Abstract
Objective
To determine feasibility of a home-based, intensive bimanual intervention with children with unilateral spastic cerebral palsy.
Methods
Eleven children (aged 29–54 months) received 90 hours of home hand-arm bimanual intensive therapy (H-HABIT) provided by their trained caregivers. Parenting stress levels and compliance were monitored using the Parenting Stress Index and daily logs. Quality of bimanual performance and changes in performance/satisfaction of functional goals were assessed using the Assisting Hand Assessment (AHA) and Canadian Occupational Performance Measure (COPM), respectively, at two pretreatment baseline sessions and two posttreatment sessions (immediate and six months).
Results
Ten children completed the study with caregivers completing on average 85.6 hours of H-HABIT. Daily logs indicated high caregiver compliance. Stress levels remained stable across the intervention. Children demonstrated significant improvements in the AHA and COPM.
Conclusion
H-HABIT is a feasible intervention for improving hand function and merits further investigation in a randomized-control trial.
Keywords: Bimanual training, family focused, hand rehabilitation, hemiplegia, home-based therapy, unilateral cerebral palsy, upper-limb function
Introduction
Children with unilateral spastic cerebral palsy (USCP) experience unilateral deficits in the execution of movement [1] that arise from early prenatal or neonatal brain injury. Children with USCP also have sensory impairments [2], impairments in movement planning [3] and deficits in the quality of bimanual performance; however, longitudinal studies of children with USCP suggest that performance improves over time when children are provided with access to therapy [4]. The goal of interventions designed for children with USCP is to improve affected limb-use in order to promote functional independence and participation.
One evident trend in treatment approaches for children with USCP is an increased involvement of the caregiver in intervention delivery [5–7]. Increased involvement on behalf of the child’s family is a notion consistent with theoretical frameworks such as family centered care [8], which suggests that caregivers and professionals are equally responsible in the promotion and delivery of health care to the child. Studies that have adapted interventions by modifying dosing schedule and training teachers or caregivers to lead manual activities have demonstrated to be an effective approach for improving hand function in children with USCP [5–7].
One approach that has yet to be formally tested when provided exclusively in the home is intensive bimanual training. Hand-arm bimanual intensive therapy (HABIT) is a motor-learning-based training focused on improving the amount and quality of involved hand-use in the context of bimanual tasks [9]. Camp-based studies of HABIT in children with USCP age four years and above have shown the therapy to improve the quality of bimanual performance [10]. This study examined the feasibility of home-based HABIT (H-HABIT) with caregivers as the primary interventionists. The aims of this study were to determine the feasibility of H-HABIT in terms of compliance, caregiver perception of difficulty in completing the activities and the impact of the intervention on the psychosocial dynamic between caregivers and their child (i.e. caregiver stress); and to collect preliminary outcome data on the effectiveness of H-HABIT to inform a power analysis for a future randomized control trial.
Methods
Study design
A single-group design was chosen to examine feasibility of the intervention. Measures were taken during a one-week baseline period, during the treatment phase and immediately after and six-months after a 90-hour home-based bimanual intervention with caregivers as the primary interventionists. Caregivers were trained to administer H-HABIT immediately following the baseline period.
Participants
Participants were recruited from referrals from clinicians, our website (http://www.tc.edu/centers/cit/), and online support groups. Eligible participants between the ages of 30 and 54 smonths with USCP were invited to participate if they met the following inclusion criteria: (1) ability to grasp and release blocks from affected hand, (2) ability to follow two-step instructions and complete testing and (3) ability of the caregiver to provide one-to-one attention to the child during the daily activities. Children were excluded from the study if they received an intensive upper extremities intervention or botulinum toxin therapy in the upper extremity within the past six months. All children continued to receive their customary individual therapy during the course of the study. Informed consent was obtained from caregivers. This study was approved by the Teachers College, Columbia University Institutional Review Board.
Caregiver training
Caregiver training was standardized and adapted from an established manual of procedures for HABIT [11]. All caregivers received training from the same experienced supervisor over a series of three sessions each lasting about 1.5–2 hours. The first training session involved only the supervisor and caregiver. Caregivers were instructed on the general intervention procedures, discussed reinforcement strategies and were guided through videos of other caregivers performing H-HABIT. We were particularly concerned about not disrupting the complex psychosocial dynamic between caregivers and children. In order to avoid disruptions, caregivers were encouraged to use a subtle cue to the child (e.g. H-HABIT hats or scarves) to indicate that H-HABIT hours were separate from the child’s typical routine. For the second session, caregivers returned with their child and watched as the supervisor modeled how to administer H-HABIT. Then, caregivers were asked to model with the child for the supervisor and were provided with feedback. The final training session occurred in the family’s home and also marked the beginning of the 90-hour intervention. The supervisor visited the family’s home and provided feedback to the caregiver as they performed activities with the child. Home visits occurred weekly throughout the intervention (1 hour/visit).
H-HABIT intervention procedures
Children completed an intervention in which they received 2 hours/day of H-HABIT, for five days/week that lasted nine consecutive weeks (90 hours total). The intervention supervisor helped caregivers design an individualized program for the child. Activities were chosen based on the ability of the child’s affected hand and focused on using the hand as an assisting hand during increasingly complex bimanual coordination. Task demands were graded by varying the constraints of the task or providing activities that required progressive skilled use as performance improved. Caregivers were instructed to place emphasis on making the intervention enjoyable and intrinsically motivating for their children. Age-appropriate reward systems (e.g. sticker charts) and age-specific knowledge of results was provided as encouragement and to ensure the activities were highly motivating and fun. Caregivers incorporated functional (e.g. cleaning and eating) and play activities (i.e. building blocks and magnets) using child-friendly games. Caregivers recorded daily activities and time spent on each activity using an online log. The supervisor monitored daily logs remotely and provided ideas for skill progression.
Measures
Participant characteristics
The Manual Ability Classification System was used to classify the children’s typical manual performance [12].
Feasibility
Aspects of feasibility included compliance, caregiver perception of difficulty in completing the activities and the caregiver stress levels. Caregiver stress levels were monitored with the Parenting Stress Index-Short Form (PSI-SF) [13] at each of the assessment time points. The PSI-SF is a 36-item self-report measure used to evaluate stress related to family interactions and has established reliability and validity [14].
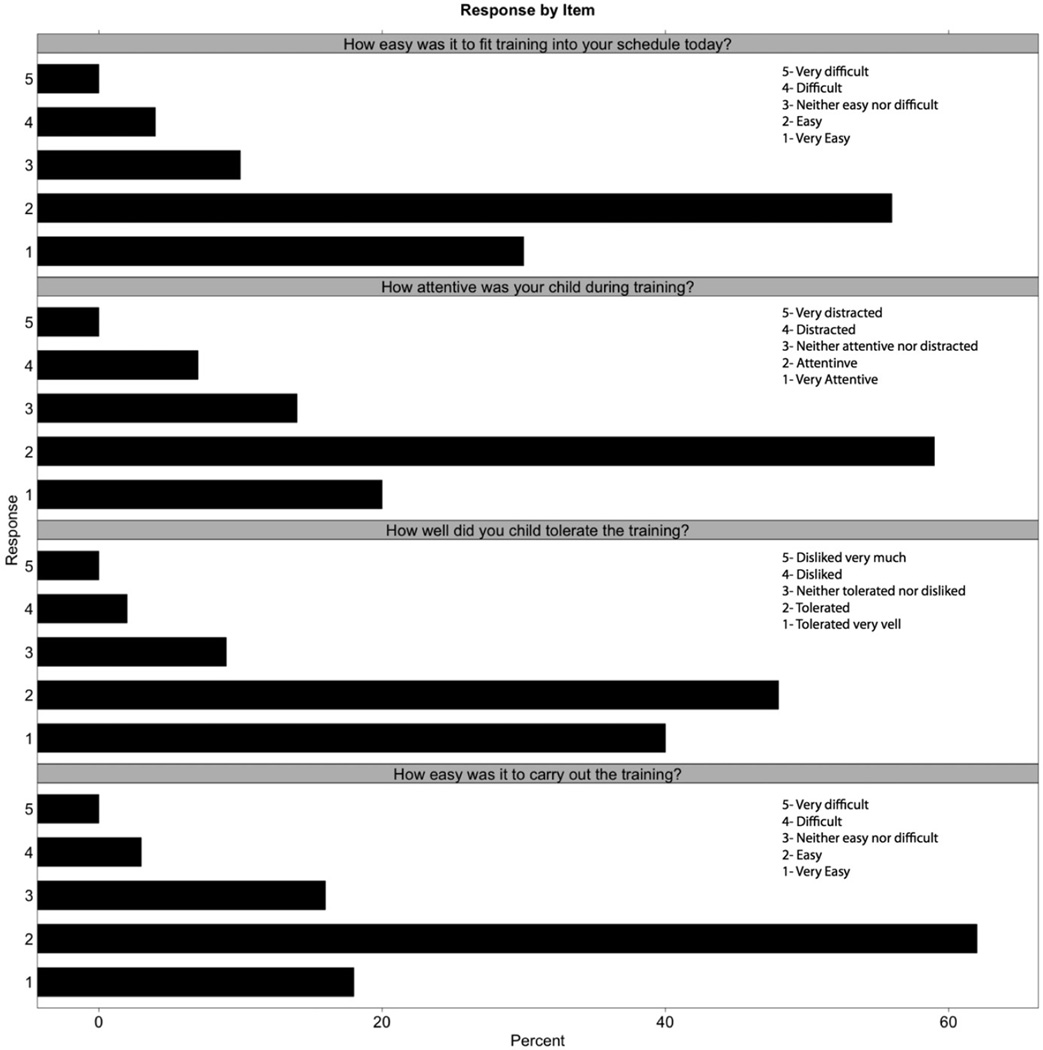
Compliance was tracked using online daily logs. Participation rate was calculated as the percentage of the required 90 hours completed by the participants. The daily logs also included questions adapted from Wallen et al. [7] and were used to elicit perceptions of the difficulty in completing the day’s activities (Figure 1).
Figure 1.
Responses to daily log questionnaire regarding feasibility.
Hand function
The Assisting Hand Assessment (AHA, version 4.3) is an instrument that quantifies how effectively a child with unilateral disability uses his/her affected hand in bimanual activities. It has excellent validity and reliability [15, 16]. A change of five AHA units is regarded as the smallest reliable difference for the AHA [17]. The tests were scored by an occupational therapist certified to score the AHA and that was blinded to the study. The AHA was administered twice before the intervention (separated by one week), immediately after and six months after the intervention.
The Canadian Occupational Performance Measure (COPM) was used with parents to establish and evaluate children’s functional goals [18], in terms of performance and caregiver satisfaction levels. It is a valid and reliable measure [19] with a change of two points indicating a clinically meaningful difference. The COPM was used to assess goal performance at the second baseline, immediate posttest and six-month follow-up.
Statistical design
A repeated-measures ANOVA on test sessions was performed on the PSI raw data, AHA-units for the AHA and on raw and log-transformed COPM data using R (R Core Team, 2012). Post hoc comparisons using Tukey HSD test were used between the first baseline and each subsequent measure and between the first posttest and second posttest. For the AHA, which included two baseline assessments, Tukey HSD test was used between the average of the two baseline measures and each subsequent measure.
The magnitude of change attributed to the intervention was also determined using net changes scores as calculated by subtracting baseline change from treatment change and comparing to published smallest detectable differences for the AHA. Change scores from baseline to immediate posttest were also calculated for the COPM to identify the number of kids achieving a minimal clinically important difference.
Results and discussion
Fifteen children were invited for pre-screening. Of those 15 children, 11 enrolled in the study. Reasons for not enrolling included too mildly impaired (n = 1), parents deciding to have child receive botulinum toxin therapy instead (n = 1), schedule of intervention was too demanding for caregiver work schedule/child’s school schedule (n = 1) and unspecified (n = 1). One family enrolled in the study dropped out after four weeks with the caregiver indicating that the intervention schedule was too demanding. A total of 10 children completed the study. Demographic data for children that enrolled are listed in Table I.
Table I.
Participant characteristics.
| Child | Sex | Age (months) |
Affected side |
MACS | Gestation period |
Enrolled in preschool |
|---|---|---|---|---|---|---|
| 1 | F | 45 | Right | II | Term | Yes |
| 2 | F | 43 | Right | III | Term | Yes |
| 3 | M | 34 | Right | II | Term | No |
| 4* | M | 45 | Right | I | Term | Yes |
| 5 | M | 52 | Left | III | Preterm | Yes |
| 6 | M | 45 | Right | II | Preterm | Yes |
| 7 | M | 47 | Right | II | Term | No |
| 8 | F | 29 | Right | IV | Term | No |
| 9 | F | 29 | Right | II | Term | Yes |
| 10 | M | 54 | Left | I | Term | Yes |
| 11 | F | 38 | Right | III | Term | Yes |
Did not complete study.
MACS: Manual Ability Classification System.
Feasibility
Ten families completed the entire nine weeks of intervention without any report of adverse events. On average, caregivers demonstrated high compliance completing 86.5 hours of H-HABIT with their children. The majority of activities included common, low cost supplies/toys appropriate for this age group (Table II). The most common type of activity performed included manipulative games/tasks (39% of all logged activities) and functional daily living tasks (22% of all logged activities). On average, families performed about 7.5 activities per day that lasted about 18.2 minutes per activity. Home observations by the supervisor and monitoring of daily logs confirmed that treatment protocols were adhered to. Responses to the daily questionnaires were consistent across the sample with the majority of logs indicating that 80% of the time caregivers found it either very easy or easy to fit the training into their daily schedule, 86% the child was very attentive or attentive during the activities, 88% of the time the child tolerated the training either very well or well and that 79% of the time it was very easy or easy to carry out the training (Figure 1).
Table II.
Description and categorization of bimanual activities performed during H-HABIT.
| Activity category | Percent of total activities |
Activity examples | Example of affected upper extremity use |
|---|---|---|---|
| Manipulative games/tasks | 39% | Molding clay, puzzles, board games, Legos, stacking cups | Stabilize construction piece while less-affected hand connects other pieces |
| Functional tasks | 22% | Dressing, undressing, cutting with scissors, eating | Hold and rotate paper during cutting with scissors |
| Miscellaneous | 11% | Book/page turning, games in bath tub, pretend play with figurines, bubbles | Supination of forearm while pouring water into cups during bath time |
| Fine motor | 10% | Beading, stickers, magnets, coin bank, marbles | Placing beads on pipe cleaner |
| Gross motor | 7% | Two-handed ball play, scooter handles, putt-putt golf, baseball | Throw and catch large ball with both hands |
| Arts and crafts | 6% | Painting, drawing, holiday-themed crafts | Stabilize/rotate paper while tracing shapes |
| Card games | 4% | Card flipping during matching | Simultaneously flip two cards |
| Video games | 1% | Tablet, computer | Holding/rotating tablet less-affected swipes on screen |
Parenting stress as measured by the PSI-SF showed no significant differences (p >0.05) across the five assessments for either the total score or the three subscales of parental distress, parent–child dysfunctional interaction and difficult child (Table III). That is, there was no increase in parental stress during the intervention. All caregivers scored within one standard deviation of the normative range for this measure [13].
Table III.
Means and 95% confidence intervals for assessments at each time point.
| Baseline 1 | Baseline 2 | Midway | Posttest 1 | Posttest 2 | Test session effect p value (η2) |
|
|---|---|---|---|---|---|---|
| PSI-SF total | 58.6 (49.7–69.3) | 61.4 (48.5–69.3) | 57.3 (46.5–68.3) | 56.8 (44.9–66.5) | 58.5 (45.5–65.1) | >0.05 (0.01) |
| PD | 19.9 (13.8–24.3) | 19.8 (11.7–22.3) | 18.6 (11.6–22.8) | 16.2 (12.0–22.5) | 19.8 (11.8–22.4) | >0.05 (0.00) |
| PCDI | 18.0 (10.1–24.3) | 18.8 (9.6–25.2) | 17.6 (9.2–25.6) | 19.6 (10.0–26.06) | 22.3 (12.1–28.07) | >0.05 (0.02) |
| DC | 20.1 (10.8–34.8) | 22.2 (10.6–35.0) | 20.3 (8.8–33.6) | 20.3 (10.4–35.6) | 20.6 (9.0–36.2) | >0.05 (0.00) |
| AHA | ||||||
| AHA units (0–100) | 56.2 (45.8–66.6) | 56.4 (47.6–65.2) | – | 59.2 (47.5–67.7) | 61.7 (51.7–71.7) | <0.01 (0.34) |
| COPM | ||||||
| Performance | – | 2.9 (2.1–3.7) | – | 5.6 (4.6–7.3) | 6.5 (5.33–7.6) | <0.05 (0.26) |
| Satisfaction | – | 3.00 (2.1–3.9) | – | 6.0 (4.6– 7.4) | 6.6 (5.8–7.4) | <0.05 (0.24) |
PSI-SF: parental stress index-short form; PD: Parental Distress Subscale; PCDI: Parent–Child Dysfunctional Interaction Subscale; DC: Difficult Child Subscale; AHA: Assisting Hand Assessment; and COPM: Canadian Occupational Performance Measure.
Bimanual and functional goal performance
Table III shows the means for the AHA and COPM at each time point. Children demonstrated significant improvements in the AHA, F(3,27) = 4.64, p <0.01, η2 = 0.34. Tukey’s HSD post-hoc tests revealed no difference between the two baseline measures and significant differences between the six-month follow-up and the baseline period (p < 0.05). There was also no difference between the immediate post-test and the six-month follow-up. Net change scores revealed that 4 of 10 children improved the smallest detectable difference between the baseline period and the immediate follow-up, and 5 of 10 between the baseline period and six-month follow-up.
The majority of functional goals established for the COPM were bimanual and related to dressing (e.g. putting on socks). Children showed a significant improvement in the performance domain of COPM F(2,27) = 4.43, p <0.05, η2 = 0.26. The post-hoc test indicated a significant difference between the baseline period and immediate posttest which was maintained at six-month follow-up, p <0.001. Children also showed a significant improvement in the satisfaction domain of COPM, F(2,27) = 3.88, p<0.05, η2 = 0.24. The post-hoc test indicated a significant difference between the baseline period and immediate posttest, which was maintained at six-month follow-up, p <0.01. For both domains of the COPM, 7 of 10 children achieved a minimal clinically important difference (i.e.>2).
The aim of this study was to examine the feasibility of caregiver-directed, home-based HABIT (H-HABIT) and to collect preliminary data in preparation for a randomized trial. Caregivers demonstrated a high rate of compliance and commitment to completing the entire duration of the intervention and indicated that the children tolerated the activities. Importantly, they were able to complete the intervention without increasing their levels of parental stress. Improvements in bimanual performance were evident and the majority of children exceeded the minimal clinically important difference for functional goal performance. These results suggest that H-HABIT is a feasible model that warrants further exploration to examine its efficacy for improving hand-function in children with USCP.
One risk of including caregivers in the delivery component of an intervention is the potential burden created by the demands of the schedule. In order to reduce potential stress, we trained caregivers to delineate the daily hours of the intervention from the child’s typical daily routine and to avoid verbal prodding to use the affected hand outside of the daily two hours. The stability of parental stress throughout the intervention period and feasibility indicated in the daily logs suggest that this may have been an effective strategy for avoiding disruption of the psychosocial family dynamic. It has previously been shown that the increased caregiving demands resulting from having a child with CP directly affects caregiver health [20] and that caregivers of children with hemiparesis are up to twice as likely to report increased levels of stress relative to parents of typically developing children [21]. Caregivers in this study demonstrated parental stress levels that are similar to caregivers of typically developing children [13]. Thus, it should be noted that the sample of caregivers participating in this study might come from a highly selective population of caregivers of children with CP. Information about parental stress could serve as a useful screening tool to identify families that might be good candidates for the model of home-based intervention used in this study. However, future studies are needed to address this question directly.
Definitive conclusions about the efficacy of H-HABIT cannot be drawn from the data in this study given that it lacked a comparison control group. Regardless, the results are encouraging as about half of the children improved the smallest detectable difference for the AHA and the majority achieved a minimal clinically important difference for the COPM. Although the children as a group demonstrated a linear trend for improvement on the AHA, the post-hoc tests only revealed significant differences between the baseline and six-month follow-up assessment. It is conceivable that the improvements might be related to development of hand function associated with age as opposed to the intervention itself. However, almost all of the children in this study were beyond the age (i.e. 3 years) at which higher functioning children (i.e. can grasp with affected hand by 18 months of age) tend to reach their maximum limit on the AHA [4]. Thus, the rates of change between the immediate post-test and the 6-month follow-up appear to exceed what one would expect on average for a high functioning group. Moreover, a larger sample may have revealed significant differences between the baseline and immediate post-test.
In summary, this study demonstrated that a home-based model of bimanual training using caregivers as interventionists is a feasible approach for improving hand function in children with USCP. A randomized trial examining this intervention model could provide an invaluable clinical intervention tool that could be used to target the deficits in children with USCP.
Footnotes
Declaration of interest
The authors report no conflicts of interest.
References
- 1.Eliasson AC, Gordon AM, Forssberg H. Basic co-ordination of manipulative forces of children with cerebral palsy. Developmental Medicine and Child Neurology. 1991;33:661–670. doi: 10.1111/j.1469-8749.1991.tb14943.x. [DOI] [PubMed] [Google Scholar]
- 2.Gordon AM, Duff SV. Relation between clinical measures and fine manipulative control in children with hemiplegic cerebral palsy. Developmental Medicine and Child Neurology. 1999;41:586–591. doi: 10.1017/s0012162299001231. [DOI] [PubMed] [Google Scholar]
- 3.Steenbergen B, Gordon AM. Activity limitation in hemiplegic cerebral palsy: Evidence for disorders in motor planning. Developmental Medicine and Child Neurology. 2006;48:780–783. doi: 10.1017/S0012162206001666. [DOI] [PubMed] [Google Scholar]
- 4.Holmefur M, Krumlinde-Sundholm L, Bergstrom J, Eliasson AC. Longitudinal development of hand function in children with unilateral cerebral palsy. Developmental Medicine and Child Neurology. 2010;52:352–357. doi: 10.1111/j.1469-8749.2009.03364.x. [DOI] [PubMed] [Google Scholar]
- 5.Eliasson AC, Krumlinde-sundholm L, Shaw K, Wang C. Effects of constraint-induced movement therapy in young children with hemiplegic cerebral palsy: An adapted model. Developmental Medicine and Child Neurology. 2005;47:266–275. doi: 10.1017/s0012162205000502. [DOI] [PubMed] [Google Scholar]
- 6.Eliasson AC, Shaw K, Berg E, Krumlinde-Sundholm L. An ecological approach of Constraint Induced Movement Therapy for 2–3-year-old children: A randomized control trial. Research in Developmental Disabilities. 2011;32:2820–2828. doi: 10.1016/j.ridd.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 7.Wallen M, Ziviani J, Naylor O, Evans R, Novak I, Herbert RD. Modified constraint-induced therapy for children with hemiplegic cerebral palsy: A randomized trial. Developmental Medicine and Child Neurology. 2011;53:1091–1099. doi: 10.1111/j.1469-8749.2011.04086.x. [DOI] [PubMed] [Google Scholar]
- 8.King S, Teplicky R, King G, Rosenbaum P. Family-centered service for children with cerebral palsy and their families: A review of the literature. Seminars in Pediatric Neurology. 2004;11:78–86. doi: 10.1016/j.spen.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Charles J, Gordon AM. Development of hand-arm bimanual intensive training (HABIT) for improving bimanual coordination in children with hemiplegic cerebral palsy. Developmental Medicine and Child Neurology. 2006;48:931–936. doi: 10.1017/S0012162206002039. [DOI] [PubMed] [Google Scholar]
- 10.Gordon AM, Schneider JA, Chinnan A, Charles JR. Efficacy of a hand-arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: A randomized control trial. Developmental Medicine and Child Neurology. 2007;49:830–838. doi: 10.1111/j.1469-8749.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- 11.Gordon AM, Hung YC, Brandao M, Ferre CL, Kuo HC, Friel K, Petra E, Chinnan A, Charles JR. Bimanual training and constraint-induced movement therapy in children with hemiplegic cerebral palsy: A randomized trial. Neurorehabilitation and Neural Repair. 2011;25:692–702. doi: 10.1177/1545968311402508. [DOI] [PubMed] [Google Scholar]
- 12.Eliasson A-C, Krumlinde-Sundholm L, Rösblad B, Beckung E, Arner M, Öhrvall A-M, Rosenbaum P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Developmental Medicine & Child Neurology. 2006;48:549–554. doi: 10.1017/S0012162206001162. [DOI] [PubMed] [Google Scholar]
- 13.Abidin R. Manual for the parenting stress index. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- 14.Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child and Adolescent Psychology. 2006;35:302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- 15.Krumlinde-Sundholm L, Holmefur M, Kottorp A, Eliasson AC. The Assisting Hand Assessment: Current evidence of validity, reliability, and responsiveness to change. Developmental Medicine and Child Neurology. 2007;49:259–264. doi: 10.1111/j.1469-8749.2007.00259.x. [DOI] [PubMed] [Google Scholar]
- 16.Holmefur M, Krumlinde-Sundholm L, Eliasson AC. Interrater and intrarater reliability of the Assisting Hand Assessment. American Journal of Occupational Therapy. 2007;61:79–84. doi: 10.5014/ajot.61.1.79. [DOI] [PubMed] [Google Scholar]
- 17.Holmefur M, Aarts P, Hoare B, Krumlinde-Sundholm L. Test-retest and alternate forms reliability of the assisting hand assessment. Journal of Rehabilitation Medicine. 2009;41:886–891. doi: 10.2340/16501977-0448. [DOI] [PubMed] [Google Scholar]
- 18.Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy. 1990;57:82–87. doi: 10.1177/000841749005700207. [DOI] [PubMed] [Google Scholar]
- 19.Verkerk GJ, Wolf MJ, Louwers AM, Meester-Delver A, Nollet F. The reproducibility and validity of the Canadian Occupational Performance Measure in parents of children with disabilities. Clinical Rehabilitation. 2006;20:980–988. doi: 10.1177/0269215506070703. [DOI] [PubMed] [Google Scholar]
- 20.Raina P, O’Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, Swinton M, Zhu B, Wood E. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115:e626–e636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- 21.Butcher PR, Wind T, Bouma A. Parenting stress in mothers and fathers of a child with a hemiparesis: Sources of stress, intervening factors and long-term expressions of stress. Child: Care, Health and Development. 2008;34:530–541. doi: 10.1111/j.1365-2214.2008.00842.x. [DOI] [PubMed] [Google Scholar]