Abstract
Introduction
The temporomandibular joint (TMJ) is anatomically complex; with its close proximity to neurovascular structures, including the facial nerve that gives a high degree of difficulty during surgical exposure. When the first description on TMJ surgery by Orlow in 1913 was published it gave an account describing the basic retroauricular, preauricular, endoaural and submandibular approaches, on treatment of articular pathologies as used today. The proposed study of the ‘Bat Wing’ approach, first described in 1993 by Garcia y Sanchez J.M. as a surgical alternative, offers great advantages is that it avoids the section of the ear canal and provides a wide surgical field. The management of the proposed technique has wide application with multiple joints addressed, achieving major objectives such as avoiding facial nerve damage, as well as avoiding the section of the external auditory canal with an optimum visibility of the operative field.
Material and methods
The Department of Maxillofacial Surgery National Medical Center XXI Century records over a period of approximately 18 months have completed twenty TMJ surgeries using the ‘Bat Wing’, approach.
Conclusions
The bat wing approach is a surgical alternative that offers broad exposure of the surgical field in TMJ, it is effective and meets the goal of exposing the area to intervene safely, good visibility and access to the site to intervene. It perfectly fulfills the above described.
Electronic supplementary material
The online version of this article (doi:10.1007/s12663-014-0724-7) contains supplementary material, which is available to authorized users.
Keywords: Temporomandibular joint, Facial nerve, Approach, External auditory canal
Anatomy of the Temporomandibular Joint (TMJ)
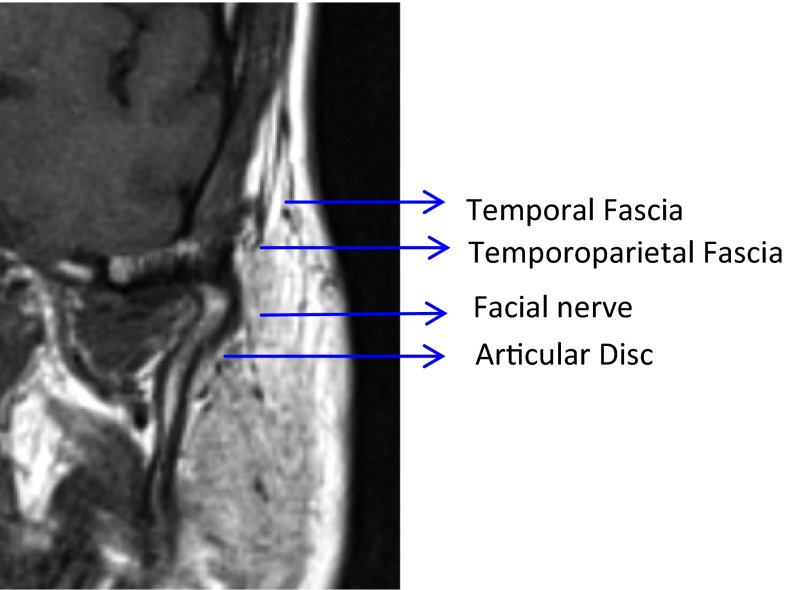
The Temporomandibular Joint (TMJ) belongs to the type of ginglymoarthrodial joint, having free motion, made at the top by a cavity (mandibular fossa, glenoid fossa) and condylar bone surface being part of the mandible inferiorly, both separated by the articular disc. The latter structure is itself complex, so this work is focused to study the division of it, as follows (Fig. 1).
Fig. 1.
Magnetic resonance view of anatomy of the temporomandibular joint
The superficial temporal artery, transverse facial artery, the auriculotemporal nerve and the facial nerve (VII cranial nerve) are intimately involved in the surgical dissection of the TMJ [1, 2].
The superficial temporal artery, one of the terminal branches of the external carotid, begins its journey behind the mandibular condylar neck and deep into the parotid level, crosses the posterior root of the zygomatic and enters the temporal, distributed in the region of the scalp [3, 4].
The transverse facial artery arises from the base of the superficial temporal artery and runs almost transversely through the face with the outer path of the masseter muscle area, approximately 1.5 cm below the zygomatic arch.
The auriculotemporal nerve, cutaneous sensory branch of the mandibular division of V cranial nerve travels just behind the neck of the condyle in the lower level of the capsule attachment. It travels up through the root of the zygomatic arch just behind the superficial temporal artery [5–7].
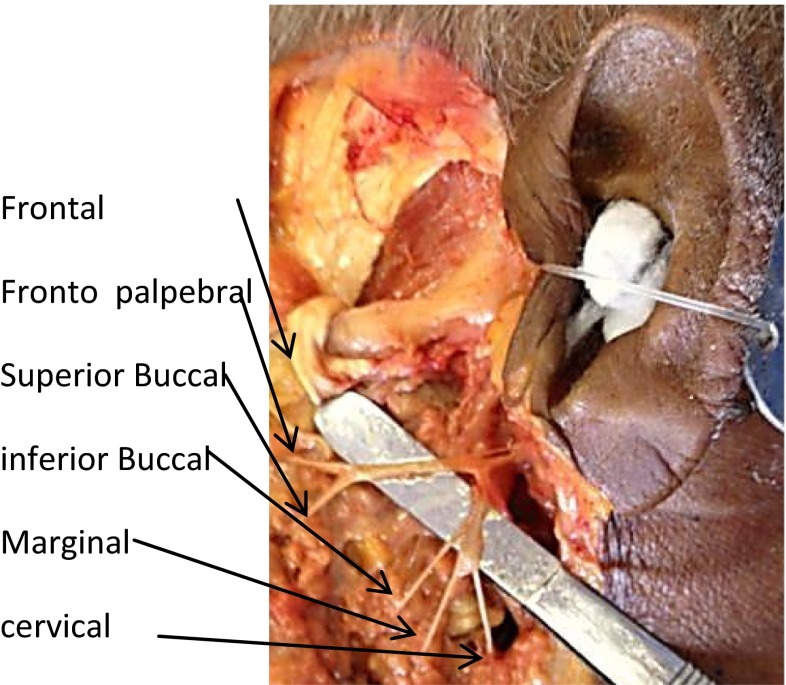
According to Kreutzinger, in a study of fifty-four dissecting cadavers, the facial nerve was measured relative to bony structures, with the results described below. The distance from the most anterior concavity of the ear canal to the temporal branch of the facial nerve, reported an average of 2.0 ± 0.5 cm, with a range of 0.8–3.5 cm. The average distance from the bifurcation of the main trunk of the facial nerve to the lower concavity of the ear canal was 2.3 ± 0.28 cm, with a range from 1.5 to 2.8 cm. The average distance from the bifurcation of the facial nerve to post-glenoid tubercle was 3.0 ± 0.31 cm, with a range of 2.4–3.5 cm. The knowledge of the distances and the range of the branches of the facial nerve from bony landmarks within the surgical field provide the surgeon a better understanding of the areas of greatest risk [5, 8–10] (Fig. 2).
Fig. 2.
View in corpse of anatomical relations to the zygomatic arch facial nerve respect to the extent of external auditory canal
Surgical Technique
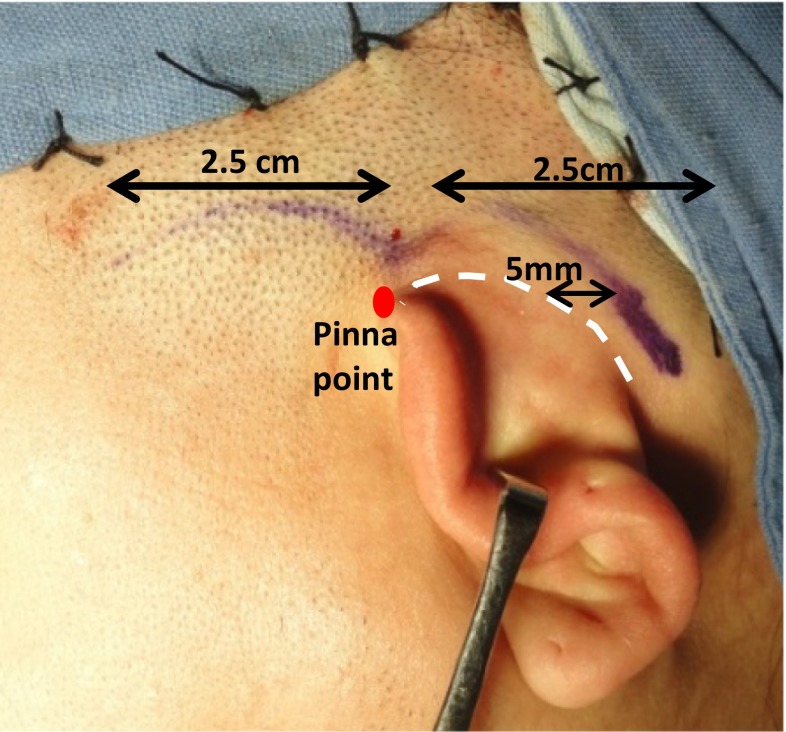
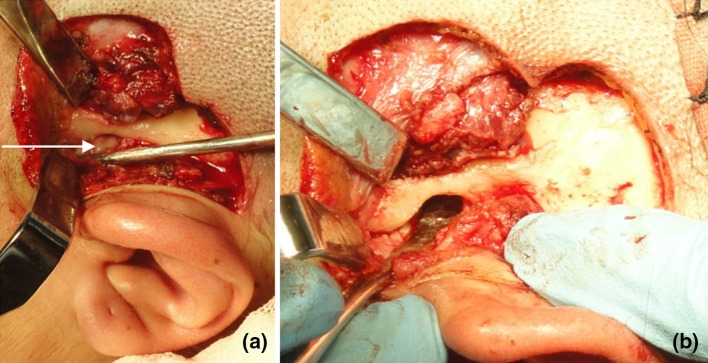
The approach described by Garcia y Sanchez J.M. in 1993, (Fig. 3a, b) avoids the section of the external auditory canal (EAC).
Fig. 3.
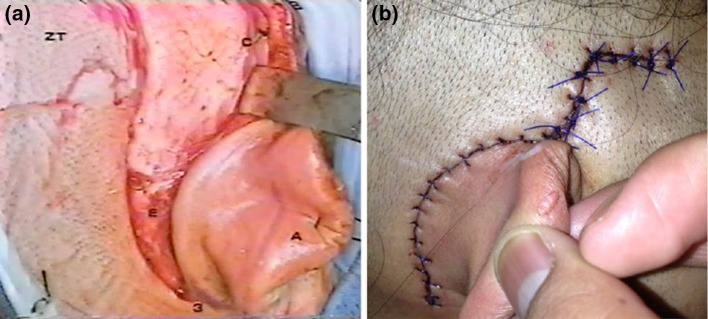
a, b, Original technique of modified retroauricular approach without external auditory canal section
The incision design starts supra pinna, and is 2.5 cm long. Incise from anterior region to posterior, above the top implantation of the pinna point and parallel to the path of the zygomatic arch.
From this point, the incision is continuous 5 mm behind and following the retroauricular creasing half way to mastoid region 2.5 cm (Fig. 4).
Fig. 4.
Marking of the bat wing approach
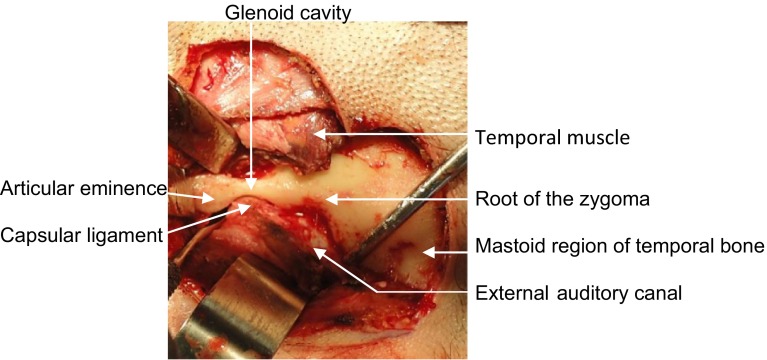
Incision is made in the first instance with a scalpel, covering the skin and subcutaneous tissue, allowing exposure of the superficial temporal fascia (Fig. 5). From here, incision is directed to the retroauricular region with an electro scalpel to the periosteum and continues with the lift of a subperiosteal flap, dissection is made 5 mm before the entire exposure of EAC; once EAC is located, dissection continues forward until you find the root of the zygoma arch (Fig. 6). This allows keeping intact the EAC (Fig. 7).
Fig. 5.

The incision is made in the first instance covering the skin and subcutaneous tissue
Fig. 6.

Incision in retroauricular region with an electro scalpel to the periosteum
Fig. 7.
Dissection takes a course perpendicular to the ear canal
At this point no longer cut monopolar electrocautery, only use bipolar and scalpel, mindful that palpebral branch damage is possible crossing any part of the articular eminence to its anterior portion.
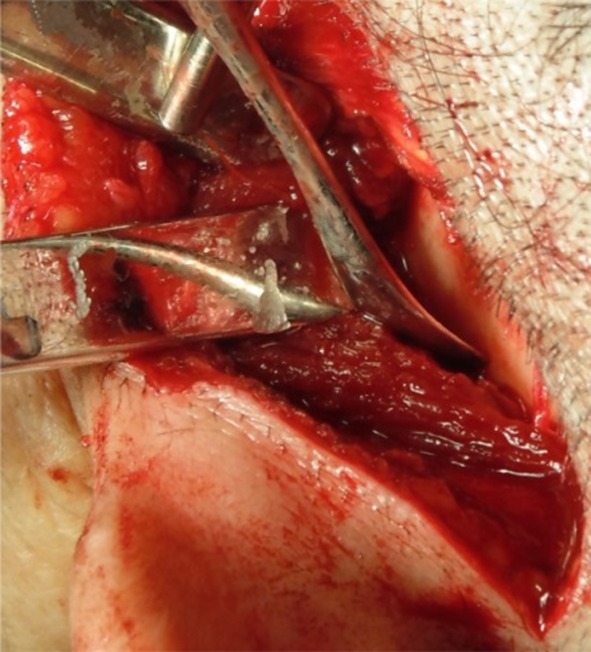
Now above along zygomatic arch, start tunneling portion of temporal muscle with metzembaum scissors, clamping with two hemostat clamps, cutting with scalpel and cauterizing with bipolar, repeating these steps from the superficial temporal fascia and the posterior fibers of the temporalis muscle (Fig. 8). It should be noted that this dissection is subperiosteal and the above limit is the anterior slope of the articular eminence.
Fig. 8.
Tunneling along the zygomatic arch
If you want to extend this incision for reconstructive purposes resection of neoplasms, there is no contraindication.
Proceed to approach the superior articular space which can be performed in two ways:
Make a hydro dissection by infiltration of saline solution on external superior insertion of the joint capsule.
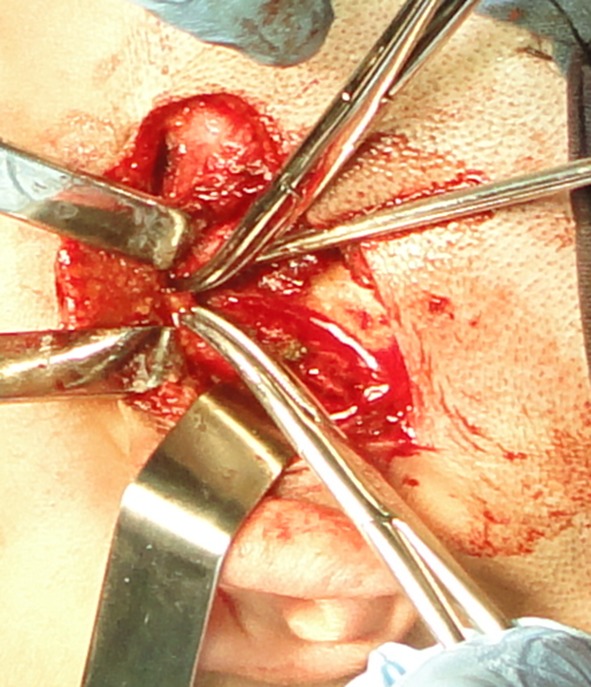
With a sharp dissector capsule is detached from posterior portion, addressing for superior joint space maintaining the cutting part of the tool in bone contact and the flat part to the capsule and articular disc (Fig. 9).
Fig. 9.
Detachment of the capsule with a sharp dissector
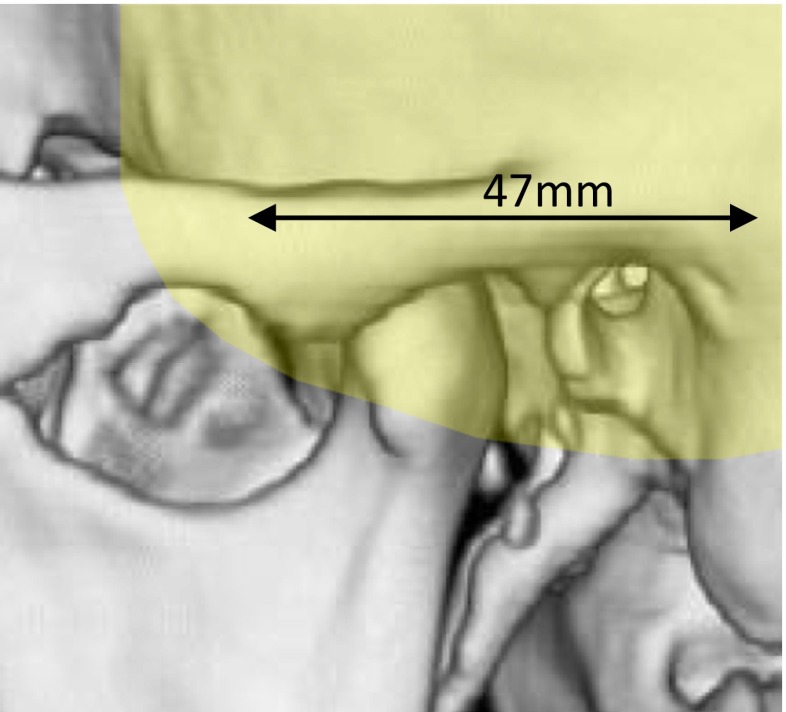
The approach gives a view from the front of the articular eminence to the posterior part of the glenoid cavity and union with the ear canal, as shown in the 3D reconstruction which gives longitudinal exposure of 47 mm (Fig. 10).
Fig. 10.
Exposition área
Dissection and Opening of the Glenoid (Articular Decompression)
With a curved dissector with the cutting part always attached to the bone so as to prevent damage to the meniscus, dissection begins at the zenith of the glenoid cavity, detaching joint capsule from the zenith or entering from top of the cavity making a lateral move from the back to the front of the glenoid cavity. Capsule is detached in its entirety and all around the articular tubercle. Once this step is achieved, start again on the zenith of the glenoid to the medial wall of the joint and proceed toward the rear wall and to the anterior part of the articular tubercle medially.
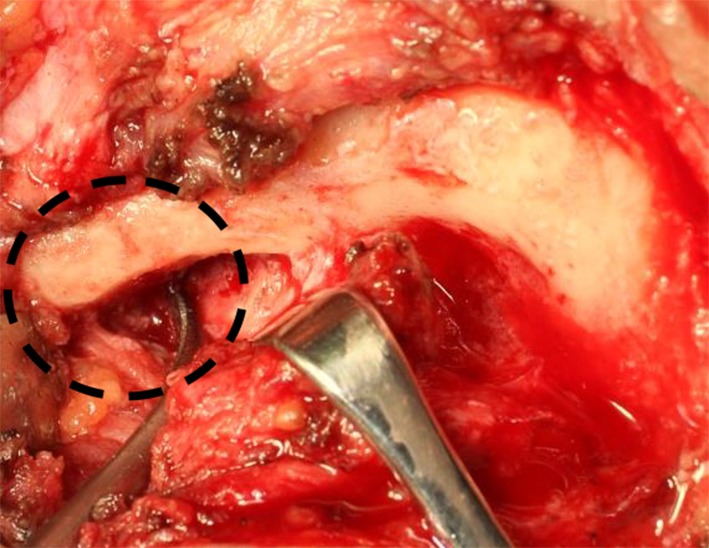
Decompression of the articular meniscus is made with a wider dissector (seldin) introduced to this zenith medial wall with strong traction with the blunt edge of seldin, down about 6–10 mm, which eliminates adhesions. Having released and completely exposed the superior joint space, you can proceed with arthroplasty, properly protecting the meniscus with a dissector Molt (Fig. 11a, b).
Fig. 11.
a Exposure of meniscus (arrow) b Protection of the meniscus with a dissector
Fulguration of Bilaminar Zone
It will be done, once decompression of the articular meniscus is made and prior to the emineplasty, with bipolar electrocautery the bilaminar zone, this eliminate pain symptoms that runs from the back wall of the fissure of glaser and emerges into the bilaminar zone.
Eminoplasty (Myraugh Technique)
After fulguration, proceed to eminoplasty of the tubercle of the articular eminence (Figs. 12, 13), with the seldin and another médium dissector with the edge in contact with the bone surface of the tuber nerve to disk; proceed to shave almost fully leaving it at the level of the zygomatic arch and verify that there are no bone spicules.
Fig. 12.

Pre-eminoplasty
Fig. 13.
Post eminoplasty
It is important to remember that the joint spaces should be washed to remove blood remnants before undertaking the capsulorrhaphy.
Once the procedure is finished (Fig. 14) it is necessary to suture in layers, first instance with the repair of the joint capsule with an absorbable material suturing to the superficial temporal fascia (Fig. 15).
Fig. 14.
Eminectomy
Fig. 15.

Suture in layers
The temporalis muscle fibers that have been cut and the superficial temporal fascia at its posterior portion is repaired. The skin is sutured with 4–0 nylon leaving a scar in an area without aesthetic implications (Figs. 16, 17).
Fig. 16.

Skin suture
Fig. 17.

Sixth month postoperative view of bat wing approach, is completely aesthetic and the covered by the hair
The patient undergoes early physical treatment as orally tolerated, is installed a fibrous diet and mouth opening and closing exercises. This postoperative treatment is essential for the success of the surgery [11, 12].
In a period of 18 months, The Department of Maxillofacial Surgery, National Medical Center XXI Century, have completed 20 TMJ surgeries using the ‘Bat Wing’, with excellent results. This approach has indications and contraindications. [Table 1; 13–15].
Table 1.
Approach indications and contraindications
| Indications and advantages | Contraindications |
|---|---|
| An excellent technique to avoid damaging the facial nerve in its palpebral branch, and can be facially addressed from the back of the TMJ to the front of the articular eminence without causing tearing of EAC | Treatment of ankylosis and condylar prosthesis. For these cases the preauricular approach exposes better access to the region |
| You can easily address the upper and lower joint compartment and have a broad perspective of the bilaminar zone and meniscus, until the anterior tubercle, where it attaches to the upper fibers of the lateral pterygoid (external) | Treatment for fully displaced fractures, both towards the medial intracapsular and extracapsular wall, requiring osteosynthesis of the subcondylar part or low anterior medial displaced fractures |
| Approaches with purpose of electro-lightening purposes the bilaminar zone | The same with respect to pathology of the subcondylar region |
| Plasty of articular tubercle or partial or total eminectomy | Approach the medial below space at articular tubercle level |
| Plication of condylar meniscus | Fractures involving the region subcondylar or a lower level |
| Reshaping the top of the condylar head | |
| Approaches for intracapsular fractures of the upper third of the condylar head | |
| The technique allows a vertical incision of the capsule from the top of the greater curvature of the glenoid to 1 cm below this. For procedures of the top condylar head and inferior articular space | |
| Approach for zygomatic arch fractures | |
| Neuro-surgical procedures | |
| Surgical access of low temporal fossa and even involving the middle cranial fossa as well as the roof of the glenoid | |
| Ear surgery procedures of upper EAC |
Conclusion
The Bat Wing approach is a surgical alternative that offers broad exposure of the surgical field in TMJ also offers the important advantage of avoiding the section of the ear canal, besides the important advantage of having full security to prevent severe cranial nerve damage.
One of the main fears of surgeons approaching TMJ is the palpebral branch of the seventh pair since there is uncertainty in recovering the patient’s anesthetic effect, submitting a paresis or serious injury to the facial nerve. In cases where this technique has been used since 1993 to date no damage to palpebral branch of the facial nerve or stenosis of the EAC was found.
One of the goals of any surgical technique proposed is that it is effective and meets the goal of exposing the area to intervene safely, good visibility and access to the site to intervene. It perfectly fulfills the above described.
Finally we can say that the Bat Wing approach is superior to any existing pre auricular approach because it achieves an average exposure of almost 50 mm without damage to facial nerve or EAC section.
Electronic supplementary material
References
- 1.Gérard JM, Monnoye V, Deggouj N, Gersdorff M. A classical retro-auricular incision in cochlear implantation. Mediterr J Otol. 2005;1(3):105–109. [Google Scholar]
- 2.Cordova S, D’Arpa F, Moschella M. An innervated retroauricular skin flap for total earlobule reconstruction. Br Assoc Plast Surg. 2003;56:818–821. doi: 10.1016/S0007-1226(03)00378-3. [DOI] [PubMed] [Google Scholar]
- 3.Bolini JC, Monteiro Marone S, Martucci O, Gonçalez F. Evaluation of the organic and functional results of tympanoplasties through a retro-auricular approach at a medical residency unit. Braz J Otorhinolaryngol. 2011;77(2):229–236. doi: 10.1590/S1808-86942011000200013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanno T, Kiya N, Sunil MV (2003) Microsurgical anatomy of the retroauricular, transcervico mastoid infralabyrinthine approach to jugular foramen. Neuroanatomy 2:28–34
- 5.Cordova A, D’Arpa S, Pirrello R, Giambona C, Moschella F (2008) Retroauricular skin: a flaps bank for ear reconstruction. J Plast Reconstr Aesthet Surg 61–3 [DOI] [PubMed]
- 6.Kalantar-Hormozi A, Loghmani S, Motamed S. Using hairy and non-hairy retroauricular-temporal composite flap in facial reconstruction. Arch Iran Med. 2009;12(6):566–569. [PubMed] [Google Scholar]
- 7.Jong-Lyel R. Extracapsular dissection of benign parotid tumors using a retroauricular hairline incision approach. Am J Surg. 2009;197:e53–e56. doi: 10.1016/j.amjsurg.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 8.Datta G, Carlucci S. Reconstruction of the retroauricular fold by ‘nonpedicled’ superficial mastoid fascia: details of anatomy and surgical technique. J Plast Reconstr Aesthet Surg. 2008;61:S92–S97. doi: 10.1016/j.bjps.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Wei-Liang C, Si-Lian F. Removal of second branchial cleft cysts using a retroauricular approach. Head Neck Surg. 2009;31:695–698. doi: 10.1002/hed.20980. [DOI] [PubMed] [Google Scholar]
- 10.Lopez-Arcas JM, Martın M, Gomez E, Del Castillo J, Abelairas J, Salamanca L, Burguen M. The Guyuron retroauricular island flap for eyelid and eye socket reconstruction in children. Int J Oral Maxillofac Surg. 2009;38:744–750. doi: 10.1016/j.ijom.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 11.Weiliang C, Jingsong L, Zhaohui Y, Wang Y, Wang Z, Youyuan W. SMAS fold flap and ADM repair of the parotid bed following removal of parotid haemangiomas via pre- and retroauricular incisions to improve cosmetic outcome and prevent Frey’s syndrome. J Plast Reconstr Aesthet Surg. 2008;61:894–900. doi: 10.1016/j.bjps.2007.10.061. [DOI] [PubMed] [Google Scholar]
- 12.Morrison CM, Bond JS, Leonard A. Nasal reconstruction using the Washio retroauricular temporal flap. Br J Plast Surg. 2003;56:224–229. doi: 10.1016/S0007-1226(03)00092-4. [DOI] [PubMed] [Google Scholar]
- 13.Güven O. Treatment of temporomandibular joint ankylosis by a modified fossa prosthesis. J CranioMaxillofac Surg. 2004;32:236–242. doi: 10.1016/j.jcms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 14.García PJA, Gomez PA, Flores AM (2011) Uso de colgajo miofascial temporal remplazo de disco articular con abordaje retroauricular modificado. AMCBM Vol. 7: Núm. 3 o Septiembre-Diciembre o pp. 98
- 15.Garcia y Sanchez JM, Gomez PA, Vargas LD, Rengifo Lozano C (1993) Tratamiento definitivo para el dolor de la articulación temporomandibular. Pract odontol 14(5):11–8
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.