Abstract
Objective
Little is known about the information providers share with patients when ordering a co-test, or combined human papillomavirus (HPV) and Papanicolaou (Pap) test, for cervical cancer screening. We assessed provider perceptions of such communication practices with female patients aged 30–60 years.
Methods
We analyzed data from 98 providers in 15 Federally Qualified Health Center clinics across Illinois (2009–2010).
Results
About 70% of the providers reported that when ordering a co-test, they would usually or always communicate information about the HPV test to their patients, explain the test detects a sexually transmitted infection, and discuss how the test results may determine their next screening interval. Most (> 85%) reported that they were comfortable discussing co-test results. Compared with concordant positive results (HPV positive/Pap positive), providers were more likely to perceive that discordant results (HPV positive/Pap negative) would be too complex for patients to understand (25% vs. 15%, p = 0.006), and make patients feel less assured that they were getting the best standard of care (67% vs. 88%, p < 0.001).
Conclusion
As HPV testing plays a more prominent role in cervical cancer screening, more attention should be given to communications between providers and patients about the benefits and harms of different screening options.
Keywords: Cervical cancer screening, Human papillomavirus, Co-test, Communication practices
Introduction
Current cervical cancer screening recommendations state that average-risk women aged 30–65 years have a Papanicolaou (Pap) test alone every 3 years or a combination of human papillomavirus (HPV) and Pap test (i.e., co-test) every 5 years (ACOG Committee on Practice Bulletins-Gynecology, 2012, Saslow et al., 2012, US Preventive Services Task Force, 2012). The current recommendations have caused confusion among providers and patients about the appropriate screening options (Hawkins et al., 2013, Roland et al., 2013), presenting challenges in clinical implementation. Recent studies showed that the overall proportions of co-testing have gradually increased (Phelan et al., 2011, Tatsas et al., 2012), indicating that providers are incorporating the HPV test into their screening practices. As co-testing has become more prevalent, it is important to understand what information providers share with their patients when ordering the co-test. The study objectives were to assess provider perceptions of 1) their communication practices about the co-test, and 2) the risks and benefits of discussing co-test results with female patients aged 30–60 years.
Methods
The Centers for Disease Control and Prevention (CDC) launched the CDC Cervical Cancer (Cx3) Study to survey both provider and patient attitudes and beliefs regarding the co-test (Benard et al., 2014, Roland et al., 2013). The study was conducted in 15 clinics associated with six Federally Qualified Health Centers (FQHCs) across Illinois. FQHCs were selected as the study site because the client base is predominately low income and under- or uninsured, and assessing practices in these settings will help CDC provide technical assistance to its national cancer programs. Of note, the survey took place between 2009 and 2010, at which time the cervical cancer screening guidelines recommended screening every 3 years in women aged 30–65 years who had either a negative co-test or three consecutive negative screening tests (Smith et al., 2010). Baseline surveys were completed by 98 providers including physicians, nurse practitioners, certified nurse midwives, and physician assistants (89.9% response rate). Providers were eligible to participate if they personally performed Pap testing for routine cervical cancer screening. A $50 cash incentive was given to providers for their participation. This study was approved by CDC's Institutional Review Board.
Communication practices were assessed by asking a series of questions, with response options ranging from never to always: If you order a co-test, how often would you:
-
a)
Tell the patient that you are ordering an HPV test?
-
b)
Explain to the patient the purpose of an HPV test in relation to the Pap test?
-
c)
Explain to the patient that the HPV test detects a sexually transmitted infection?
-
d)
Discuss with the patient how HPV test results may determine when she will need to be screened for cervical cancer again?
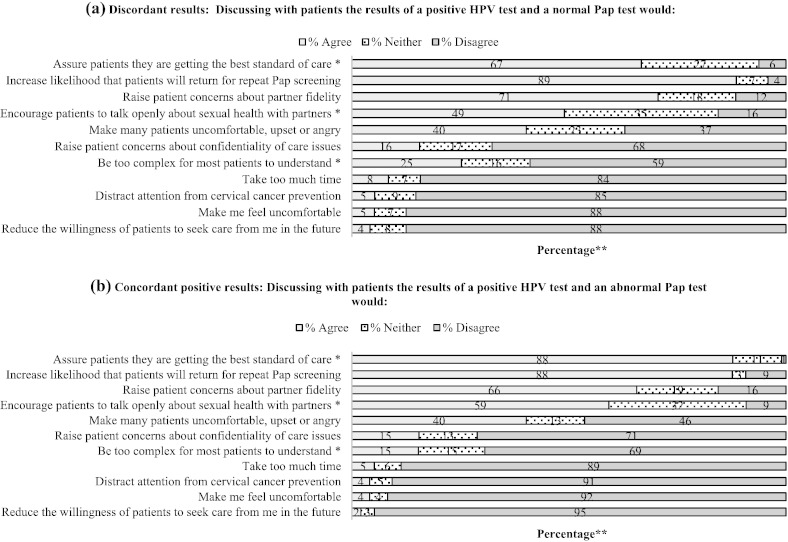
In addition, eleven statements were developed to assess provider perceived risks and benefits of discussing co-test results with patients (Fig. 1). Statements were presented in two sections: discordant results (HPV positive/Pap negative) and concordant positive results (HPV positive/Pap positive). Providers were instructed to indicate the extent to which they agree or disagree with each statement. For example, providers were asked if they agreed, disagreed, or were neutral regarding a discordant result statement such as, “Discussing with patients the results of a positive HPV test and a normal Pap test would… assure patients that they are getting the best standard of care.”
Fig. 1.
Provider perceived risks and benefits of discussing co-test results with female patients aged 30–60 years, 2009–2010 (n = 95–97).
Abbreviation: Pap = Papanicolaou test.
*Significant differences (p < 0.05) between provider responses to the discussion of discordant and concordant positive results.
**Percentages may not total to 100 because of rounding.
Notes: Two-tailed exact McNemar's test compares the proportion “agree” vs. “neither/disagree.” Study was conducted in 15 Federally Qualified Health Center clinics in Illinois, USA.
Descriptive statistics are presented for all measures. We used the exact McNemar's test to detect significant differences (p < 0.05) between provider responses to the discussion of discordant and concordant positive results. For the McNemar's test, responses were transformed into binary measures of “agree” vs. “neither/disagree.” Analyses were conducted using Stata (Release 13, StataCorp LP, College Station, TX, USA).
Results
Providers were predominantly female (77%). Most were physicians (66%) or nurse practitioners (20%), were trained in obstetrics/gynecology (53%) or family medicine (36%), and had an average of 8.8 years providing clinical care (N = 98, not reported in a table or figure).
When ordering a co-test, providers reported that they would usually or always explain the purpose of an HPV test in relation to the Pap test (75%), discuss how HPV test results may determine when the patient will need to be screened for cervical cancer again (75%), tell the patient that they are ordering an HPV test (72%), and explain that the HPV test detects a sexually transmitted infection (69%) (Table 1).
Table 1.
Provider reported communication practices about ordering the co-test, or combined human papillomavirus and Papanicolaou test, for female patients aged 30–60 years, 2009–2010 (n = 97).
| Discussion content | Always or usually | Half the time or sometimes | Never |
|---|---|---|---|
| Explain to the patient the purpose of an HPV test in relation to the Pap test | 75% | 21% | 4% |
| Discuss with the patient how HPV test results may determine when she will need to be screened for cervical cancer again | 75% | 23% | 2% |
| Tell the patient that you are ordering an HPV test | 72% | 23% | 5% |
| Explain to the patient that the HPV test detects a sexually transmitted infection | 69% | 27% | 4% |
Abbreviation: HPV = human papillomavirus.
Note: Study was conducted in 15 Federally Qualified Health Center clinics in Illinois, USA.
The perceived risks and benefits of discussing co-test results are shown in Fig. 1. Overall, providers reported that they were comfortable discussing co-test results with patients (discordant: 88%; concordant positive: 92%). Some risks perceived by providers included raising patient concerns about partner fidelity (discordant: 71%; concordant positive: 66%), and making them feel uncomfortable, upset, or angry (discordant: 40%; concordant positive: 40%). Compared with discussing concordant positive results, providers were more likely to perceive that discussing discordant results would be too complex for patients to understand (25% vs. 15%, p = 0.006), and make patients feel less assured that they were getting the best standard of care (67% vs. 88%, p < 0.001).
Discussion
About 70% of the 97 providers in our study reported that when ordering a co-test for cervical cancer screening, they would usually or always communicate information about the HPV test to their patients, explain that the test detects a sexually transmitted infection, and discuss how HPV test results may determine their next screening interval. However, in studies of patient perceptions of provider educational efforts regarding HPV, patients reported not being educated well during their routine exams (Blake et al., 2015, Cermak et al., 2010). They stated that specific HPV topics, such as the differences between the HPV and Pap tests, risk factors associated with HPV infection, and preventive measures were not mentioned (Cermak et al., 2010). It is therefore essential that information regarding cervical cancer screening options be provided to patients clearly, to ensure that patients understand the disease and their choices for management. Providers may also increase patient involvement in making clinical decisions that are consistent with individuals' preferences and values while promoting recommended guidelines. Strategies such as communication training, decision aids, or patient education may be warranted to facilitate this process (Harper, 2004).
Overall, providers in our study were comfortable discussing co-test results with patients. In comparison with the discussion of concordant positive results, providers were more likely to perceive that the discussion of discordant results would be too complex for patients to understand, and make patients feel less assured that they were getting the best standard of care. This could be because of the options available for follow-up management in the case of discordant results. Whereas women with concordant positive results are referred directly for colposcopy, women with discordant results either wait 12 months for repeat co-testing or undergo HPV genotype-specific testing for types 16/18, according to the current guidelines (Massad et al., 2013). Immediate referral for colposcopy for women with discordant results is not recommended because the risk for imminent cancer is low (Katki et al., 2011). However, one concern is that women may not return the following year, resulting in loss to follow-up, particularly for those with lower socioeconomic status (Saraiya et al., 2014).
Some commonly perceived risks inherent to the discussion of co-test results included raising patient concerns about partner fidelity, and making them feel uncomfortable, upset, or angry. The reported concerns are consistent with patient experiences on receiving an HPV positive result (McCaffery et al., 2006). One study found that the adverse social and psychological consequences resulting from testing positive for HPV were beyond those experienced by abnormal Pap test results alone (McCaffery et al., 2006). The sexually transmitted nature of the HPV virus has led to stigma, anxiety, and concern about sexual relationships (McCaffery et al., 2006). Emphasizing the high prevalence of HPV may reduce the negative psychosocial consequences of testing positive for HPV (Waller et al., 2007). Continued efforts are needed to educate patients about how common HPV is in the general population.
This is one of the few studies to assess provider communication practices about the co-test. Limitations of this study include the small sample size of providers, the use of self-reported data, and the primary focus on the perceptions of provider behaviors, as opposed to their actual practices. Providers were recruited from six FQHCs and are not meant to be representative of all FQHCs in Illinois. Further research may replicate the design of this study to compare with non-FQHC settings. The survey was conducted before the 2012 changes in practice guidelines and may not reflect provider responses to the revised recommendations. However, this is unlikely to have had a significant impact, as the guidelines advocated for less frequent screening with co-testing and recent literature continued to show that providers have been slow to adopt the changing guidelines (Teoh et al., 2015, Verrilli et al., 2014). This study in turn contributes to the literature by serving as a baseline for future studies aimed at assessing and improving provider communication practices about HPV testing. As HPV testing plays a more prominent role in cervical cancer screening, more attention should be given to communication between providers and patients about the benefits and harms of different screening options.
Conflict of interest statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The findings and conclusions in this report are solely those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Acknowledgments
This research was supported in part by an appointment (LL) to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and CDC. The study was supported by Contract Number 200-2002-00573, Task Order No. 0006 and No. 0017, from the Centers for Disease Control and Prevention to Battelle. The authors gratefully acknowledge the medical directors and administrators from the Federally Qualified Health Centers who participated in the study, and the Illinois Breast and Cervical Cancer Early Detection Program.
References
- ACOG Committee on Practice Bulletins-Gynecology ACOG practice bulletin number 131: screening for cervical cancer. Obstet. Gynecol. 2012;120:1222–1238. doi: 10.1097/aog.0b013e318277c92a. [DOI] [PubMed] [Google Scholar]
- Benard V.B., Saraiya M., Greek A. Overview of the CDC Cervical Cancer (Cx3) Study: an educational intervention of HPV testing for cervical cancer screening. J. Womens Health (Larchmt) 2014;23:197–203. doi: 10.1089/jwh.2013.4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake S.C., Andes K., Hilb L. Facilitators and barriers to cervical cancer screening, diagnosis, and enrollment in Medicaid: experiences of Georgia's Women's Health Medicaid Program enrollees. J. Cancer Educ. 2015;30(1):45–52. doi: 10.1007/s13187-014-0685-z. [DOI] [PubMed] [Google Scholar]
- Cermak M., Cottrell R., Murnan J. Women's knowledge of HPV and their perceptions of physician educational efforts regarding HPV and cervical cancer. J. Community Health. 2010;35:229–234. doi: 10.1007/s10900-010-9232-y. [DOI] [PubMed] [Google Scholar]
- Harper D.M. Why am I scared of HPV? CA Cancer J. 2004;54:245–247. doi: 10.3322/canjclin.54.5.245. [DOI] [PubMed] [Google Scholar]
- Hawkins N.A., Benard V.B., Greek A., Roland K.B., Manninen D., Saraiya M. Patient knowledge and beliefs as barriers to extending cervical cancer screening intervals in Federally Qualified Health Centers. Prev. Med. 2013;57:641–645. doi: 10.1016/j.ypmed.2013.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katki H.A., Kinney W.K., Fetterman B. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663–672. doi: 10.1016/S1470-2045(11)70145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massad L.S., Einstein M.H., Huh W.K. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Obstet. Gynecol. 2013;121:829–846. doi: 10.1097/AOG.0b013e3182883a34. [DOI] [PubMed] [Google Scholar]
- McCaffery K., Waller J., Nazroo J., Wardle J. Social and psychological impact of HPV testing in cervical screening: a qualitative study. Sex. Transm. Infect. 2006;82:169–174. doi: 10.1136/sti.2005.016436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan D.F., Boitnott J.K., Clark D.P., Dubay L.C., Gravitt P.E. Trends of human papillomavirus testing in cervical cancer screening at a large academic cytology laboratory. Obstet. Gynecol. 2011;118:289–295. doi: 10.1097/AOG.0b013e3182253c33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland K.B., Benard V.B., Greek A., Hawkins N.A., Manninen D., Saraiya M. Primary care provider practices and beliefs related to cervical cancer screening with the HPV test in Federally Qualified Health Centers. Prev. Med. 2013;57:419–425. doi: 10.1016/j.ypmed.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraiya M., Benard V.B., Greek A.A. Type-specific HPV and Pap test results among low-income, underserved women: providing insights into management strategies. Am. J. Obstet. Gynecol. 2014;211(4):354.e1–354.e6. doi: 10.1016/j.ajog.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saslow D., Solomon D., Lawson H.W. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J. Low. Genit. Tract Dis. 2012;16:175–204. doi: 10.1097/LGT.0b013e31824ca9d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R.A., Cokkinides V., Brooks D., Saslow D., Brawley O.W. Cancer screening in the United States, 2010: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J. Clin. 2010;60:99–119. doi: 10.3322/caac.20063. [DOI] [PubMed] [Google Scholar]
- Tatsas A.D., Phelan D.F., Gravitt P.E., Boitnott J.K., Clark D.P. Practice patterns in cervical cancer screening and human papillomavirus testing. Am. J. Clin. Pathol. 2012;138:223–229. doi: 10.1309/AJCPPVX91HQMNYZZ. [DOI] [PubMed] [Google Scholar]
- Teoh D.G., Marriott A.E., Isaksson Vogel R. Adherence to the 2012 national cervical cancer screening guidelines: a pilot study. Am. J. Obstet. Gynecol. 2015;212(62):e1–e9. doi: 10.1016/j.ajog.2014.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Preventive Services Task Force . 2012. Screening for Cervical Cancer: U.S. Preventive Services Task Force Recommendation Statement. [Google Scholar]
- Verrilli L., Winer R.L., Mao C. Adherence to cervical cancer screening guidelines by gynecologists in the Pacific Northwest. J. Low. Genit. Tract Dis. 2014;18:228–234. doi: 10.1097/LGT.0000000000000008. [DOI] [PubMed] [Google Scholar]
- Waller J., Marlow L.A., Wardle J. The association between knowledge of HPV and feelings of stigma, shame and anxiety. Sex. Transm. Infect. 2007;83:155–159. doi: 10.1136/sti.2006.023333. [DOI] [PMC free article] [PubMed] [Google Scholar]