Abstract
Physical inactivity constitutes the fourth leading cause of death worldwide. Health care providers (HCPs) should play a key role in counseling and appropriately referring their patients to adopt physical activity (PA). Previous reports suggest that active HCPs are more likely to provide better, more credible, and motivating preventive counseling to their patients. This review summarizes the available evidence on the association between HCPs’ personal PA habits and their related PA counseling practices. Based on relevant studies, a snowball search strategy identified, out of 196 studies screened, a total of 47 pertinent articles published between 1979 and 2012. Of those, 23 described HCPs’ PA habits and/or their counseling practices and 24 analytic studies evaluated the association between HCPs’ personal PA habits and their PA counseling practices. The majority of studies came from the United States (n = 33), and 9 studies included nonphysicians (nurses, pharmacists, and other HCPs). PA levels were mostly self-reported, and counseling was typically assessed as self-reported frequency or perceived self-efficacy in clinical practice. Most (19 out of 24) analytic studies reported a significant positive association between HCPs’ PA habits and counseling frequency, with odds ratios ranging between 1.4 and 5.7 (P < .05), in 6 studies allowing direct comparison. This review found consistent evidence supporting the notion that physically active physicians and other HCPs are more likely to provide PA counseling to their patients and can indeed become powerful PA role models. This evidence appears sufficient to justify randomized trials to determine if adding interventions to promote PA among HCPs, also results in improvements in the frequency and quality of PA preventive counseling and referrals, delivered by HCPs, to patients in primary care settings. Future studies should also aim at objectively quantifying the effect of HCPs’ PA role-modeling and how it influences patients’ PA levels. More evidence from low-to-middle income countries is needed, where 80% of the deaths due to inactivity and related noncommunicable diseases already occur.
Keywords: health care personnel, physical activity, lifestyle medicine, counseling
‘Physical inactivity ranks as the second leading cause of death worldwide and constitutes a priority target for global action to help control the rising burden of noncommunicable diseases.’
Physical activity (PA) recommendations encourage every adult to engage in at least 150 minutes a week of moderate to vigorous activity.1,2 Physical inactivity ranks as the fourth leading cause of death worldwide3,4 and constitutes a priority target for global action to help control the rising burden of noncommunicable diseases (NCDs).5 In 2010, almost one third of the world population was categorized as being physically inactive,6 and an estimated 5 million deaths worldwide could be attributable to inactivity.4
Reducing physical inactivity requires a “whole of society” approach, including environmental and policy changes to make physically active choices an easier choice for leisure or transportation purposes. Beyond the physical environment, changes in the “social” environment are also required, including cultural and social norms in relation to PA and the value populations and health care providers (HCPs) assign to PA.
Counseling by physicians and other HCPs has been shown to be useful in helping patients improve their lifestyles. When done adequately, HCP-initiated PA counseling is moderately effective, resulting in short-term (12 months) improvements in patients’ PA levels7,8 and has the potential to improve years lived free from disease.9 In addition, evidence suggests that schemes where PA counseling is done by a team of HCPs providing referrals to accessible community resources for PA can be cost-effective.10 Regular PA counseling by HCPs is included as a national public health objective in the United States (Healthy People 2020).11 Additionally, PA counseling and referral schemes are part of health care systems in the United Kingdom,10 Sweden,12 Switzerland,13 and Brazil.14 However, rates of PA counseling by physician and other HCPs still remain unacceptably low in those countries with available data.15-19
Many barriers have been identified as contributors to HCPs’ low rates of PA counseling, including inadequate knowledge, provider self-efficacy, office time constraints, lack of reimbursement, as well as intrinsic HCP factors, including poor personal habits.20,21 Although some studies show physicians’ lifestyle habits are relatively better when compared with those of the general population,17 there is less evidence on the personal habits of other HCPs involved in primary health care, such as nurses, physician assistants, social workers, dietitians, physical therapists, or exercise specialists. In addition, studies report that HCPs who engage in healthy habits such as not smoking, eating a healthy diet, or having periodic preventive health screenings and immunizations also provide preventive counseling to their own patients more frequently and more confidently,22-25 and their patients engage in related preventive practices more often.26 In addition, we and others have proposed that physically active HCPs will be more sensitive to the obstacles to starting or maintaining an active lifestyle and, therefore, may have higher success in initiating and sustaining counseling for their own patients on this topic.27-29
Based on the premise of “preach what you practice” and given that HCPs are one of the primary sources of preventive care information for the public, a better understanding of the relation between HCPs’ personal PA behaviors and their related counseling practices can help guide the development of interventions to promote active lifestyles among HCPs. In turn, these interventions may also help improve population health and reduce the risk of inactivity-related NCDs. Consequently, the purpose of this review is to summarize the evidence evaluating the role of health care providers as models for PA among their patients.
Methods
In 2010, the US Preventive Services Task Force (USPSTF) published an updated report of PA counseling in primary care, which included the latest evidence on PA interventions delivered in primary care settings. Results showed that, overall over an average follow-up of 12 months, counseling increased participants’ self-reported PA levels, by approximately 38 minutes per week, in randomized controlled trials (RCT) that provided at least medium-intensity interventions. Medium- to high-intensity PA counseling resulted in changes in self-reported PA. However, there was very limited evidence for maintenance of behavioral effects beyond 12 months, particularly for low- and medium-intensity interventions; so the Task Force concluded in 2012 that
although the correlation among healthful diet, physical activity, and the incidence of cardiovascular disease is strong, existing evidence indicates that the health benefit of initiating behavioral counseling in the primary care setting to promote a healthful diet and physical activity is small. Clinicians may choose to selectively counsel patients rather than incorporate counseling into the care of all adults in the general population.
Our framework for this review was based on the latest available evidence from the USPSTF review, which indicates that PA counseling by HCPs in primary care settings can be moderately effective in improving patients’ PA levels, at least in the short term. To inform our research, we summarized the information from the most recent USPSTF update regarding the effectiveness of PA behavioral counseling in the 31 RCTs included in the 2010 USPSTF review (Table 1). In addition, we went back to the original RCT reports to better understand which HCPs (physicians, nurses, health educators) were involved in providing the PA behavioral counseling and summarized that information in Table 1.
Table 1.
Summary of Available Evidence to Recommend PA Counseling by Health Care Provider and Setting (Adapted From USPSTFa).
| Author/Year/Country | Intensity/Quality of Intervention | HCP Involved in PA Counseling/Setting | Counseling Intervention Details |
|---|---|---|---|
| Aittasalo/2006/Finland | Low/fair | Physicians/Primary care | One counseling session with PCP with a subset receiving a pedometer |
| de Vet/2009/Netherlands | Low/fair | Self-assessment and intention to increase PA/Worksite | Questionnaire with section encouraging implementation plan for walking or self-selected activity, with a subset receiving 2 follow-up questionnaires |
| Grandes*/2009/Spain | Low/good | Physicians/Primary care | One brief counseling visit with PCP using Web-based software, additional visit offered, printed pamphlet |
| Goldstein/1999/United States | Low/fair | Physicians/Primary care | One brief counseling visit with PCP including PA prescription, follow-up session scheduled, monthly mailed materials, PCP training and materials |
| Halbert*/2000/Australia | Low/fair | Exercise specialist/Primary care | One visit with exercise physiologist with 3 follow-up mail or phone questionnaires (3, 6, and 12 months) |
| Katz/2008/United States | Low/fair | Physicians/Primary care | Special training for PA counseling for internal medicine residents |
| Marcus*/2007/United States | Low/fair | Health educators, computer and phone based/Home | Print or telephone individual tailored messages, 14 contacts over 12 months |
| Marshall/2003/Australia | Low/fair | Mailed booklet/Home | Mailed booklets and tailored letter |
| Napolitano/2006/United States | Low/fair | Mailed booklet/Community | Personalized letter with AHA booklet and another group received 4 tailored reports plus booklets |
| Pekmezi/2009/United States | Low/fair | Computer tailored/Community | Six monthly mailings including tailored manuals, pedometer, physical activity logs, and tip sheets |
| Stensel*/1994/United Kingdom | Low/fair | Not specified | Gradually build up walking until 20-25 min/d. Then increase to 40-45 min/d during the next 6 months |
| Connell*/2009/United States | Medium/fair | Behavioral-change counselors, videos, and newsletters/Home based | Fourteen individualized counseling phone calls over 6 months, videos, pamphlet, workbooks, and newsletters |
| Delichatsios/2001/United States | Medium/fair | Automated phone intervention)/Home based | Eighteen automated 10-minute phone calls over 6 months using phone-linked expert system |
| Elley*/2003/New Zealand | Medium/good | Physician/Primary care | One brief visit with general practitioner plus PA prescription, 3 phone calls from exercise physiologist, quarterly newsletters |
| Green/2002/United States | Medium/fair | Physician/Primary care | Tailored report from PCP, self-help workbook, three 20- to 30-minute phone calls |
| Greene/2008/United States | Medium/fair | Trained counselors (specialty not specified)/Community | Stage-based manual plus 9 newsletters, 3 phone calls with mailed tailored reports |
| Harland/1999/United Kingdom | Medium/fair | Health visitor/Primary care | IG1: Report from PCP, 40-minute motivational interview with specialty provider |
| IG2: IG1 + 30 vouchers for community leisure centers | |||
| IG3: IG1 + 5 additional visits with specialty provider | |||
| IG4: IG3 + 30 vouchers for community leisure centers | |||
| Hellenius*/1993/Sweden | Medium/fair | Physician/Primary care | One counseling visit with physician, offered aerobic exercise class 2-3 times per week (attendance not required) |
| Kallings*/2009/Sweden | Medium/good | Physician and health care professional/Primary care | One group session with physician, 1 individual counseling session with specialty provider including PA prescription |
| King*/2002/United States | Medium/fair | Health educator/Home based | One 30- to 40-minute counseling session with specialty provider, fourteen 15- to 20-minute phone calls |
| King*/2007/United States | Medium/fair | Health educator or automated computer system/Home based | Four 45-minute and two 15-minute counseling phone calls, multiple mailings |
| Kinmonth/2008/United Kingdom | Medium/fair | Trained facilitators (range of health professions)/Home based | Four 45-minute and two 15-minute counseling phone calls, postal contact for 7 months |
| Kolt*/2007/New Zealand | Medium/good | Physician/Primary care | Eight phone counseling sessions, mailed materials |
| Lawton*/2008/New Zealand | Medium/good | Nurse/Primary care | One brief motivational interview including PA prescription and 30-minute follow-up visit with primary care nurse; five 15-minute calls, from community exercise specialist |
| Marcus/2007/United States | Medium/fair | Health educator/community | Mailed booklets, 14 counseling phone calls |
| Martinson*/2008/United States | Medium/good | Activity coaches/Community | Four lectures, 1 group orientation, 23 phone calls, library or materials available or use, 3 motivational contests over 24 months, but not all completed at 6-month assessment |
| Morey*/2009/United States | Medium/good | Lifestyle counselor and physician/Primary care | One visit and 13 phone calls with health counselor, workbook, exercise, and in-person endorsement and individualized automated phone calls from PCP, quarterly tailored mailings |
| Norris/2000/United States | Medium/fair | Physician/Primary care | Counseling visit with PCP, phone call from research assistant; a subset received 3 additional phone calls |
| Pinto*/2005/United States | Medium/fair | Physician/Primary care | Brief advice by clinician, 3 in-person and 12 phone counseling sessions with health educator; mailed materials |
| Yates*/2009/United Kingdom | Medium/fair | Health educators/Primary care | Three-hour group session, two 10-minute follow-up sessions, and a subset received a pedometer |
| Stewart*/2001/United States | High/fair | Trained staff (not specified)/Primary care | Eleven group sessions, one individual session, booklets, phone calls from counselor, monthly newsletters |
Abbreviations: PA, physical activity; USPSTF, US Preventive Services Task Force; HCP, health care provider; PCP, primary care physician.
Adapted from Lin et al.30
Statistically significant.
Search Strategy
For this review, search terms such as “attitudes/habits,” “health personnel,” “health care providers,” “physical activity,” “exercise,” and “role model” were used to find articles evaluating the role of HCPs as models for PA among their patients in PubMed/Medline between 1979 and June 2012. The resulting articles were retrieved and an additional snowball literature search strategy was used31 to identify other sources and relevant articles. Selected articles came from observational studies describing HCPs’ PA habits, HCPs’ counseling practices, and/or analytic studies describing the association between HCPs’ PA habits and their counseling on PA. Studies that did not report a measure of HCPs’ personal PA habits (either self-reported or objectively assessed) or HCPs’ PA counseling practices (self-reported frequency of PA counseling, self-efficacy for PA counseling, attitude toward PA counseling, perceived relevance of PA counseling, or patient report of receiving PA counseling) were excluded. The resulting studies were organized based on characteristics such as country of origin, study design, population, PA assessment methodology, and main outcome measure.
Results
A total of 196 articles were screened from our search strategy, and of those, 47 were included in this review. Of the studies included, 23 described either the HCP PA habits or counseling practices and 24 studies evaluated the association between HCPs’ PA habits and their PA counseling practices (Figure 1).
Figure 1.
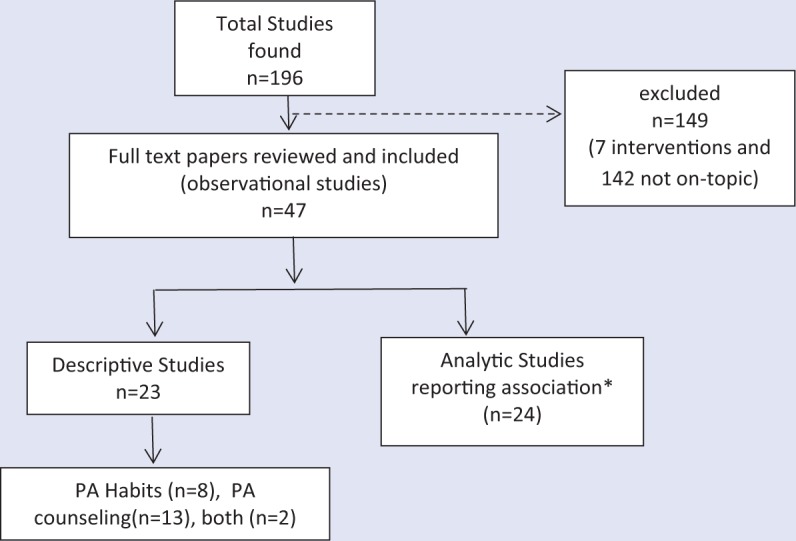
Overview of Included Studies.
Abbreviations: HCP, health care provider; PA, physical activity.
*Analytic studies that reported the association between HCPs’ PA habits and their PA counseling practices.
Most of the studies were conducted in the United States (n = 33). The rest took place in the United Kingdom (n = 6), Canada (n = 3), Spain (n = 2), India (n = 1), Colombia (n = 1), and the Netherlands (n = 1).
Several studies focused only on physicians (n = 35) while others (n = 9) included other HCPs such as nurses, dietitians, pharmacists, health educators, and health care staff in general. The rest (n = 3) were studies that included a multidisciplinary team of physicians and other HCPs. The most frequent PA assessment method was self-administered questionnaires, but there were also phone interviews and interviewer-administered questionnaires. Very few studies measured PA habits with objective methods. HCPs’ counseling practices and behaviors were mostly self-reported as perceived frequency or self-efficacy.
A total of 13 articles were published before 2000 (from 1984 to 1999), and the rest (n = 34) were published from 2000 to 2012. Studies done before 2000 (n = 13) were done mostly in physicians (n = 10) and the remaining (n = 3) in nurses; no other HCPs were included before 2000. There were no studies done in students before 2000, compared with the most recent findings after this date from medical and nursing students. Barriers reported for PA attainment did not differ from the old studies to the new ones published after 2000. Rates of PA counseling for studies published before 2000 were higher, ranging from 40% to 70%, compared to studies published after the year 2000, which found lower rates of PA counseling, ranging from 12% to 40%.
PA counseling was defined very differently from study to study, with some studies not defining clearly what method was used by the HCP to counsel their patients. Some studies defined counseling as the frequency of talking to their patients about PA or exercise habits (ie, “How frequently do you talk about PA with your patients?”),32-35 others defined it as a composite of measures between assessment (fitness, anthropometry) and education (providing pamphlets and discussion),36 and fewer studies went into details such as counseling for intensity and type of activity.36,37
Out of the 47 studies included in this review, all but one38 were cross-sectional and described either HCPs’ personal PA habits (n = 8), HCPs’ PA counseling practices (n = 13), both (n = 2), or the association between personal PA habits and related PA counseling (n = 24; Figure 1).
In Table 1, we summarized the USPSTF PA interventions offered by the 31 studies included in the latest review on PA behavioral counseling in primary care in particular as it related to the settings and type of HCPs providing the PA counseling. Out of 31 RCTs, 17 found a significant positive effect on participants’ PA levels. Out of those RCTs, health educators were primarily in charge of providing the PA behavioral counseling in 8 interventions, physicians in 6 interventions, nurses in 1 study, and technology-based approaches (Web-based, automated calls) in 2 interventions.
Physical Activity Habits of HCPs
Out of the 23 descriptive studies that reported PA habits or PA counseling practices (Table 2), 8 studies were identified that only described HCPs’ PA levels. Physicians reported higher compliance with current PA guidelines, ranging from 45% to 90%, while the reported compliance among other HCPs (nurses and dietitians) ranged from 39% to 70%.
Table 2.
Descriptive Studies Reporting HCPs’ Personal PA Habits, Their PA Counseling Practices, or Both, 1979-2012.
| Author | Year | Populationa | Location | Main Outcomeb | Results |
|---|---|---|---|---|---|
| Adelman et al32 | 2011 | P | United States | 2 | Exercise was discussed in 13% of visits and was raised equally by physicians and patients. Physician sex (female) and patient education (more than high school) were predictors of discussing exercise |
| Bazargan et al39 | 2009 | P | United States | 1 | Thirty-five percent of participants reported “no” or “occasional” exercise. Over 35% reported almost no or occasional exercise, while 63% of physicians claimed to engage in moderate (31%) to vigorous exercise (32%) for at least 1½ three times per week |
| Ferrante et al40 | 2009 | P | Canada | 1 | 90% reported being in good to excellent health. Averaged 4.7 hours of exercise per week |
| Painter et al41 | 2004 | H | United States | 2 | 24% never or rarely encourage patients to exercise; 72% of the respondents said it is not part of their responsibility to encourage PA |
| Williford et al33 | 1992 | P | United States | 2 | 91% encouraged patients to participate in regular exercise; 49% required exercise history as an initial examination. Only 23% familiar with ACSM guidelines |
| Chambers and Bowen42 | 1985 | P | United Kingdom | 3 | Only 11% said they do not participate in any PA at all, but the majority (85%) said they would like to do more than what they do now; 96% agreed that exercise is a great contribution to health. For PA assessment 55% only use history talking to record and assess PA |
| Blake et al43 | 2011 | H | United Kingdom | 1 | 45% met the current PA recommendations. Reported high level of knowledge, low levels of self-efficacy and social support to PA |
| Buchholz and Purath36 | 2007 | H | United States | 3 | 75% reported that they engaged in moderate PA 30 minutes most days of the week. Most ANPs (95%) counsel patients on PA at least once a year |
| Douglas et al44 | 2006 | H | United Kingdom | 2 | High level of reported PA given by nurses and HV. However, low knowledge of current recommendations |
| Douglas et al37 | 2006 | B | United Kingdom | 2 | Confidence and enthusiasm for prescribing PA was high but knowledge was low. Health visitors and nurses more likely than general practitioners to advice on PA |
| Galuska et al34 | 2002 | P | United States | 2 | Percentage of pediatricians that always counsel on PA was 41.4% (2-5 years old), 51.3% (6-12 years old), and 58.7% (13-18 year olds) |
| Anis et al45 | 2004 | P | United States | 2 | Counseling rates ranged from 0% in some offices to 55% in others. Counseling for dietary habits was associated with counseling for exercise (P < .05). Counseling was not associated with physicians’ age, years in practice, or number of patients per week |
| Janes et al46 | 1992 | B | Canada | 1 | More male physicians than female physicians reported exercising 3 times a week for 20 minutes (60% vs 46%) |
| Mullen and Tabak47 | 1989 | P | United States | 2 | Results indicated no relationships or weak relationships between counseling approaches and physician gender, year of graduation, board status, region, community size, practice type, average visit length, and patient characteristics |
| Rogers et al35 | 2002 | P | United States | 2 | Only 15.5% reported counseling more than 80% of the clinic patients about exercise and only 29% felt successful at getting their patients to start exercising |
| Van der Veer et al48 | 2011 | P | Netherlands | 1 | Nine percent of students did not meet the minimum amount of PA per week |
| Walsh et al49 | 1999 | P | United States | 2 | Two thirds of physicians reported asking more than half of their patients about exercise, 43% counseled more than half of their patients about exercise, but only 14% prescribed exercise for more than half of their patients. Only 12% were familiar with the new ACSM recommendations |
| Wells et al50 | 1984 | P | United States | 2 | Physicians reported counseling a narrower range of patients and less aggressively about exercise and alcohol than diet and smoking |
| Frank et al51 | 2006 | P | United States | 1 | Students exercised a median of at least 4 hours per week, and preferred strenuous exercise |
| Rao et al52 | 2012 | P | India | 1 | 61% reported current practice of PA (frequency/duration not specified) |
| Huang et al53 | 2011 | P | United States | 2 | Family physicians were less likely than pediatricians to provide guidance on PA. Women were more likely than men to provide guidance on PA independently of their specialty |
| Smith et al15 | 2011 | P | United States | 2 | Less than 50% reported always providing specific guidance on diet, PA, or weight control. PCPs were more likely to counsel on PA than on diet or weight control |
| Pronk et al54 | 2012 | P | United States | 2 | The knowledge of guidelines for PA was 70.9% among PCPs |
Abbreviations: PA, physical activity; FP, family practice; IM, internal medicine; PCP, primary care physician.
Population: P = physician; H = other health care provider; B = both.
Main outcome of the study: (a) HCPs’ PA habits, (b) HCPs’ PA counseling, and (c) Both.
We found 6 studies that reported PA habits and behaviors among medical (n = 5) or nursing students (n = 1).38,48,51,52,55,56 Medical students included in these studies, although not all samples were fully representative, also appear to have healthier habits than the general population, with less evidence from other HCPs. No information was found on studies evaluating the PA habits from other HCPs such as dietitians or social workers. For medical students, 4 studies were conducted in high-income countries (the United States, Spain, and the Netherlands) and 2 in low- to middle-income countries (India and Colombia). A study of medical students performed in 10 medical schools in Colombia (n = 661) found that half of first- and fifth-year students complied with PA guidelines.56 The study also reported that 85% and 91% of first- and fifth-year students respectively, had a positive attitude toward always counseling patients about PA. Frank et al38,57 also studied PA habits and behaviors of medical students in the United States. In her study, which included 17 medical schools (n = 1906), students reported engaging on average in 80 minutes/week of moderate exercise and 100 minutes/week of vigorous exercise, with 74% of the sample meeting PA guidelines. In contrast, a study from Spain55 found female nursing students to be somehow less active than students in non–health disciplines; however, these differences were not statistically significant: 50% physical inactivity among first-year nursing students, 47.5% among last-year nursing, and 43.6% among nonnursing students. Overall, the studies report that in general medical students complied with current PA recommendations (average between 70% and 90%). One study among nursing students showed higher rates of physical inactivity; however, the results were less consistent.
Physical Activity Counseling Among HCPs
We identified a total of 15 studies* (Table 2) describing the self-reported frequency, self-efficacy, and attitudes of HCPs toward PA and exercise counseling. The majority of studies (n = 12) included physicians or medical students’ PA counseling, 1 included a sample of both physicians and nonphysicians, and 2 included other HCPs such as nurses, social workers, and dietitians. We found several enabling factors for HCPs to counsel on PA and these were consistent among physicians and nonphysicians. Factors included higher patient level of education,32 being a female HCP,32,34,53 primary care specialty,15,49,53 and in some cases provider’s age >35 years.49 Specifically, a study with older adults found female physicians who cared for patients with a higher education (more than high school) to be significant predictors of the physicians’ likelihood of providing PA counseling among older patients.32
Very few studies reported nonphysician HCPs’ counseling for PA36,37,41,44; however we found that these groups, especially nurses and social workers, include regular preventive counseling recommendations more frequently than physicians into their practice.
HCPs Continue to Be Often Ill Prepared for PA Counseling
Callaghan reported that nurses who exercised in the previous week were more likely to rate exercise as important to health (P < .0003) and thus recommend it more to their patients.58 Douglas et al37 found UK nurses and health visitors were more likely to recommend PA to their patients than physician assistants, even when knowledge of current PA recommendations was very low: 13% of general practitioners, 9% of health visitors, and 7% of nurses described correctly current PA recommendations. For all studies found, knowledge of current PA recommendations was low and ranged from 12% to 27% among physicians and from 7% to 9% among other HCPs.
In terms of who is responsible for providing PA advice, a study among internal medicine residents35 found that more than 90% felt it was the physicians’ responsibility to counsel patients on exercise but only 15% of the residents reported counseling their patients. On the other hand, a study among dietitians, nurses, patient care technicians, and social workers showed that 72% of the respondents did not think it was their responsibility to encourage PA among their patients.41
The most common perceived barriers for not counseling on PA were similar among physicians and nonphysician HCPs. We found a total of 7 studies reporting HCPs’ most frequent barriers to counsel on PA, all of them from either the United States or the United Kingdom. The most frequent reported barriers were lack of time,35,36,44,49,59 HCPs’ low self-efficacy for PA counseling,41,49,59 lack of PA counseling materials,60 lack of reimbursement,36,37 lack of knowledge and counseling skills,37,41,44,60 and patient’s comorbidities.35
Association Between HCPs’ Personal PA Habits and Their Related PA Counseling Practices
In this review, we found a total of 24 analytic studies (Table 3) describing HCPs’ own PA habits as a correlate of the PA counseling they provide to their patients. Out of these 24 studies, 19 reported a significant positive association between HCPs’ PA habits and counseling frequency, self-efficacy, or perceived importance. The remaining 5 studies either did not report a measure of association61-63 or had nonsignificant results, although a trend was observed toward a positive association.55,56
Table 3.
Analytic Studies That Have Evaluated the Association Between HCPs’ Personal PA Habits and Their Related PA Counseling, 1979-2012.
| Author | Year | Study Design | Populationa | Specialty | Location | PA Assessment | Counseling Assessment | Results |
|---|---|---|---|---|---|---|---|---|
| DuMonthier et al61 | 2009 | CS | P | Chiropractic students/faculty and staff | United States | ACSM/AHA recommendations for aerobic and muscular strength | Perception of importance for counseling in PA | 74.8% reported having moderate to vigorous weekly PA; 76% felt role modeling and patient education is a very important attribute for chiropractors |
| Abramson et al59 | 2000 | CS | P | FP, pediatricians, geriatricians, IM | United States | Frequency, duration and intensity of PA | Percentage of patients counseled regarding each type of exercise and amount of time devoted | Physicians who performed aerobic exercise regularly were more likely to counsel patients about aerobic exercise than those who did not (OR 5.72, CI 2.41-13.54; P < .0005) |
| Sherman and Hershman64 | 1993 | CS | P | IM | United States | Physician resting heart rate | Frequency of counseling about PA | Physicians that exercise ≥3 times per week (OR 2.69, CI 1.50-4.85) and physicians with higher resting heart rate (<65 bpm) counseled more patients on PA (OR 3.4, CI 1.46-8.18) |
| Frank et al65 | 2010 | CS | P | PCP and non-PCP | Canada | Frequency, duration and intensity of PA | Frequency of counseling (usually/always/never) | Physicians that counseled frequently on PA were more likely to strongly agree that a physician that exercises is a better role model (P < .0001) |
| Frank et al20 | 2003 | CS | P | PCP and non-PCP | United States | Frequency, type and duration of PA | Frequency of counseling | Physicians who comply with ACSM recommendations were more likely to counsel patients on exercise in every visit (P < .004) |
| Binns et al66 | 2007 | CS | P | Pediatricians | United States | Self-report of subjective measures on physical fitness and health | Assessment and counseling of PA (frequency) | Healthy and fit pediatricians more routinely recommended PA (OR 3.2, CI 1.6-6.3) and assessed TV viewing (OR 4.4, CI 2.0-10.1) |
| Callaghan58 | 1999 | CS | H | Nurse | United Kingdom | Frequency of self-reported exercise measure (exercise in the previous week) | Nurses’ health beliefs about counseling | Nurses who rated the importance of PA to health as high also reported exercising more than those who rated it lower (P < .0003) |
| Duperly et al56 | 2009 | CS | P | Medical students (1st and 5th year) | Colombia | Frequency and duration of PA | Perceived relevance of counseling in their medical practice | Medical students that complied with PA guidelines (≥150 min/week of moderate to vigorous PA) had a better attitude toward counseling than students that did not comply with the guidelines. Not statistically significant (OR 1.4, CI .88-2.25) |
| Esposito and Fitzpatrick67 | 2011 | CS | H | Nurse | United States | PA subscale of the HPLP-II | Counseling regular exercise for health promotion (1-10 scale) | Significant correlation between PA habits and teaching for health promotion (r = .20, P = .03) as well as teaching as part of a treatment plan (r = .25, P = .007) |
| Frank22 | 2004 | CS | P | Students | United States | Frequency, type, and intensity (achieving or not achieving ACSM recommendations) | Perceived relevance of intended exercise practices | Medical students that spent more time doing strenuous exercise were more likely to report exercise counseling as highly relevant to their practice (OR1.1, CI 1.2-1.7, P < .0027) |
| Frank et al38 | 2008 | Prospective | P | Students | United States | Frequency and duration of PA | Perceived relevance of counseling and self-reported counseling | Those who comply with CDC PA recommendations were more likely to rate exercise counseling as highly relevant (P < .04) and always or usually counsel on PA (P < .008) |
| Howe et al68 | 2010 | CS | P | IM, FP, endocrinologists, cardiologists | United States | Frequency and duration (compliance of ACSM guidelines) | Frequency of counseling PA | Providers’ own exercise time of >150 minutes per week was a strong predictor for providers increased confidence in counseling (P = .01) |
| Harsha et al62 | 1996 | CS | P | Not specified | United States | Patients’ perception of physician exercise level | Patients perception of influence by counseling | 70% of the respondents said they would be more willing to exercise if their physician exercised regularly |
| Irazusta et al55 | 2006 | CS | H | Nursing students | Spain | VO max, vertical jump, and PA self-assessment for frequency and intensity | Competence (knowledge) regarding PA counseling | Increase (not significant) in the percentage of students who were competent to prescribe adequate PA counseling from the sedentary group (17.2%) to the active group (36.4%) |
| Lewis et al69 | 1986 | CS | P | FP, IM, IM subspecialties, ob/gyn | United States | Perception of exercise compliance (if he/she gets “enough” exercise) | Perception of when and how they counsel patients | Physicians that think get enough exercise counseled more patients and more frequently (significant association—not shown) |
| Livaudais et al70 | 2005 | CS | P | FP, IM, ob/gyn | United States | Frequency and duration of PA | Percentage of patients counseled in the past year about PA | When compared with very active physicians, sedentary physicians were less likely to counsel their patients about PA (OR 0.41, CI 0.23, 0.74, P < .01) |
| Rogers et al71 | 2006 | CS | P | IM residents | United States | Treadmill fitness testing, 7-day PA recall | Self-reported counseling and self-efficacy | Greater perceived success in counseling reported was associated to greater self-efficacy in the ability to personally engage in regular PA (r = .37, P = .007) |
| Connolly et al63 | 1997 | CS | H | Nurse | United States | Frequency, type, duration questionnaire | Self-reported counseling | 76% reported exercising frequently and 70% also said they would recommend their lifestyle to their patients |
| Frank et al72 | 2007 | CS | P | Students | United States | Personal health index measure (PA, smoking, diet, alcohol). Frequency, intensity and duration of exercise | Perceived counseling relevance score and perceived counseling frequency score | Those with better health behaviors (by PHI measure) were more likely to think counseling is relevant to their practice (P = .0001) and reported counseling more frequently (P = .0001). *No dissociation of PHI it is a composite measure of PA, diet, smoke, alcohol |
| Frank et al73 | 2000 | CS | P | PCP and non-PCP | United States | Frequency, duration and type | Self-reported counseling practices, relevance and self-confidence | Women physicians reporting practicing exercise had a significant correlation of counseling at least once a year about exercise (P < .05) |
| Lewis et al74 | 1991 | CS | P | IM | United States | PA frequency and intensity | Self-reported counseling practices | Being very active was a predictor for internists to counsel PA among their inactive patients (P ≤ .05) |
| McDowell et al75 | 1997 | CS | H | Nurse | United Kingdom | Stage of change for own PA habits | Stage of change for PA promotion | Correlation between being physically active and promoting PA was statistically significant (r = .26, P < .001) |
| Puig-Ribera et al76 | 2005 | CS | B | Physicians, nurses | Spain | Stages of change for personal PA behavior | Self-reported promotion, perceived priority | Stage of change for personal PA (either in action or maintenance) was positively associated with current PA promotion (χ2 = 15.16, P < .05) |
| Frank et al73 | 2000 | CS | P | Not specified | United States | NA | Patient motivation and perceptions of physicians disclosing healthy behaviors | Viewers of the physician disclosure video considered the doctor to be more believable (P < .002) and motivating to do PA (P < .001) |
Abbreviations: PA, physical activity; CS, cross-sectional study; FP, family practice; IM, internal medicine; PCP, primary care physician; OR, odds ratio; CI, confidence interval.
Population: P = physician; H = other health care provider; B = both.
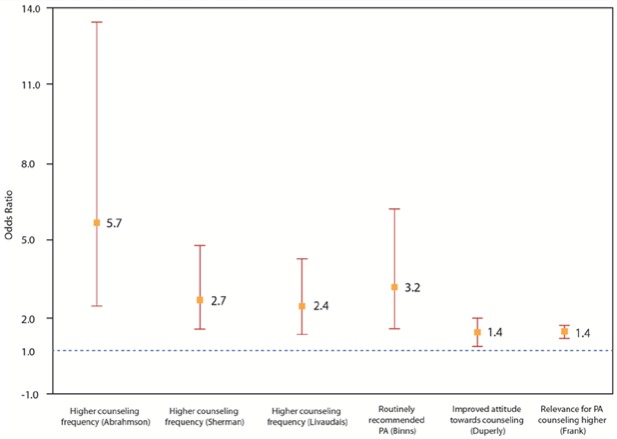
Figure 2 shows 6 studies found in this review that allowed a head-to-head comparison. These were studies that reported an odds ratio (OR) as a measure of the association between physicians self-reported PA habits and their PA counseling attitudes and practices, after controlling for potential measured confounders. Five out of these 6 studies reported a significant positive association, suggesting that physicians’ personal PA levels are a consistent and independent correlate of their PA counseling attitudes and practices (ORs ranging between 1.4 and 5.7; all P < .05). Other studies reported a significant positive association between the regularity and intensity of HCPs’ PA and the frequency with which they counseled their patients about PA.*
Figure 2.
Association Between Physicians’ Personal PA Levels and Their Attitudes and Practices Toward PA Counseling.a
aOR = odds ratio. OR reported by 6 analytic studies that allowed a face-to-face comparison. These studies included only physicians. Association (OR) between physicians’ physical activity (PA) levels and related counseling practices. PA levels were determined by self-report or fitness tests. Only observational (n = 6) studies were included. All the studies except one (“improved attitude toward counseling”) reported a statistically significant association (P < .05).
Active HCPs Provide More and Better PA Counseling Irrespective of Specialty or Time in Practice
With regard to physicians’ specialty, we found studies evaluating family practitioners, pediatricians, geriatricians, and internists,59,69,70,74 and they found the same positive association between personal PA habits and counseling provided on PA. Even those who perceived themselves as healthy and fit recommended PA more frequently (OR 3.2, CI 1.6-6.3) and assessed sedentary behavior such as TV viewing (OR 4.4, CI 2.0-10.1) more frequently among their patients.66 Frank has studied this association in-depth, among Canadian physicians,65 US physicians,20 and medical students.38 Among a sample of female physicians in the United States, those who complied with PA recommendations were more likely to counsel patients about exercise (P = .004).20 Canadian physicians reported a positive association between attitudes toward being a role model for their patients and higher frequency of PA counseling (P < .001).65 Another study64 used resting heart rate as a proxy for cardiorespiratory fitness among physicians and found that those who reported counseling less frequently about PA had higher resting heart rates (OR 3.4, CI 1.46-8.18).
The association between frequency of counseling and PA habits was found among nurses too. McDowell et al75 observed a sample of nurses in the United Kingdom and found that there was a correlation between nurses categorized as “active” and their PA counseling frequency (r = .26, P < .001). Puig-Ribera et al,76 in Spain, reported a positive association between active nurses and higher frequency of PA counseling (P < .05). Esposito and Fitzpatrick found a significant correlation between registered nurses’ PA habits and increased health promotion activities (including PA counseling) among their patients (r = .20, P = .03).67 Connolly and colleagues found that 76% of nurses reported exercising regularly, and among those, 70% would recommend their lifestyle to their patients.63
Some studies among nursing and medical students show that even early in their training, there is an association between HCPs’ personal lifestyles and what they will preach in their future clinical practice. Frank et al showed, as part of the “Healthy Doctor = Healthy Patient” project, in a cross-sectional sample of 17 US medical schools, that first-year students who reported more vigorous exercise had a more positive attitude toward counseling for exercise in their future practice.57 Students were followed-up for 4 years and it was found that those who complied with the PA guidelines were more likely to rate exercise counseling as important (P = .04).38 Additionally, more students thought exercise counseling was highly relevant for their future clinical practice at their entry-to-ward year than in their senior year (69% vs 53%, P < .01). Duperly et al56 replicated some aspects of the “Healthy Doctor = Healthy Patient” study in a sample of Colombian medical students, and even though the association between higher PA levels and better attitudes toward PA counseling was not statistically significant, the association was found for other health habits (better diet, not smoking, non–binge drinking) and related counseling. Among a sample of nursing students in Spain,55 a lower proportion of inactive students felt competent to prescribe PA (17.2%) compared with the proportion among active students (36.4%).
Patients Find Active HCPs’ Counseling More Compelling
From the patients’ perspective, HCP habits appear to be also influential. Harsha et al62 surveyed patients from a University Family Practice Center and found that 70% of patients said they would be more willing to exercise if their physicians also exercised regularly (P < .01). Patients were also more willing to comply with exercise recommendations if the recommending physicians were a family practitioner or a cardiologist. Patients in this study who met the PA guidelines were more willing to comply with their physicians if he or she exercised (P < .05) and almost 85% of them were more willing to comply if their physicians gave them a written exercise prescription. Frank et al73 showed 2 brief videos about improving diet and PA to a group of patients. In one video the physician disclosed information about his or her diet and exercise personal habits and included a bike helmet and an apple visible on their desk; in the second video, the physician did not disclose any personal habits (control video). Patients who viewed the physician-disclosure video considered the physicians to be healthier (P = .001), more motivating (P = .001), and more believable (P = .002) than those patients that were exposed the control video.
Perceived importance, success, or self-efficacy was also associated with HCPs’ own PA habits: nurses who rated PA as highly important for their practice also reported exercising more than those who rated it lower (P < .0003).58 Two other studies found a significant association between providers who complied with the PA guidelines and increased confidence in counseling (P = .01)68 and greater perceived success in counseling PA to their patients (r = .37, P = .007).71
Discussion
This literature review is a comprehensive evaluation of HCPs’ PA levels, the counseling they give patients, and the influence HCPs’ own personal habits may have on their PA counseling practices. Similar to other preventive measures such as smoking cessation, alcohol consumption, diet improvement, regular health screenings, or vaccinations,69,74,77 the available evidence shows that physicians and HCPs’ personal habits are a key, independent correlate, and may predict the manner in which they counsel and influence their patients’ behaviors on related health habits. For example, physicians who do not smoke are more likely to encourage patients to quit smoking.78 In a recent study26 among 1488 primary care physicians and their adult patients (n = 1 886 791), 8 different screening and vaccination preventive practices were objectively assessed using electronic medical records. Patients whose physicians were compliant with the preventive practices were significantly more likely to also have undergone these preventive measures, than patients with noncompliant physicians. For example, among patients whose physician had received the influenza vaccine, 49.1% of eligible patients received flu vaccines compared with 43.2% of patients whose physicians did not receive the vaccine (5.9% absolute difference, 13.7% relative difference). Additionally, physicians who are trying to improve their health habits counsel significantly more and with more confidence on that specific habit than HCPs not attempting to improve their behaviors.69 It has even been suggested79 that physician wellness, including PA levels, should be routinely measured in health systems as a quality indicator. This review found evidence to support the hypothesis that physically active HCPs, including those in the process of becoming more active, are more likely to counsel more frequently and more confidently about the importance of PA to their patients. Therefore, efforts to improve HCPs’ PA habits may not only benefit their health, but may also be an avenue to improve the frequency and quality of PA preventive counseling that patients and the general population receive. Such an approach, coupled with established referral mechanisms for community PA opportunities, can be effective in helping reduce inactivity, the fourth leading cause of death globally.5
Out of 24 analytic studies found in our review that examined the association between HCPs’ personal habits and counseling practices, 19 reported statistically significant positive associations. Despite the existence of prevailing barriers to PA counseling by HCPs and the fact that there are other factors associated with the frequency and quality of HCPs’ PA counseling to patients,80 HCPs’ personal PA habits were found to be a consistent correlate of counseling. In studies that allowed a head-to-head comparison, a measure of the magnitude of this association (OR) was found to range between 1.4 and 5.7.* Furthermore, this association was reported for physicians versus other HCPs, practicing or in-training HCPs, in different countries, health care systems, and settings, suggesting that the connection between HCPs’ habits and their PA counseling practices is consistent. The extent to which provider-initiated PA counseling can be translated into behavioral change among patients is modest and opens opportunities to further research. However, physicians and other HCPs are in a privileged position to provide PA advice as they are one of the first and most trusted sources of health information for patients, and some studies have described patients’ willingness to change a health behavior if their provider has a healthier, active lifestyle.73
There Is a Lack of Global Data on Rates of HCP PA Counseling, and When They Are Assessed, Rates Are Often Unacceptably Low
Evidence indicates that physicians report having better health habits than the general population, including slightly higher compliance with PA guidelines, although still far from optimal.17,81,82 This is important since active physicians can be role models for patients and be more credible and motivating to help them adopt or maintain an active lifestyle. However, and partly because of HCPs’ PA habits have room for improvement, PA counseling rates by HCPs still remain unacceptably low in many countries. For example, it is estimated that less than 40% of US primary care providers provide regular counseling on PA, even though PA counseling is a national health objective and many physician professional and scientific organizations recommend counseling on PA.83 On the other hand, more information is needed on the PA habits of HCPs other than physicians. Some studies report that nurses are somewhat more active than the general population, but when compared with physicians, studies show they have poorer health habits and report more barriers to engage in PA.43,46 However, nurses do report being more motivated and are enthusiastic about counseling on PA, and they ranked exercise as an important strategy to address NCDs among their patients.37 Of interest, RCTs that have been shown to be effective in improving PA levels via primary care–based PA behavioral counseling as part of the 2010 USPSTF review update, included interventions delivered mostly by health educators and physicians and in one study by nurses. These data emphasize the need to incorporate strategies to support all HCPs’ PA habits as part of interventions to improve PA counseling in primary care and referral schemes.
Many System and Personal Barriers Hinder HCP PA Counseling Efforts
Our literature search also explored HCPs’ perception of barriers to provide counseling, mainly lack of time and low self-efficacy. A recent systematic literature review80 on the perceptions of providers show physicians and nurses rank PA counseling as very important and agree that they should be involved in counseling activities; however, lack of needed skills, training, time, and reimbursement are still noted as important barriers to provide counseling. A persistent finding among all HCPs is the low level of knowledge on basic PA guidelines for health and the lack of training on simple exercise prescriptions, despite global efforts to elevate the status of PA as key for the prevention and management of NCDs.84-86 These findings highlight the importance of critically assessing and improving the lifestyle medicine and health promotion curriculums of medical and health sciences schools globally. One approach that needs to be thoroughly evaluated could be to implement continuing medical education programs for physicians and other HCPs on the basics of PA counseling. On this end, initiatives such as Exercise is Medicine,87-89 which aims to make PA assessment (PA “vital sign”), prescription, and referral an integral part of medical practice in the United States and globally, have the potential to effect change if implemented at a large scale and in addition to other environmental and community approaches.90 There is no “silver-bullet” to solve the global inactivity epidemic. An “all of the above” and “whole of society” approach, including PA counseling and referral in the health care context, will be required.91,92
PA Counseling Is Not Standardized Across Studies
The majority of the studies included in this literature review had limitations because of their self-reported nature. PA habits and counseling were generally assessed through self-reports and very few studies used objective measures for activity or PA counseling.55,64,93,94 Additional studies that validate HCPs’ self-reports on counseling practices, possibly cross-checking with medical records or patients’ perceptions, and objective measures of HCPs’ PA levels are needed in order to decrease bias due to the desirability of HCPs to score well in both categories. Another limitation is the heterogeneity with which many studies reported both PA levels and counseling attitudes and practices, which prevented a more quantitative approach to summarizing the evidence using meta-analytic techniques. Finally, there is risk of under-ascertainment of studies since the literature review focused only in one database published in English or Spanish.
Health care providers’ health is not only important for their own benefit but also because of the potential positive effects it may bring to their patients. This review found that HCPs may preach what they practice and those that are active are more likely to advice PA to their patients. Increasing PA levels among HCPs may be an additional intervention that, in addition to other public health and clinical strategies, may help reduce inactivity levels in the general population.
In conclusion, this review found consistent evidence supporting the notion that physically active physicians and other HCPs are more likely to provide PA counseling to their patients and can indeed become powerful PA role models. This evidence appears sufficient to justify randomized trials to determine if adding interventions to promote PA among HCPs, also results in improvements in the frequency and quality of PA preventive counseling and referrals, delivered by HCPs, to patients in primary care settings. Future studies should aim at objectively quantifying the effect of physicians’ PA role-modeling and how it influences PA in their patients. Specifically, whether promoting PA among HCPs can independently result in meaningful increases in the PA levels of patients, or potentiate the effect of interventions to address barriers for effective PA counseling in health care settings. The fact that our search identified only 2 studies from low- and middle-income countries, India and Colombia,52,56 is of concern and constitutes a call for further research in these settings, where 80% of the deaths due to inactivity and related NCDs occur.95
Footnotes
Authors’ Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1. US Department of Health and Human Services. 2008 physical activity guidelines for Americans. http://www.health.gov/PAGuidelines. Published 2008. Accessed January 7, 2013.
- 2. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva, Switzerland: World Health Organization; 2010. [PubMed] [Google Scholar]
- 3. World Health Organization. Global Health Risks. Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva, Switzerland: World Health Organization; 2009. http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf. Accessed December 30, 2013. [Google Scholar]
- 4. Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. Draft action plan for the prevention and control of Non-communicable diseases 2013-2020. http://apps.who.int/gb/ebwha/pdf_files/EB132/B132_7-en.pdf. Published 2012. Accessed December 30, 2013.
- 6. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247-257. [DOI] [PubMed] [Google Scholar]
- 7. Orrow G, Kinmonth AL, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344:e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gulliford MC, Charlton J, Bhattarai N, Charlton C, Rudisill C. Impact and cost-effectiveness of a universal strategy to promote physical activity in primary care: population-based cohort study and Markov model [published online April 10, 2013]. Eur J Health Econ. doi: 10.1007/s10198-013-0477-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murphy SM, Edwards RT, Williams N, et al. An evaluation of the effectiveness and cost effectiveness of the National Exercise Referral Scheme in Wales, UK: a randomised controlled trial of a public health policy initiative. J Epidemiol Community Health. 2012;66:745-753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. US Department of Health and Human Services. Healthy People 2020. Washington, DC: US Department of Health and Human Services. [DOI] [PubMed] [Google Scholar]
- 12. Leijon ME, Bendtsen P, Nilsen P, Ekberg K, Ståhle A. Physical activity referrals in Swedish primary health care—prescriber and patient characteristics, reasons for prescriptions, and prescribed activities. BMC Health Serv Res. 2008;8:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wanner M, Martin-Diener E, Bauer GF, Stamm H, Martin BW. Allez Hop, a nationwide programme for the promotion of physical activity in Switzerland: what is the evidence for a population impact after one decade of implementation? Br J Sports Med. 2011;45:1202-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Malta DC, Barbosa da Silva J. Policies to promote physical activity in Brazil. Lancet. 2012;380:195-196. [DOI] [PubMed] [Google Scholar]
- 15. Smith AW, Borowski LA, Liu B, et al. U.S. primary care physicians’ diet-, physical activity-, and weight-related care of adult patients. Am J Prev Med. 2011;41:33-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Van Wormer J, Pronk N, Kroeninger G. Clinical counseling for physical activity: translation of a systematic review into care recommendations. Diabetes Spectrum. 2009;22:48-55. [Google Scholar]
- 17. Frank E, Segura C. Health practices of Canadian physicians. Can Fam Physician. 2009;55:810-811.e7. [PMC free article] [PubMed] [Google Scholar]
- 18. Epel OB, Ziva Regev M. Quality and correlates of physical activity counseling by health care providers in Israel. Prev Med. 2000;31:618-626. [DOI] [PubMed] [Google Scholar]
- 19. van der Ploeg HP, Smith BJ, Stubbs T, Vita P, Holford R, Bauman AE. Physical activity promotion—are GPs getting the message? Aust Fam Physician. 2007;36:871-874. [PubMed] [Google Scholar]
- 20. Frank E, Bhat Schelbert K, Elon L. Exercise counseling and personal exercise habits of US women physicians. J Am Med Womens Assoc. 2003;58:178-184. [PubMed] [Google Scholar]
- 21. Kosteva AR, Salata BM, Krishnan SM, et al. Physician variation in perceived barriers to personal health. Int J Gen Med. 2012;5:53-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Frank E. STUDENTJAMA. Physician health and patient care. JAMA. 2004;291:637. [DOI] [PubMed] [Google Scholar]
- 23. Araya AMV, Leal SF, Huerta GP, Fernández AN, Fernández OG, Millones EJP. The influence of smoking habits of Chilean physicians on the use of the structured medical advice about smoking. Rev Med Chil. 2012;140:347-352. [DOI] [PubMed] [Google Scholar]
- 24. Dresner Y, Frank E, Baevsky T, Rotman E, Vinker S. Screening practices of Israeli doctors’ and their patients. Prev Med. 2010;50:300-303. [DOI] [PubMed] [Google Scholar]
- 25. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20:999-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Frank E, Dresner Y, Shani M, Vinker S. The association between physicians’ and patients’ preventive health practices. CMAJ. 2013;185:649-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their counselling practices. Br J Sports Med. 2009;43:89-92. [DOI] [PubMed] [Google Scholar]
- 28. Yancey AK, Sallis RE, Bastani R. Changing physical activity participation for the medical profession. JAMA. 2013;309:141-142. [DOI] [PubMed] [Google Scholar]
- 29. Joy EL, Blair SN, McBride P, Sallis R. Physical activity counselling in sports medicine: a call to action. Br J Sports Med. 2013;47:49-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lin JS, O’Connor E, Whitlock EP, et al. Behavioral Counseling to Promote Physical Activity and a Healthful Diet to Prevent Cardiovascular Disease in Adults: Update of the Evidence for the U.S. Preventive Services Task Force (Evidence Synthesis No. 79; AHRQ Publication No. 11-05149-EF-1). Rockville, MD: Agency for Healthcare Research and Quality; December 2010. [PubMed] [Google Scholar]
- 31. Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005;331:1064-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Adelman RD, Greene MG, Friedmann E, Ory MG, Snow CE. Older patient-physician discussions about exercise. J Aging Phys Act. 2011;19:225-238. [DOI] [PubMed] [Google Scholar]
- 33. Williford HN, Barfield BR, Lazenby RB, Olson MS. A survey of physicians’ attitudes and practices related to exercise promotion. Prev Med. 1992;21:630-636. [DOI] [PubMed] [Google Scholar]
- 34. Galuska DA, Fulton JE, Powell KE, et al. Pediatrician counseling about preventive health topics: results from the Physicians’ Practices Survey, 1998-1999. Pediatrics. 2002;109:E83-3. [DOI] [PubMed] [Google Scholar]
- 35. Rogers LQ, Bailey JE, Gutin B, et al. Teaching resident physicians to provide exercise counseling: a needs assessment. Acad Med. 2002;77:841-844. [DOI] [PubMed] [Google Scholar]
- 36. Buchholz SW, Purath J. Physical activity and physical fitness counseling patterns of adult nurse practitioners. J Am Acad Nurse Pract. 2007;19:86-92. [DOI] [PubMed] [Google Scholar]
- 37. Douglas F, Torrance N, van Teijlingen E, Meloni S, Kerr A. Primary care staff’s views and experiences related to routinely advising patients about physical activity. A questionnaire survey. BMC Public Health. 2006;6:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Frank E, Tong E, Lobelo F, Carrera J, Duperly J. Physical activity levels and counseling practices of U.S. medical students. Med Sci Sports Exerc. 2008;40:413-421. [DOI] [PubMed] [Google Scholar]
- 39. Bazargan M, Makar M, Bazargan-Hejazi S, Ani C, Wolf KE. Preventive, lifestyle, and personal health behaviors among physicians. Acad Psychiatry. 2009;33:289-295. [DOI] [PubMed] [Google Scholar]
- 40. Ferrante JM, Piasecki AK, Ohman-Strickland PA, Crabtree BF. Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity (Silver Spring). 2009;17:1710-1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Painter P, Carlson L, Carey S, Myll J, Paul S. Determinants of exercise encouragement practices in hemodialysis staff. Nephrol Nurs J. 2004;31:67-74. [PubMed] [Google Scholar]
- 42. Chambers JS, Bowen FE. Exercise and health: participation and promotion by general practitioners. J R Coll Gen Pract. 1985;35:189-191. [PMC free article] [PubMed] [Google Scholar]
- 43. Blake H, Malik S, Mo PK, Pisano C. “Do as say, but not as I do”: are next generation nurses role models for health? Perspect Public Health. 2011;131:231-239. [DOI] [PubMed] [Google Scholar]
- 44. Douglas F, van Teijlingen E, Torrance N, Fearn P, Kerr A, Meloni S. Promoting physical activity in primary care settings: health visitors’ and practice nurses’ views and experiences. J Adv Nurs. 2006;55:159-168. [DOI] [PubMed] [Google Scholar]
- 45. Anis NA, Lee RE, Ellerbeck EF, Nazir N, Greiner KA, Ahluwalia JS. Direct observation of physician counseling on dietary habits and exercise: patient, physician, and office correlates. Prev Med. 2004;38:198-202. [DOI] [PubMed] [Google Scholar]
- 46. Janes RD, Wilson DM, Singer J. Physicians’ and nurses’ own health practices: a survey. Can Fam Physician. 1992;38:277-283. [PMC free article] [PubMed] [Google Scholar]
- 47. Mullen PD, Tabak ER. Patterns of counseling techniques used by family practice physicians for smoking, weight, exercise, and stress. Med Care. 1989;27: 694-704. [DOI] [PubMed] [Google Scholar]
- 48. Van der Veer T, Frings-Dresen MH, Sluiter JK, Health behaviors, care needs and attitudes towards self-prescription: a cross-sectional survey among Dutch medical students. PLoS One. 2011;6:e28038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Walsh JM, Swangard DM, Davis T, McPhee SJ. Exercise counseling by primary care physicians in the era of managed care. Am J Prev Med. 1999;16:307-313. [DOI] [PubMed] [Google Scholar]
- 50. Wells KB, Lewis CE, Leake B, Ware JE., Jr. Do physicians preach what they practice? A study of physicians’ health habits and counseling practices. JAMA. 1984;252:2846-2848. [PubMed] [Google Scholar]
- 51. Frank E, Carrera JS, Elon L, Hertzberg VS. Basic demographics, health practices, and health status of U.S. medical students. Am J Prev Med. 2006;31:499-505. [DOI] [PubMed] [Google Scholar]
- 52. Rao CR, Darshan B, Das N, Rajan V, Bhogun M, Gupta A. Practice of physical activity among future doctors: a cross sectional analysis. Int J Prev Med. 2012;3:365-369. [PMC free article] [PubMed] [Google Scholar]
- 53. Huang TT, Borowski LA, Liu B, et al. Pediatricians’ and family physicians’ weight-related care of children in the U.S. Am J Prev Med. 2011;41:24-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pronk NP, Krebs-Smith SM, Galuska DA, et al. Knowledge of energy balance guidelines and associated clinical care practices: the U.S. National Survey of Energy Balance Related Care among Primary Care Physicians. Prev Med. 2012;55:28-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Irazusta A, Gil S, Ruiz F, et al. Exercise, physical fitness, and dietary habits of first-year female nursing students. Biol Res Nurs. 2006;7:175-186. [DOI] [PubMed] [Google Scholar]
- 56. Duperly J, Lobelo F, Segura C, et al. The association between Colombian medical students’ healthy personal habits and a positive attitude toward preventive counseling: cross-sectional analyses. BMC Public Health. 2009;9:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Frank E, Galuska DA, Elon LK, Wright EH. Personal and clinical exercise-related attitudes and behaviors of freshmen U.S. medical students. Res Q Exerc Sport. 2004;75:112-121. [DOI] [PubMed] [Google Scholar]
- 58. Callaghan P. Health beliefs and their influence on United Kingdom nurses’ health-related behaviours. J Adv Nurs. 1999;29:28-35. [DOI] [PubMed] [Google Scholar]
- 59. Abramson S, Stein J, Schaufele M, Frates E, Rogan S. Personal exercise habits and counseling practices of primary care physicians: a national survey. Clin J Sport Med. 2000;10:40-48. [DOI] [PubMed] [Google Scholar]
- 60. Douglas JG, Ferdinand KC, Bakris GL, Sowers JR. Barriers to blood pressure control in African Americans. Overcoming obstacles is challenging, but target goals can be attained. Postgrad Med. 2002;112(4):51-52, 55, 59-62. [DOI] [PubMed] [Google Scholar]
- 61. DuMonthier WN, Haneline MT, Smith M. Survey of health attitudes and behaviors of a chiropractic college population. J Manipulative Physiol Ther. 2009;32:477-484. [DOI] [PubMed] [Google Scholar]
- 62. Harsha DM, Saywell RM, Jr, Thygerson S, Panozzo J. Physician factors affecting patient willingness to comply with exercise recommendations. Clin J Sport Med. 1996;6:112-118. [DOI] [PubMed] [Google Scholar]
- 63. Connolly MA, Gulanick M, Keough V, Holm K. Health practices of critical care nurses: are these nurses good role models for patients? Am J Crit Care. 1997;6:261-266. [PubMed] [Google Scholar]
- 64. Sherman SE, Hershman WY. Exercise counseling: how do general internists do? J Gen Intern Med. 1993;8:243-248. [DOI] [PubMed] [Google Scholar]
- 65. Frank E, Segura C, Shen H, Oberg E. Predictors of Canadian physicians’ prevention counseling practices. Can J Public Health. 2010;101:390-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Binns HJ, Mueller MM, Ariza AJ. Healthy and fit for prevention: the influence of clinician health and fitness on promotion of healthy lifestyles during health supervision visits. Clin Pediatr (Phila). 2007;46:780-786. [DOI] [PubMed] [Google Scholar]
- 67. Esposito EM, Fitzpatrick JJ. Registered nurses’ beliefs of the benefits of exercise, their exercise behaviour and their patient teaching regarding exercise. Int J Nurs Pract. 2011;17:351-356. [DOI] [PubMed] [Google Scholar]
- 68. Howe M, Leidel A, Krishnan SM, Weber A, Rubenfire M, Jackson EA. Patient-related diet and exercise counseling: do providers’ own lifestyle habits matter? Prev Cardiol. 2010;13:180-185. [DOI] [PubMed] [Google Scholar]
- 69. Lewis C, Wells K, Ware JE. A model for predicting the counseling practices of physicians. J Gen Intern Med. 1986;1:154. [DOI] [PubMed] [Google Scholar]
- 70. Livaudais JC, Kaplan CP, Haas JS, Pérez-Stable EJ, Stewart S, Jarlais GD. Lifestyle behavior counseling for women patients among a sample of California physicians. J Womens Health (Larchmt). 2005;14:485-495. [DOI] [PubMed] [Google Scholar]
- 71. Rogers LQ, Gutin B, Humphries MC, Evaluation of internal medicine residents as exercise role models and associations with self-reported counseling behavior, confidence, and perceived success. Teach Learn Med. 2006;18:215-221. [DOI] [PubMed] [Google Scholar]
- 72. Frank E, Elon L, Hertzberg V. A quantitative assessment of a 4-year intervention that improved patient counseling through improving medical student health. MedGenMed. 2007;9(2):58. [PMC free article] [PubMed] [Google Scholar]
- 73. Frank E, Breyan J, Elon L. Physician disclosure of healthy personal behaviors improves credibility and ability to motivate. Arch Fam Med. 2000;9:287-290. [DOI] [PubMed] [Google Scholar]
- 74. Lewis CE, Clancy C, Leake B, Schwartz JS. The counseling practices of internists. Ann Intern Med. 1991;114:54-58. [DOI] [PubMed] [Google Scholar]
- 75. McDowell N, McKenna J, Naylor PJ. Factors that influence practice nurses to promote physical activity. Br J Sports Med. 1997;31:308-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Puig-Ribera A, McKenna J, Riddoch C. Attitudes and practices of physicians and nurses regarding physical activity promotion in the Catalan primary health-care system. Eur J Public Health. 2005;15:569-575. [DOI] [PubMed] [Google Scholar]
- 77. Frank E, Wright EH, Serdula MK, Elon LK, Baldwin G. Personal and professional nutrition-related practices of US female physicians. Am J Clin Nutr. 2002;75:326-332. [DOI] [PubMed] [Google Scholar]
- 78. Meshefedjian GA, Gervais A, Tremblay M, Villeneuve D, O’Loughlin J. Physician smoking status may influence cessation counseling practices. Can J Public Health. 2010;101:290-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-1721. [DOI] [PubMed] [Google Scholar]
- 80. Hebert ET, Caughy MO, Shuval K. Primary care providers’ perceptions of physical activity counselling in a clinical setting: a systematic review. Br J Sports Med. 2012;46:625-631. [DOI] [PubMed] [Google Scholar]
- 81. Frank E, Biola H, Burnett CA. Mortality rates and causes among U.S. physicians. Am J Prev Med. 2000;19:155-159. [DOI] [PubMed] [Google Scholar]
- 82. Frank E, Brogan DJ, Mokdad AH, Simoes EJ, Kahn HS, Greenberg RS. Health-related behaviors of women physicians vs other women in the United States. Arch Intern Med. 1998;158:342-348. [DOI] [PubMed] [Google Scholar]
- 83. Barnes P, Schoenborn C. Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief. 2012;(86):1-8. [PubMed] [Google Scholar]
- 84. Kohl HW, 3rd, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294-305. [DOI] [PubMed] [Google Scholar]
- 85. Bornstein DB, Pate RR, Pratt M. A review of the national physical activity plans of six countries. J Phys Act Health. 2009;6(suppl 2):S245-S264. [PubMed] [Google Scholar]
- 86. World Health Organization. WHO Global Strategy on Diet, Physical Activity and Health. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 87. Exercise is Medicine. http://exerciseismedicine.org/. Accessed March 5, 2013.
- 88. Blair SN, Sallis RE, Hutber A, Archer E. Exercise therapy—the public health message. Scand J Med Sci Sports. 2012;22(4):e24-e28. [DOI] [PubMed] [Google Scholar]
- 89. Sallis RE. Exercise is medicine and physicians need to prescribe it! Br J Sports Med. 2009;43:3-4. [DOI] [PubMed] [Google Scholar]
- 90. Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44:2071-2076. [DOI] [PubMed] [Google Scholar]
- 91. Global Advocacy Council for Physical Activity. Toronto charter for physical activity. http://www.globalpa.org.uk/charter/. Published May 2010. Accessed December 30, 2013.
- 92. Heath GW, Parra DC, Sarmiento OL, et al. , Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380:272-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Rogers LQ, Gutin B, Humphries MC, et al. A physician fitness program: enhancing the physician as an “exercise” role model for patients. Teach Learn Med. 2005;17:27-35. [DOI] [PubMed] [Google Scholar]
- 94. Yeh L, Chen CH, Wang CJ, Wen MJ, Fetzer SJ. A preliminary study of a healthy-lifestyle-promoting program for nursing students in Taiwan. J Nurs Educ. 2005;44:563-565. [DOI] [PubMed] [Google Scholar]
- 95. World Health Organization. Global Status Report on Noncommunicable Diseases. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]