Abstract
Introduction
Replacement of missing tooth has evolved from removable dentures to fixed dentures and recently to dental implants. The need of sufficient bone around the endosseous implant is critical for the success of the implant. The present study was aimed to evaluate the efficacy of a novel implant (HYBRID IMPLANT-submitted for patency) for replacement of the missing teeth.
Materials and methods
1. Research design A prospective research design with a follow up after 1st week ,2nd week ,3rd week,1st month ,3rd month,6th month and 1st year postoperatively. 2. Sampling method Population: All patients who reported for replacement of missing teeth. Inclusion criteria 1. All patients above the age group of 16years 2. Patients who need replacement of single or multiple teeth in the anterior or posterior region of the maxilla and mandible. Exclusion criteria 1. Medically compromised patients. 2. Patients having craniofacial syndromes. 3. Sample size 5 patients were selected taking into consideration the inclusion and exclusion Criteria. Results PAIN All the patients were non symptomatic during the 1st month to 1st year postoperative periods.
Mobility
We experienced mobility during the 1st and 2nd postoperative periods where the implants were inserted in the mandibular molar region.
Bone loss
Radiographic assessment showed no bone loss during the postoperative periods.
Conclusion
The novel implant (hybrid implant) showed good stability and minimum patient discomfort during one year postoperative period evaluation. The implant system leads to new prospect in the field of prosthetic rehabilitation.
Keywords: Hybrid, Implant, Ossteointergration, Rigid fixation
Introduction
Replacement of missing tooth has evolved from removable dentures to fixed dentures and recently to dental implants. Dental implants are conventionally intended to, substitute missing teeth in maxilla and mandible. In the field of prosthodontics the ultimate objective is to provide one or more artificial teeth which are firmly mounted within the mouth which will remain firm under the normal oral activities of the patient and which will appear natural to the sight.
Dental implants eliminate the need of trimming the adjacent teeth needed for placement of fixed partial denture. The need of sufficient bone around the endosseous implant is critical for the success of the implant. In the maxillary sinus region the reduction of the bone height due to postextraction pneumatisation and resorption poses a challenge for implant placement. In the mandibular region if the height of bone is compromised, the placement of endosseous implant may lead to injury to the neurovascular bundle. Keeping in mind the above said difficulties we initiated a search for an implant system which will be cost effective and easy to use with adequate strength to support prosthesis. The present study was aimed to evaluate the efficacy of a novel implant (HYBRID IMPLANT-submitted for patency) for replacement of the missing teeth.
Aim of the study
To evaluate efficacy of hybrid implant for replacement of missing teeth.
Materials and Methods
Research Design
A prospective research design with a follow up after 1st, 2nd, 3rd week, 1st, 3rd, 6th month and 1st year postoperatively.
Sampling Method
Population: All patients who reported to the outpatient department of Mar Baselios Dental College, Kothmangalam for replacement of missing teeth according to the inclusion and exclusion criteria. Institutional ethical committee permission was obtained for conducting the study.
Inclusion criteria
All patients above the age group of 16 years
Patients who need replacement of single or multiple teeth in the anterior or posterior region of the maxilla and mandible.
Exclusion criteria
Medically compromised patients.
Patients having craniofacial syndromes.
Sample Size
Five patients were selected taking into consideration the inclusion and exclusion criteria (Table 1).
Table 1.
Sample size
| Site | Anterior (implant size) | Posterior (implant size) |
|---|---|---|
| Maxilla | 2 (Abutment: 2.5 mm diameter. Plate 0.5 mm thick and 35 mm length) | 2 (Abutment: 3.5 mm diameter. Plate 0.5 mm thick and 35 mm length) |
| Mandible | 5 (Abutment: 3.5 mm diameter. Plate 0.5 mm thick and 35 mm length) |
Implant Design
The implant consists of a long malleable plate having a length of 30–45 mm, thickness of 0.4–1 mm and breadth of 3–5 mm with screw holes and a stump called abutment, projecting from the flat surface of the plate (Fig. 1a, b).The prosthetic tooth can be fixed to the abutment. The implant is a prefabricated malleable thin elongated laminar plate having a vestibular anchoring part with at least three screw holes and a lingual or palate anchoring part with at least two screw holes for fixing at the most appropriate area of the jaw bone by means of screws. Out of the three screw holes in vestibular region minimum of two holes are used for anchoring and one screw hole on palatal and/or lingual side. Two arms on either side of the abutment are of variable length. However number of holes on the plate and the diameter and length of the abutment are also variable and is in the range of 1.5–7 mm diameter with 4–8 mm length. The length of abutment can be cut to size as required. These variations are decided according to the site of placement of the implant on the jaw. The elongated laminar plate, abutment and screws are made of titanium (Ti6Al4V).
Fig. 1.

Hybrid implant
The screws are of variable length and size ranging from 4 to 12 mm length and 1.5 to 2.5 mm diameter, which are meant to screw the plate to the alveolar bone. The screws on the vestibular and lingual/palatal plate are positioned in such a way that the screw ends do not meet each other.
Procedure of Implant Placement
Step 1: The alveolar bone of the maxilla or mandible was exposed by elevating a mucoperiosteal flap under local anesthesia. The implant is moulded to the contour of the alveolus in such a way that the abutment is projecting into the oral cavity in the direction of the tooth to be replaced.
Step 2: The implant is fixed to the alveolar bone using screws. The surgical part is completed by closing the mucoperiosteal flap to its normal position and covering the plate and screws of the implant. The abutment will be the only exposed part of the implant projecting into the oral cavity in the direction of missing tooth that has to be replaced (Figs. 2, 3).
Fig. 2.

Preoperative view of maxilla
Fig. 3.

Preoperative view of mandible
Evaluation
Pain: All patients were evaluated using Visual Analogue Scale having 0–10 markings on the 1st, 2nd, 3rd week, 1st, 3rd, 6th month and 1st year postoperatively.
Mobility: All patients were evaluated clinically for mobility of the implant during the 1st, 2nd, 3rd week, 1st, 3rd, 6th month and 1st year postoperatively (Table 2).
Bone Loss: All patients were evaluated radiographically using IOPA and OPG to assess the marginal bone loss around the screws of the implant at the end of 1st, 6th month and 1st year postoperatively.
Table 2.
Mobility criteria
| Criteria | Score (mm) |
|---|---|
| No mobility | 0–0.5 |
| Mild mobility | 0.5–2 |
| Moderate mobility | 2–3 |
| Severe mobility | >3 |
Results
Pain
All the patients experienced pain during the 1st postoperative period that gradually decreased in intensity. All the patients were non symptomatic during the 1st month to 1st year postoperative periods (Fig. 4).
Fig. 4.
Pain
Mobility
All the patients were assessed clinically for mobility. We experienced mobility during the 1st and 2nd postoperative periods in the 2nd and 3rd patients where the implants were inserted in the mandibular molar region (Fig. 5).
Fig. 5.
Mobility
Bone Loss
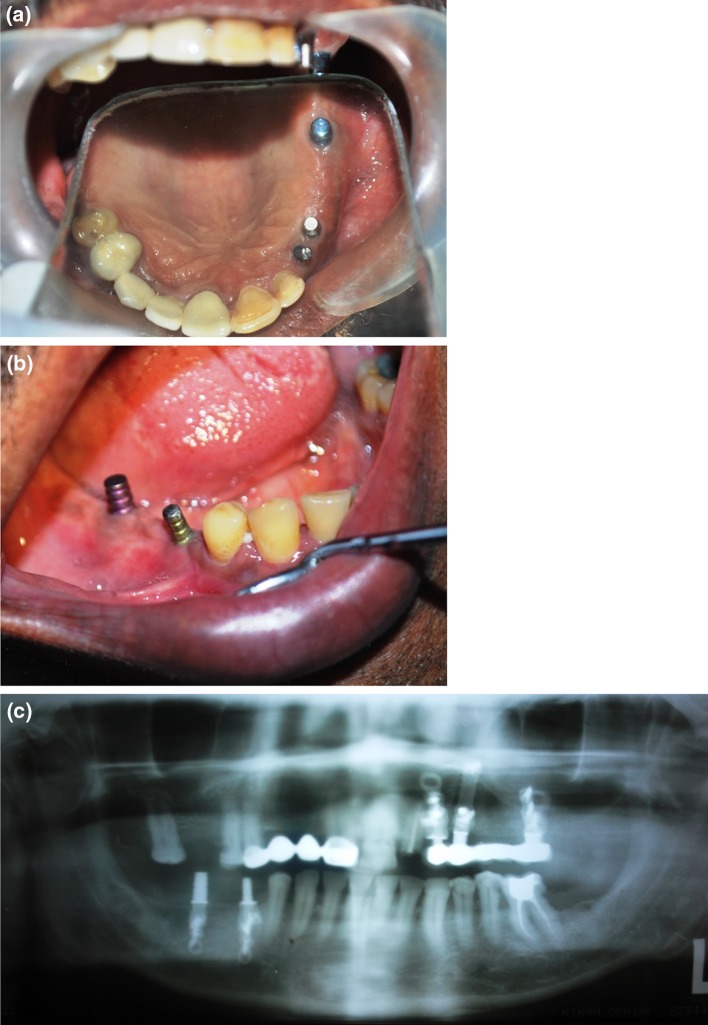
All the patients were assessed radiographically for bone loss. We had not experienced any bone loss during the postoperative periods (Fig. 6).
Fig. 6.
Bone loss
Discussion
The concept of osseointegration proposed by Branemark et al. [1, 2] and the replacement of lost teeth by implants have revolutionized oral rehabilitation with a significant advancement in restorative dentistry. In prosthodontics, dental implants have gained significant importance in tooth replacement [3, 4]. High implant success rate of 78–100 % have been published with more than 15 years of observation time [5–7]. Despite these success rates, certain limitations are often encountered in implanted sites. The major drawbacks of the endosseous implant are (1) the width of the bone in the bucco-lingual direction is crucial as more than 1 mm of bone should be around the endosteal implant [8]. (2) The length of the root form implant is often 8 mm upwards. If the length is decreased due to inadequate bone height, the diameter of the implant has to be increased to achieve adequate bone implant interface. (3)There is a risk of involvement of neurovascular bundle in mandible if the height of the crestal bone is not adequate. A minimum distance of 2 mm has to be maintained to avoid nerve injury [9] (4) In the sinus area of the maxilla, the vertical thickness of the bone is often less than 5 mm [10]. In such a situation ‘sinus lift bone grafting, is required, which is a major technique sensitive surgical procedure. More than 6 months are required for the take up of the graft. Moreover, the bone formation is unpredictable. (5) The angulation of the abutment is crucial in the implant placement. Control of the angulation of the abutment sometimes becomes difficult in certain situations. (6) Higher cost of the armamentarium eventually leads to increased treatment charges. (7) Highly technique sensitive procedures lead to need for special training.
Keeping in mind the above problems we developed an implant system that can easily overcome the difficulties and is economical, technically less sensitive requiring minimum armamentarium for implant placement. We selected patients according to the inclusion and exclusion criteria. We involved 5 patients as part of the study that was aimed to evaluate the efficacy of the new implant system over a period of 1 year. A total of 9 implants were placed into the maxillary and mandibular posterior and maxillary anterior region involving 5 patients (Table 1). Patients were evaluated clinically and radiographically during the 1st, 2nd, 3rd week, 1st, 3rd, 6th month and 1st year postoperative periods (Figs. 7, 8, 9). We experienced mobility and screw exposure in the lingual region during the first three postoperative periods, in two patients who had undergone implant placement in the mandibular posterior region. Mobility decreased as we had replaced the screws in the lingual aspect on the alternate screw hole. The visual analogue scale showed gradually decreasing pain in the postoperative periods. Radiographic and Cone Beam Computer Tomographic (Fig. 10) evaluation revealed no significant bone loss around the anchoring screws and at the alveolar ridge. All patients were given prosthetic crown after a period of 3 months, no temporary crowns were given. During the 1st postoperative period, patients were given routine antibiotics (Amoxicillin with Clauvalanic acid) and analgesics (Acelofenac and Paracetamol).
Fig. 7.
a, b Preoperative occlusion, c preoperative view
Fig. 8.
a 3rd week postoperative maxilla, b 3rd week postoperative mandible, c 1 month postoperative maxilla
Fig. 9.
1 year postoperative view
Fig. 10.

a Cone beam computer tomography—Maxilla. b Cone beam computer tomography—Mandible
The distinguishing features of the implant system are:
The implant is a plate which is malleable, with an abutment projecting from its central area. The plate has got screw holes on the two arms extending from the abutment. The arms can be of variable length, width and thickness.
The abutment is projecting from the central part of the plate. The height, width, taper and slots on the abutment are variable according to the requirement.
The implant design overcomes the height and width problem of alveolar bone, as it hugs the bone and is fixed to the cortical bone using screws.
The implant system overcomes the risk of nerve damage as it is placed subperiostealy and fixed by screw of variable lengths to the bone. As the screw holes are multiple one can select the screw hole which is not in proximity to the nerve.
In the sinus area of the maxilla the thickness of the bone between the sinus and oral cavity at the alveolar crest is often less to support the endosteal implant. This is overcome by the proposed implant as it is subperiosteal and hugging the bone and is fixed to the cortical bone. This avoids sinus lift bone grafting which is a very technique sensitive major surgical procedure.
Moreover 6 months are required for the take up of the bone graft which is unpredictable. Only after the take up and ensuring the thickness of bone the endosteal implant can be placed. The dental implants have taken a long and innovative path of evolution from subperiosteal, blade vent, bicortical, cylindrical, tapered with multiple designs for the abutment. Hybrid implant is designed to overcome the limitation of the root form implants taking the advantage of malleability of titanium alloys and the properties of endosteal screws and subperiosteal plate. We hope that this will be another step towards the progress of the dental implant system.
Conclusion
The novel implant (hybrid implant) showed good stability and minimum patient discomfort during 1 year postoperative period evaluation. The implant system leads to new prospects in the field of prosthetic rehabilitation. Longer period of follow up and more number of cases and a multicentre study is required for a more confirmative efficacy about the hybrid implant system.
References
- 1.Branemark PI, Adell R, Breine U, et al. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3(2):81–100. doi: 10.3109/02844316909036699. [DOI] [PubMed] [Google Scholar]
- 2.Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387–416. doi: 10.1016/S0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 3.Branemark PI, Hansson BO, Adell R, et al. (1977) Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plastic Reconstr Surg 16:1–132 [PubMed]
- 4.Albrektsson T, Zarb G, Worthington P, Erikson RA. The long term efficacy of currently used dental implants. A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 5.Albrektsson T, Dahl E, Enbom L, et al. Osseointegrated oral implants. A Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol. 1988;59:287–296. doi: 10.1902/jop.1988.59.5.287. [DOI] [PubMed] [Google Scholar]
- 6.Engquist B, Bergendal T, Kallus T, Linden U. A retrospective multicenter evaluation of osseointegrated implants supporting overdentures. Intern J Oral Maxillofac Implants. 1998;3:129–134. [PubMed] [Google Scholar]
- 7.Jemt T, Lekholm U, Adell R. Osseointegrated implants in the treatment of partially edentulous patients: a preliminary study on 876 consecutively placed fixtures. Int J Oral Maxillofac Implants. 1989;4:211–217. [PubMed] [Google Scholar]
- 8.Belser UC, Bernard JP, Buser D. Implant-supported restorations in the anterior region: prosthetic considerations. Pract Periodontics Aesthet Dent. 1996;8:875–883. [PubMed] [Google Scholar]
- 9.Shenoy VK (2012) Single tooth implants: Pretreatment considerations and pretreatment evaluation. J Interdiscip Dent 2(3):149–157
- 10.Nimigean V, Nimigean VR, Maru N, Salavastru DI, Badita D, Tuculina MJ. The maxillary sinus floor in the oral implantology. Rom J Morphol Embryol. 2008;49(4):485–489. [PubMed] [Google Scholar]