Abstract
Rehabilitation of patients with ectodermal dysplasia often presents clinical challenge due to hypodontia, anodontia, and severe atrophy of edentulous ridges. Zygomatic implant therapy can be used as a method of achieving osseointegration without bone grafting in such situations. This clinical report describes the dental rehabilitation of atrophic maxilla of a 26-year old female patient with a fixed prosthesis, immediately loaded on four zygomatic implants.
Keywords: Quadruple zygomatic implants, Atrophic maxilla, Ectodermal dysplasia, Immediate loading, Fixed prosthesis
Introduction
Ectodermal dysplasia (ED) is a syndromic disorder characterized by more than 170 clinical signs involving at least two structures derived from the embryonic ectoderm [1]. Individuals affected by ED may have combination of symptoms including sparse hair, brittle nails, dental malformations, skin problems, absence of sweat glands, complications of swallowing, vision and hearing [2]. Hypodontia and anodontia associated with ED and the resultant lack of alveolar bone formation often creates restorative difficulties due to inadequate bone volume, increased interridge clearance, and abnormal jaw relationship [3].
Oral rehabilitation of patients with ED not only restores the function but also aids in facial esthetics, speech and emotional development [4–6]. Treatment options for edentulous patients with ED include tissue-supported removable prosthesis, implant-supported removable prosthesis, and implant supported fixed prosthesis [4]. Despite the anatomical abnormalities of bone structure, implant supported restorations have high success rate similar to normal individuals [7]. The presence of inadequate bone quantity poses a potential problem for implant placement necessitating various bone augmentation procedures [8, 9]. Implant placement in grafted bone has shown success as good as implants placed in native bone [10]. However, bone grafting procedures have few limitations like need for hospitalization, morbidity of donor site, unpredictable resorption of the bone graft, and delayed placement of implant for the graft consolidation time [11–13].
Treatment concepts with zygomatic implants have evolved as an alternative for bone augmentation procedures. Combination of conventional implants and zygomatic implants has been used successfully for restoration of atrophic maxilla [14, 15]. Oral rehabilitation of a patient with ED with zygomatic implants has also been reported in the literature [16]. Placement of anterior conventional implants without grafting will be extremely difficult in severely atrophic pre-maxilla. In such situations, quadruple zygomatic implants can be used for the restoration of edentulous maxilla [17]. This clinical report describes the restoration of maxillary dentition of a patient with ED by using four zygomatic implants.
Case Report
A 26 year old female patient diagnosed with ED was referred to our private dental practice. Patient had complaints of poor esthetics and masticatory inefficiency with the existing removable prosthesis. Dental history revealed the usage of a removable prosthesis for the past 13 years. Oral and radiographic examination showed extensive bone loss around the supporting abutment teeth (Figs. 1, 2, 3). Both the maxillary and mandibular ridges were severely atrophic. The height of the remaining alveolus was approximately 2 mm sub-antrally and the inferior alveolar canal was close to the crest of the ridge. Patient expressed desire for a fixed dental prosthesis.
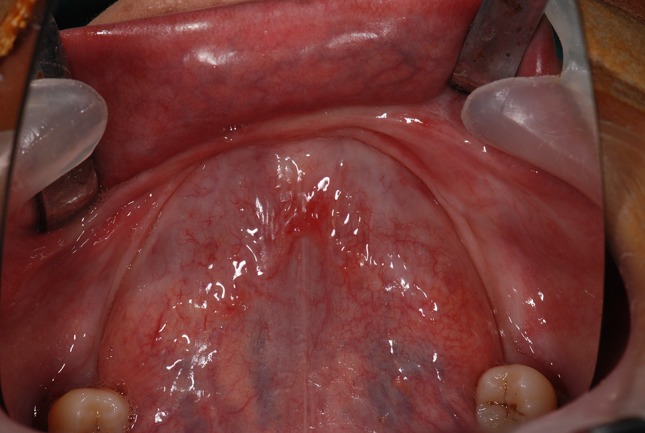
Fig. 1.

Occlusal view of edentulous maxillary ridge
Fig. 2.
Occlusal view of edentulous mandibular ridge
Fig. 3.
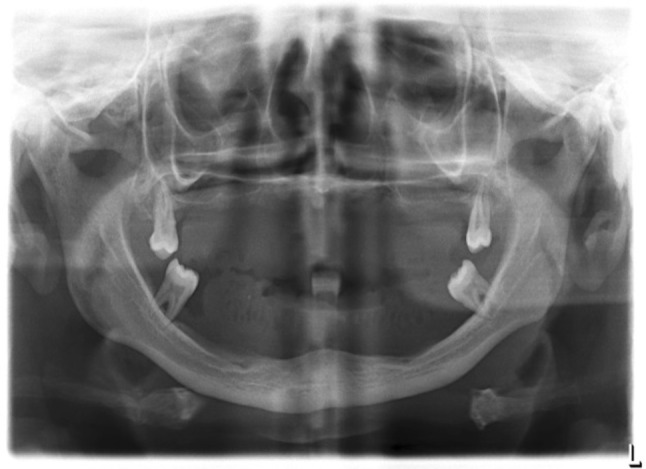
Preoperative panoramic view
A diagnostic complete denture was fabricated to assess the esthetics, lip support, interridge clearance, and the relationship of the artificial teeth to the underlying alveolus. Radiographic markers were embedded in the diagnostic denture and cone beam computerized tomographic (CBCT) scan was performed. CBCT images showed knife edged pre-maxilla and bone height of about 2 mm subantrally (Figs. 4, 5). The mandibular ridge had adequate width but was deficient in height in the interforaminal region. Treatment options of onlay grafting followed by conventional implant placement, and zygomatic implant supported prosthesis were discussed with the patient. Patient opted for zygomatic implant supported prosthesis considering the advantages of immediate loading, elimination of morbidity, and consolidation time related to bone grafting procedures.
Fig. 4.
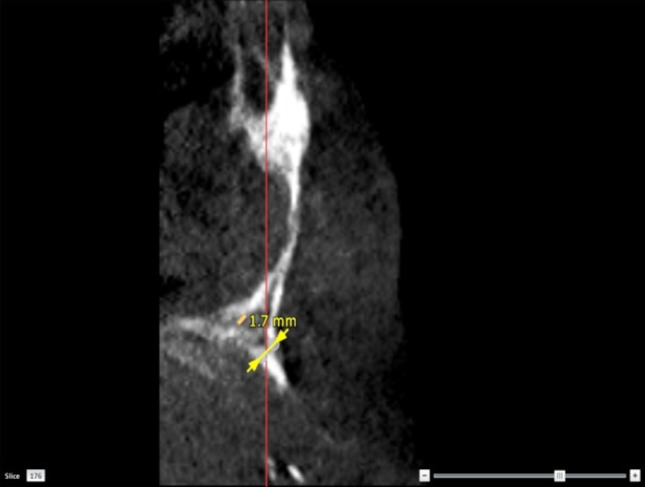
CBCT image of the atrophic maxillary canine region
Fig. 5.
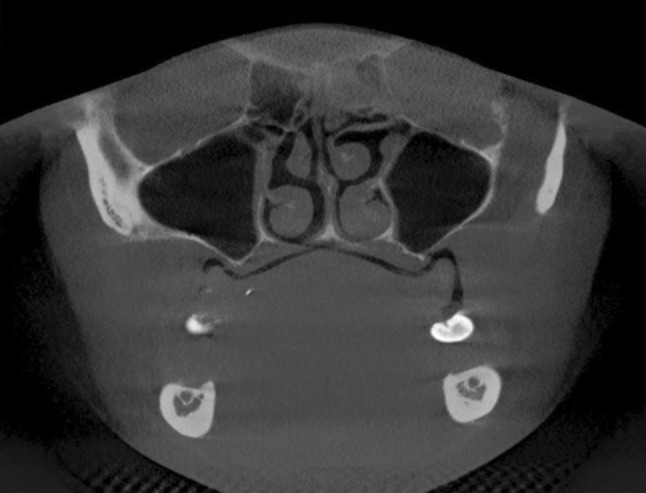
CBCT image of the sub-antral region
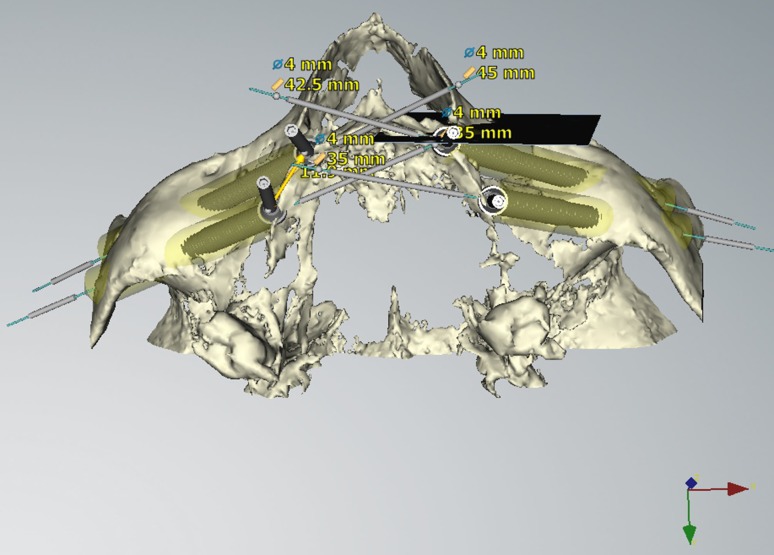
The CBCT that was made using the diagnostic denture with markers was used for treatment planning. Two zygomatic implants on either side of the maxillary arch were planned using virtual planning software (Nobel clinician, Nobel Biocare AB, Goteborg, Sweden) (Fig. 6). Virtual planning was utilized to maintain 3 mm of inter-implant distance, 3 mm between anterior zygomatic implant and infra orbital nerve, and maximum cortical anchorage within the zygomatic bone. Four conventional implants were planned for the mandibular arch, with the distal implants bypassing the mandibular nerve. Surgical template was fabricated to identify the prosthetically determined osteotomy sites during the surgical procedure.
Fig. 6.
Virtual planning for zygomatic implants
Under nasotracheal intubation, general anaesthesia was administered and 2 % lignocaine with adrenaline was infiltrated into the right and left buccal vestibule. Crestal, anterior, and posterior vestibular releasing incisions were made, and mucoperiosteal flap was elevated to expose the alveolar crest, the lateral wall of the maxillary sinus, infra orbital nerve and the inferior rim of the zygomatic arch. A small window was made on the lateral wall of the sinus to assist visualization of drills during osteotomy preparation. The surgical guide was positioned to identify the prosthetically determined osteotomy positions. Sequential osteotomy was done with 2.9 mm round bur, 2.9 mm cylindrical bur and 3.5 mm pilot drill. The anterior implants (Branemark System Zygoma TiUnite Implants; Nobel Biocare AB) were placed first engaging the zygomatic bone with their platforms emerging at the canine region. The posterior zygomatic implants (Branemark System Zygoma TiUnite Implants; Nobel Biocare AB) were then placed through the infra-zygomatic crest emerging near the second premolar and first molar region. The flaps were approximated and sutured using resorbable 3-0 vicryl.
Angulated multi-unit abutments (Branemark System Zygoma Multiunit abutments RP; Nobel Biocare AB) were connected to all the implants to orient their prosthetic screw axis in the same path of insertion (Fig. 7). Abutment level impression was made after splinting the open tray impression copings with auto-polymerizing acrylic resin (GC Pattern resin, GC Asia). Healing caps were connected to the abutments (Fig. 8). Facebow transfer and inter-occlusal records were made. Screw retained metal reinforced acrylic provisional prosthesis was fabricated and connected to the implants within 48 h after surgery. Patient was given instructions regarding oral hygiene measures and was followed up at regular intervals of 15 days, 1 month, 3 months, and 6 months. Exposure of few implant threads in the anterior two zygomatic implants was observed (Fig. 9). The provisional prosthesis was replaced with a definitive prosthesis after 6 months (Figs. 10, 11, 12). Patient was followed up for 3 years without any further complications.
Fig. 7.
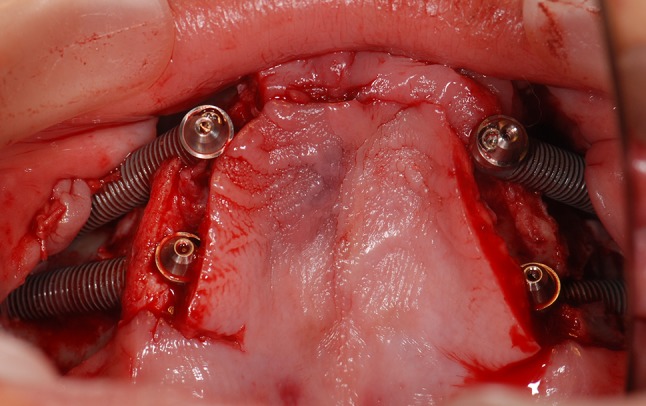
Multi-unit abutments connected with implants
Fig. 8.
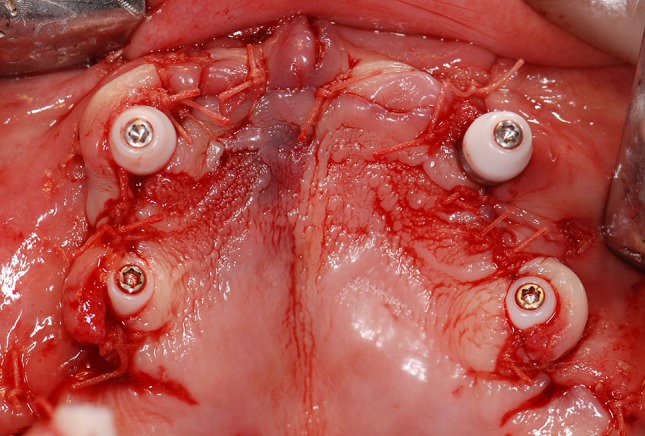
Healing caps on multi-unit abutments
Fig. 9.
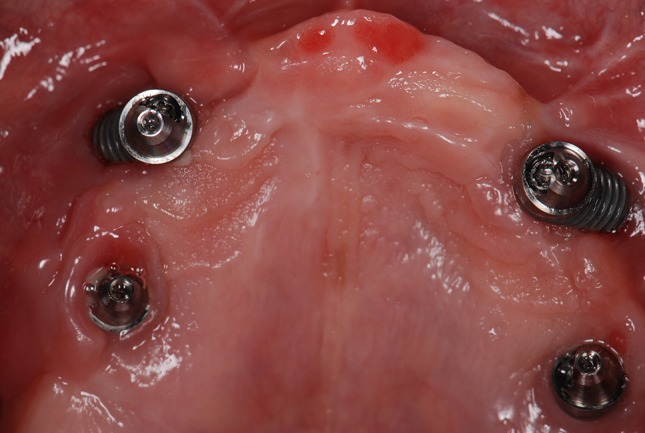
Thread exposure during recall visit
Fig. 10.

Occlusal view of definitive prosthesis
Fig. 11.

Frontal view of definitive prosthesis
Fig. 12.

Panoramic view with definitive prosthesis
Discussion
Zygomatic implants in ED patients have been reported to be clinically successful. The use of quadruple zygomatic implants in ED patient is lacking in literature. Micro structural analysis of female ED bone has been shown to be more compact and with greater trabecular patterns than males [18]. Considering the high success rate of dental implants in ED patients [7], and the need for immediate fixed prosthesis without grafting procedures, the use of four zygomatic implants for a maxillary fixed prosthesis can be a valuable treatment option.
The anatomical configuration of the maxilla and zygoma facilitated an extra sinus approach for placement of the zygomatic implants [19]. Considering the high primary stability of more than 45 N cm for the zygomatic implants, immediate restoration with a provisional prosthesis was done. This also prevented the micro movement of the implants due to the splinting provided by the prosthesis. The severe deficiency of the maxillary alveolus facilitated a gradual emergence of the prosthesis from the abutment platform providing the desired facial esthetics and lip support without causing lip entrapment.
Recession of soft tissue on the buccal aspect of the anterior zygomatic implants was observed during the follow-up period. Labial positioning of the anterior implants as determined by the prosthetically guided planning and the lack of keratinized mucosa around the implants could have resulted in recession [20]. Plaque accumulation in the exposed threads can be a challenge for hygiene maintenance. Bacterial ingress along the implant surface could cause maxillary sinusitis [21]. Soft tissue grafting can be done to address this recession. The use of the zygomatic implants with the smooth surface near the crest can facilitate good hygiene maintenance even after recession [22]. It can be concluded that oral rehabilitation with zygomatic implants, for patients with developmental disorders like ED, can be considered as a viable treatment option.
References
- 1.Pinheiro M, Freire-Maia N. Ectodermal dysplasias: a clinical classification and a causal review. Am J Med Genet. 1994;53:153–162. doi: 10.1002/ajmg.1320530207. [DOI] [PubMed] [Google Scholar]
- 2.Kargul B, Alcan T, Kabalay U, Atasu M. Hypohidritic ectodermal dysplasia: dental, clinical, genetic and dermatoglyphic findings of three cases. J Clin Pediatr Dent. 2001;26:5–12. doi: 10.17796/jcpd.26.1.g156r02u66w30729. [DOI] [PubMed] [Google Scholar]
- 3.Durstberder G, Celar A, Watzek G. Implant-surgical and prosthetic rehabilitation of patients with multiple dental aplasia: a clinical report. Int J Oral Maxillofac Implant. 1999;14:417–423. [PubMed] [Google Scholar]
- 4.Hickey AJ, Vergo TJ. Prosthetic treatments for patients with ectodermal dysplasia. J Prosthet Dent. 2001;86:364–368. doi: 10.1067/mpr.2001.118876. [DOI] [PubMed] [Google Scholar]
- 5.Pigno MA, Blackman RB, Cronin RJ, Cavazos E. Prosthodontic management of ectodermal dysplasia: a review of the literature. J Prosthet Dent. 1996;76:541–545. doi: 10.1016/S0022-3913(96)90015-3. [DOI] [PubMed] [Google Scholar]
- 6.Allison PJ, Locker D, Feine JS. Quality of life: a dynamic construct. Soc Sci Med. 1997;45:221–230. doi: 10.1016/S0277-9536(96)00339-5. [DOI] [PubMed] [Google Scholar]
- 7.Yap AK, Klineberg I. Dental implants in patients with ectodermal dysplasia and tooth agenesis: a critical review of the literature. Int J Prosthodont. 2009;22:268–276. [PubMed] [Google Scholar]
- 8.Guckes AD, Scurria MS, King TS, McCarthy GR, Brahim JS. Prospective clinical trial of dental implants in persons with ectodermal dysplasia. J Prosthet Dent. 2002;88:21–25. doi: 10.1067/mpr.2002.127099. [DOI] [PubMed] [Google Scholar]
- 9.Guckes AD, Brahim JS, McCarthy GR, Rudy SF, Cooper LF. Using endosseous dental implants for patients with ectodermal dysplasia. J Am Dent Assoc. 1991;122:59–62. doi: 10.14219/jada.archive.1991.0307. [DOI] [PubMed] [Google Scholar]
- 10.Grecchi F, Zingari F, Bianco R, Zollino I, Casadio C, Carinci F. Implant rehabilitation in grafted and native bone in patients affected by ectodermal dysplasia: evaluation of 78 implants inserted in 8 patients. Implant Dent. 2010;19:400–408. doi: 10.1097/ID.0b013e3181e40609. [DOI] [PubMed] [Google Scholar]
- 11.Seiler JG, 3rd, Johnson J. Iliac crest autogenous bone grafting: donor site complications. J South Orthop Assoc. 2000;9:91–97. [PubMed] [Google Scholar]
- 12.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res. 1996;329:300–309. doi: 10.1097/00003086-199608000-00037. [DOI] [PubMed] [Google Scholar]
- 13.Rasmusson L, Meredith N, Cho IH, Sennerby L. The influence of simultaneous versus delayed placement on the stability of titanium implants in onlay bone grafts. A histologic and biomechanic study in the rabbit. Int J Oral Maxillofac Surg. 1999;28:224–231. doi: 10.1016/S0901-5027(99)80143-X. [DOI] [PubMed] [Google Scholar]
- 14.Malevez C, Abarca M, Durdu F, Daelemans P. Clinical outcome of 103 consecutive zygomatic implants: a 6–48 months follow-up study. Clin Oral Implant Res. 2004;15:18–22. doi: 10.1046/j.1600-0501.2003.00985.x. [DOI] [PubMed] [Google Scholar]
- 15.Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implant. 2010;25:1213–1221. [PubMed] [Google Scholar]
- 16.Balshi TJ, Wolfinger GJ. Treatment of congenital ectodermal dysplasia with zygomatic implants: a case report. Int J Oral Maxillofac Implant. 2002;17:277–281. [PubMed] [Google Scholar]
- 17.Davo R, Pons O, Rojas J, Carpio E. Immediate function of four zygomatic implants: a 1-year report of a prospective study. Eur J Oral Implant. 2010;3:323–334. [PubMed] [Google Scholar]
- 18.Silthampitag P, Klineberg I, Austin B, Jones AS. Bone micro architecture at oral implant sites in ectodermal dysplasia (ED): a comparison between males and females. Clin Oral Implant Res. 2011 doi: 10.1111/j.1600-0501.2011.02303.x. [DOI] [PubMed] [Google Scholar]
- 19.Aparicio C (2011) A proposed classification for zygomatic implant patient based on zygoma anatomy guided approach (ZAGA): a cross-sectional survey. Eur J Oral Implant 4:269–275 [PubMed]
- 20.Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Five year evaluation of the influence of keratinized mucosa on peri-implant soft- tissue health and stability around implants supporting full arch mandibular prosthesis. Clin Oral Implant Res. 2009;20:1170–1177. doi: 10.1111/j.1600-0501.2009.01795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stie´venart M, Malevez C. Rehabilitation of totally atrophied maxilla by means of four zygomatic implants and fixed prosthesis: a 6–40-month follow-up. Int J Oral Maxillofac Surg. 2010;39:358–363. doi: 10.1016/j.ijom.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 22.Maló P, Nobre M, Lopes I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: a pilot study. J Prosthet Dent. 2008;100:354–366. doi: 10.1016/S0022-3913(08)60237-1. [DOI] [PubMed] [Google Scholar]