Abstract
Introduction
Orbital wall fracture implies a situation where disruptions of the walls or floor have occurred. It is a blowout type fracture where bone fragments with torn periosteum are pushed outside of the original bony orbit. There is no intact bone even near the defect area except the thin bone rim surrounding the blowout fracture. The purpose of this defect repair is to support orbital contents, free entrapped tissue, and, especially, restore the original orbital volume.
Material and methods
Ten patients (seven males and three females) who underwent repair of orbital floor factures with maxillary sinus bone grafts were included in this study. Surgical procedure for harvesting graft and its fixation was almost same in all operated cases.
Conclusion
The collection in the maxillary sinus due to fracture of floor of orbit, blood and bony fragments collected in the maxillary sinus can be easily drained and removed after removal of anterior wall of maxillary sinus and through the same approach you can reduce the floor of orbit manually to the proper position which helps to decease the orbital floor defect.
Keywords: Orbital floor, Anterior wall of maxillary sinus, Blowout fracture and autogenous bone graft
Introduction
Orbital floor fractures can be broadly classified as pure blowout fractures (isolated orbital floor fracture) or impure blowout fractures (associated with orbital rim fractures) often related to midface fractures as zygomatic-orbital-maxillary complex bone segments [1]. Because of the complex structure of the orbital walls, the fracture patterns vary considerably in their location as well as in their degree of severity. Multiple portions of the orbit can be fractured and several internal orbital walls therefore injure simultaneously [2]. Treatment of traumatic orbital injuries in damaged orbital wall reconstruction will continue to be a topic of considerable controversy. The ideal technique, which may involve different reconstructive materials and various surgical access sites, could be influenced by many factors, including characteristics of the maxillofacial trauma and the experience of the surgeons [1].
The ideal reconstruction material for orbital floor or wall reconstruction should be easy to mold, easy to anchor, biocompatible, strong, and readily available. It should restore orbital form and support function [2]. For orbital floor fractures the surgeon has the option of using either alloplastic or autogenous implants. The autogenous sites used in orbital surgery include the calvarial and iliac bone, mandibular symphyseal graft, split rib and cartilage. There are two main types of alloplastic materials: resorbable and nonresorbable. The resorbable include Gelfilm, polygalactin film, and a variety of homografts. The nonresorbable materials include Silastic sheets, Marlex mesh, Teflon, Prolene, polyethylene and metallic alloys [3]. Alloplastic materials have been used with caution, because they increase the risk of infection and have the potential for extrusion. The treatment of choice to restore absent bone segments in facial skeleton is to replace the defect with autogenous bone. Currently, the trend is to favour the use of autogenous grafts. This article reports the use of maxillary bone for the repair of traumatic orbital floor defects in ten cases.
Patients and Methods
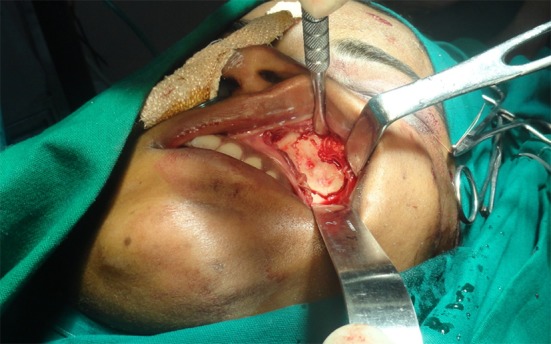
Ten patients (seven males and three females) who underwent repair of orbital floor fractures with maxillary sinus bone grafts at Swargiya Dadasaheb Kalmegh Smruti dental college and hospital in the department of oral and maxillofacial surgery were included in this study. Surgical procedure for harvesting graft and its fixation was almost same in all operated cases. The typical appearance of orbital floor fracture in coronal computed tomographic scan of a patient with orbital floor fracture can be seen in Figs. 1 and 2. The orbit was approached through a subciliary approach (Fig. 3). The temporary tarsorrhaphy suture was carried out. The retraction was carried out by malleable retractor to the level of the inferior orbital rim. The periosteum overlying the orbital rim was incised and elevation of the periosteum and orbital floor exploration was accomplished in the routine fashion until the fracture was exposed [3].
Fig. 1.
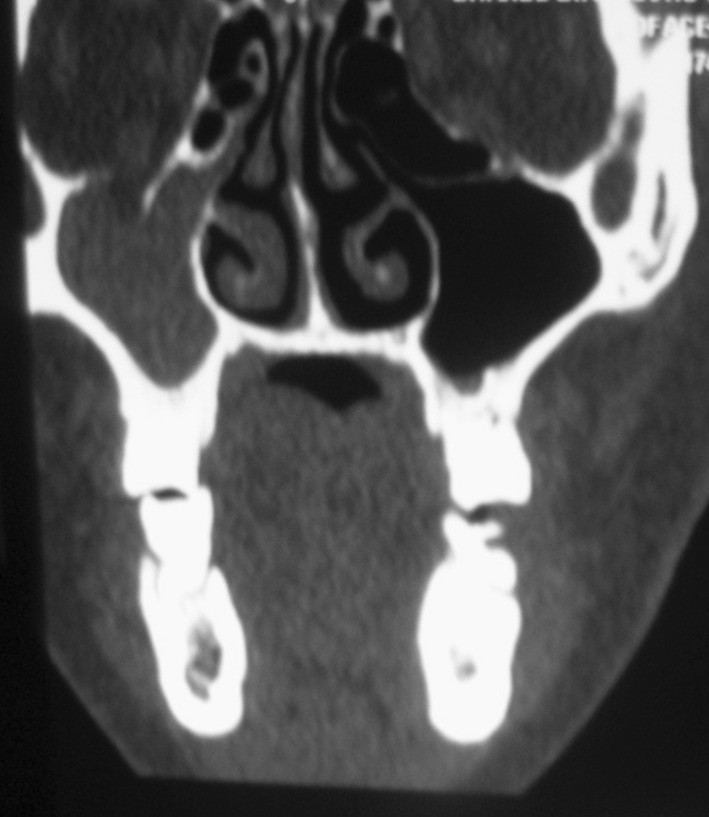
Coronal computed tomographic scan of a patient with right orbital floor fracture
Fig. 2.
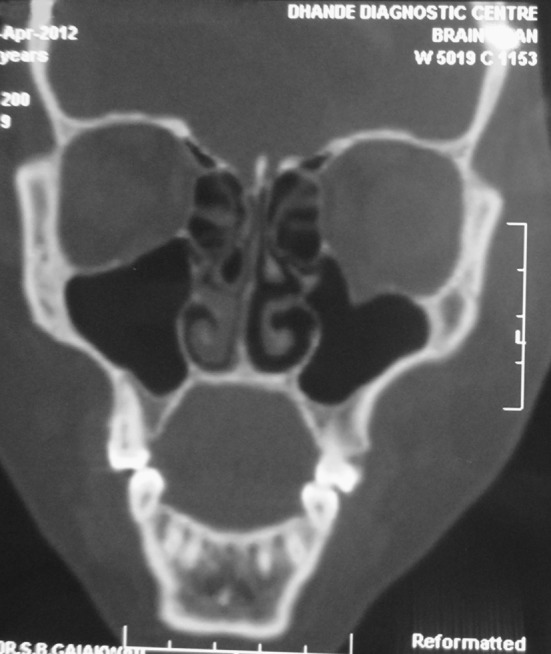
Coronal computed tomographic scan of a patient with left orbital floor fracture
Fig. 3.

Case 1—subciliary approach for orbital floor fracture
After this the intraoral vestibular incision was made through mucosa and periosteum in the upper gingival buccal sulcus (Fig. 4) leaving 0.5 cm of mucosa inferiorly so that resuturing of the mucosa is facilitated. The area was first injected with xylocaine 1 % with 1:100,000 epinephrine to enhance hemostasis. The mucoperiosteum was raised with a periosteal elevator to the level of the infra orbital nerve superiorly; laterally to the beginning of the curvature of the maxillary sinus, and medially to 1 cm before approaching the pyriform aperture. Soft tissue retractors were then placed deep into the periosteum, and the anterior maxillary wall was visualized with this blunt dissection. An area of anterior maxillary sinus wall was outlined with methylene blue (approximately 2.5 × 1.5 cm) and a high-speed drill was used circumferentially to harvest the anterior maxillary bone for grafting (Fig. 5). The graft outlined for harvesting (Fig. 6) was well marked away from maxillary teeth apices, pyriform aperture and infraorbital foramen to avoid inadvertent trauma to these vital structures. The antrum was then entered and suctioned clear of debris and blood. The infraorbital nerve in the roof of the sinus was identified and isolated [4].
Fig. 4.

Intraoral approach for anterior wall of maxillary sinus through mucosa and periosteum in the upper gingival buccal sulcus
Fig. 5.

Harvesting of the anterior maxillary bone for grafting
Fig. 6.
Graft outlined for harvesting
The repair was continued with placement of the anterior maxillary bone graft (Fig. 7) into the floor of the orbit. This harvested graft was guided into place through the subciliary approach after all scarred and fibrosed parts of the orbital musculature and periorbita were placed back into the orbit (Fig. 8). The maxillary bone graft was placed over the orbital floor in order to completely cover the margins of the defect. No metal fixation of the graft was used, but care was taken to ensure that the graft was well behind the inferior orbital margin and it was secured to the infraorbital margin by drilling small holes and passing vicryl suture through the graft and infraorbital bony ridge (Fig. 9). The subciliary incision was closed with absorbable 5/0 Vicryl suture and 6/0 prolene suture layer wise [3]. Intraorally, the periosteum and overlying mucosa were then repositioned and sutured. Post operative evaluation was done of the recipient site after 6 months with coronal view of CT scan (Fig. 10) and the donor site evaluation was done with PNS(waters) view of maxilla (Fig. 11) along with the axial view of the CT scan (Fig. 12). Both the recipient as well as donor site healing was uneventful.
Fig. 7.

Anterior maxillary bone graft
Fig. 8.

Bone graft guiding through the subciliary approach into the orbital floor defect
Fig. 9.

Graft placement well behind the inferior orbital margin
Fig. 10.

Post-operative coronal CT showing repair of the defect with the graft after 6 months
Fig. 11.

Postoperative PNS view of patient at 6 months follow up showing healing of graft on right side of orbital floor and anterior wall of maxillary sinus
Fig. 12.
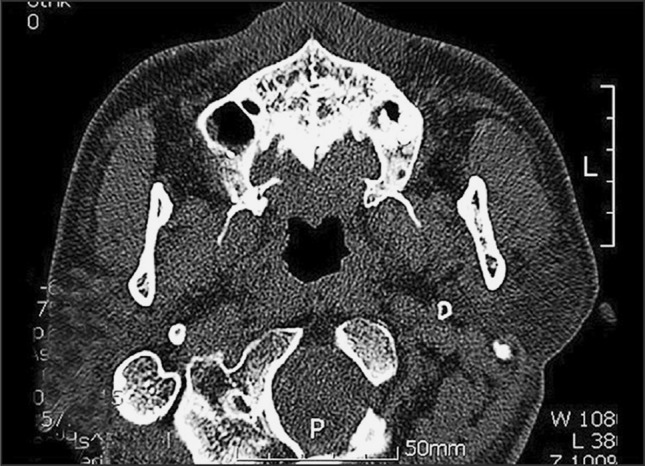
Post-operative axial CT evaluating the healing of the donor site after 10 months
The postoperative clinical course was successful in all patients with full recovery of ophthalmological function except one case of postoperative epiphora (Table 1) which subsided on its own after some days without any intervention by ophthalmologist. The preoperative and compared postoperative ophthalmological examination was normal in all operated cases. The patients were satisfied with the aesthetic results (Table 2). There was no inflammatory or infectious complication at the surgical sites or the maxillary sinus, nor any intraoral complications, such as oro-antral fistulas, dental pulp or periodontal problems. Furthermore, there has been no other complication, such as cutaneous fistula, eversion of an eyelid, cysts of sebaceous glands, or periorbital cellulitis, extrusion of graft in the close clinical follow-up of 1 year period.
Table 1.
Postoperative complications
| Complications | Number (n-10) |
|---|---|
| Epiphora | 1 |
| Infection | 0 |
| Enophthalmos | 0 |
| Graft exposure | 0 |
| Graft rejection | 0 |
Table 2.
Results of all ten cases
| Serial number and findings | Diplopia | Ocular level | Vision | |||
|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Postop | |
| Case 1 (male) | NS | NS | C | N | N | N |
| Case 2 (female) | NS | NS | N | N | N | N |
| Case 3 (male) | NS | NS | N | N | N | N |
| Case 4 (male) | NS | NS | N | N | N | N |
| Case 5 (male) | NS | NS | N | N | N | N |
| Case 6 (male) | NS | NS | N | N | N | N |
| Case 7 (female) | NS | NS | C | N | N | N |
| Case 8 (male) | NS | NS | N | N | N | N |
| Case 9 (male) | NS | NS | N | N | N | N |
| Case 10 (female) | NS | NS | N | N | N | N |
NS not seen, N normal, C change
Discussion
Orbital wall fracture implies a situation where disruptions of the walls or floor have occurred. It is a defect fracture where bone fragments with torn periosteum are pushed outside of the original bony orbit. There is no intact bone even near the defect area except the thin bone rim surrounding the defect fracture. The purpose of defect repair is to support orbital contents, free entrapped tissue, and, especially, restore the original orbital volume. If the volume cannot be restored, enophthalmos will inevitably occur. Even a 5 % change in volume leads to clinically detectable changes in soft tissue position, resulting in enophthalmos [2].
A case reported by Kanno et al. [1] concluded that use of the anterior maxillary sinus wall in corrective surgery of open reductions and internal fixation of maxillo-zygomatico-orbital complex fractures can allow for good orbital floor reconstruction. It is less invasive and less time consuming, and successful clinical results have been obtained.
The maxillary approach to the repair of orbital fractures either in the early immediate stage or the late reconstructive stage is a valuable adjunct to the reconstructive surgeon. The anterior wall of the maxillary antrum not only is an excellent source of implant material but also allows the added advantage of increased exposure for visualization and manipulation. It is also particularly advantageous to use the maxillary antrum as a further means of support when the orbital floor is compromised and needs additional inferiorly based support through either gauze or balloon. This is particularly applicable when the orbital floor fracture is complicated by adjacent facial bone fracture [4].
The study conducted by Cieślik et al. [5] in eighteen patients indicates that the maxillary bone graft technique is a good and simple orbital floor reconstruction method. They suggested that shortening of surgery time and limitation of operative procedures are advantages of this method.
A case report by Sabnis et al. [3] suggested that the anterior antral wall bone is the ideal implant material for the reconstruction of orbital floor defects in the severely injured patient. The bone is thin and membranous and possesses characteristics that are similar to those of the bone of the orbital floor. Because of its biocompatibility and lack of donor site morbidity, the use of an antral wall bone graft is a superior reconstructive option.
The study conducted by Lee [6] in 41 patients concluded that the use of maxillary antral wall bone for the repair of orbital floor fractures is a highly reliable technique that carries minimal morbidity.
Autologous bone grafting has thus persisted as a reliable, safe, and lifelong material for reconstruction of the orbit, except when donor site morbidity results in the need for surgical intervention. Very good clinical results have been reported by some surgeons, justifying the use of grafts from the anterior maxillary sinus wall primarily for pure blowout fractures. The main advantage of this technique is the adjacent locations of the injury and operative field, facilitating the performance of open reduction and eliminating the need for further surgical interventions. Further, we can manipulate the site of the removed anterior maxillary sinus to reduce the herniated orbital contents, usually with a forefinger, and we can examine the condition of the reconstructed support through the anterior sinus [1].
Conclusion
As per our method, it proves to be one of the best methods for reconstruction of floor of orbit. Considering the accessibility for anterior wall of maxillary sinus, it is easy through intraoral incision. As there is collection in the maxillary sinus due to fracture of floor of orbit, blood and bony fragments collected in the maxillary sinus can be easily drained and removed after removal of anterior wall of maxillary sinus and through the same approach you can reduce the floor of orbit manually to the proper position which helps to decease the orbital floor defect. It also helps in inspection of maxillary sinus and floor of orbit. Quality of anterior wall of maxillary sinus as a graft is thin and adaptable and it is well adapted and contoured to the defect in the floor of orbit. This type of bone graft is mainly suitable for moderate size defect in floor of the orbit.
Conflict of interest
None.
Funding
None
References
- 1.Kanno T, Sukegawa S, Takabatake K, Takahashi Y, Furuki Y. Orbital floor reconstruction in zygomatic-orbital-maxillary fracture with a fractured maxillary sinus wall segment as useful bone graft material. J Oral Maxillofac Surg Med Pathol. 2013;25:28–31. doi: 10.1016/j.ajoms.2011.09.003. [DOI] [Google Scholar]
- 2.Kontio R. Treatment of orbital fractures the case for reconstruction with autogenous bone. J Oral Maxillofac Surg. 2004;62:863–868. doi: 10.1016/j.joms.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Sabnis R, Vyas S, Satish M, Pandit M (2011) Reconstruction of orbital floor fractures with maxillary bone: a case report. Indian J Dent Res Rev 31–32
- 4.Sachs ME. Orbital floor fractures: the maxillary approach. Adv Ophthalmic Plast Reconstr Surg. 1981;6:387–391. [PubMed] [Google Scholar]
- 5.Cieślik T, Skowronek J, Cieślik M, Cieślik-Bielecka A. Bone graft application from anterior sinus maxillary wall in orbital floor reconstruction. J Craniofac Surg. 2009;20(2):512–515. doi: 10.1097/SCS.0b013e31818436a5. [DOI] [PubMed] [Google Scholar]
- 6.Lee HH. Reconstruction of orbital floor fractures with maxillary bone. Arch Otolaryngol Head Neck Surg. 1998;124:56–59. doi: 10.1001/archotol.124.1.56. [DOI] [PubMed] [Google Scholar]


