Abstract
Objective
To evaluate clinically and functionally the pos-operative results of patients submitted to tibiotalocalcaneal arthrodesis for the treatment of traumatic arthropathy and neuropathy.
Methods
Retrospective study of 29 patients undergoing ankle arthrodesis with intramedullary retrograde nail. All patients were evaluated for fusion time, AOFAS and VAS scores, satisfaction, and complications of surgery. The mean follow-up was 36 months (range 6–60 months).
Results
The union rate was 82%, and the consolidation occurred on average at 16 weeks (10–24 weeks). The pos-operative AOFAS score improved in 65.5% (average of 57.7 on neurological cases and 75.7 on cases pos-traumatic) and VAS score improved 94.1% (average of 2.3 on neurological cases and 4,2 on post-traumatic cases), and 86% of patients were satisfied with the procedure performed. Complications occurred in 11 patients (38%), including pseudoarthrosis (17.24%), infection (17.24%), material failure (13.8%) and fracture (13.8%).
Conclusion
Tibiotalocalcaneal arthrodesis with retrograde intramedullary nail proved to be a good option for saving the ankle joint, with improvement of clinical and functional scores (AOFAS = 65.5% and VAS = 94.1%).
Keywords: Osteoarthritis, Arthrodesis, Ankle, Fracture fixation, Intramedullary
Resumo
Objetivo
avaliar clínica e funcionalmente o pós-operatório de pacientes submetidos à artrodese tibiotalocalcaneana para o tratamento das artropatias traumáticas e neurológicas do tornozelo.
Métodos
estudo retrospectivo de 29 pacientes submetidos à artrodese do tornozelo com haste intramedular retrógrada. Todos os pacientes foram avaliados em relação ao tempo de consolidação, escores Aofas e EVA e grau de satisfação, além de complicações do ato cirúrgico. O tempo de seguimento médio foi de 36 meses (variação de 6–60).
Resultados
a taxa de união foi de 82% e o tempo médio de consolidação foi de 16 semanas (10-24). O critério Aofas melhorou no pós-operatório em 65,5% (média de 57,7 nos casos neurológicos e de 75,7 nos pós-traumáticos) e a EVA melhorou 94,1% (média de 2,3 nos casos neurológicos e de 4,2 nos pós-traumáticos) e 86% dos pacientes mostraram-se satisfeitos com o procedimento feito. As complicações ocorreram em 11 pacientes (38%), entre elas pseudartrose (17,24%), infecção (17,24%), falha do material (13,8%) e fratura (13,8%).
Conclusão
a artrodese tibiotalocalcaneana com haste intramedular retrógrada mostrou ser uma boa opção para o salvamento da articulação do tornozelo, com melhoria dos critérios clínicos e funcionais (Aofas = 65,5% e EVA = 94,1%).
Palavras-chave: Osteoartrite, Artrodese, Tornozelo, Fixação intramedular de fraturas
Introduction
The tibiotalocalcaneal arthrodesis is used as a salvage procedure for the ankle joint in patients with changes in the subtalar junction of the tibiotarsal joint.1, 2, 3, 4 The indications for this procedure are mostly post-traumatic arthrodesis, rheumatoid arthritis, sequelae of infection, neuromuscular conditions, and failures of total ankle arthroplasty.2, 5, 6, 7, 8, 9, 10, 11 In 1906, Lexer described for the first time the tibiotalocalcaneal arthrodesis with intramedullary fixation using cadaveric bone graft among the calcaneus, talus and tibia.12 Since the introduction of the concept of ankle arthrodesis by compression by Charnley in 1951, more than 30 techniques and a number of technical modifications have been described.8
Patients with ankle arthropathy often present with bone loss, osteopenia or severe deformities (Fig. 1, Fig. 2), which hinders the arthrodesis fixation.2, 11, 13, 14 The literature has pointed to high infection rates (10–20%) and pseudoarthrosis6, 12, 15 (10–20%)8 associated with arthrodesis, especially for the treatment of neuromuscular arthropathies.5, 12, 13
Fig. 1.
Clinical appearance of sequelae of right tibial pylon fracture, and evolution with infection. Attempted arthrodesis was performed with an external fixator, without success. The lesion evolved to infection healing with pain, however with mobility in the focus of arthrodesis, valgus deformity of ankle, and inability to march.
Fig. 2.

Anteroposterior (A) and lateral (B) ankle radiographs, depicting non-consolidation of the previous arthrodesis, valgus deformity and joint degeneration.
Intramedullary fixation in tibiotalocalcaneal arthrodesis represents a modern approach, with the advantage of promoting rigid internal fixation with minimal periosteal aggression and vascular damage.6, 7, 15 In addition, the procedure promotes compression in the focus of the arthrodesis, with high consolidation ratios (85%) and an average arthrodesis fusion time of approximately three months.14, 15 However, the procedure is not free of complications (30–80% in most series).7, 14
The present study aimed to evaluate clinically and functionally patients undergoing tibiotalocalcaneal arthrodesis using a locked retrograde intramedullary nail for the treatment of neurological and traumatic arthropathy of the ankle and subtalar joint.
Materials and methods
This is a retrospective study with a convenience sample of 29 patients with arthrosis of ankle and subtalar joints by traumatic and neurological causes. The mean age was 41.3 years (13–72), and 15 patients (51.7%) were male and 14 (48.3%) females. Regarding etiology, 16 patients had post-traumatic arthropathy (55.2%), and in 13 (44.8%) the lesion had neurologic causes (Charcot arthropathy, sequelae of cerebral palsy and polio). The average follow-up time was 36 months (6–60) after the arthrodesis.
The surgical technique employed, from January 2005 to January 2011, was tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing of the ankle. The surgical technique follows a protocol with the patient in the lateral position. By a lateral access port of 10 cm, an osteotomy is made at right angles to the resection of distal fibula. The joint surfaces of the talus and distal tibia are decorticated by this access. A medial access is used to facilitate joint debridement and placement of the talus and the medial malleolus. The surgeon removes minimal amounts of bone to prevent shortening of the limb. A medial access is used to facilitate joint debridement and placement of the talus, with the medial malleolus. To make the fixation with the intramedullary nail, the surgeon makes an incision at the junction of middle and distal thirds of the fat pad of the heel. The foot is held in the desired position; then the surgeon passes a guide wire through the calcaneus and the talus to reach the center of the tibia. The position is checked in the image intensifier and then the surgeon proceeds with the milling. Usually, we use the 12 mm-nail and the milling is done up to 11 mm. After the removal of the intramedullary guide wire, the locking screws are inserted percutaneously with the drill guide. We use two medial screws into the tibia for the proximal locking, and one screw into the talus and calcaneus for the distal locking. This procedure does not allow the shank's dynamisation, because it results only in static locking. The procedures were performed by the surgery of the foot and ankle staff, who are members of the Department of Orthopedics and Traumatology, Hospital das Clínicas, Federal University of Goiás (UFG-DOT-HC). The study was approved by the ethics committee of the HC-UFG.
The patients were requested to fill the questionnaires of the American Orthopedic Foot & Ankle Society (AOFAS) and to a Visual Analog Scale (VAS) preoperatively. According to the AOFAS criteria, the patient can be classified with a poor (0–69), fair (70–80), good (80–90) or excellent (90–100) function. The VAS criterion classifies pain as absent (0), mild (1–3), moderate (4–6), high intensity (7–9) and intolerable (10). Patients classified as AOFAS’ poor function (less than 69) and severe VAS (between eight and 10) were selected preoperatively for the arthrodesis procedure. After surgery and after six months of evolution, the same patients answered again to the questionnaires (AOFAS and VAS). Later, we divided the cases into two groups, according to the etiology of the arthrosis (traumatic or neurological) and evaluated the following variables: time for the consolidation, smoking habits (more than 20 cigarettes/day), patient satisfaction and post-operative complications. The joint fusion was assessed by radiographs of the ankle (anteroposterior [AP] and lateral views) (Fig. 3A and B) and have been considered as a pseudoarthrosis in cases in which there were no signs of bone healing and osseous trabeculation in the AP and lateral views up to six months (24 weeks) after surgery.
Fig. 3.
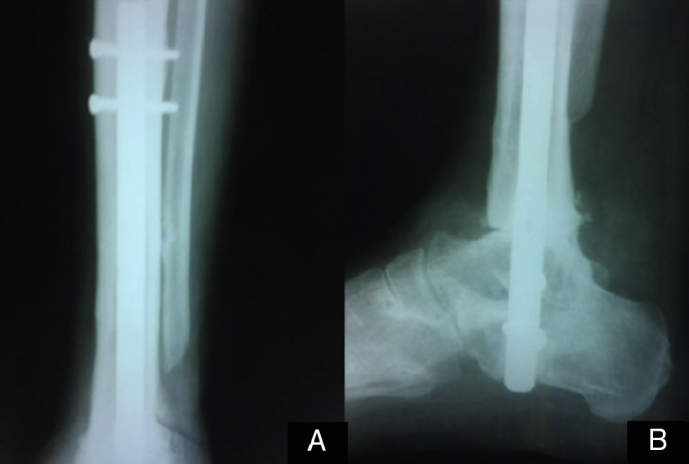
Radiological consolidation observed at six months post-operatively on anteroposterior (A) and lateral (B) radiographs.
The statistical analysis was descriptive and analytical, using Fischer's exact and chi-squared tests and comparing qualitative variables by frequency. The database is stored in the Microsoft Excel program and analyzed using SPSS version 15.0.
Results
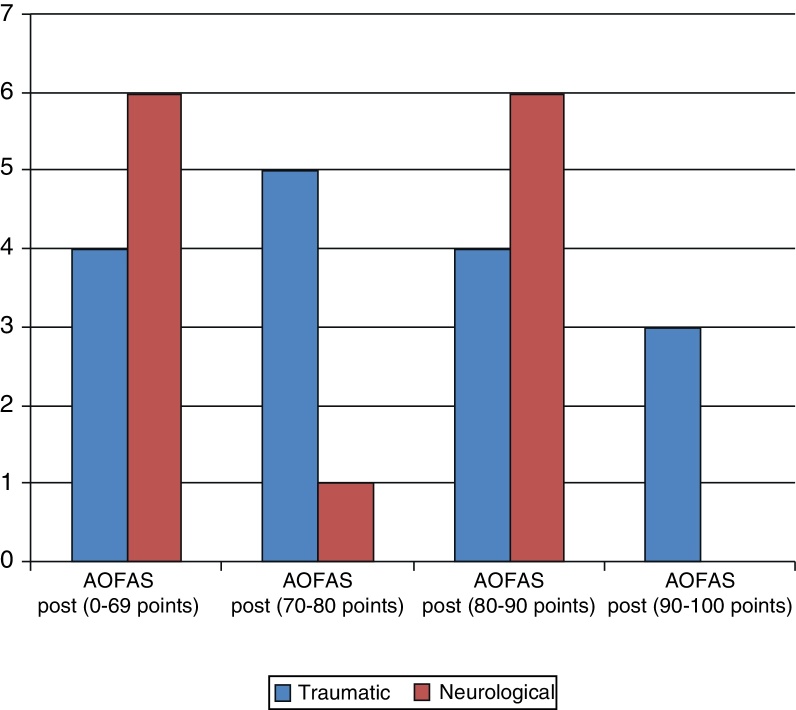
In the evaluation of the AOFAS questionnaire in the post-operative period, we noted improved scores, when compared with the values in the preoperative period, since our findings were 34.5% poor (10 cases), 20.7% fair (six cases), 34.5% good (10 cases), and 10.3% excellent (three cases) (Table 1). When analyzed by etiology, the post-operative AOFAS for traumatic cases (mean 75.7) was 21.2% better vs. neurological cases (57.7) (Fig. 4).
Table 1.
Comparison between AOFAS criteria in pre- and post-operative period.
| AOFAS | Preoperative | Post-operative | ||
|---|---|---|---|---|
| Poor | 29 | 10 | 34.5% | |
| Fair | 0 | 6 | 20.5 | 65.5% |
| Good | 0 | 10 | 34.5% | |
| Excellent | 0 | 3 | 10.5 |
Fig. 4.
Comparison between AOFAS criteria post-operatively according to etiology (traumatic vs. neurological).
Regarding the VAS questionnaire (Table 2), in the post-operative period we found 48.3% mild (14 cases), 44.8% moderate (13 cases), and 6.9% severe (two cases) – an improvement of 94.1% (average of 2.3 in neurological cases and 4.2 in post-traumatic cases). The rate of satisfaction with the procedure was 86% (25 of 29 patients). Of the 29 patients, 12 were smokers (41.4%).
Table 2.
Comparison of Visual Analog Scale for pain in pre- and post-operative period.
| VAS | Preoperative | Post-operative | ||
|---|---|---|---|---|
| Mild | 0 | 14 | 48.3% | 94.1% |
| Moderate | 0 | 13 | 44.8% | |
| Severe | 29 | 2 | 5.9% |
VAS, Visual Analog Scale.
Of the 29 patients, the arthrodesis consolidation was radiographically confirmed in 24 (82%), and five (17.2%) had nonunions. The average healing time was 16 weeks (10–24). Although we observed a trend toward an association between smoking and nonunion (pseudoarthrosis more frequent in smokers) and between nonunion and neurological etiology, no statistical significance was observed, probably because of the small sample size.
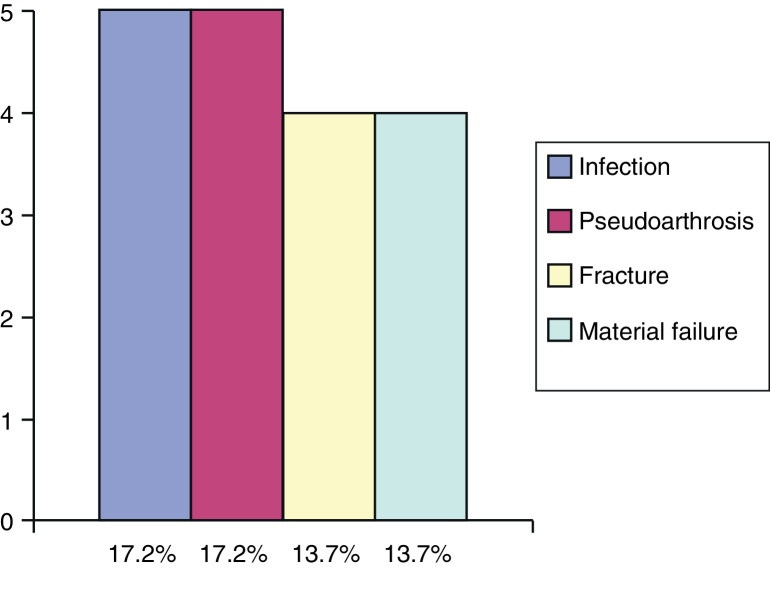
Regarding complications, 11 patients (38%) developed some kind of complication. Of those, five had more than one type of complication. So, in 29 patients, 18 complications occurred: 5 (17.2%) nonunions, 5 (17.2%) infections, 4 (13.7%) tibial fractures and 4 (13.7%) material failures (Fig. 5).
Fig. 5.
Post-operative complications of tibiotalocalcaneal arthrodesis.
Discussion
The treatment of patients with arthritis, pain and deformity of the ankle and subtalar junction is still a challenge and is extremely difficult to get excellent results. The main surgical goals of the tibiotalocalcaneal arthrodesis are to reduce pain and promote a stable and plantigrade foot with good function for deambulation.1, 4, 9 This is a procedure with high risk of complications. However, in recent years the procedure has gained acceptance as an option for saving the tibiotarsal and subtalar joints.2, 6, 12, 13, 14, 15 (Table 3).
Table 3.
Comparison of results among studies in the literature.
| Study | Pat. Nr. | Age | Follow-up (months) | Union rate | Time for consolidation (weeks) | AOFAS | VAS | Satisfaction |
|---|---|---|---|---|---|---|---|---|
| Chou et al.17 | 37 | 53 (19–79) | 26 (12–168) | 86% | 19 (12–65) | 66 | – | 87% |
| Hammett et al.13 | 47 | 57.1 (25–81) | 34 (8–37) | 87% | 17 (13–39) | 63 (13–84) | – | 82% |
| Pelton et al.6 | 33 | 54 (32–88) | 14 | 88% | 16 | – | – | – |
| Boer et al.2 | 50 | 57.6 (22–82) | 51 (12–84) | 96% | 20.4 (12–72) | 70 (32–86) | – | 92% |
| Niinimäki et al.15 | 34 | 57 (25–77) | 24 (6–43) | 76% | 16 (6–45) | – | 1.9 | 90% |
| Smith et al.16 | 10 | 60.6 (48–78) | 14.7 (12–18) | 80% | – | 69 (14–51) | 2 (0–7) | – |
| Mendicino et al.12 | 19 | 56 (33–81) | 19.8 (8–42) | 95% | 17 | – | – | – |
| This study | 29 | 41 (13–72) | 36 (6–60) | 82% | 16 (10–24) | 69 (16–96) | 3.5 (0–6) | 86% |
VAS, Visual Analog Scale.
In the last decade, a number of studies reporting complications and high rates of nonunion (4–24%) was published.13, 15, 16 Nonunion is not uncommon, mainly in cases of surgical re-approaches, as previously reported by Kim et al.14 Chou et al.17 reported union in 86% of their patients with a mean of 19 weeks (12–65). Boer et al.2 published a minimum consolidation period of 12 weeks, with a mean of 20.4 weeks (12–72). Mendicino et al.12 obtained 95% of fusions at approximately 4.1 months (17 weeks). Niinimäki et al.15 reported radiographic signals of fusion in 26 (76%) of 34 patients after 16 weeks. Pelton et al.6 reported 88% of fusion at a mean period of 3.7 months (16 weeks). Hammett et al.13 achieved complete fusion of the arthrodesis in 88.46% of their series of 52 patients in about four months (17 weeks). We obtained a fusion rate of 82.7% in our 29 patients at a mean time of 3.6 months (16 weeks) – findings similar to the average observed in the literature.
In 2007, Smith et al.16 prospectively analyzed AOFAS and VAS criteria in 10 patients. These authors found a significant increase of these criteria, with a preoperative AOFAS of 39 (range 14–51) that increased to 69 (range 51–91) post-operatively.16 VAS was also evaluated prospectively and ranged from 8.3 points in the preoperative period to 2 points after the operation.16 in our series of 29 cases, we also observed a favorable evolution for AOFAS and VAS criteria. The AOFAS of all our cases evaluated was poor preoperatively; after surgery, the mean was 69 points (range 12–96 points). VAS has also evolved considerably, from a severe pain preoperatively in 100% of cases, to a mean of 3.5 points. Only two patients (6.9%) remained with severe pain post-operatively.
Other authors also used in their series the AOFAS criteria, but only after the surgery. This was the case of Boer et al.,2 with a mean of 70 points in this regard. Hamett et al.13 obtained an average of 63 points. Chou et al.17 found a mean of 66 points. In our study, the mean score by AOFAS’ criteria was 69 points (range 12–96).
In the series of Boer et al.2 there was only one complication. The patient had sensory loss on the dorsum of the foot and radiolucency at the nail entry point. Niinimäki et al.15 reported 15% of complications in 34 patients, four post-operative infections (two patients in need of implant removal) and one case of venous thromboembolism. Smith et al.16 reported 20% of complications (nonunions) and related this occurrence to smoking.
Patient satisfaction with the procedure was also one criterion assessed in our study; when compared with data in the literature, there was discordance of findings. Chou et al.17 found 87% satisfaction with the post-operative result. In their series, Hammett et al.13 reported 82% satisfaction. Boer et al.2 reported 92% satisfaction of their patients. Niinimäki et al.15 obtained 90% satisfaction. In our study, 25 of 29 patients (86.2%) were satisfied with the treatment.
Conclusion
In our study we found a favorable evolution of AOFAS criteria, of 65.5% (mean of 57.7 in neurological and 75.7 in post-traumatic cases) and of VAS, of 94.1% (mean of 2.3 in neurological and 4.2 in post-traumatic cases) in the patients assessed. Despite the incomplete improvement of pain, most patients (86%) were satisfied with the end result.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Caixeta TB, Júnior MOC, de Castro RV, Martins JS, Costa EN, Albieri AD, et al. Artrodese tibiotalocalcaneana com haste intramedular retrógrada: avaliação clínica e funcional de 29 pacientes. Rev Bras Ortop. 2014;49:56–61.
Study conducted at the Department of Orthopedics and Traumatology, Hospital das Clínicas, Universidade Federal de Goiás, Goiânia, GO, Brazil.
References
- 1.O’Neill P.J., Logel K.J., Parks B.G., Schon L.C. Rigidity comparison of locking plate and intramedullary fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2008;29(6):581–586. doi: 10.3113/FAI.2008.0581. [DOI] [PubMed] [Google Scholar]
- 2.Boer R., Mader K., Pennig D., Verheyen C.C. Tibiotalocalcaneal arthrodesis using a reamed retrograde locking nail. Clin Orthop Relat Res. 2007;(463):151–156. [PubMed] [Google Scholar]
- 3.Lowery N.J., Joseph A.M., Burns P.R. Tibiotalocalcaneal arthrodesis with the use of a humeral locking plate. Clin Podiatr Med Surg. 2009;26(3):485–492. doi: 10.1016/j.cpm.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Noonan T., Pinzur M., Paxinos O., Havey R., Patwardhin A. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail: a biomechanical analysis of the effect of nail length. Foot Ankle Int. 2005;26(4):304–308. doi: 10.1177/107110070502600406. [DOI] [PubMed] [Google Scholar]
- 5.Ahmad J., Pour A.E., Raikin S.M. The modified use of a proximal humeral locking plate for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2007;28(9):977–983. doi: 10.3113/FAI.2007.0977. [DOI] [PubMed] [Google Scholar]
- 6.Pelton K., Hofer J.K., Thordarson D.B. Tibiotalocalcaneal arthrodesis using a dynamically locked retrograde intramedullary nail. Foot Ankle Int. 2006;27(10):759–763. doi: 10.1177/107110070602701001. [DOI] [PubMed] [Google Scholar]
- 7.Alfahd U., Roth S.E., Stephen D., Whyne C.M. Biomechanical comparison of intramedullary nail and blade plate fixation for tibiotalocalcaneal arthrodesis. J Orthop Trauma. 2005;19(10):703–708. doi: 10.1097/01.bot.0000184142.90448.e3. [DOI] [PubMed] [Google Scholar]
- 8.Pickering R.M. Artrodese de tornozelo, joelho e quadril. In: Canale S.T., editor. Cirurgia ortopédica de Campbell. 10a ed. Manole; Barueri: 2006. pp. 155–178. [Google Scholar]
- 9.Means K.R., Parks B.G., Nguyen A., Schon L.C. Intramedullary nail fixation with posterior-to-anterior compared to transverse distal screw placement for tibiotalocalcaneal arthrodesis: a biomechanical investigation. Foot Ankle Int. 2006;27(12):1137–1142. doi: 10.1177/107110070602701221. [DOI] [PubMed] [Google Scholar]
- 10.Bennett G.L., Cameron B., Njus G., Saunders M., Kay D.B. Tibiotalocalcaneal arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2005;26(7):530–536. doi: 10.1177/107110070502600706. [DOI] [PubMed] [Google Scholar]
- 11.Santangelo J.R., Glisson R.R., Garras D.N., Easley M.E. Tibiotalocalcaneal arthrodesis: a biomechanical comparison of multiplanar external fixation with intramedullary fixation. Foot Ankle Int. 2008;29(9):936–941. doi: 10.3113/FAI.2008.0936. [DOI] [PubMed] [Google Scholar]
- 12.Mendicino R.W., Catanzariti A.R., Saltrick K.R., Dombek M.F., Tullis B.L., Statler T.K. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing. J Foot Ankle Surg. 2004;43(2):82–86. doi: 10.1053/j.jfas.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 13.Hammett R., Hepple S., Forster B., Winson I. Tibiotalocalcaneal (hindfoot) arthrodesis by retrograde intramedullary nailing using a curved locking nail. The results of 52 procedures. Foot Ankle Int. 2005;26(10):810–815. doi: 10.1177/107110070502601004. [DOI] [PubMed] [Google Scholar]
- 14.Kim C., Catanzariti A.R., Mendicino R.W. Tibiotalocalcaneal arthrodesis for salvage of severe ankle degeneration. Clin Podiatr Med Surg. 2009;26(2):283–302. doi: 10.1016/j.cpm.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Niinimäki T.T., Klemola T.M., Leppilahti J.I. Tibiotalocalcaneal arthrodesis with a compressive retrograde intramedullary nail: a report of 34 consecutive patients. Foot Ankle Int. 2007;28(4):431–434. doi: 10.3113/FAI.2007.0431. [DOI] [PubMed] [Google Scholar]
- 16.Smith J.W., Moore T.J., Fleming S., Pochatko D., Principe R. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail. Foot Ankle Int. 2007;19(16):433–436. doi: 10.1177/107110079501600710. [DOI] [PubMed] [Google Scholar]
- 17.Chou L.B., Mann R.A., Yaszay B., Graves S.C., McPeake W.T., 3rd, Dreeben S.M. Tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2000;21(10):804–808. doi: 10.1177/107110070002101002. [DOI] [PubMed] [Google Scholar]