Abstract
This article tested a contingency-oriented perspective to examine the dynamic relationships between in-the-moment borderline personality disorder (BPD) symptom events and in-the-moment triggers. An experience sampling study with 282 adults, including 77 participants with BPD, obtained reports of situational triggers and BPD symptom events five times daily for two weeks. Triggers included being rejected, betrayed, abandoned, offended, disappointed, having one’s self-concept threatened, being in a boring situation, and being alone. BPD was associated with increased situational triggers. Multilevel models revealed significant within-person associations between situational triggers and BPD symptoms for the average participant in the study, with significant individual variance in the strength and direction of trigger-symptom contingencies. Most trigger-symptom contingencies were stronger for individuals with higher borderline symptomatology, suggesting that triggers are meaningfully related to BPD. These findings highlight possible proximal mechanisms that maintain BPD and help explain the course of a disorder often described as chaotic and unpredictable.
Research aimed at understanding and disentangling the chaotic, burdensome course of borderline personality disorder (BPD) has rightly pursued the identification of underlying etiological mechanisms. By identifying etiological mechanisms, information is learned about how BPD develops and what maintains the disorder’s patterns. Predominantly, this line of research has focused on distal mechanisms, such as biological sensitivities and subjection to invalidating childhood experiences (e.g., Widom, Czaja, & Paris, 2009; Zanarini et al., 2002). While these studies have identified distal mechanisms associated with the development of BPD, they have not identified the proximal mechanisms underlying symptom occurrences. The goal of the current study was to examine proximal mechanisms associated with in-the-moment BPD symptoms, specifically contingencies of symptoms on situational triggers.
The Importance of Proximal Mechanisms in the Production of BPD Symptoms
Unlike distal mechanisms, proximal mechanisms largely drive the acute, short-term occurrences of BPD symptoms. Rather than increasing risk for the development of BPD symptoms in a lifetime, proximal mechanisms increase risk for the occurrence of BPD symptoms at a given moment. Proximal mechanisms may also have symptom-specific effects, such that different symptoms occur in response to different triggers.
When focusing on proximal mechanisms, each occurrence of a symptom is taken as a short-lasting event of personal significance. For example, a hollow sense of self occurring for a few hours is taken as a distinct event of significance to the individual feeling hollow. This approach recognizes that symptom expression of BPD is not constant; rather, there is variability in daily experiences – a person’s anger, emptiness, or impulsivity flares (sometimes violently) and then subsides within hours.
The proximal mechanisms that drive the moment-to-moment experiences of BPD symptoms can be conceptualized as trigger-symptom contingencies (Furr, Fleeson, Anderson, & Arnold, in preparation). According to this perspective, within-person variability in symptom experience might be mapped onto within-person variability in the presence of situational triggers. Thus, a person’s individual variability in daily BPD symptom occurrences, and by extension, differences between individuals’ symptom occurrences, can be accounted for by the particular triggers encountered in everyday life. Research on proximal mechanisms is intended not only to build upon empirical data on the life course of BPD, but also to uncover order in an apparently volatile disorder.
Indeed, we believe that nearly all theories of BPD and nearly all therapeutic approaches for BPD have a contingency approach at their core (Furr et al., in preparation). Proximal mechanisms are particularly important in therapy, and empirically-supported treatments increasingly focus on managing trigger-symptom contingencies. Some treatments focus on identifying and understanding the proximal processes that trigger psychological difficulties (Verheugt-Pleiter & Deben-Mager, 2006). Others teach skills for managing reactions to potential triggers (Linehan, 1993), and on interpretations and schemata (Young, Klosko, & Weishaar, 2003) for making sense of interpersonal triggers (Wenzel, Chapman, Newman, Beck, & Brown, 2006).
Because of the compelling nature of the contingency approach, there has been a recent surge of studies investigating contingencies. These studies use experience-sampling methods (ESM) and multi-level modeling (MLM) to assess the frequency and magnitude with which certain symptoms are associated with certain triggers. Studies have demonstrated contingencies between negative emotions and BPD symptom experiences (Law, Fleeson, Arnold, & Furr, in press), rage and devaluation on rejection (Berenson, Downey, Rafaeli, Coifman, & Paquin, 2011), affective and interpersonal experiences on risky/impulsive behaviors (Coifman, Berenson, Rafaeli, & Downey, 2012), psychotic and dissociative symptoms on stress (Glaser, Van Os, Thewissen, & Myin-Germeys, 2010; Stiglmayr et al., 2008), self-esteem on stressful events (Zeigler-Hill & Abraham, 2006), quarrelsomeness on others’ quarrelsomeness (Sadikaj, Moskowitz, Russell, Zuroff, & Paris, 2013), and drinking on affective instability (Jahng et al., 2011).
Such findings provide important insights into the proximal mechanisms associated with the moment-by-moment flare-ups of BPD symptoms; however, they highlight only a few specific combinations of triggers and symptoms (e.g., rage and rejection, drinking and affective instability). A more comprehensive approach would integrate a wide range of theoretically-relevant triggers, and it would reflect the full scope of BPD symptoms.
In the current study, we take a comprehensive approach to discovering contingencies. We assess momentary occurrences of a wide variety of theoretically-identified triggers and all nine symptoms of BPD. We use wording as close as possible to the DSM-IV-TR and DSM-5 Section II wording of symptoms (American Psychiatric Association, 2000, 2013). By sticking closely to the DSM-IV-TR and DSM-5 wording of the symptoms, we are able to test whether occurrences of the defining symptoms of BPD are contingent. That is, we test whether BPD symptom occurrences are reactions associated with the presence of proximal triggers, and disappear when the triggers disappear (see Law et al., in press). By using a wide variety of theoretical triggers derived from a literature search, we are able to investigate which triggers are associated with which symptoms.
Which Situational Triggers to Study?
Theoretical accounts and empirical studies of BPD have produced a rich literature of potential proximal mechanisms underlying momentary BPD symptoms (e.g., Berenson et al., 2011; Coifman et al., 2012; Sadikaj et al., 2013). However, they have not been combined into a joint model. They also generally have not been tested in individuals’ actual lives, as contributors to naturally-occurring symptoms. Reviewing several theoretical accounts of BPD led to our observation that many of the theories share the contingency model. After our review of the literature, we came to the following list of potential triggers (see Law et al., in press for negative emotions triggering BPD symptoms). Although this list is not exhaustive, it is inclusive of a variety of proposed triggers of BPD in the literature.
Because of heightened rejection sensitivity, rejection and abandonment are theorized to be two important triggers, leading in particular to interpersonal symptoms (Berenson et al., 2011; Zeigler-Hill & Abraham, 2006). Because of insecure attachment styles, disappointment in others and being alone are proposed as triggers (Bender & Skodol, 2007; Gunderson, 1996). Disappointment and being alone may lead to intense devaluing of the disappointing others, anger, and paranoid ideation. Because of temperamental sensitivity to inner psychological pain from interpersonal conflict, interpersonal offenses and betrayals are proposed as important triggers for BPD (Howell, 2002; Tragesser, Lippman, Trull, & Barrett, 2008; Zanarini et al., 1998). Emotional instability, anger, impulsivity, and self-injurious behavior are all proposed to result from these triggers. Because of poor mood regulation strategies, boring situations are proposed as triggers (Linehan, 1993), particularly for identity symptoms and impulsivity. Because of a chronically unstable self-image, identity threat has been proposed as a trigger (Bender & Skodol, 2007). Identity threat refers to events or others’ behaviors that threaten cherished self-images of BPD sufferers, and may lead to loss of self and a sense of emptiness.
We test whether in-the-moment occurrences of these theoretically-identified triggers predict in-the-moment occurrences of the nine defining symptoms of BPD. Each individual reported his or her current triggers and current symptoms multiple times per day, over the course of several days. We predict that contingencies are likely to be significant and differ across symptom-trigger pairs. We predict that contingencies are likely to be stronger for those with greater BPD severity. However, the contingency approach suggests that contingencies are normal processes of responding to the stresses of daily life, so we expect that all individuals are likely to show the contingencies to some extent (Furr et al., in preparation).
Both the triggers and the symptoms are likely to co-occur (Hawkins et al., 2014). Thus, our hypotheses about the specific symptoms to follow from the specific triggers are mostly exploratory. We are also able to test whether triggers are distinct from each other or whether they have a common core that is responsible for their association with BPD symptoms, by controlling for each other in the prediction of symptoms.
The Three Components of the Contingency and the Role of BPD Severity
The contingency model allows separation of three components of the contingency process. The three components of the contingency model are the trigger, the symptom, and the contingency between the trigger and the symptom (see Figure 1).
Figure 1.
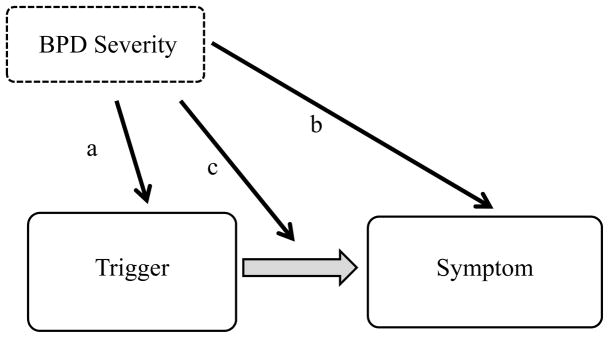
The contingency is the association of symptoms with theoretically relevant triggers. BPD severity is hypothesized to affect all three components of the contingency: (a) increased frequency and intensity of triggers; (b) increased frequency and intensity of symptoms; and (c) increased strength of the contingency between symptoms and triggers.
We expect BPD severity to relate to all three components of the contingency. First, we predict that BPD severity is likely to be associated with increased presence of triggers in everyday life. Trigger occurrences are likely to be associated with BPD severity because symptom occurrences themselves may produce an increased likelihood of triggers, particularly via their impact on interpersonal relationships. Additionally, triggers are likely to be associated with BPD severity because BPD severity likely influences the perception and interpretation of events as stressful (Arntz & Veen, 2001; Tragesser et al., 2008). In this paper, we do not attempt to discover whether the events themselves or the perceptions of the events are responsible for increased triggers. Rather, we are undertaking the first step of testing whether BPD severity is indeed associated with the frequency of situational triggers.
Second, we predict that BPD severity moderates the contingencies between triggers and symptoms, such that those with high BPD severity have stronger contingencies of symptoms on triggers. If BPD severity moderates the contingency, then this would suggest that a key feature of the disorder is a hyper-reactivity to triggers. Such a finding would suggest defining the disorder in part by dynamic processes rather than only by symptom counts. It would also support contingency-based treatments. If BPD severity does not moderate the contingencies, then this would imply that reacting to triggers (e.g., betrayal) with symptoms (e.g., intense anger) is a normal psychological process, not unique to BPD. It would imply continuity of symptom-relevant psychological functioning across the spectrum.
Third, we make the straightforward prediction that BPD severity is associated with frequency of BPD symptoms in everyday life. Fourth, we test whether BPD severity continues to predict the frequency of symptoms after accounting for the contingency of symptoms on triggers. If the associations between BPD severity and symptoms are reduced, then this would imply that the contingency accounts for part of the reason that individuals with BPD experience increased symptoms. That is, we predict that the difference in symptom occurrences across the BPD severity spectrum is partially accounted for by trigger-symptom contingencies.
Method
The current study was part of the first phase of a larger, five year longitudinal personality project. For more information about the study see Hawkins et al. (2014) and Law et al. (in press). The method described focuses on the relevant measures and procedures for the current study.
Participants
Two-hundred and eighty-two adults participated in the first phase of the project. Participants were recruited using two recruitment protocols: one targeted individuals with high borderline pathology (n = 187) and the other recruited for a community subsample (n = 95). For the former subsample, participants had to endorse seven items on the McLean Screening Instrument for BPD (MSI-BPD; Zanarini et al., 2003). There was no requirement on the MSI-BPD score for participants in the community subsample. Inclusion criteria for both subsamples included 1) age 18–65, 2) proficiency with English, and 3) residing within 50 miles. Exclusion criteria for both subsamples included 1) a court-appointed guardian, 2) current alcohol or substance dependency, 3) current psychotic disorder, 4) current suicidal ideation, 5) score below 24 on the Mini-Mental Status Examination (MMSE; Folstein, Folstein, & McHugh, 1975), 6) inability to complete ESM reports, and 7) arrest for a violent crime.
Of the 282 participants, 255 had analyzable ESM reports (at least 20% valid). The 255 participant sample (67.8% female; Mage = 44 years, SD = 11.2 years) was racially diverse (60% White, 34.5% Black) and economically diverse (median annual household income = $25,000–$29,000, range = below $0 to $149,000). Lifetime individual psychotherapy was 56%, lifetime psychiatric medication was 45%, and lifetime psychiatric hospitalization was 22%. Forty-seven percent met criteria for a mood disorder, 44% met criteria for an anxiety disorder, and 11% met criteria for an alcohol or substance disorder, as assessed by the Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). Seventy-seven participants met criteria for BPD according to their scores on the Structured Interview DSM-IV Personality (SIDP-IV; Pfhol, Blum, & Zimmerman, 1997). BPD and non-BPD (NBPD) groups had similar percentages of females (BPD = 74.0%; NBPD = 65.2%) and Caucasians (BPD = 53.2%; NBPD = 61.2%), but differed with regard to mean number of BPD symptoms (BPD = 6.3; NBPD = 1.5), mean age (BPD = 41.15; NBPD = 45.29), mean years of education (BPD = 13.75; NBPD = 15.08), and median income (BPD = $12,000–$12,999; NBPD = $35,000–$39,999). Controlling for these demographic differences in the subsequent analyses did not change the findings substantively.
Procedure and Measures
After screening and consent, participants completed demographic and self-report questionnaires before coming into the laboratory for a second individual meeting. A research staff member with a Master’s or Doctoral degree administered the MINI and SIDP-IV and provided instructions for completing ESM reports. Following this meeting, participants carried a PDA for 14 days and were prompted to complete ESM reports at specific times five times per day (i.e., 10 a.m., 1 p.m., 4 p.m., 7 p.m., and 10 p.m.). Participants received up to $175 for participating in phase one of the project.
ESM Reports
Participants responded to questions based upon their experiences in the last 60 minutes. BPD symptoms were measured using a 6-point scale ranging from 0 (does not describe me at all) to 5 (describes me very well), whereas situational triggers were measured using a 6-point scale ranging from 0 (disagree strongly) to 5 (agree strongly). Each of the nine DSM symptoms was measured by two items, except self-harm which was measured by one item1. Symptoms assessed by two items were averaged to create a BPD symptom score. The reliability for each symptom to measure systematic change was as follows: effort to avoid abandonment = .59, relationship intensity = .48, uncertain sense of self = .62, impulsive behavior = .65, unstable mood = .78, feeling empty = .88, intense anger = .83, unreal experience = .37 (see Cranford et al., 2006). Situational triggers were measured by one item each (e.g., “Someone rejected me or left me out,” “I was alone and isolated from others”). ESM reports were considered invalid if they were completed too quickly (i.e., 500 ms or faster), completed more than three hours after a designated start time or five minutes before a designated start time, or if there was an insufficient number of reports (i.e., less than 14 valid reports). Across the 70 possible reports, participants completed an average of 44 reports (63%), which is somewhat lower than the completion rate of a prior ESM study of BPD (71%; Coifman et al., 2012). As in a prior study (Sadikaj et al., 2013), the BPD group completed fewer reports compared to the NBPD group (BPD = 40.5; NBPD = 45.2).
SIDP-IV
We used the SIDP-IV (Pfhol et al., 1997) to assess BPD. Each of the nine BPD symptoms was rated using the scoring guidelines provided by Pfhol et al. (1997) on the following scale (0–3): not present, subthreshold, present, or strongly present. Responses are rated on a scale from 0 to 3, and a rating of 0 or 1 means the criterion for the symptom is not met and a rating of 2 or 3 means the criterion is met (Pfhol et al., 1997). Interviews were audio-taped, and 20 were reviewed by a second rater for purposes of reliability estimation. For those 20 interviews, across the nine symptoms, inter-rater reliability ranged from .79 to .92, mean = .88. To improve reliability and power (Morey et al., 2007), we treated BPD symptoms dimensionally in the subsequent analyses.
Results
Relationship Between Situational Triggers and BPD Severity
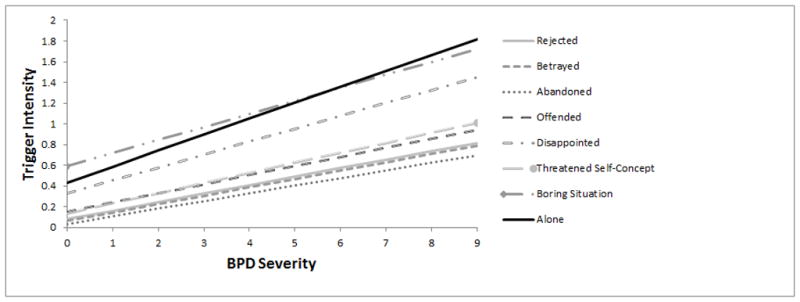
The first question is whether BPD severity predicted increased triggers. The overall average of each trigger across the two-week period was computed for each participant. As shown in Figure 2, BPD severity was associated positively with trigger intensity, b’s = .07 – .15, all p’s < .001. The heightened occurrence of triggers among those with high BPD severity may be due to interpretation of events or to objective occurrence of triggers.
Figure 2.
Within-Person Dynamic Relations Between Situational Triggers and Symptoms
The central test of the contingency model is whether the occurrences of symptoms are timed to the occurrences of triggers. We used MLM to take into account the hierarchical nature of ESM data and the differential number of ESM reports completed, and to investigate within-person relationships. Triggers were centered around each person’s mean to control for between-person differences in the level of triggers. In the first set of analyses, all triggers were entered individually as fixed and random effects at level 1. All analyses included random intercepts. Each symptom served as a dependent variable.
As can be seen in Table 1, all symptoms except self-harm were highly contingent on the triggers. Symptoms occurred more often when triggers were present and occurred less often when triggers were not present. Some of these contingencies were quite strong. In a second set of analyses, all triggers were entered simultaneously (as fixed but not random effects due to the large number of predictors). Thus, in these analyses, each trigger’s effect was estimated after controlling for the co-occurrence of other triggers. As shown in Table 1 with superscript a’s and b’s, each trigger had at least four unique effects on symptoms. Trigger-symptom contingencies often occurred in discriminative and meaningful patterns. For example, being betrayed uniquely predicted intense relationships, uncertain sense of self, intense anger, and unreal experiences, but did not uniquely predict feeling empty.
Table 1.
Contingencies of Momentary BPD Symptoms on Triggers
| Avoid Aband. | Relation Intens. | Uncert. Self | Impuls Behav | Self Harm | Unstab. Mood | Feeling Empty | Intense Anger | Unreal Exp. | |
|---|---|---|---|---|---|---|---|---|---|
| Rejected | .149**b (.190**) | .276**b (.210**) | .173**b (.200**) | .139**b (.170**) | .008 (.051**) | .394**b (.223**) | .248**b (.234**) | .242** (.254**) | .161**b (.194**) |
| Betrayed | .127** (.180**) | .318**b (.226**) | .192**b (.219**) | .155**b (.179**) | .010 (.044**) | .442**b (.251**) | .230** (.256**) | .354**b (.277**) | .204**b (.219**) |
| Abandoned | .210**b (.184**) | .300**b (.226**) | .216**a (.233**) | .134** (.187**) | .025*b (.085**) | .420** (.251**) | .301**b (.280**) | .220**b (.262**) | .235**b (.250**) |
| Offended | .065**b (.137**) | .265**b (.210**) | .141**b (.185**) | .119**b (.166**) | .014*b (.063**) | .353**b (.208**) | .163** (.216**) | .337**b (.244**) | .125**a (.148**) |
| Disappointed | .081**b (.117**) | .217**b (.181**) | .113**b (.161**) | .102**b (.147**) | .007 (.035**) | .302**b (.211**) | .160**b (.192**) | .240**b (.227**) | .099**b (.133**) |
| Threatened Self-Concept | .090**b (.139**) | .245**b (.194**) | .225**b (.212**) | .140**b (.193**) | .017b (.100**) | .361**b (.250**) | .242**b (.235**) | .283**b (.279**) | .145**b (.160**) |
| Boring Situation | .014 (.081**) | .040** (.135**) | .051**b (.128**) | .033** (.113**) | .005 (.036**) | .076**b (.188**) | .120**b (.211**) | .029* (.146**) | .035**b (.098**) |
| Alone | .050**a (.126**) | .043** (.157**) | .074**b (.162**) | .048**b (.121**) | .006 (.062**) | .100**a (.218**) | .163**b (.200**) | .041** (.175**) | .058**b (.132**) |
Note. Table entries are unstandardized coefficients from multilevel models predicting a BPD symptom from individual triggers. Numbers in parentheses are standard deviations of the contingency across individuals, representing the amount individuals have different contingencies from each other.
BPD = Borderline personality disorder; Avoid Aband = efforts to avoid abandonment; Rel Intens = relationship intensity; Uncertain Self = uncertain sense of self; Impulsive Beh = impulsive behavior; Unreal Exp = unreal experience.
p < .05,
p < .01;
p < .05 when controlling for other triggers,
p < .01 when controlling for other triggers.
The standard deviations in parentheses indicate the degree to which individuals differed from each other in their contingencies in the first set of analyses. As can be seen, all contingencies differed significantly between individuals. For example, although the typical person’s momentary symptoms of intense anger co-occurred with being offended, some individuals had no relationship between intense anger and being offended, whereas other individuals had very strong relationships between intense anger and being offended.
Trigger-Symptom Contingency: Links to BPD Severity
One reason individuals may differ in contingencies is their degree of BPD severity. BPD severity was entered as a level 2 between-person variable in separate analyses predicting a symptom from a trigger, both as a main effect and in interaction with the trigger. Fixed effects, random intercepts, and random slopes for the triggers were included in these analyses.
BPD severity moderated the trigger-symptom relationships for most BPD symptom experiences (see Table 2). Trigger-symptom contingencies involving disappointment, self-view challenge, and personal offenses were moderated by BPD severity for all or nearly all symptoms, whereas trigger-symptom contingencies involving rejection, betrayal, and abandonment were moderated by BPD severity for several symptoms. Effects of BPD on contingencies were positive, meaning that they were stronger at the high end of BPD severity. The coefficients describe the change in the contingency slope for each additional diagnosed BPD symptom; thus, the difference across levels of BPD severity was a matter of degree. For example, someone with five BPD symptoms would have a contingency of efforts to avoid abandonment on rejection of .10 points higher than would someone with no BPD symptoms (nearly double the contingency). These results show that not only do specific triggers have unique predictions of symptoms, but that they interact with BPD severity in unique ways to predict symptoms.
Table 2.
Interactions Between Triggers and BPD Severity in Predicting Momentary Symptom Occurrences
| Avoid Aband. | Relation Intens. | Uncert. Self | Impuls Behav | Self Harm | Unstab. Mood | Feeling Empty | Intense Anger | Unreal Exp. | |
|---|---|---|---|---|---|---|---|---|---|
| Rejected | .022** | .020* | .017* | .007 | .003 | .008 | .009 | .020* | .011* |
| Betrayed | .003 | .022* | .014* | .009 | .001 | −.006 | .010 | .009 | .003 |
| Abandoned | .016 | .017 | .025* | .021* | .006 | .004 | .019 | .022* | .007 |
| Offended | .013* | .017* | .024** | .015* | .006* | .018* | .023** | .022** | .011* |
| Disappointed | .017** | .029** | .026** | .016** | .005** | .029** | .023** | .022** | .019** |
| Threatened Self-Concept | .013* | .019** | .033** | .029** | .011** | .021* | .027** | .016 | .021** |
| Boring Situation | .001 | .002 | .013** | .005 | .002 | .011 | .024** | .010* | .007* |
| Alone | −.001 | .008 | .017** | .010* | −.001 | .016* | .022** | .017** | .014** |
Note. Table entries are unstandardized interaction coefficients between BPD severity and the listed trigger from multilevel models. They describe the degree to which increases in interview-rated BPD symptoms are associated with symptom-trigger contingencies.
BPD = Borderline personality disorder; Avoid Aband = efforts to avoid abandonment; Rel Intens = relationship intensity; Uncertain Self = uncertain sense of self; Impulsive Beh = impulsive behavior; Unreal Exp = unreal experience.
p < .05,
p < .01.
Do Contingencies and Trigger Levels Explain the Heightened Symptoms of Those with BPD?
The contingency model makes the claim that one important cause of BPD symptoms is contingent reactions of symptoms to everyday triggers. Thus, it is possible that controlling for the effects of these contingencies eliminates or reduces the associations between BPD severity and the everyday experience of BPD symptoms. The following analyses tested this possibility. All analyses included fixed effects and random intercepts.
First, we assessed the main effects of BPD severity on each symptom without accounting for triggers or contingencies. The first row of Table 3 shows the associations of BPD severity with each symptom from MLM’s. As can be seen, those with high BPD severity experienced a great deal more symptoms in everyday life than those with low BPD severity.
Table 3.
Relationships Between BPD Severity and Momentary BPD Symptoms: Before and After Accounting for Triggers
| Avoid Aband. | Relation Intens. | Uncert. Self | Impuls Behav | Self Harm | Unstab. Mood | Feeling Empty | Intense Anger | Unreal Exp. | |
|---|---|---|---|---|---|---|---|---|---|
| BPD Effect Alone | .116** | .124** | .119** | .091** | .018** | .182** | .176** | .088** | .112** |
| BPD Effect Controlling for Triggers and Contingencies | .090** | .069** | .072** | .057** | .012** | .114** | .109** | .035** | .077** |
| BPD Effect Controlling for Triggers, Contingencies, and Contingency Severity Differences | .088** | .062** | .048** | .049** | .007* | .099** | .080** | .024* | .064** |
Note. Table entries are unstandardized coefficients from multilevel models, showing the increase in frequency of the symptom for each point of BPD severity. In each analysis, the DV is the symptom from the top row of the table, and the IV’s are listed on the left. Given the strong relationships between BPD severity and triggers, the fact that triggers remained significant predictors of symptoms (except for isolated triggers predicting anger or self-harm) means that the reductions in the BPD associations were meaningful.
BPD = borderline personality disorder; Avoid Aband = efforts to avoid abandonment; Relation Intens = relationship intensity; Uncert Self = uncertain sense of self; Impuls Behav = impulsive behavior; Unstab Mood = unstable mood; Unreal Exp = unreal experience.
p < .05,
p < .01.
To test whether contingencies account for these heightened symptom levels, we predicted symptom levels from BPD after controlling for all triggers at level 1 in MLM’s. Because the effects of triggers on symptoms can only go through contingencies, and because the MLM’s control for within-person associations, this analysis essentially controls for both contingencies and levels of triggers. As can be seen in the second row of Table 3, there were reductions in the associations between BPD severity and all symptom occurrences. That is, much of the reason that those with high BPD severity experience more symptoms is that they encounter more triggers, and that symptoms are contingent upon the presence of triggers.
To more explicitly control for contingencies, the final analyses predicted triggers from BPD severity while controlling for all triggers, and also controlling for BPD severity differences in contingencies (by controlling for the interactions between BPD and triggers). The third row of Table 3 shows the results of these analyses. As can be seen, the associations between BPD severity and symptoms were still present, but were reduced still further. The reductions were due to the fact that contingencies were stronger for those with high BPD severity than for those with low BPD severity.
Discussion
The first goal of this study was to test the idea that symptoms of BPD are short-term events, tied systematically to the appearances of triggers in everyday life, as suggested in the contingency model. The second goal was to identify which triggers were associated with which symptoms. The third goal was to investigate whether BPD differs from normal functioning in terms of trigger-symptom contingencies.
Results revealed a rich set of concurrent relations between a variety of triggers and BPD symptoms. Triggers co-occurred independently with all symptoms of BPD for the average participant. Each trigger had unique relations with multiple symptoms, even while controlling for the overlap among the triggers. These unique relations were related discriminatively to the content of the triggers and the symptoms, in ways that made intuitive sense. Each of the defining symptoms of BPD was contingent on at least some triggers occurring in everyday life.
BPD severity predicted all three components of the contingency. People with high BPD severity had more triggers in their lives, they had more symptoms in their lives, and they had greater contingencies of symptoms on the triggers compared to people with low BPD severity. This enhanced symptomatic reactivity was a matter of degree, because individuals at both ends of the BPD severity spectrum reacted to triggers with symptoms, indicating a common psychological process. Triggers and contingencies accounted for much of the effects of BPD severity on experienced symptoms, suggesting that those with high BPD severity experience more symptoms compared to those with low BPD severity in part because they experience more triggers and react to them more strongly in their everyday lives. Accounting for this made individuals with high BPD severity appear more similar to those with low BPD severity in terms of the number of symptoms experienced; however, some disparity in symptom occurrences remained across the severity spectrum, suggesting that other proximal mechanisms may also account for the everyday experience of symptoms among people with high BPD severity.
Implications for the Contingency Approach and the Relevance of Proximal Mechanisms
There is a growing interest in testing the contingency approach to personality disorders in general and to BPD in particular (Furr et al., in preparation; Pincus, Lukowitsky, Wright, & Eichler, 2009; Wright, Pincus, & Lenzenweger, 2010). The contingency approach argues that it is important to look not only to distal mechanisms (e.g., childhood abuse), but also to proximal mechanisms underlying BPD symptoms.
A few studies have provided initial evidence that contingencies are present in BPD. Using ESM, studies have found that people with BPD experience more symptoms following negative emotional experiences (Law et al., in press), react with rage and devaluation to rejection (Berenson et al., 2011), react with impulsive and risky behavior to positive and negative affective and interpersonal experiences (Coifman et al., 2012), and react to others’ quarrelsome behavior with quarrelsomeness of their own (Sadikaj et al. 2013).
The current study adds strong evidence for a contingency approach by showing that all nine defining symptoms of BPD are associated with situational triggers and by showing that a variety of theoretically-proposed triggers indeed predict symptoms. Because the symptoms were worded closely to the symptoms in the DSM-IV-TR and section II of the DSM-5, our results mean that even the defining symptoms of BPD appear to occur at least somewhat as short-term, partly contingent events. To the extent that the DSM-IV-TR and DSM-5 section II BPD criteria are similar to the newly proposed BPD criteria in section III of the DSM-5, our findings may apply to those criteria, meaning that those criteria may also be short-term, partly contingent events. Additional research would be needed to evaluate this possibility.
Implications for the Role of Specific Triggers and Symptoms in BPD and in Everyday Life
Each of the triggers was chosen because a theory had proposed it to be important in understanding the etiology of BPD. The results showed that each of these theoretical propositions was supported: All of the proposed triggers uniquely predicted symptoms. Thus, rejection, betrayal, abandonment, offense, disappointment, self-concept threats, boredom, and isolation have different and powerful meanings for BPD symptoms. Further investigation of these meanings is likely to reveal independent information about the proximal mechanisms underlying BPD.
The triggers with the strongest unique predictions were being offended, being disappointed by others, and having one’s self-concept threatened. These triggers uniquely predicted all or almost all of the symptoms and did so strongly, particularly among people with high BPD severity. These results suggest future research be directed to these triggers in particular.
The contingencies made logical sense given the content of the associated triggers and symptoms. For example, being abandoned uniquely predicted efforts to avoid abandonment. Being offended was the strongest unique predictor of intense anger. Having one’s self-concept threatened was the strongest unique predictor of uncertain sense of self. In addition to providing validity evidence for the method, these findings demonstrate the sophistication and complexity with which symptoms and triggers are discriminated and connected to each other across the flow of daily life.
Implications for Distinctiveness/Continuity with Normal Functioning
Individuals across the BPD spectrum experienced the same kinds of triggers, experienced the same symptoms, and demonstrated the same contingencies of symptoms on triggers, despite differences in the degree of triggers, symptoms, and contingencies across the BPD spectrum. The finding that the contingencies were found across the BPD spectrum suggests that the psychological process of reacting to triggers with symptoms is a process common to those all along the BPD severity spectrum. Furthermore, it is a process at the core of BPD, in that it explains the occurrence of defining symptoms of BPD. Additionally, when triggers and contingencies were taken into account, nearly half of the symptom disparity between those with high and low BPD severity was eliminated. Combined with the finding that the unique trigger-symptom contingencies were logical based on their content, our findings suggest that BPD does not involve a particularly unusual set of responses to the stresses of everyday life.
Rather, in regards to the experience of BPD symptoms in everyday life, the difference between those with high and low BPD severity appears to be largely a matter of degree. Those with high BPD severity have more triggers, more symptoms, and stronger symptomatic reactions to the triggers than those with low BPD severity. For example, intense anger was contingent upon all triggers for all individuals, and also had many interactions with BPD severity. This means that all individuals’ intense anger was contingent on these triggers, and this was especially true for those with high BPD severity. Thus, the proportionality of response appears to be more important than the response itself in understanding the proximal etiology of BPD symptoms.
Implications for Treatment
The findings of contingencies between triggers and symptoms are consistent with treatments that focus on teaching individuals how to cope with events that have been associated with symptom occurrences. For example, behavioral analysis is a key component of Dialectical Behavioral Therapy (DBT), in which a therapist works with a patient to identify problem behaviors and then subsequently identify events that trigger those behaviors (Linehan, 1993). If patients become aware of their personal “triggering” events, then they can work with their therapist to improve their emotion regulation skills. More broadly, all six empirically-supported treatments for BPD include or highlight a component of interpreting and reacting to triggers appropriately. Thus, these findings provide empirical support for major components of those treatment approaches.
The findings of significant individual differences in contingencies across-the-board are interesting in the treatment context. These findings suggest that different individuals responded to the triggers in different ways. Particular triggers may be more upsetting to some individuals than to others, and particular triggers may co-occur with symptomatic responses to a greater degree among some individuals than others. Individualized treatment that recognizes these differences and focuses on each individual’s particularly problematic contingencies may be the most effective (e.g., Roche, Pincus, Rebar, Conroy, & Ram, 2014).
In fact, experience-sampling assessment may eventually be developed into an effective treatment aid (e.g., Kramer et al., 2014; Telford, McCarthy-Jones, & Rowse, 2012). Participants could complete an experience-sampling assessment of contingencies early in treatment. Therapists could then use the results to guide treatment based on the client’s particularly strong contingencies. Later in treatment, experience-sampling assessment could be used to evaluate treatment progress.
Limitations and Future Directions
One limitation of this study is that concurrent associations cannot determine the direction of causality. It is plausible that heightened levels of BPD symptoms could lead an individual to perceive more interpersonal stress or detachment in his/her immediate environment, or that third variables cause both triggers and symptoms. One trade-off to obtaining rich data from everyday life using ESM is a reduced ability to test causal direction. Future research should address the causal direction of these contingencies.
A second limitation was the fact that triggers and symptoms were self-reported. The reports of trigger presence and intensity may not correspond exactly to what independent observers might perceive. Indeed, those with high BPD severity reported more triggers than did those with low BPD severity, and we cannot be sure whether that finding represents an actual greater presence of triggers, a negatively-biased interpretation of events, or both (Arntz & Veen, 2001). In either case, however, that finding reveals that those with high BPD severity experience and perceive more triggers in their everyday lives than those with low BPD severity.
Similarly, self-reports of symptoms may not be exactly the same as what independent observers would provide. However, self-reports of symptoms were tied in meaningful and subtly discriminating ways to triggers and BPD severity. Moreover, a recent study conducted in our laboratory found that the clinician-rated and self-reported BPD symptoms assessed in this study showed similar unidimensional factor structures (Hawkins et al., 2014), while Hopwood et al. (2008) found minimal differences between BPD symptoms as assessed by interview and self-report on measures of functioning. Together, these studies suggest that people can report their symptom occurrences in a valid and reliable manner. Nevertheless, future research is needed to determine the accuracy of self-reports of triggers and symptoms.
Third, although BPD severity was a predictor of all three components of the contingency, it is not clear what specific aspects of BPD bring about such findings. BPD may be a kind of general proxy variable for specific psychological features of an individual. For example, it may not be BPD, per se, that affects contingency strength, but rather having a history of childhood abuse or neglect (Zanarini et al., 2002), learning impairments (Ebner-Premier et al., 2009), or maladaptive schemata (Young et al., 2003). Similarly, personality traits such as neuroticism or antagonism may be the source of heightened triggers, symptoms, and contingencies among those with BPD. Future research should be conducted to identify the specific aspects of BPD that bring about the findings of this study. Identifying such active features of BPD would bring proximal and distal causes into conjunction in the explanation of BPD. The distal causes would work partly through heightening the three components of the contingency: heightening trigger frequency, symptom frequency, and contingency strength.
A fourth limitation is that we conducted a large number of analyses, thereby raising the possibility of a Type I error. We believe it is unlikely that we have made many, if any, Type I errors because most of the significant findings have small p-values, the symptoms are strongly correlated with one another (Hawkins et al., 2014) and our findings are consistent with theories of BPD and nearly all therapeutic approaches for BPD.
Conclusions
The findings of this study indicate that the contingency model of symptoms is a useful framework for investigating the proximal mechanisms underlying the experience of all nine defining symptoms of BPD. This study revealed that BPD symptoms are short-term events, tied systematically to the occurrences of triggers in everyday life. Triggers previously identified in the literature as important to BPD all had significant, unique, and meaningful predictions of symptoms. People across the BPD spectrum experienced the same stressors, symptoms, and trigger-symptom contingencies. However, those with high BPD severity had quantitatively more of all three components of the contingency: more triggers, more symptoms, and stronger contingencies. Together, these results provide strong evidence that trigger-symptom contingencies may be key proximal mechanisms that contribute to symptom expression in everyday life.
Acknowledgments
Research presented in this manuscript was supported by the National Institute of Mental Health of the National Institutes of Health under award number R01MH70571. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Jennifer L. Wages, Michelle Anderson, and Lara Kammrath for their valuable contributions to this work.
Footnotes
Symptom items included the following: Efforts to avoid abandonment: I called someone to reassure themselves that he or she still cared about the target; I did things to avoid feeling abandoned or being abandoned, like trying to stop someone from leaving or keeping tabs on someone. Relationship instability: An interpersonal relationship of mine was unstable and intense; I thought that people close to me were worthless, although recently I have thought they were wonderful. Identity disturbance: My sense of self was unstable; I felt like I didn’t know who I am or like I had no identity. Impulsivity: I couldn’t stop myself from overdoing something bad; I had a problem with impulsivity (e.g., an eating binge, spending spree, drinking too much, or a verbal outburst). Self-harm: I hurt myself on purpose (e.g. punched myself, cut myself, or burned myself). Affective instability: My emotions were on a roller coaster; I was extremely moody. Emptiness: I felt hollow inside; I had feelings of emptiness. Uncontrollable anger: I had difficulty controlling my anger; I lost my temper with someone. Transient paranoid ideation: I was thinking suspicious or paranoid thoughts; I felt unreal or things around me felt unreal.
Contributor Information
Kelly Miskewicz, Wake Forest University.
William Fleeson, Wake Forest University.
Elizabeth Mayfield Arnold, Wake Forest School of Medicine.
Mary Kate Law, Western State Hospital.
Malek Mneimne, Wake Forest University.
R. Michael Furr, Wake Forest University.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders – Text revision. 4. Washington, DC: 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Arntz A, Veen G. Evaluations of others by borderline patients. Journal of Nervous and Mental Disease. 2001;189(8):513–521. doi: 10.1097/00005053-200108000-00004. [DOI] [PubMed] [Google Scholar]
- Bender DS, Skodol AE. Borderline personality as self-other representational disturbance. Journal of Personality Disorders. 2007;21(5):500–517. doi: 10.1521/pedi.2007.21.5.500. [DOI] [PubMed] [Google Scholar]
- Berenson KR, Downey G, Rafaeli E, Coifman KG, Paquin NL. The rejection–rage contingency in borderline personality disorder. Journal of Abnormal Psychology. 2011;120(3):681–690. doi: 10.1037/a0023335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coifman KG, Berenson KR, Rafaeli E, Downey G. From negative to positive and back again: Polarized affective and relational experience in borderline personality disorder. Journal of Abnormal Psychology. 2012;121(3):668–679. doi: 10.1037/a0028502. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Shrout PE, Iida M, Rafaeli E, Yip T, Bolger N. A procedure for evaluating sensitivity to within-person change: Can mood measures in diary studies detect change reliably? Personality and Social Psychology Bulletin. 2006;32(7):917–929. doi: 10.1177/0146167206287721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Mauchnik J, Kleindienst N, Schmahl C, Peper M, Rosenthal MZ, Bohus M. Emotional learning during dissociative states in borderline personality disorder. Journal of Psychiatry & Neuroscience. 2009;34(3):214–222. [PMC free article] [PubMed] [Google Scholar]
- Fleeson W. Perspectives on the person: Rapid growth and opportunities for integration. In: Deaux K, Snyder M, editors. The Oxford handbook of personality and social psychology. New York, NY US: Oxford University Press; 2012. pp. 33–63. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Furr RM, Fleeson W, Anderson M, Arnold EM. A general model of borderline symptomology based on the core-contingency principle. in preparation. Manuscript in Preparation. [Google Scholar]
- Glaser JP, Van Os J, Thewissen V, Myin-Germeys I. Psychotic reactivity in borderline personality disorder. Acta Psychiatrica Scandinavica. 2010;121(2):125–134. doi: 10.1111/j.1600-0447.2009.01427.x. [DOI] [PubMed] [Google Scholar]
- Gunderson JG. Borderline patient’s intolerance of aloneness: Insecure attachments and therapist availability. The American Journal of Psychiatry. 1996;153(6):752–758. doi: 10.1176/ajp.153.6.752. [DOI] [PubMed] [Google Scholar]
- Hawkins AA, Furr RM, Arnold EM, Law MK, Mneimne M, Fleeson W. The structure of borderline personality disorder symptoms: A multi-method, multi-sample examination. Personality Disorders: Theory, Research, and Treatment. 2014;5(4):380–389. doi: 10.1037/per0000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Morey LC, Edelen MO, Shea MT, Grilo CM, Sanislow CA, Skodol AE. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychological Assessment. 2008;20:81–85. doi: 10.1037/1040-3590.20.1.81. [DOI] [PubMed] [Google Scholar]
- Howell EF. Back to the “states”: Victim and abuser states in borderline personality disorder. Psychoanalytic Dialogues. 2002;12(6):921–957. doi: 10.1080/10481881209348713. [DOI] [Google Scholar]
- Jahng S, Solhan MB, Tomko RL, Wood PK, Piasecki TM, Trull TJ. Affect and alcohol use: An ecological momentary assessment study of outpatients with borderline personality disorder. Journal of Abnormal Psychology. 2011;120(3):572–584. doi: 10.1037/a0024686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer I, Simons CJP, Wigman JTW, Collip D, Jacobs N, Derom C, Wichers M. Time-lagged moment-to-moment interplay between negative affect and paranoia: New insights in the affective pathway to psychosis. Schizophrenia Bulletin. 2014;40(2):278–286. doi: 10.1093/schbul/sbs194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law MK, Fleeson W, Arnold EM, Furr RM. Using negative emotions to trace the experience of borderline personality pathology: Interconnected relationships revealed in an experience sampling study. Journal of Personality Disorders. doi: 10.1521/pedi_2015_29_180. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York, NY US: Guilford Press; 1993. [Google Scholar]
- Mischel W, Shoda Y. A cognitive-affective system theory of personality: Reconceptualizing situations, dispositions, dynamics, and invariance in personality structure. Psychological Review. 1995;102(2):246–268. doi: 10.1037/0033-295X.102.2.246. [DOI] [PubMed] [Google Scholar]
- Pfhol B, Blum N, Zimmerman M. Structured interview for DSM-IV personality (SIDP) Washington, D.C: American Psychiatric Association; 1997. [Google Scholar]
- Pincus AL, Lukowitsky MR, Wright AGC, Eichler WC. The interpersonal nexus of persons, situations, and psychopathology. Journal of Research in Personality. 2009;43(2):264–265. doi: 10.1016/j.jrp.2008.12.029. [DOI] [Google Scholar]
- Roche MJ, Pincus AL, Rebar AL, Conroy DE, Ram N. Enriching psychological assessment using a person-specific analysis of interpersonal processes in daily life. Assessment. 2014;21:515–528. doi: 10.1177/1073191114540320. [DOI] [PubMed] [Google Scholar]
- Sadikaj G, Moskowitz SD, Russell JJ, Zuroff DC, Paris J. Quarrelsome behavior in borderline personality disorder: Influence of behavioral and affective reactivity to perceptions of others. Journal of Abnormal Psychology. 2013;122(1):195–207. doi: 10.1037/a0030871. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.) The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- Stiglmayr CE, Ebner-Priemer UW, Bretz J, Behm R, Mohse M, Lammers CH, Bohus M. Dissociative symptoms are positively related to stress in borderline personality disorder. Acta Psychiatrica Scandinavica. 2008;117(2):139–147. doi: 10.1111/j.1600-0447.2007.01126.x. [DOI] [PubMed] [Google Scholar]
- Telford C, McCarthy-Jones S, Corcoran R, Rowse G. Experience sampling methodology studies of depression: The state of the art. Psychological Medicine. 2012;42(6):1119–1129. doi: 10.1017/S0033291711002200. [DOI] [PubMed] [Google Scholar]
- Tragesser SL, Lippman LG, Trull TJ, Barrett KC. Borderline personality disorder features and cognitive, emotional, and predicted behavioral reactions to teasing. Journal of Research in Personality. 2008;42(6):1512–1523. doi: 10.1016/j.jrp.2008.07.003. [DOI] [Google Scholar]
- Verheugt-Pleiter A, Deben-Mager M. Transference-focused psychotherapy and mentalization-based treatment: Brother and sister? Psychoanalytic Psychotherapy. 2006;20(4):297–315. doi: 10.1080/02668730601020374. [DOI] [Google Scholar]
- Wenzel A, Chapman JE, Newman CF, Beck AT, Brown GK. Hypothesized mechanisms of change in cognitive therapy for borderline personality disorder. Journal of Clinical Psychology. 2006;62(4):503–516. doi: 10.1002/jclp.20244. [DOI] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Paris J. A Prospective Investigation of Borderline Personality Disorder in Abused and Neglected Children Followed Up into Adulthood. Journal of Personality Disorders. 2009;23(5):433–446. doi: 10.1521/pedi.2009.23.5.433. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Lenzenweger MF. Modeling Stability and Change in Borderline Personality Disorder Symptoms Using the Revised Interpersonal Adjective Scales-Big Five (IASR-B5) Journal of Personality Assessment. 2010;92(6):501–513. doi: 10.1080/00223891.2010.513288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JF, Klosko JS, Weishaar ME. Schema therapy. A practitioner’s guide. NY: Guilford Press; 2003. [Google Scholar]
- Zanarini MC, Frankenburg FR, DeLuca CJ, Hennen J, Khera GS, Gunderson JG. The pain of being borderline: Dysphoric states specific to borderline personality disorder. Harvard Review of Psychiatry. 1998;6(4):201–207. doi: 10.3109/10673229809000330. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A Screening Measure for BPD: The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) Journal of Personality Disorders. 2003;17(6):568–573. doi: 10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Young L, Frankenburg FR, Hennen J, Reich DB, Marino MF, Vujanovic AA. Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline inpatients. The Journal of Nervous and Mental Disease. 2002;190(6):381–387. doi: 10.1097/00005053-200206000-00006. [DOI] [PubMed] [Google Scholar]
- Zeigler-Hill V, Abraham J. Borderline personality features: Instability of self-esteem and affect. Journal of Social and Clinical Psychology. 2006;25(6):668–687. doi: 10.1521/jscp.2006.25.6.668. [DOI] [Google Scholar]


