Abstract
Background
Training in patient-centered medical home (PCMH) settings may prepare new physicians to measure quality of care, manage the health of populations, work in teams, and include cost information in decision making. Transforming resident clinics to PCMHs requires funding for additional staff, electronic health records, training, and other resources not typically available to residency programs.
Objective
Describe how a 1115 Medicaid waiver was used to transform the majority of primary care training sites in New York State to the PCMH model and improve the quality of care provided.
Methods
The 2013–2014 Hospital Medical Home Program provided awards to 60 hospitals and 118 affiliated residency programs (training more than 5000 residents) to transform outpatient sites into PCMHs and provide high-quality, coordinated care. Site visits, coaching calls, resident surveys, data reporting, and feedback were used to promote and monitor change in resident continuity and quality of care. Descriptive analyses measured improvements in these areas.
Results
A total of 156 participating outpatient sites (100%) received PCMH recognition. All sites enhanced resident education using PCMH principles through patient empanelment, development of quality dashboards, and transforming resident scheduling and training. Clinical quality outcomes showed improvement across the demonstration, including better performance on colorectal and breast cancer screening rates (rate increases of 13%, P ≤ .001, and 11%, P = .011, respectively).
Conclusions
A 1115 Medicaid waiver is a viable mechanism for states to transform residency clinics to reflect new primary care models. The PCMH transformation of 156 sites led to improvements in resident continuity and clinical outcomes.
What was known and gap
Experts have advocated for the patient-centered medical home (PCMH), yet little is known how this may benefit resident education.
What is new
A statewide initiative funded by a Medicaid waiver transformed New York State's primary care training sites into PCMHs and assessed benefits to care and education.
Limitations
Lack of a comparison group and projects that met local needs limit generalizability.
Bottom line
PCMH transformation of resident clinics led to improved continuity and clinical outcomes.
Introduction
To achieve aims of health care quality, population health, and reduced health expenditures, physicians are being called on by employers, payers, regulators, and patients to provide care that is high quality, patient and family centered, coordinated, population based, and cost-effective.1,2 One approach is to use a 1115 Medicaid waiver as a vehicle to transform care and training in residency clinics to prepare future physicians to function effectively within the health care system.3
In 2010, New York State (NYS) received $250 million as part of its 1115 Medicaid waiver for the Hospital Medical Home Demonstration Program (HMH). HMH was structured as a set of project areas to be collaboratively undertaken by academic hospitals, their primary care residency programs (programs in family medicine, internal medicine, pediatrics, and internal medicine–pediatrics), and the clinics that served as the sites for residents’ longitudinal ambulatory primary care training.4 The 1115 waiver program offers states a vehicle to test new ways to deliver and pay for health care services. To our knowledge, this is the only 1115 waiver demonstration to date that has focused on residency programs. HMH sought to train the next generation of primary care physicians in a patient-centered medical home (PCMH) model, improve continuity between patients and residents, enhance resident accountability for quality outcomes, and use a team-based coordinated care approach for high-risk patients. A physician workforce proficient in these skill sets is an important part of NYS’ plan to transform its health system through its Delivery System Reform Incentive Payment Program5 and State Health Innovation Plan.6
A key aim of HMH is to prepare physicians for the new landscape of care. Participating hospital sites and Federally Qualified Health Centers provide primary care to more than 1 million Medicaid beneficiaries and are the training sites for more than 5000 resident physicians from 118 programs in internal medicine, family medicine, pediatrics, and internal medicine–pediatrics. Through HMH, NYS and participating sites tested innovations in care delivery and primary care resident education. The hypotheses for this innovative educational intervention were that (1) the majority of participating clinics would achieve level 2 or 3 PCMH recognition under the National Committee for Quality Assurance (NCQA)7 2011 standards; (2) the intervention would result in demonstrable improvements in resident continuity improvement projects; and (3) the coordination and quality of care for project participants would significantly improve.
Methods
Participating Hospitals
Hospitals submitted detailed work plans to NYS, including strategies, budgets, timetables for deliverables, demographic profiles, and community needs assessments for each participating site. Funding was provided at 6 different intervals during the project through an already established NYS Department of Health (DOH) hospital payment mechanism. Awards were subject to meeting required milestones. In some cases, funds had to be forfeited owing to unmet goals.
Sixty-five teaching hospitals, representing about 65% of eligible NYS hospitals, applied for participation in HMH, and all were accepted. Over the course of the project, 5 hospitals and their affiliated sites either closed or withdrew their applications, leaving 60 hospitals (156 affiliated ambulatory teaching sites) that completed the demonstration.
HMH Awards
The available funding was approximately $250 million in Designated State Health Program matching funds, with awards ranging from $118,000 to more than $15 million per hospital over the life of HMH. The average award was $250 per Medicaid member served by the project. Awards were proportionally based on (1) Medicaid volume (80%) and (2) the number of primary care residents by site (20%). Payments were made directly to hospitals and were used for a broad range of transformation costs, including electronic health records, new residency slots, consultant costs, and construction. Hospitals’ proposed work plans and budgets are available on the HMH website (https://hospitalmedicalhome.ipro.org).
Interventions
The primary intervention was the development and use of a resources website and a web-based reporting and feedback portal. The portal, developed by IPRO, the DOH’s designated External Quality Review Organization, allowed hospitals and residency programs to submit quarterly narrative reports and data for each site. This information was used to engage in quality improvement through small tests of change and Plan, Do, Study, Act cycles.
Information gathered through the portal helped inform coaching calls. DOH staff and reviewers monitored trends and tailored coaching calls and resource material to program aspects that proved the most challenging. These included calls on PCMH recognition, resident empanelment, health information technology, clinical quality measurement, and transitions of care, among others. DOH held 22 coaching calls over the course of 24 months (with an average of 100 individuals participating). In addition, the Office of Mental Health (OMH) hosted monthly calls for hospitals working on a behavioral health project within HMH. Individualized coaching at site visits, by telephone, and by e-mail was offered as well. DOH representatives visited 35 of 60 (58%) participating hospitals and their training clinics, and OMH staff visited another 11, to better understand implementation successes and challenges.
Outcomes of Interest
Project interventions had an educational focus, which allowed sites to identify areas in need of improvement, receive coaching, and monitor progress over time. To measure this progress, outcomes of interest included (1) the number of sites achieving high-level PCMH recognition under NCQA’s 2011 standards; (2) improvements in resident continuity; (3) implementation and improvement in at least 1 care coordination and integration project chosen from a predetermined list (box); and (4) reported improvements on measures of clinical performance.
In addition, a resident survey was created in conjunction with the Greater New York Hospital Association and was sent to residents at the beginning and end of the project. Surveys were completed via SurveyMonkey and included questions regarding knowledge and attitudes toward PCMH, quality measurement, and team-based care.
This demonstration was a component of an 1115 Centers for Medicare and Medicaid Services Medicaid waiver negotiated by NYS, and as such, did not require Institutional Review Board review or approval.
box Care Integration and Coordination Projects
Care Transitions and Medication Reconciliation
Integration of Physical-Behavioral Health Care
Improved Access and Coordination Between Primary and Specialty Care
Enhanced Interpretation Services and Culturally Competent Care
Analysis
Sites reported on both required and optional measures, using a mix of standardized (Quality Assurance Reporting Requirements, Health Care Effectiveness Data and Information Set, Meaningful Use) and tailored measures. Descriptive analyses of portal-reported data from baseline and final reports were used to assess achievement of project outcomes. For some closely related metrics, composite measures8 were created by averaging individual measures’ rates. Changes in rates were used to assess improvement, and when possible, a Student t test was used to determine statistical significance.
Results
PCMH Achievement
Before the start of the HMH project, 36% (56 of 156) of sites did not have PCMH recognition, and others were recognized under an older set of standards. By October 2014, 100% of sites had achieved high-level 2011 PCMH recognition. All programs engaged in practice redesign around NCQA’s PCMH standards, focusing on access, continuity, managing populations, and coordinated care.
Continuity of Care and Resident Understanding of PCMH Principles
Preliminary results suggest a number of improvements in resident continuity. The proportion of visits that occur with patients on the resident’s own panel surpassed 50% by the end of the demonstration (table). This represents a significant improvement, as most sites had limited use of panels before participating in HMH. A number of programs restructured their scheduling to 4+1 or 6+2 block scheduling with protected ambulatory time that prioritized training in ambulatory care.9
During site visits, residents presented innovative projects, including enhanced July handoffs, chronic disease registries, open-access scheduling, and coordination and comanagement with specialist residents. Residents also described the transformation of their clinical ambulatory experience:
“The added support of a care manager has allowed me the time to focus on more of the medical priorities of my patients.”
“The change to 4+1 has changed our quality of life . . . I’m able to actually understand how rewarding clinic time can be . . . I’ve been able to see the benefits of increased continuity with my patients as a result.”
[Commenting on resident dashboards] “I have learned so much about being able to see my own practice patterns with my patient panel and I feel so much more prepared for the future.”
Surveys invitations were sent to an estimated 5000 participating residents at the beginning and conclusion of the HMH project, with response rates of 20% (1000) and 18% (900), respectively. Most respondents reported favorable attitudes toward the PCMH and reported they had good knowledge of its principles and were able to apply them. The data from these surveys are still being analyzed.
Clinical Performance
The HMH project assessed 17 commonly reported clinical performance metrics, including measures for diabetes care, blood pressure control, cancer screening, weight assessments, and well-visits, among others. Improvements over the baseline were seen for 15 of these measures with increases ranging from 3% to 28%. Eight measures showed statistically significant improvement, with an average increase of 15% (select results shown in the Table).
TABLE .
Preliminary Outcome Results of the Demonstration
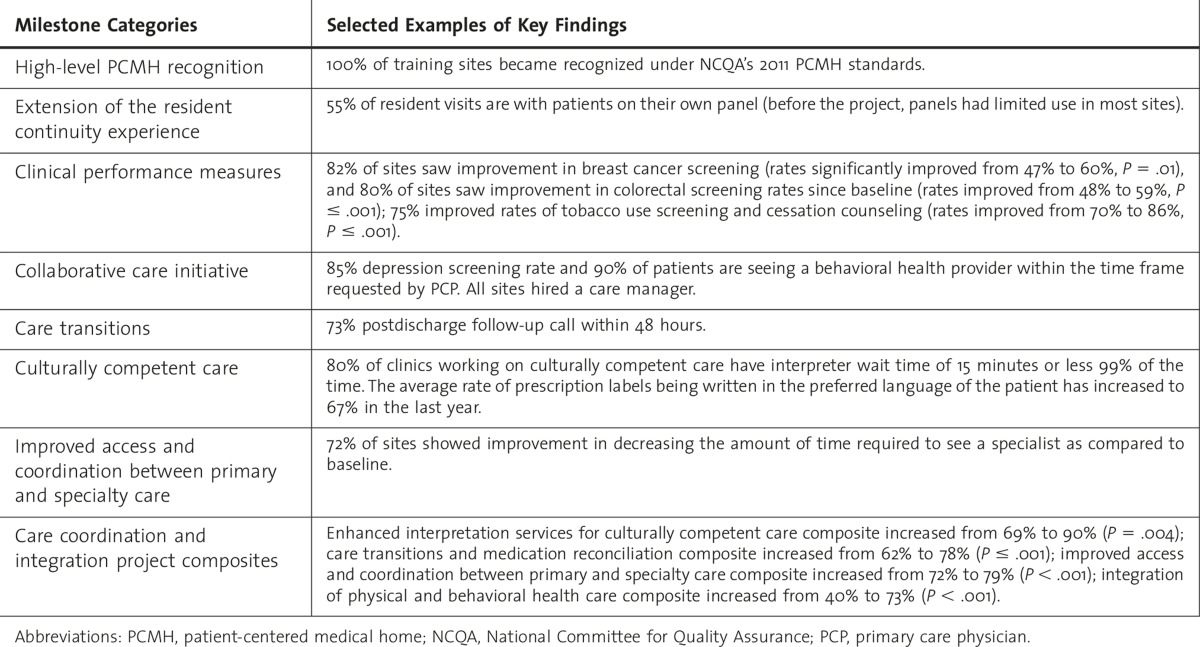
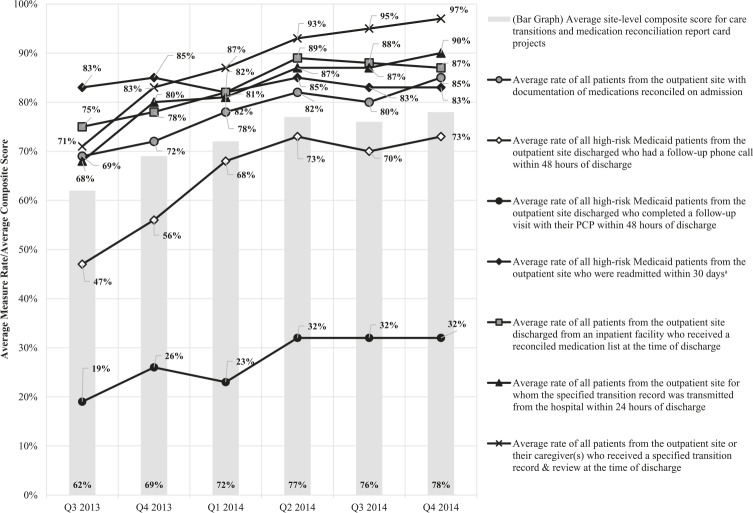
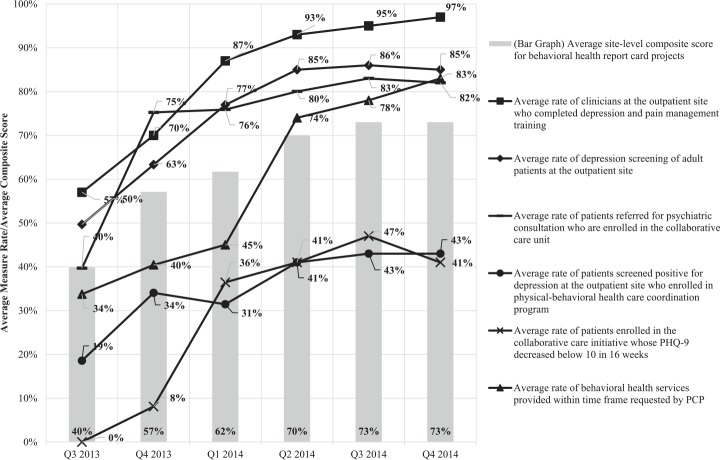
Care Coordination
Figures 1 and 2 show composite measures of care integration and coordination that include bar graphs for overall trends, and line graphs that track progress on individual components of the composite. Site-level composite scores in each of 4 care coordination project areas saw statistically significant increases over the baseline, with increases ranging from 7% to 33% (table). DOH analysts will complete a final evaluation in 2015.
FIGURE 1 .
Trends in Care Transitions and Medication Reconciliation Metrics and Composite Scores (Q3 2013–Q4 2014)
Abbreviation: PCP, primary care physician
a A lower rate is desirable for 1 measure in this graph and the inverted rate is displayed.
FIGURE 2 .
Trends in Integration of Physical and Behavioral Health Care Project Metrics and Composite Scores (Q3 2013–Q4 2014)
Abbreviations: PHQ, patient health questionnaire; PCP, primary care physician.
a Higher rates are desirable for all measures in this figure.
Discussion
The HMH project was unique in its focus on multidisciplinary coaching and education at hospitals and residency clinics, with an evaluation component that assessed the effect of transforming resident training settings, all funded through an 1115 Medicaid waiver. Other studies have identified innovations in residency settings, such as the PCMH model, strong health information technology infrastructure, improvements in continuity, and increased access,10,11 or have examined resident and patient satisfaction with PCMH settings,12 but have not collected data to study changes in both continuity and performance throughout the transformation to a PCMH model. HMH builds on research calling for the adoption of PCMH by hospital networks or residency training clinics13 by implementing a systematic approach to coaching and continuous quality improvement.
Lessons Learned
The structural discontinuity imposed by rotating residents and attending physicians’ schedules presents unique challenges to implementing a PCMH model in a residency clinic and also provides opportunities for improvement. The structure and relationship between hospitals, residency programs, and ambulatory training sites can make communication and coordination difficult especially when staffing and system resources are not in place. For example, notification systems and rapid follow-up appointments must be available to provide timely follow-up care to high-risk patients after discharge from inpatient care. It was important for hospitals to identify the staffing and resource demands of such a transformation, and allocate resources accordingly.
As sites transformed, the need for nonphysician staff grew. To meet these needs, some sites used existing staff, while others shared staff across sites or used external care management services. Standardized measurement also was new to many participants, although residents became increasingly familiar with measurement, risk-adjustment challenges, nuances of accountability, and instances when outcomes are not completely controlled by clinicians.
As with many innovative interventions, sustainability is a challenge. Programs are now confronting the reality that sustaining changes will require resources that may not yet be offset by savings from the new model of care. Overlap with other care improvement initiatives ensures some continued support for care managers, patient navigators, and other personnel required for team-based care in HMH’s participating sites.
Limitations of our intervention include the fact that HMH was structured primarily as a quality improvement project. Each participating site’s project or projects had unique features that related to its patient demographics and residency programs. For this reason, comparison to a control group was not pursued. Data were checked for consistency with standardized measures and were compared with statewide averages, but additional checks of data accuracy were not conducted. Resident surveys completed during HMH were conducted informally; while results are suggestive, they are not representative of, or generalizable to, all residents. Conclusions about significant behavior change cannot be drawn. HMH’s impact on lasting transformations in systems and behaviors are as yet unknown. While results suggest improvements in resident continuity, clinical performance, and care coordination, the extent to which these changes were caused by project activities, funding, or other factors are unknown, as is the effect on patient outcomes.
It may be useful to conduct a study of quality and utilization in HMH sites compared to other PCMH and non-PCMH sites to assess program effects. Results from this and other future evaluations may be used to inform policy recommendations related to residency training structure.
Conclusion
New York State’s 1115 Medicaid waiver-funded HMH project for ambulatory residency training proved a viable strategy for transforming residency training sites into PCMHs. HMH prepared future physicians to function effectively within the system by aligning their clinical learning environment with how they will be required to practice in the future. The project met its added aim of improving care for patients in resident clinics, as shown by beneficial preliminary results for outcomes that include cancer screening, diabetes care, and well-child visits and immunizations.
Footnotes
Marietta Angelotti, MD, is Associate Medical Director, Office of Quality and Patient Safety, New York State Department of Health; Kathryn Bliss, MSW, is Research Scientist, Office of Quality and Patient Safety, New York State Department of Health; Dana Schiffman, MPH, is Data Analyst, IPRO; Erin Weaver, BS, is Project Manager, IPRO; Laura Graham, MS, is Health Program Specialist, IPRO; Thomas Lemme, PA-C, MBA, MA, is Senior Quality Improvement Specialist, Healthcare Quality Improvement Program, IPRO; Veronica Pryor, RN, MPA, is Project Manager, Healthcare Quality Improvement Program, IPRO; and Foster C. Gesten, MD, FACP, is Medical Director, Office of Quality and Patient Safety, New York State Department of Health.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Eden J, Berwick D, Wilensky G, editors. Graduate Medical Education That Meets the Nation’s Health Needs. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 2.Nasca TJ, Weiss KB, Bagian JP. Improving clinical learning environments for tomorrow’s physicians. N Engl J Med. 2014;370(11):991–993. doi: 10.1056/NEJMp1314628. [DOI] [PubMed] [Google Scholar]
- 3.Rockey PH, Rieselbach RE, Neuhausen K, Nasca TJ, Phillips RL, Sundwall DN, et al. States can transform their health care workforce. J Grad Med Educ. 2014;6(4):805–808. doi: 10.4300/JGME-D-14-00502.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Medicare and Medicaid Services. 2015. New York State Medicaid section 1115 partnership plan approval letter. https://www.health.ny.gov/health_care/managed_care/appextension/partnership_plan/docs/pp_extension_approval_letter.pdf. Accessed April 8, [Google Scholar]
- 5.New York State Department of Health. Delivery System Reform Incentive Payment Program. https://www.health.ny.gov/health_care/medicaid/redesign/delivery_system_reform_incentive_payment_program.htm. Accessed April 8, 2015. [Google Scholar]
- 6.New York State Department of Health. The New York State Health Innovation Plan. https://www.health.ny.gov/technology/innovation_plan_initiative/. Accessed April 8, 2015. [Google Scholar]
- 7.National Commission on Quality Assurance. PCMH 2011 standards, elements, and factors. http://www.ncqa.org/portals/0/Programs/Recognition/PCMH_2011_Data_Sources_6.6.12.pdf. Accessed April 8, 2015. [Google Scholar]
- 8.New York State Department of Health. Required metrics for composite calculations by care integration and coordination project. https://hospitalmedicalhome.ipro.org/pdf/Required_Metrics_for_Composite_Calculations.pdf. Accessed March 25, 2015. [Google Scholar]
- 9.Mariotti J, Shalaby M, Fitzgibbons J. The 4:1 schedule: a novel template for internal medicine residents. J Grad Med Educ. 2010;2(4):541–547. doi: 10.4300/JGME-D-10-00044.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cordasco K, Wynn B. 2010. Site visits to selected institutions with innovations in residency training [working paper]. RAND Health. http://67.59.137.244/documents/Oct10_Sitevisits_Contractor.pdf. Accessed April 9, 2015. [Google Scholar]
- 11.Association of American Medical Colleges. Moving the medical home forward: innovations in primary care training and delivery. 2010. http://www.ucdmc.ucdavis.edu/internalmedicine/newsroom/teach_aamc.pdf. Accessed April 3, 2015. [Google Scholar]
- 12. Hochman ME, Asch S, Jibilian A, Chaudry B, Ben-Ari R, Hsieh E, et al. Patient-centered medical home intervention at an internal medicine resident safety-net clinic. JAMA Intern Med 2013. 173 18 1694 1701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Townley C, Mooney K. 2014. The role of hospitals in medical home initiatives and strategies to secure their support and participation. State Health Policy Briefing: a publication of the National Academy for State Health Policy. http://www.nashp.org/sites/default/files/Hosp_PCMH_Brf.pdf. Accessed April 8, 2015. [Google Scholar]