judged by their rheumatologist to have a stable disease course at the moment of inclusion. There were differences between the patients recruited by the web survey and those recruited by their rheumatologists. Interestingly, patients included by rheumatologists had a comparable mean age and disease duration (data not shown) but lower disease activity and better physical functioning compared with the patients recruited by patient organisations. In four iteration cycles Rasch analyses identified misfit in 4 items and DIF in 15 items. More than 50% of the items showed a residual correlation between each other above 0.3 in the first round. However, after removal of 33 items the final iteration cycle showed a good targeting to the sample (figure 1). The item location was 0.00±1.8 with a fit residual of 0.06±1.2 and the person location was 0.01 ±1.8 with a fit residual of −0.30±0.7. The χ2 probability was 0.73 for the draft version. The reliability between individual items at T1 and T2 according to the κ coefficient ranged between 0.4 and 0.9. These results were confirmed with the validation sample.
Consensus meeting: After presentation of the results of the second postal survey, the steering committee decided to remove another 14 items–mainly because of existing residual correlation. No correlating items were allowed in order to avoid local response dependency. The final remaining 17 items fit the model without residual correlation and absence of constant DIF. The Person Separation Index was 0.82 (see table 3). These final 17 items represented all levels of functioning of patients and covered 15 out of 66 categories of the ICF Core Set for AS.
Table 2.
Demographic and disease characteristics of participants
| Patient meeting (n=13) | 1st postal survey (n=1754)*† | 2nd postal survey (n=687)*‡ | |
|---|---|---|---|
| Male (%) | 11 (84.6) | 929 (53.0) | 372 (54.1) |
| Age (years), mean±SD 56.8±13.3 | 48.3±13.4 | 48.3±14.1 | |
| Duration of disease (years), mean±SD | 35.3±13.2 | 22.8±14.0 | 20.4±13.8 |
| BASDAI, mean±SD | 2.6±1.5 | 5.5±2.4 | 5.4±2.4 |
| BASFI, mean±SD | No data | 4.6±2.6 | 4.5±2.6 |
| Total back pain (NRS 0–10), mean±SD | No data | 6.0±2.8 | 4.7±2.8 |
Analysis based on complete dataset regarding demographic questionnaires.
Patients from seven English speaking countries (Australia (n=24), Canada (n=255), Ireland (n=91), New Zealand (n=36), Singapore (n=40), UK (n=706) and USA (n=602)) represented four continents (Europe, America, Asia, Australia/New Zealand).
Patients coming from Canada (n=94), Ireland (n=81), New Zealand (n=39), Singapore (n=36), the UK (n=190) and the USA (n=248).
BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath Ankylosing Spondylitis Functional Index; NRS, numerical rating scale.
Figure 1.
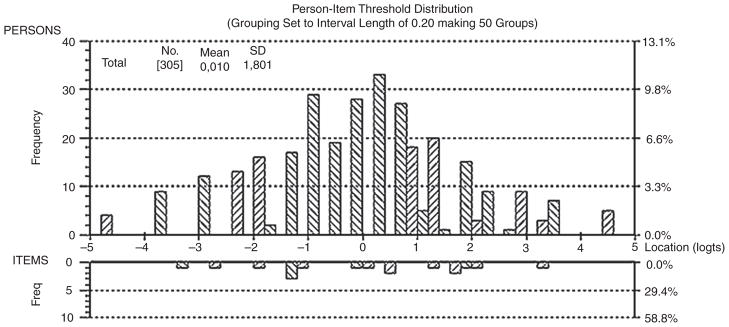
Person-Item distribution of the sample with the final 17 items. Interpretation of the figure: The horizontal line represents the latent trait ‘functioning’ according to the International Classification of Functioning, Disability and Health. The value of −3 means that a patient with a score result on the left side of the continuum has no major limitation in functioning. The lower the score, the better the ‘functioning’.
Table 3.
Details of the final 17 items of the ASAS HI
| Summary statistics | Person-Separation Index | χ2 Probability | Item location (mean±SD) | Item fit residual (mean±SD) | Person location (mean±SD) | Person Fit residual (mean±SD) |
|---|---|---|---|---|---|---|
| ASAS Health Index (final 17 items) | 0.82 | 0.73 | 0.0±1.8 | 0.0±1.2 | 0.0±1.8 | −0.3±0.7 |
| Categories | Difficulty level | Fit residual | χ2 probability | κ agreement | ICF | Origin |
| Pain | −3.3 | −0.9 | 0.77 | 0.6 | b280 | Patient proposal |
| Maintaining a body position | −1.3 | −0.5 | 0.67 | 0.7 | d415 | NHP, DFI, BASFI (adapted) |
| Moving around | −2.8 | −1.1 | 0.2 | 0.8 | d455 | DFI (adapted) |
| Toileting | 1.6 | 1.8 | 0.2 | 0.6 | d530 | RAQoL |
| Energy and drive | −1.9 | −0.3 | 0.4 | 0.8 | b130 | Patient proposal |
| Motivation | −1.2 | 0.2 | 0.3 | 0.7 | b1301 | MSQoL |
| Sexual functions | 0.6 | 0.7 | 0.9 | 0.9 | b640 | Patient proposal |
| Driving | 2.0 | −0.6 | 0.8 | 0.8 | d475 | Patient proposal |
| Community life | 1.8 | −0.8 | 0.7 | 0.8 | d910 | NHP |
| Moving around | 3.3 | 0.7 | 4.7 | 0.7 | d455 | HAQ-S (adapted) |
| Handling stress | 0.1 | −0.4 | 2.1 | 0.7 | d240 | RAQoL |
| Recreation and leisure | 0.4 | −1.5 | 7.2 | 0.7 | d920 | Proposal |
| Emotional functions | −1.2 | −1.5 | 5.3 | 0.8 | b152 | RAQoL, ASQoL |
| Washing oneself | 1.8 | 1.6 | 2.8 | 0.4 | d510 | ASQoL, HAQ (adapted) |
| Economic self-sufficiency | −0.01 | 2.2 | 2.9 | 0.8 | d870 | Environmental Status Scale (adapted) |
| Sleep | −1.2 | 2.1 | 4.9 | 0.8 | b134 | NHP, RAQoL |
| Handling stress | 1.2 | −0.5 | 1.0 | 0.6 | d240 | GHQ (adapted) |
ASAS HI, Assessment of SpondyloArthritis international Society Health Index; ASQol, Ankylosing Spondylitis Quality of Life; BASFI, Bath Ankylosing Spondylitis Functional Index; DFI, Dougados Functional Index; GHQ, General Health Questionnaire; HAQ-S, Health Assessment Questionnaire; ICF, International Classification of Functioning, Disability and Health; MSQoL, Multiple Sclerosis Quality of Life Inventory; NHP, Nottingham Health Profile; RAQoL, Rheumatoid Arthritis Quality of Life.
ASAS HI final version
Since the item selection has been carried out based on the Rasch Model, the responses to the 17 dichotomous items can be summed up to give a total score ranging from 0 to 17—with a lower score indicating a better and a higher score indicating an inferior health status. The ASAS HI sum score was calculated and tested in the population of the second postal survey. The mean sum score was 8.37±3.9 (range 0—17) with no relevant floor and ceiling effects (sum score 0 and 17 in only 1.0% of the population). The sum scores correlated significantly with BASDAI and total back pain (r=0.6) as well as with Bath AS Functional Index and Bath AS—patient Global Score (r=0.7), (all p<0.0001). Preliminary validity is also demonstrated by the distribution of the ASAS sum score stratified for different levels of disease activity and functioning (see table 4).
Table 4.
Distribution of the ASAS HI sum score stratified on different disease activity and functioning levels
| Group I (0–3.9)*
BASDAI (n=146) |
Group II (4–6)*
BASDAI (n=166) |
Group III (6.1–10)*
BASDAI (n=293) |
|
|---|---|---|---|
| ASAS HI mean±SD | 5.0±3.2 | 7.4±3.1 | 10.6±3.0 |
| Group I (0–3.9)* | Group II (4–6)* | Group III (6.1–10)* | |
| BASFI (n=256) | BASFI (n=152) | BASFI (n=195) | |
| ASAS HI, mean±SD | 5.7±3.0 | 8.5±2.8 | 11.7±2.8 |
| Group I (0–3.9)* | Group II (4–7)* | Group III (7.1–10)* | |
| Total back pain (n=205) | Total back pain (n=264) | Total back pain (n=131) | |
| ASAS HI, mean±SD | 5.6±3.4 | 9.0±3.1 | 11.4±2.9 |
On a numerical rating scale of 0–10.
BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath Ankylosing Spondylitis Functional Index; ASAS HI, Assessment of SpondyloArthritis international Society Health Index.
The ASAS HI has been endorsed by ASAS members at their annual meeting in January 2013 (38 positive votes, 1 negative vote, 3 abstentions from voting).
Field test
Forty patients (age 45.35±15.66 years, 70% male, 72% patients with AS, BASDAI 4.0±2.5), participated in the field test in four English-speaking countries (Australia, Canada, UK, USA). The final ASAS HI was well understood and only minor changes were necessary to obtain the final version of the ASAS HI (see online supplement and ASAS homepage),
DISCUSSION
This manuscript presents the development of the first disease-specific patient-reported outcome measure aimed at the measurement of overall functioning and health in patients with AS to be based on the ICF. This large effort has been undertaken under the auspices of ASAS in collaboration with the ICF research branch, resulting in the development of the ASAS Health Index (ASAS HI). This index presented here for the first time contains 17 patient-rated items, each with dichotomous ‘agree/do not agree’ response. A wide range of ICF categories are assessed including pain, emotional functions, sleep, sexual functions, mobility, self-care and community life. The ICF categories of the ASAS/WHO Comprehensive ICF Core Set for AS were only used to guide us to include the most important topics/categories from the patient point of view. The index is unidimensional and covers the content of the functioning part of the ASAS/WHO Comprehensive ICF Core Set for AS. We also present the preliminary data regarding truth and reliability of this health index that is now available in the public domain.
Existing instruments for patients with AS have focused on specific symptoms, physical function and health-related quality of life (HR-QoL).15,17 However, these tools cannot provide information about the whole range of common difficulties of patients with AS as defined by the ICF Core Set for AS, which was our conceptual basis and content validity standard during the whole process.2 This is what makes the process unique compared with the development of existing patient-reported outcome measures. In addition, we specifically aimed to ensure the unidimensionality of items according to the ICF concept.
It is important to emphasise that the ASAS HI is a health index and not a HR-QoL instrument. Health is thereby operationalised through the ICF concept of functioning. With the ASAS HI we capture whether problems are present in different categories of functioning and not the subjective experience of those problems. This differentiation is frequently not clear because the functioning categories that are assessed, such as pain and moving around, are the same, but they are captured from a different perspective. The functioning perspective is based on an objective description while the HR-Qol perspective is based on a subjective appraisal. Furthermore, existing AS-specific questionnaires usually cover aspects of physical function or mobility, but seldom address aspects of self-care or leisure activities which are considered important from the patient perspective.2,18,19
Patients provided a major contribution to the process of development of the ASAS HI by proposing concepts which they felt were not addressed within the existing item pool. Thus, 10 concepts proposed by patients were included in the final version of the ASAS HI addressing: ‘pain during normal activities’ to assess the ICF category pain (b280), ‘exhausting’ to assess the ICF category energy and drive (b132), ‘sexual functions’ to assess the ICF category sexual functions (b640) and ‘operating pedals in the car’ to address the ICF category ‘driving’ (d475). Altogether four patients with AS account for a dual perspective during the development process of the ASAS HI since these patients were also physicians (three rheumatologists, one ophthalmologist). Using their individual view on the complexity of global functioning, we benefit from their experience but at the same time have to face the limitation of a potentially missing objectivity. However, since only the minority of members have had a dual perspective we minimise the risk of biased opinion.
On initiation of the project in early 2008, the ASAS classifica-tion criteria for axial SpA (axSpA) and peripheral SpA had not been published.20,21 These patients were therefore not included in the early development phase of this study. The further validation of the ASAS HI will be addressed in an upcoming international study that has been designed to include patients with AS, non-radiographic axial SpA and with peripheral SpA.
As mentioned above, the ICF model also recognised the role of contextual factors representing the environmental and personal traits of the patients. We also engaged in the selection of EF which will be reported in a subsequent manuscript.
The main limitation of our study is that we included patients from patient support organisations and we cannot be entirely sure that such patients had a definitive diagnosis of AS. However, we tried to minimise this uncertainty by asking patients whether AS had been confirmed by a physician before they completed the survey.
In conclusion, the ASAS HI is a health index based on the ICF Core Set developed for patients with AS. This index forms an unidimensional scale providing a sum score representing all different levels of functioning.9,10 The items which comprise the ASAS HI represent a whole range of functioning of patients with AS, are unidimensional, independent from each other and unambiguous. Furthermore, the use of the ASAS HI seems feasible since it contains only 17 dichotomous items addressing categories of pain, emotional functions, sleep, sexual functions, mobility, self-care, community life and employment. The ASAS HI should soon be used in clinical trials and in clinical practice to test its real life performance and to confirm that this new composite index captures relevant information on functioning and health of patients with AS. It will require translation into other languages together with field testing to assess its applicability worldwide. It needs further studies to assess whether the ASAS HI can be used as a proxy to assess the global burden of disease in patients with axSpA.
Supplementary Material
Acknowledgments
The authors acknowledge the contributions of rheumatologists all over the world, especially from Jane Zochling (Australia) and Will Taylor (New Zealand). We acknowledge the contributions of the national patient organisation of Canada (Canadian Spondylitis Association (CSA)), UK (National Ankylosing Spondylitis Society (NASS)) and USA (Spondylitis Association of America (SAA)) as well as of Ankylosing Spondylitis International Federation (ASIF) Ireland.
Collaborators List of participants of the patient meeting (phase Ib): Campbell Barr, UK; Cor van Drogen, The Netherlands; Eric Eustance, UK; Ernst Feldtkeller, Germany; Britta Hattebuhr, Germany; Merryn Jongkees, The Netherlands; Uta Kiltz, Germany; Michael Mallinson, Canada; Ken Mulholland, Canada; Salih Özgocmen, Turkey; Michael Pianin, USA; Peter Staub, Switzerland; Michael Supancich, USA.
Footnotes
Competing interests
None.
Ethics approval Local ethics committee.
Provenance and peer review Not commissioned; externally peer reviewed.
Additional material is published online only. To view this file please visit the journal online (http://dx.doi.org/10.1136/annrheumdis-2013-203967).
References
- 1.Vander Cruyssen B, Ribbens C, Boonen A, et al. The epidemiology of ankylosing spondylitis and the commencement of anti-TNF therapy in daily rheumatology practice. Ann Rheum Dis. 2007;66:1072–7. doi: 10.1136/ard.2006.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Echteld I, Cieza A, Boonen A, et al. Identification of the most common problems by patients with ankylosing spondylitis using the international classification of functioning, disability and health. J Rheumatol. 2006;33:2475–83. [PubMed] [Google Scholar]
- 3.Ward MM. Health-related quality of life in ankylosing spondylitis: a survey of 175 patients. Arthritis Care Res. 1999;12:247–55. [PubMed] [Google Scholar]
- 4.Machado P, Landewé R, Braun J, et al. A stratified model for health outcomes in ankylosing spondylitis. Ann Rheum Dis. 2011;70:1758–64. doi: 10.1136/ard.2011.150037. [DOI] [PubMed] [Google Scholar]
- 5.The International Classification of Functioning Disability and Health. Geneva: World Health Organization; 2001. [Google Scholar]
- 6.Boonen A, Braun J, van der Horst-Bruinsma IE, et al. ASAS/WHO ICF Core Sets for ankylosing spondylitis (AS): how to classify the impact of AS on functioning and health. Ann Rheum Dis. 2010;69:102–7. doi: 10.1136/ard.2008.104117. [DOI] [PubMed] [Google Scholar]
- 7.Gordeev VS, Maksymowych WP, Evers SM, et al. Role of contextual factors in health-related quality of life in ankylosing spondylitis. Ann Rheum Dis. 2010;69:108–12. doi: 10.1136/ard.2008.100164. [DOI] [PubMed] [Google Scholar]
- 8.Boers M, Idzerda L, Kirwan J, et al. Towards a generalized framework of core measurement areas in clinical trials: a position paper for OMERACT 11. J Rheumatol. 2013 doi: 10.3899/jrheum.131307. (accepted) [DOI] [PubMed] [Google Scholar]
- 9.Cieza A, Bickenbach J, Chatterji S. The ICF as a conceptual platform to specify and discuss health and health-related concepts. Gesundheitswesen. 2008;70:e47–56. doi: 10.1055/s-2008-1080933. [DOI] [PubMed] [Google Scholar]
- 10.Cieza A, Hilfiker R, Boonen A, et al. Towards an ICF-based clinical measure of functioning in people with ankylosing spondylitis: a methodological exploration. Disabil Rehabil. 2009;31:528–37. doi: 10.1080/09638280802173475. [DOI] [PubMed] [Google Scholar]
- 11.Kiltz U, van der heijde D, Cieza A, et al. Developing and validating an index for measuring health in patients with ankylosing spondylitis. Rheumatology. 2011;50:894–8. doi: 10.1093/rheumatology/keq315. [DOI] [PubMed] [Google Scholar]
- 12.Cieza A, Brockow T, Ewert T, et al. Linking health-status measurements to the international classification of functioning, disability and health. J Rehabil Med. 2002;34:205–10. doi: 10.1080/165019702760279189. [DOI] [PubMed] [Google Scholar]
- 13.Cieza A, Geyh S, Chatterji S, et al. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2005;37:212–18. doi: 10.1080/16501970510040263. [DOI] [PubMed] [Google Scholar]
- 14.Calin A, Garrett S, Whitelock H, et al. A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol. 1994;21:2281–5. [PubMed] [Google Scholar]
- 15.Garrett S, Jenkinson T, Kennedy LG, et al. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21:2286–91. [PubMed] [Google Scholar]
- 16.Jones SD, Steiner A, Garrett SL, et al. The Bath Ankylosing Spondylitis Patient Global Score (BAS-G) Br J Rheumatol. 1996;35:66–71. doi: 10.1093/rheumatology/35.1.66. [DOI] [PubMed] [Google Scholar]
- 17.Doward LC, Spoorenberg A, Cook SA, et al. Development of the ASQoL: a quality of life instrument specific to ankylosing spondylitis. Ann Rheum Dis. 2003;62:20–6. doi: 10.1136/ard.62.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boonen A, van Berkel M, Cieza A, et al. Which aspects of functioning are relevant for patients with ankylosing spondylitis: results of focus group interviews. J Rheumatol. 2009;36:2501–11. doi: 10.3899/jrheum.090156. [DOI] [PubMed] [Google Scholar]
- 19.Sigl T, Cieza A, van der Heijde D, et al. ICF based comparison of disease specific instruments measuring physical functional ability in ankylosing spondylitis. Ann Rheum Dis. 2005;64:1576–81. doi: 10.1136/ard.2004.027185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68:777–83. doi: 10.1136/ard.2009.108233. [DOI] [PubMed] [Google Scholar]
- 21.Rudwaleit M, van der Heijde D, Landewé R, et al. The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis. 2011;70:25–31. doi: 10.1136/ard.2010.133645. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


