Abstract
One of the most commonly asked question by a patient who comes for extraction especially in the rural areas is whether the procedure will cause problems to the eye!! In reality however, ophthalmic complications following routine maxillary molar extractions are practically unheard of. When they occur they can be extremely unnerving not just to the patient but also to the surgeon. Patients generally panic which makes it tougher for the clinician to assess the situation. We present a case of a 26 year old female patient developing ophthalmic complication following local anesthesia administration during extraction of upper left maxillary third molar. In this article, ophthalmic complications arising from posterior superior alveolar nerve block are discussed and management guidelines are highlighted.
Keywords: Ophthalmic, Diplopia, Nerve block, Extraction
Introduction
Ophthalmic complications following routine maxillary molar extractions are practically unheard of. Ocular complication following a nerve block is very rare and can perplex even the most experienced clinician at times. These complications are often related to the technique rather than the anesthetic material itself. A few documented cases of ophthalmic complications point at a few ways in which these occur following administration of posterior superior alveolar nerve block for a maxillary molar extraction. This report details the complication of transient diplopia following local anesthetic delivery using the posterior superior alveolar nerve block technique.
Case Report
A twenty-six year old female outpatient came to our unit with pain in her maxillary left third molar, secondary to irreversible pulpitis. A detailed case history was recorded. Following clinical and radiographic examination, it was decided to extract the offending tooth.
After obtaining written & verbal consent for extraction of tooth, the patient was placed in recumbent position & 1.5 ml of 2 % lidocaine with 1: 80,000 adrenaline was administered using a twenty-six gauge Unilok® needle, for posterior superior alveolar nerve block followed by greater palatine nerve block with 0.3 ml solution of same after ensuring negative aspiration.
After appropriate anesthesia was achieved the tooth was elevated and delivered using standard flapless forceps technique. Following the procedure, patient’s chair was slowly returned to an upright position. The entire procedure lasted around 10 min.
Soon afterwards she complained of double vision. She appeared extremely apprehensive, anxious and started crying. The absence of tears from only the left eye was noted (Fig. 1). Patient’s vital signs were recorded which turned out to be normal. Ocular examination revealed pupils which were equally round and reactive to light. The patient was unable to abduct her left eye past midline however, ocular movements in all other directions were normal.
Fig. 1.

Patient’s photograph immediately and two hours after procedure. (Color figure online)
Diagnosis of transient diplopia was made based on the events leading to the clinical symptoms (administration of local anesthesia to anaesthetize the posterior superior alveolar nerve followed by extraction of the tooth). The patient was assured of the temporary nature of this condition. Her left eyelid was taped in closed position to reduce the effect of diplopia. She was driven home by her escort. When contacted later that evening, the patient reported that her vision had returned to normal. She was referred to an ophthalmologist the next day. He confirmed our diagnosis and deemed that no further treatment was necessary.
Discussion
Every year millions of local anesthetic injections are safely delivered by dental practitioners with minimal complications and good success rates. Visual disturbances are uncommon following the administration of local anesthesia and are rarely documented because of their transient nature.
Documented but rare ophthalmic complications include temporary blindness, diplopia, and temporary paralysis of cranial nerve III, IV and VI, mydriasis, palpebralptosis [1]. Rishiraj et al. [2] have documented a case of permanent vision loss in one eye following administration of local anesthesia for dental extraction. Our patient experienced transient diplopia along with temporary loss of lacrimal secretions after administration of posterior superior alveolar nerve block for extraction of maxillary left third molar.
Ophthalmic complications following a posterior superior alveolar nerve block can be due to vascular causes or diffusion through bony channels.
Panarrocha et al. [3] proposed a theory that ophthalmic disorders are caused by direct diffusion of the anesthetic solution from pterygomaxillary (Fig. 2) fossa through the sphenomaxillary cavity to the orbit which could affect the ciliary ganglion located between optic nerve and external rectus muscle of eye. Lignocaine action around ciliary ganglion may explain the different manifestations in terms of either sympathetic or parasympathetic involvement.
Fig. 2.
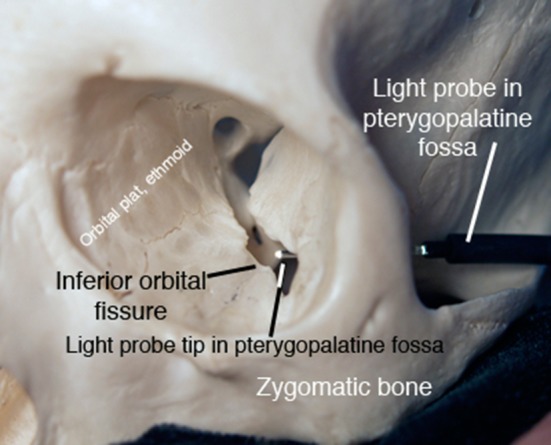
Line of communication between pterygomaxillary fissure and the orbital apex. (Color figure online)
Chun-kei lee [4] hypothesized that intra-arterial injection of the local anesthesia can reach the cavernous sinus through arteries and cause paralysis of third, fourth and sixth cranial nerves. Goldenberg [5] in his study further expanded that a local anesthetic could pass through the cavernous sinus towards the ophthalmic vein, ultimately reaching the ophthalmic artery by way of a series of anastomoses (Fig. 3). The three cranial nerves (III, IV, and VI) are closely related to the cavernous sinus and the solution could have a direct anaesthetic effect on these nerves.
Fig. 3.
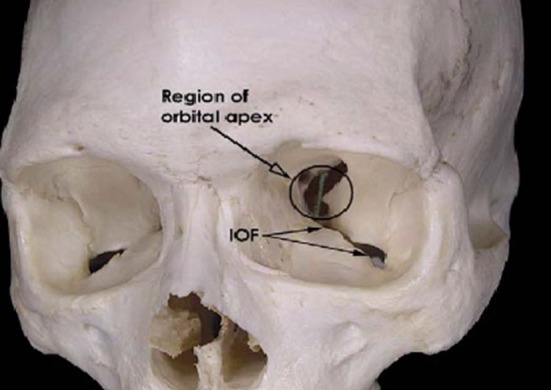
Communication between pterygopalatine fossa and infraorbital fissure. (Color figure online)
Crean et al. [6] observed peripheral fifth and sixth cranial nerve palsy in their patient who complained of double vision. They hypothesised that deposition of anesthetic solution within the PSA artery causes a back flow into the connecting maxillary artery and subsequently into middle meningeal artery. There exist several anastomoses between orbital branch of the middle meningeal artery and recurrent meningeal division of the lacrimal artery. Lacrimal artery supplies the lateral rectus muscle, lacrimal gland and outer half of eyelids. These anatomical considerations can explain all documented ophthalmic complications following administration of local anesthesia through the posterior superior alveolar nerve block technique.
In our case, inadvertent intra-arterial injection of local anesthetic seems to be less probable because, adequate aspiration was done prior to injecting and all the safe injection procedures were followed. However the abnormal lacrimation seems to indicate some intraarterial diffusion of the solution. The more probable cause could be venous diffusion leading to entry of the local anaesthetic solution into the ophthalmic vein leading to development of symptoms as suggested by Chun-kei lee [4] and Goldenberg [5]. The recumbent position of the patient during anaesthetic delivery may have also played a role [7]. This position could have aided in diffusion of the local anasethetic solution through the bony as well as the vascular channels.
Complete recovery was observed in nearly all reported cases within a few hours of the incident’s discovery, which is the approximate amount of time necessary for complete cessation of the anaesthetic’s physiologic effects [8] as noticed in this case too. The available literature on ophthalmic complications following a PSA nerve block does not point towards usefulness of medications including steroids which could help to alleviate the symptoms which are anyway most often transient in nature. Reported cases of ophthalmic complications following intra-oral nerve blocks in literature show that the duration of symptoms is limited and that they tend to resolve with no sequelae [3]. Patient reassurance and a good follow-up with an early ophthalmic consultation form the bed rock of the treatment protocol.
Conclusion
Complications can occur at any given time during a surgical procedure. Certain common complications can be predicted or expected. However certain unexpected and rarely documented complications during routine procedures may stump even experienced clinicians. The clinician especially oral and maxillofacial surgeons should be aware of all possible complications and their management. This is because only if they are aware will they be able to manage the situation and in turn, reassure the patient.
Predicting the possibility of the above mentioned complication is virtually impossible. Even the etiology can only be speculated with some degree of confidence based on sound knowledge of anatomical structures and pathways. Although the anatomical location of deposition of the local anesthetic solution is the most probable and accepted cause of transient diplopia, role of the chemical nature and concentration of the local anesthetic solution (in this case 2 % lignocaine with 1:80,000 adrenaline) also perhaps warrants an investigation. There are studies which hint at incidences of ophthalmic complications following usage of 2 % articane [8].
The following management guidelines can be utilized in cases with transient diplopia following local anesthesia administration through the posterior alveolar nerve block technique:
Recording a detailed case history with special emphasis on medical details and history of previous extractions and similar experiences.
Small gauge needle should be used and carefully aspiration should be done before injection. Proper concentration and volume of the LA solution should be injected slowly with least possible pressure. These measures help in reducing the incidence of not just this but many complications.
The patient should be reassured about the temporary nature of these complications.
The affected eye should be covered with moist gauze dressing to protect the cornea. The affected eye could also be taped to reduce the effect of double vision.
The patient should be immediately referred to an ophthalmologist. This will aid in early diagnosis of the nerves involved and also in the management.
The patient should be escorted by a responsible adult. If the patient has come alone, he/she should be asked to stay back in the dental office till the symptoms persist.
Declarations
The authors have received no grant for the completion of the study and declare that they have no conflict of interest to declare. In addition, a written consent was obtained from the patient. Appropriate permission was also obtained to use clinical photographs for the purpose of further academic research and publication in academic journals.
Contributor Information
Abhishek Ghosh, Email: abhishekghosh13@gmail.com.
N. Vaibhav, Phone: 9844258076, Email: vaibsarticles@gmail.com
Rohan Raut, Email: 30.rohan@gmail.com.
Anchita Venkatesh, Email: anchita.venkatesh@gmail.com.
References
- 1.Agarwal, Dolas, Managutti A. Temporary pupillary dilatation and ptosis: complications of PSA nerve block: a case report and review of literature. J Maxillofac Oral Surg. 2009;8(2):181–183. doi: 10.1007/s12663-009-0044-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rishiraj B, Epstein JB, Fine D, NAbi S, Wade NK. Permanent vision loss in one eye following administration of local anesthesia for a dental extraction. Int J Maxillofac Oral Surg. 2005;34(2):220–223. doi: 10.1016/j.ijom.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Panarrocha-Diago M, Sanchis-Bielsa JM. Ophthalmic complications after intraoral local anesthesia with articane. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:21–24. doi: 10.1067/moe.2000.107506. [DOI] [PubMed] [Google Scholar]
- 4.Chun-kei L. Ocular complications after inferior alveolar nerve block. Dent Bull. 2006;11:4–5. [Google Scholar]
- 5.Goldenberg AS. Transient diplopia from a posterior alveolar injection. J Endod. 1990;16:550–551. doi: 10.1016/S0099-2399(07)80220-2. [DOI] [PubMed] [Google Scholar]
- 6.Crean SJ, Powis A. Neurological complications of local anesthetics in dentistry. Dent Update. 1999;26:344–349. doi: 10.12968/denu.1999.26.8.344. [DOI] [PubMed] [Google Scholar]
- 7.Walker M, Drangsholt M, Czartoski TJ, Longstreth WT., Jr Dental diplopia with transient abducens palsy. Neurology. 2004;63:2449–2450. doi: 10.1212/01.WNL.0000147323.73848.BE. [DOI] [PubMed] [Google Scholar]
- 8.Magliocca KR, Kessel NC, Cortright GW. Transient diplopia following maxillary local anesthetic injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:730–733. doi: 10.1016/j.tripleo.2005.08.012. [DOI] [PubMed] [Google Scholar]


