Abstract
Introduction
Fibro-osseous lesions are a diverse group of bone disorders and include developmental, reactive or dysplastic diseases and neoplasms. They share overlapping clinical, radiographic and histopathologic features and demonstrate a wide range of biological behaviour.
Aim
To evaluate the characteristics, treatment and outcome of benign fibro-osseous lesions of the jaws.
Patients and Method
All patients with fibro-osseous lesions of the jaws treated at the department of Oral and Maxillofacial Surgery of the Kamineni Institute of Dental Sciences from 2007 to 2013 were included in this study.
Results
Six males and four females were treated. Juvenile ossifying fibroma was most often encountered (40 %), and the mandible was the most frequent location (70 %). Main clinical feature in most of the cases was a painless expansile swelling with facial asymmetry, and radiologically mixed (radiolucent and radiopaque lesions) were seen in majority of cases. All cases were surgically treated and histopathologically confirmed. Segmental ostectomy was performed in six cases; maxillectomy was done in one case and excision along with margin in three cases. Mean follow-up was of 3.3 years with no recurrence.
Conclusions
Fibro-osseous lesions, although sharing similar microscopic features, exhibit a variety of clinical behavior rendering their treatment highly individualized. Radical treatment is the choice to achieve an outcome without recurrence.
Keywords: Maxillofacial, Juvenile ossifying fibroma, Children, Ossifying fibroma
Introduction
Α diverse group of osseous disorders including hereditary or developmental lesions, reactive or dysplastic diseases and neoplasms have been described as benign fibro-osseous lesions [1].
The term fibro-osseous lesion is largely descriptive, limited and diagnostically non-specific. They represent—replacement of normal bone by fibrous tissue composed of collagen fibers, fibroblasts and certain varying amounts of mineralized substance, which may be bone or cementum like in appearance. Waldron described them as “A group of pathological changes within the jaw bones, in which normal bone is replaced by fibrous tissue with or without calcification” [2]. Again in 1985 Waldron described the benign FOL of jaws “as replacement of normal bone by tissue composed of collagen fibers and fibroblasts, containing varying amount of mineralized substance that may be bony or cementum like in appearance” [3].
They frequently develop in the craniofacial skeleton and especially in the jaws, the nasal cavity, the paranasal sinuses and the orbit.
Fibro-osseous lesions (FO lesions) of the maxillofacial bones share overlapping clinical, radiographic and histopathologic features that may lead to diagnostic confusion and difficulty in differentiation.
There is a relative disagreement among authors in pertinent literature, about their classification and this issue has clinical implications, as the wide range of biologic behaviour these lesions demonstrate different management strategies. Although the term fibro-osseous lesion had not been included in the WHO’s classification of 1992 [4], these lesions were formally re-classified in 1993 [5] and have been included ever since, based on their biological behaviour and histopathology and in agreement with Waldron’s recommendations of 1985. Thus FO lesions nowadays constitute a group of “neoplasms and other tumours related to bone” [5].
The main clinical symptom is soft tissue swelling and enlargement of the affected bones, which may lead to cosmetic and functional disturbances. The presence of pain, paraesthesia, trismus or dental occlusal findings has been reported, depending on location.
Alternatively FO lesions may be completely asymptomatic, identified only on routine radiographs, while fibrous dysplasia can be associated with generalized endocrinopathy.
The radiological appearance of fibro-osseous lesions varies depending on the stage of development. In the early stages the lesion is radiolucent and well-defined, while at later stages it changes into radio-opacity with ill-defined borders.
The radiographic appearance may thus be either a radiolucent, a mixed radiolucent-radiopaque, a predominantly radiopaque, or groundglass appearance. In craniofacial lesions the bone appearance has been sub classified into three different patterns: pagetoid, cystic or sclerotic.
The treatment of fibro-osseous lesions, generally based on their biological behaviour and regional aggressiveness, is highly individualized. A conservative approach is indicated in some cases, and a more radical approach including a surgical resection may be warranted in others. Fibro-osseous lesions in adults have been well documented in many studies and although they often occur in children and adolescents, relevant reports are rather infrequent.
The purpose of this retrospective study was to evaluate the characteristics, treatment outcome of benign fibro-osseous lesions of the jaws, in children, adolescents and adults.
Aims and objectives of the study are (a) to study clinical and radiographic characteristics of fibro-osseous lesions, (b) treatment outcome following radical resection in the maxillofacial region.
Materials and Methods
All patients with fibro-osseous lesions of the jaws treated at the Department of Oral and Maxillofacial Surgery of the Kamineni Institute of Dental Sciences from 2007 to 2013 were included in this study. The criteria for inclusion of the various lesions were their prior classification as fibro-osseous lesion in previous studies. Data from the patients’ files including age, sex, location, type of lesion, applied treatment and outcome, were registered. Most of the patients are still under follow-up and are regularly called for examination.
Results
Ten patients were included in the study. There was a male predilection with six males (60 %) and four females (40 %), with a mean age of 27.2 years (range from 12 to 50 years). The mean age for male patients was 22 years (12–50 years), while the mean age for female patients was 34 years (22–50 years). All parameters and findings registered have been summarized in Table 1.
Table 1.
Data of the patients included in the study, concerning gender, age (in years), type of the lesion, localization, clinical features, radiographic features, treatment and time elapsed between surgery and follow up (in years)
| S.no | Sex | Age | Type | Localization | Clinical features | Radiographic appearance | Treatment | Follow up in years |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 27 | OF | Mandible-body | Symptomatic | Mixed | Segmental ostectomy | 5 |
| 2 | M | 13 | JOF | Mandible-angle | Symptomatic | Mixed | Segmental ostectomy | 5 |
| 3 | M | 12 | JOF | Mandible-body | Symptomatic | Mixed | Segmental ostectomy | 5 |
| 4 | F | 25 | COF | Mandible-body | Symptomatic | Mixed | Segmental ostectomy | 4 |
| 5 | M | 17 | JOF | Maxilla-right maxilla | Symptomatic | Mixed | Maxillectomy | 4 |
| 6 | M | 50 | POF | Mandible-Lingual alveolar bone | Asymptomatic | Sclerotic and radiopaque | Excision along with margin | 3.5 |
| 7 | F | 22 | COF | Mandible-body | Symptomatic | Mixed | Segmental ostectomy | 3 |
| 8 | F | 50 | POF | Maxilla-tooth bearing apparatus | Symptomatic | Sclerotic and radiopaque | Excision along with margin | 1.5 |
| 9 | M | 14 | JOF | Mandible-angle | Symptomatic | Mixed | Segmental ostectomy | 1 |
| 10 | F | 42 | POF | Maxilla-tooth bearing apparatus | Symptomatic | Sclerotic and radiopaque | Excision along with margin | 1 |
M male, F female, OF ossifying fibroma, COF central ossifying fibroma, JOF juvenile ossifying fibroma, POF peripheral ossifying fibroma
The most frequent location was the mandible (seven cases, 70 %); in four cases, the mandibular body, in two cases, the mandibular angle was involved, in one case lingual alveolar bone was involved. As far as the maxilla was concerned, the entire right maxillary bone was affected in one case of central ossifying fibroma and in two cases of peripheral ossifying fibroma where the lesion arises from the tooth bearing apparatus.
The main clinical symptom for all patients was painless enlargement of the jaw with disfigurement being the main complaint of the patient; CT scans and simple X-rays were available in all cases. Radiologic examination showed a mixed appearance in seven cases (70 %) and sclerotic and radiopaque in three cases (Table 1).
Treatment was surgical in all cases. More specifically, regarding the mandibular lesions, six cases were treated by segmental ostectomy (nos: 1, 2, 3, 4, 7, 9) through an extraoral approach. The resultant mandibular defects were reconstructed with a bone graft from the iliac crest in three cases and by the costochondral rib graft in three cases and in one case excision along with margin was carried out (no: 6). Regarding the maxillary lesions, in one case the surgical treatment was carried out by maxillectomy (no: 5), in two cases excision along with margin was done (nos: 8, 10). Post-operative healing was uneventful in all cases.
All the patients were regularly followed-up for a mean of 3.3 years with no recurrence. Follow-up is still going on in few cases (Figs. 1–12).
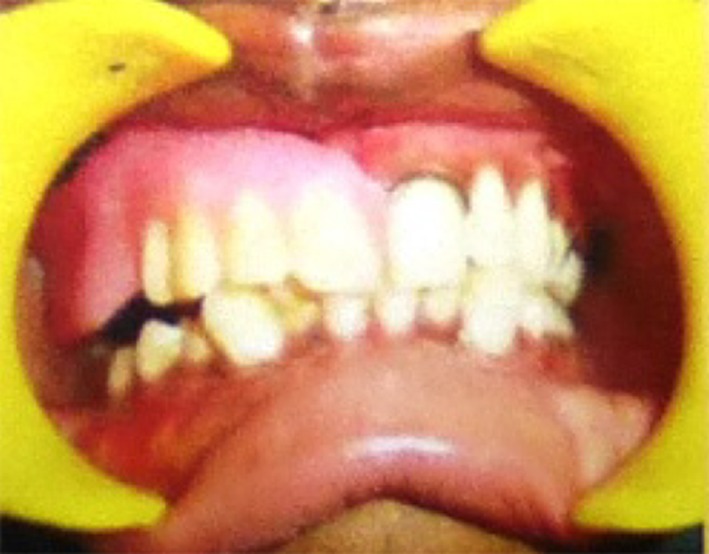
Fig. 2.

Vestibular obliteration seen on the right side from 12 to 17
Fig. 3.

MDCT axial section showing well defined lesion occupying the entire right maxilla measuring about 5.7 × 6 cm roughly oval in shape, encapsulated by a hypodense fibrous capsule, surrounded by a hyperdense corticated border. Internal structure appears to have heterogeneous density giving ground glass appearance extending medially into the nasal cavity and laterally involving the maxillary sinus
Fig. 4.
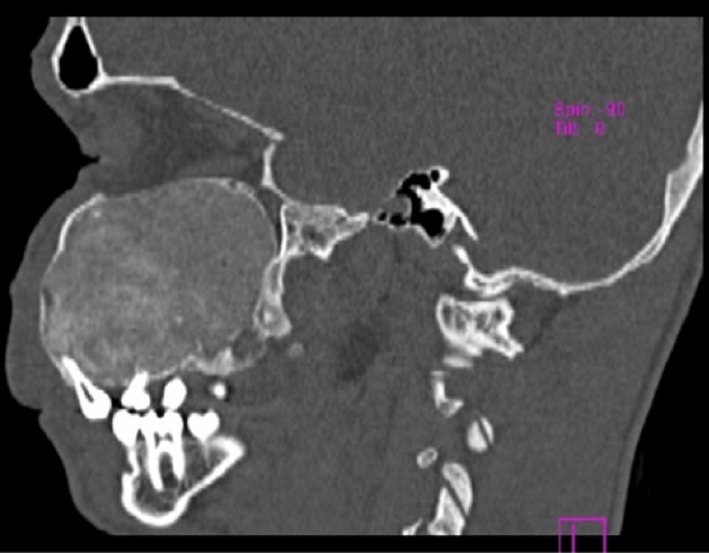
MDCT sagittal section extending posteriorly into the pterygoid plate and superiorly into the orbital floor
Fig. 5.

MDCT 3D reconstruction sections showing expansion of the right maxillary bone with multiple destruction of the bone, extending medially into the nasal cavity, pushing the orbital contents superiorly and laterally involving the maxillary tuberosity
Fig. 6.
Modified Weber Ferguson incision was given, tumor mass identified and the resection carried out using the palatal obturator. The defect was closed with skin graft harvested from the patient’s thigh
Fig. 7.

Facial symmetry attained, with no visible marks
Fig. 8.
Obturator placed
Fig. 9.
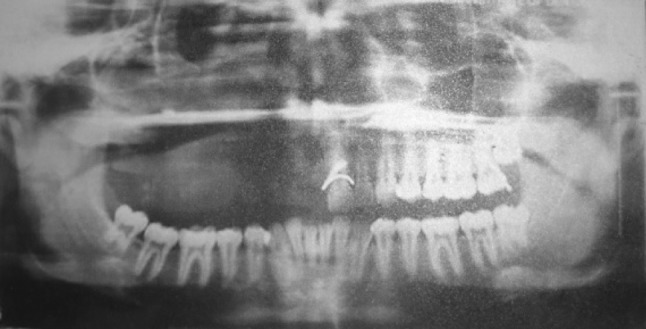
OPG showing the resected margin—with no recurrence
Fig. 11.

POF in the anterior maxilla (case no-8)
Fig. 1.

A seventeen year old male patient with a swelling on the right side of the face since 5 years
Fig. 12.

POF in the mandibular region (case no-6)
Discussion
Juvenile ossifying fibroma (JOF) remains one of the most frequently encountered benign FO lesion in maxillofacial region, most often diagnosed in children and adolescents. In the majority of previous reports [6], FD, central ossifying fibroma, cemento ossifying fibroma, juvenile ossifying fibroma [7] and osseous dysplasias [8] have been categorized as FO lesions.
Benign fibro-osseous lesions (FOLs) are a poorly defined and to some extent controversial group of lesions affecting the jaws and craniofacial bones.
FO lesions of the jaws have been generally divided into two major groups: those originating from the medullary bone (most often fibrous dysplasia, as well as osteoblastoma, cherubism, aneurysmal bone cyst) and those originating from the periodontal ligament, including ossifying and cemento-ossifying fibromas, and cemento-osseous dysplasias [9]. The above differentiation is important, because those from the medullary bone are usually more aggressive in their biological behaviour [10].
FO lesions are more frequent in female patients with a variable age of presentation; they often occur in children and adolescents, with average age at diagnosis being 9.5 years [1]. A male predilection was found in our study and the mean age of presentation was 22 years.
In childhood, although all varieties of odontogenic and nonodontogenic tumours may appear in the jaws, FO lesions have been reported to be the most common [11].
Maxilla has been reported to be the most common bone involved, with an incidence of 81 % [12], although previously it was reported that the ethmoid bone was the most common bone involved in craniofacial region [13]. On the contrary, in our study, the mandible was the most common bone affected (70 %); these differences may be attributed to the nosological entities included in each study.
Although the histological, and usually the clinical and radiographic features, may be similar for many of the FO lesions, they demonstrate a wide range of biological behaviour [14]. In our study all patients had painless expansile swelling; including enlargement of the jaws with facial asymmetry which was the main stay for their desire to seek treatment. In one patient where it was in maxilla the main symptom was blurred vision due to the compression of the orbit through its floor.
The diagnosis of these lesions is established by combining all acquired data. The panoramic radiograph usually followed by a CT (Computed Tomography) contributes to determine the lesion’s margins and its relation to vital structures [15]. An important radiologic diagnostic factor is the association of the lesion with the mandibular canal; odontogenic lesions, such as cemento-ossifying fibromas, cementoblastomas or cemento-osseous dysplasias, displace the mandibular canal downwards as they expand.
Conversely, lesions arising and developing below the canal, displacing it upwards, such as fibrous dysplasia, may be considered as non-odontogenic [16]. Biopsy (or a fineneedle aspiration biopsy) according to August et al. [17], is mandatory for histopathological diagnosis. In cases of large lesions, small biopsy specimens can be misleading, especially when heterogeneous or atypical tissue is present. For this reason multiple biopsies from different sites may be required [14]. In this study radiographic screening and biopsies were performed in all our cases.
Microscopically, benign FO lesions exhibit a connective-tissue matrix and islands/trabeculae of bone. Regardless of subtype, all lesions have a replacement of normal bone architecture by fibrous connective-tissue composed of fibroblasts and collagen, which contains varying amounts of mineralized material, including osteoid, mature bone, and/or cementum-like calcifications (Fig. 10). Overlapping of histopathologic findings renders sub-classification of benign FO lesions problematic.
Fig. 10.
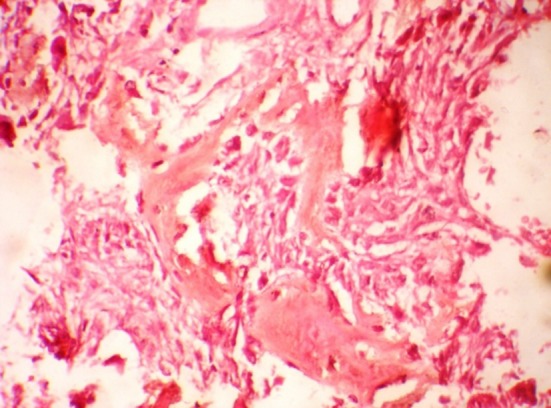
Photomicrograph of tumour shows the presence of trabeculae of fibrillar osteoid and woven bone (hematoxylin and eosin stain, original magnification x40)
Lately, different studies indicate that cytogenetics might be of ancillary use in the diagnosis of benign FO lesions because they possess distinct karyotypic abnormalities (for example a characteristic chromosomal arrangement is associated with ossifying fibroma) [18, 19]. Other studies of Toyosawa et al. [20], indicate that although FO lesions (especially fibrous dysplasia and ossifying fibroma) are similar disease entities, they show distinct differences that can be revealed by immunohistochemical detection of osteocalcin expression and PCR analysis with PNA for GNAS mutations at the Arg (201) codon.
Since the histological appearance does not predict the prognosis of the lesion or the rate of growth, therapeutic management should be based on the biological behaviour of the tumour, the clinical diagnosis, the careful interpretation of radiographs, the medical and family history and the disease process.
Treatment of FO lesions of the facial bones is highly individualized and once diagnosed, the management of each one is different ranging from wait-and-see period (observation and follow-up), to compulsory surgery to save the patient’s sight or reduce deformity [12, 16]. Most authors prefer conservative surgical treatment, but they avoid simple curettage, which may leave residual disease and make histological estimation difficult [1, 14].
A more radical approach including a craniofacial resection may be warranted for lesions that behave destructively, with rapid growth, pain and displacement of teeth [12, 14]. Conversely in our study the main stay of treatment was radical surgery in all of the cases. To avoid any chances to leave any residual disease and make histological estimation easy and further avoid any secondary surgery, segmental ostectomy was performed in six cases; maxillectomy was done in one case, excision along with margin in three cases.
In our study the following were positive findings, the lesion has male predilection with mandible being the most frequent location at body and angle region. The most common clinical presentation is asymptomatic swelling with asymmetry of face. Radiologically radiolucent along with radiopaque lesions are more commonly found. Our study also indicated radical resection of the tumor mass along with margin of healthy tissue proved to be the best method of treating these tumours, as there were no recurrences even after the mean follow up of 3.3 years.
Conclusion
Fibro-osseous lesions are a heterogeneous group of entities which share similar microscopic features, but exhibit a variety of clinical behaviour [21]. Thus, their treatment is highly individualized. In all of the cases the main stay of the treatment was radical surgery. Occasionally the post-operative bone defect requires restoration with bone grafts. In all the cases long-term follow-up is always necessary, to document the clinical biological behaviour and because recurrence can appear even after a long time post-operatively.
References
- 1.Mehta D, Clifton N, McClelland L, Jones NS. Paediatric fibro-osseous lesions of the nose and paranasal sinuses. Int J Pediatr Otorhinolaryngol. 2006;70:193–199. doi: 10.1016/j.ijporl.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 2.Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1985;43:249–262. doi: 10.1016/0278-2391(85)90283-6. [DOI] [PubMed] [Google Scholar]
- 3.Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1993;51:828–835. doi: 10.1016/S0278-2391(10)80097-7. [DOI] [PubMed] [Google Scholar]
- 4.Kramer IRH, Pindborg JJ, Shear M. Histological typing of odontogenic tumours WHO international classification of tumours. 2. London: Springer; 1992. [Google Scholar]
- 5.Kramer I, Pindborg J, Shear M. The WHO histological typing of odontogenic tumors, a commentary on the second edition. Cancer. 1993;70:2988–2994. doi: 10.1002/1097-0142(19921215)70:12<2988::AID-CNCR2820701242>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 6.Vegas Bustamante E, Gargallo Albiol J, Berini Aytés L, Gay Escoda C. Benign fibro-osseous lesions of the maxillas: analysis of 11 cases. Med Oral Pathol Oral Cir Bucal. 2008;13:653–656. [PubMed] [Google Scholar]
- 7.Slootweg PJ, Panders AK, Koopmans R, Nikkels PGJ. Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathological aspects. J Oral Pathol Med. 1994;23:385–388. doi: 10.1111/j.1600-0714.1994.tb00081.x. [DOI] [PubMed] [Google Scholar]
- 8.Abdelsayed RA, Eversole LR, Singh BS, Scarbrough FE. Gigantiform cementoma: clinicopathologic presentation of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:438–444. doi: 10.1067/moe.2001.113108. [DOI] [PubMed] [Google Scholar]
- 9.Sarwar HG, Jindal MK, Ahmad SS. Cemento-ossifying fibroma—a rare case. J Indian Soc Pedod Prev Dent. 2008;26:128–131. doi: 10.4103/0970-4388.43195. [DOI] [PubMed] [Google Scholar]
- 10.Hamner JE, III, Scofield HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane origin. An analysis of 249 cases. Cancer. 1968;22:861–878. doi: 10.1002/1097-0142(196810)22:4<861::AID-CNCR2820220425>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 11.Khanna S, Khanna NN, Varanasi MS. Primary tumors of the jaws in children. J Oral Surg. 1979;37:800–804. [PubMed] [Google Scholar]
- 12.Panda NK, Parida PK, Sharma R, Jain A, Bapuraj JR. A clinicoradiologic analysis of symptomatic craniofacial fibro-osseous lesions. Otolaryngol Head Neck Surg. 2007;136:928–933. doi: 10.1016/j.otohns.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 13.Lustig LR, Holliday MJ, McCarthy F, Nager GT. Fibrous dysplasia involving the skull base and temporal bone. Arch Otolaryngol Head Neck Surg. 2001;127:1239–1247. doi: 10.1001/archotol.127.10.1239. [DOI] [PubMed] [Google Scholar]
- 14.Koury ME, Regezi JA, Perrott DH, Kaban LB. “Atypical” fibro-osseous lesions: diagnostic challenges and treatment concepts. Int J Oral Maxillofac Surg. 1995;24:162–169. doi: 10.1016/S0901-5027(06)80094-9. [DOI] [PubMed] [Google Scholar]
- 15. Assaf AT, Benecke AW, Riecke B, Zustin J, Fuhrmann AW, Heiland M et al (2012) Craniofacial fibrous dysplasia (CFD) of the maxilla in an 11-year old boy: a case report. J Craniomaxillofac Surg 40(8):788–792 [DOI] [PubMed]
- 16.McDonald-Jankowski DS. Fibro-osseous lesions of the face and jaws. Clin Radiol. 2004;59:11–25. doi: 10.1016/j.crad.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 17.August M, Faquin WC, Ferraro NF, Kaban LB. Fine-needle aspiration biopsy of intraosseous jaw lesions. J Oral Maxillofac Surg. 1999;57:1282–1286. doi: 10.1016/S0278-2391(99)90859-5. [DOI] [PubMed] [Google Scholar]
- 18.Parham DM, Bridge JA, Lukacs JL, Ding Y, Tryka AF, Sawyer JR. Cytogenetic distinction among benign fibro-osseous lesions of bone in children and adolescents: value of karyotypic findings in differential diagnosis. Pediatr Dev Pathol. 2004;7:148–158. doi: 10.1007/s10024-003-6065-z. [DOI] [PubMed] [Google Scholar]
- 19.Pimenta FJ, Gontijo Silveira LF, Tavares GC, Silva AC, Perdigão PF, Castro WH, et al. HRPT2 gene alterations in ossifying fibroma of the jaws. Oral Oncol. 2006;42:735–739. doi: 10.1016/j.oraloncology.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 20.Toyosawa S, Yuki M, Kishino M, Ogawa Y, Ueda T, Murakami S, et al. Ossifying fibroma vs fibrous dysplasia of the jaw: molecular and immunological characterization. Mod Pathol. 2007;20:389–396. doi: 10.1038/modpathol.3800753. [DOI] [PubMed] [Google Scholar]
- 21.Kolomvos N, Theologie-Lygidakis N, Christopoulos P, Iatrou I. Benign fibro-osseous lesions of the jaws in children. A 12-year retrospective study. J Craniomaxillofac Surg. 2013;41(7):574–580. doi: 10.1016/j.jcms.2012.11.029. [DOI] [PubMed] [Google Scholar]



