Abstract
Objective
Otologic complaints may place a significant burden on emergency departments (EDs) in the United States; however, few studies have comprehensively examined this discrete patient population. We aim to identify utilization of EDs by patients with primary otologic complaints.
Study Design
Retrospective analysis of the Nationwide Emergency Department Sample (NEDS) from 2009 through 2011.
Methods
The NEDS database was queried for patient encounters with a primary otologic diagnosis based on ICD9 codes (380–389). Weighted estimates for demographic, diagnostic characteristics, SES, and trends over time were extracted. Predictors of mortality and admission were determined by multivariable logistic regression.
Results
A weighted total of 8,611,282 visits between 2009 and 2011 were attributed to otologic diagnoses, representing 2.21% of all ED visits. Stratified by patient age, otologic diagnoses encompassed 1.01% and 6.79% of all adult and pediatric ED visits, respectively. The majority of patients were treated and released (98.17%). The average age of patients presenting with an otologic complaint was 17.9 years (Standard Error [SE] = 0.23). Overall, 62.7% of patients that presented with an otologic complaint were 0–17 years old. The most common diagnoses among all age groups included otitis media NOS (60.6%), infected otitis externa NOS (11.8%), and otalgia NOS (6.8%).
Conclusions
We provide a comprehensive overview of otologic complaints that are an overlooked diagnostic category in public health research. NEDS data demonstrates significant number of visits related to otologic complaints, especially in the pediatric population, that are non-emergent.
Keywords: otology, emergency department, specialized emergency care, resource utilization
Introduction
Emergency Departments (ED) in the United States are overcrowded1, and patients with acute complaints may result in long wait times and inferior outcomes2–5. Otologic complaints, in particular, are commonly treated in the ED setting. According to the National Hospital Ambulatory Medical Care Survey, over 2 million patients were seen in an ED for otitis media and Eustachian tube disorders in 2010 alone.6 Other major otologic complaints evaluated in the ED include dizziness and vertigo,7–16 as well as generalized ear pain.17,18
The Patient Protection and Affordable Care Act aims to insure a greater number of Americans. This influx in new patients seeking care will likely contribute to additional strain on emergency departments, emergency health care providers, as well as affiliated specialists and ancillary staff.19 Solutions to meeting increased patient demands hinge on providing access to care while maintaining high quality outcomes and minimizing cost. As otologic complaints may encompass a sizable portion of ED complaints, it is vital to understand the scope of otologic diagnoses in the nation’s emergency health care safety net. For more complex or urgent otologic complaints, a team of ED physicians, neurologists, otolaryngologists, radiologists, and audiologists may be needed for diagnosis and treatment. Primary care providers are also crucial for follow-up care of otologic complaints. Although not all patients presenting to the ED with otologic complaints will require complex management, it is vital for both providers and payers to understand the extent of otologic disease evaluated in the ED setting to help shape future policy decisions and ensure proper care of patients.
An accurate assessment of otologic diagnoses can help guide triage, risk stratification, resource allocation from the perspective of EDs, as well as provider training and allocation of specialty personnel. Herein, we report estimates for the prevalence and incidence of primary otologic complaints in children and adults using the largest publically available ED database in the United States. We provide detailed analysis of patient demographics, including socioeconomic status, predictors of inpatient admission, charge data, as well as geocoding analysis to depict variation in diagnostic patterns across the United States over a three-year period (2009–2011).
Methodology
This study was approved by the Massachusetts Eye and Ear Infirmary Institutional Review Board. The 2009–2011 Nationwide Emergency Department Sample (NEDS), published by the Healthcare Cost and Utilization Project (HCUP) and sponsored by the Agency for Healthcare Research and Quality (AHRQ), was used to estimate the national prevalence and incidence of otologic diagnoses. NEDS is the largest publically available, all-payer ED database in the United States. It contains discharge abstracts for 86,866,759 ED visits at 951 hospitals in 30 states and provides a twenty percent stratified sample of all hospital-based EDs in the country between 2009 and 2011. Individual ED encounters can be weighted according to the sample design, therefore the 2009–2011 NEDS provides a national weighted sample of over 388 million ED visits. In NEDS, all diagnostic and therapeutic procedures are recorded using ICD-9CM procedure codes. Diseases of the ear and mastoid process (ICD9CM 380–389) listed in the first diagnostic position were included in our analysis.
Descriptive analysis was performed to characterize patient demographics (age, race, gender, national quartile for median household income [as categorized by HCUP according to patient zip code data], and insurance payer), visit characteristics (day of week and month), and hospital characteristics (teaching status, trauma designation, and geographic region). The ten most frequent diagnoses were tabulated. NEDS is a stratified two-stage cluster sample; therefore discharge weights and standard formulas for a two-stage cluster sample were used to generate national estimates and calculate standard errors.
Patient demographics, visit, injury, and hospital characteristics were compared by patient disposition (admission vs. treatment and release) in bivariable analysis. Differences in proportions and means were assessed using sample design-adjusted statistical tests including the Wald Chi-Square test (for proportions) and two-sided unpaired T-tests (for means).
Significant predictors of admission and mortality were determined in separate multivariable logistic regression models. Complex survey sample design was accounted for in the regression analysis. Each model was inclusive of all independent variables previously listed (patient demographics, visit characteristics, hospital characteristics and injury characteristics) in order to account for all potential predictors available in NEDS. Statistical significance was determined by a type I error threshold of 0.05. Data linkages and statistical analysis were performed using SAS v.9.3 (SAS Institute, Cary, NC).
Results
Emergency Department Visits for Otologic Complaints
There was a weighted total of 388,904,009 ED visits in 2009–2011. A total of 8,611,282 visits were attributed to a primary otologic diagnosis, which represents 2.21% of all ED visits. The annual volume of otologic visits was stable during the study period; there were 2,946,080 visits in 2009, 2,794,345 visits in 2010 and 2,870,857 visits in 2011. There were 921 visits per 100,000 population in 2011. Stratified by patient age, otologic diagnoses encompassed 1.01% and 6.79% of all adult and pediatric emergency department encounters, respectively. All values listed hereafter in the text and tables represent weighted estimates. The majority of patients were treated and released (n=8,453,260, 98.17%) compared to admitted to the hospital (n=157,876, 1.83%). An exceedingly low number of patients died in the ED or hospital (n=219, 0.0025%).
Patient Demographics
Demographic statistics are outlined in Table 1. In summary, patients with primary otologic complaints were on average 17.9 years old (Standard Error [SE] = 0.23). Overall, 62.7% of patients that presented with an otologic complaint were 0–17 years old and a slightly greater proportion was women (52.1%). Patients with lower income (<$39,000, 34.5%) and living in large central metropolitan areas (26.0%) presented more commonly than those with higher income or those living in small metropolitan areas. The major insurance providers were Medicaid (46.7%) and private insurance (28.9%). The majority of complaints presented at a non-trauma or level III hospital (76.2%).
Table 1.
Characteristics of ED encounters for primary otologic diagnosis, stratified by admission versus treatment and release (2009 to 2011).
| Weighted Frequency, %† (Standard Error) | ||||
|---|---|---|---|---|
| Variable | Total (N=8,611,282) |
Admitted* (N=157,876) |
Treated & Released (N=8,453,260) | P-Value** |
| Age category: | <0.0001 | |||
| 0–17 | 62.7% (0.5) | 15.4% (1.5) | 63.6% (0.5) | |
| 18–44 | 23.4% (0.3) | 12.1% (0.5) | 23.6% (0.3) | |
| 45–64 | 9.2% (0.2) | 25.7% (0.6) | 8.9% (0.2) | |
| >65 | 4.7% (0.1) | 46.9% (1.3) | 4.0% (0.1) | |
| Male gender | 47.9% (0.1) | 39.9% (0.4) | 48.0% (0.1) | <0.0001 |
| Year: | 0.5719 | |||
| 2009 | 34.2% (1.0) | 35.6% (2.1) | 34.2% (1.0) | |
| 2010 | 32.5% (1.0) | 33.3% (1.9) | 33.3% (1.0) | |
| 2011 | 33.3% (1.0) | 31.2% (1.5) | 32.5% (1.0) | |
| Patient’s residence: | <0.0001 | |||
| Large central, metropolitan | 26.0% (1.1) | 34.3% (1.8) | 25.9% (1.1) | |
| Large fringe, metropolitan | 20.6% (1.0) | 27.3% (1.4) | 20.5% (1.0) | |
| Medium metropolitan | 21.5% (1.0) | 16.2% (1.0) | 21.6% (1.0) | |
| Small metropolitan | 9.9% (0.7) | 9.2% (1.8) | 10.0% (0.7) | |
| Micropolitan | 13.3% (0.5) | 8.3% (0.5) | 13.4% (0.5) | |
| Other | 8.7% (0.3) | 4.8% (0.3) | 8.7% (0.3) | |
| Median household income: | <0.0001 | |||
| $1–$38,999 | 34.5% (0.8) | 24.3% (1.1) | 34.7% (0.9) | |
| $39,000–$47,999 | 30.2% (0.7) | 26.5% (1.6) | 30.3% (0.7) | |
| $48,000–$63,999 | 21.9% (0.6) | 25.2% (0.7) | 21.8% (0.6) | |
| $64,000 or more | 13.4% (0.5) | 24.1% (1.1) | 13.2% (0.5) | |
| Primary payer: | <0.0001 | |||
| Medicaid | 46.7% (0.6) | 15.8% (0.8) | 47.2% (0.6) | |
| Private Insurance | 28.9% (0.5) | 28.5% (1.1) | 28.9% (0.5) | |
| Self-pay | 14.0% (0.2) | 5.1% (0.3) | 14.2% (0.2) | |
| Medicare | 6.3% (0.1) | 47.3% (1.3) | 5.6% (0.1) | |
| Other | 3.6% (0.2) | 2.7% (0.3) | 3.6% (0.2) | |
| No charge | 0.5% (0.1) | 0.6% (0.1) | 0.5% (0.1) | |
| Weekend visit (Sat or Sun) | 33.2% (0.1) | 28.4% (0.3) | 33.3% (0.1) | <0.0001 |
| Injury diagnosis‡ (vs. non-injury) | 1.1% (0.02) | 3.3% (0.1) | 1.0% (0.1) | <0.0001 |
| Hospital trauma designation: | 0.0104 | |||
| Trauma level I or II | 23.8% (1.0) | 27.3% (1.4) | 23.7% (1.0) | |
| Non trauma or level III | 76.2% (1.0) | 72.7% (1.4) | 76.3% (1.0) | |
| Hospital teaching status: | <0.0001 | |||
| Non-teaching, Metropolitan | 42.5% (1.0) | 46.7% (1.9) | 42.4% (1.0) | |
| Teaching, Metropolitan | 35.9% (1.1) | 42.2% (1.7) | 35.8% (1.1) | |
| Non-metropolitan | 21.5% (0.6) | 11.1% (0.7) | 21.7% (0.6) | |
Some variables may not add to 100% due to missing data.
Denotes injury-related diagnosis in the first or second diagnostic position in NEDS.
Admission data missing for 29 patients.
P-value denotes level of significance for comparison between admitted and discharged patients.
For independent variables with mutually exclusive categories, P-value denotes results of a chi-square test of independence.
Common Otologic Complaints for Patients Discharged the Same Day
The ten most common diagnoses made in the ED among all patients with a primary otologic complaint are listed in Table 2. The most common diagnoses among all age groups included otitis media NOS (60.6%), infected otitis externa NOS (11.8%), and otalgia NOS (6.8%). Other notable diagnoses included impacted cerumen (3.6%) and peripheral vertigo (0.9%). In terms of pediatric versus adult patients, the most common diagnoses for pediatric age group were suppurative or unspecified otitis media (82.1%) followed by disorders of the external ear (9.0%) and other disorders of the ear (5.5%). In contrast, the most common diagnoses for adult patients were more evenly distributed with suppurative or unspecified otitis media (32.4%) being most common followed by disorders of the external ear (28.8%), vertiginous syndromes (19.1%), and other disorders of the ear (12.3%). (Table 5)
Table 2.
List of 10 most common otologic diagnoses made in emergency departments (2009–2011) among all patients with a primary otologic complaint.
| All Patients | Percentage (SE) | Admitted Patients | Percentage (SE) |
|---|---|---|---|
| Otitis Media NOS (382.9) | 60.6 (0.5) | Benign Paroxysmal Vertigo (386.11) | 33.3 (1.0) |
| Infected Otitis Externa NOS (380.10) | 11.8 (0.1) | Labyrinthitis NOS (386.30) | 12.1 (0.4) |
| Otalgia NOS (388.70) | 6.8 (0.2) | Otitis Media NOS (382.9) | 11.5 (1.3) |
| Impacted Cerumen (380.4) | 3.6 (0.1) | Vestibular Neuronitis (386.12) | 8.1 (0.4) |
| Benign Paroxysmal Vertigo (386.11) | 3.2 (0.1) | Infected Otitis Externa NOS (380.10) | 7.3 (0.2) |
| Acute Suppurative Otitis Media NOS (382.00) | 2.6 (0.4) | Peripheral Vertigo NOS (386.10) | 3.1 (0.2) |
| Labyrinthitis NOS (386.30) | 1.9 (0.1) | Acute mastoiditis without complication (383.00) | 2.8 (0.1) |
| Nonsuppurative Otitis Media NOS (381.4) | 1.2 (0.1) | Mastoiditis NOS (383.9) | 2.6 (0.1) |
| Peripheral Vertigo NOS (386.10) | 0.9 (0.1) | Meniere’s Disease NOS (386.00) | 2.6 (0.1) |
| Acute Serous Otitis Media (381.01) | 0.8 (0.1) | Viral labyrinthitis (386.35) | 2.2 (0.1) |
NOS=not otherwise specified.
Table 5. Variation in total charges for ED services for otologic diagnoses.
Mean ED Charge (09–11): $793.35 (SE 11.77)
| All Patients | Mean Charge (SE) |
|---|---|
| Otalgia NOS (388.70) | $584.74 (11.06) |
| Nonsuppurative Otitis Media NOS (381.4) | $598.64 (14.57) |
| Impacted Cerumen (380.4) | $607.96 (10.06) |
| Acute Suppurative Otitis Media NOS (382.00) | $650.09 (37.57) |
| Otitis Media NOS (382.9) | $622.29 (9.41) |
| Acute Serous Otitis Media (381.01) | $661.76 (24.86) |
| Infected Otitis Externa NOS (380.10) | $648.23 (8.83) |
| Labyrinthitis NOS (386.30) | $2694.17 (47.42) |
| Peripheral Vertigo NOS (386.10) | $2902.93 (104.36) |
| Benign Paroxysmal Vertigo (386.11) | $3123.68 (69.91) |
Timing and Geographic Distribution of Otologic Complaints
Patients typically presented during weekdays (66.8%) versus weekends (32.2%). Patients presented commonly throughout the year without significant variation in month of presentation (peak: January 9.1%, trough: September 6.9%). (Figure 1) Certain diagnoses, such as otitis externa and otitis media demonstrated seasonal variation. (Figure 2.) Geographically, ED visits for otologic complaints occurred most commonly in the South (39.4%), followed by the Midwest (25.2%), Northwest (18.0%), and West (17.3%). (Figure 3.)
Figure 1.
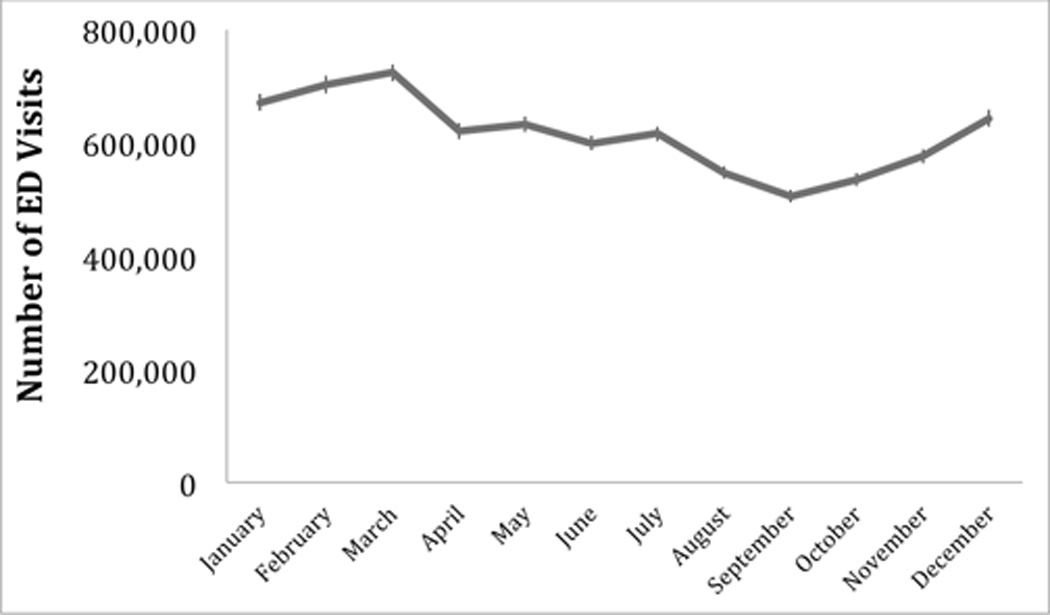
Monthly variation in volume of primary otologic-related visits to hospital-based emergency departments in the United States (2009 to 2011).
*Error bars denote standard deviation of weighted frequency.
Figure 2.
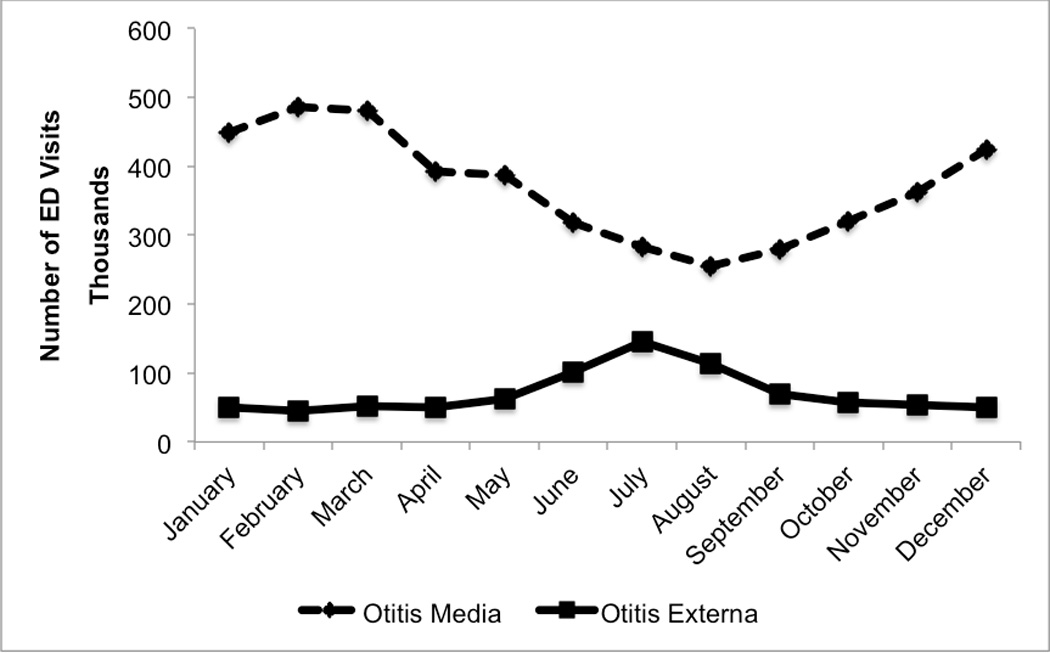
Monthly variation in primary diagnoses of otitis media and otitis externa in hospital-based emergency departments in the United States (2009–2011).
Figure 3.
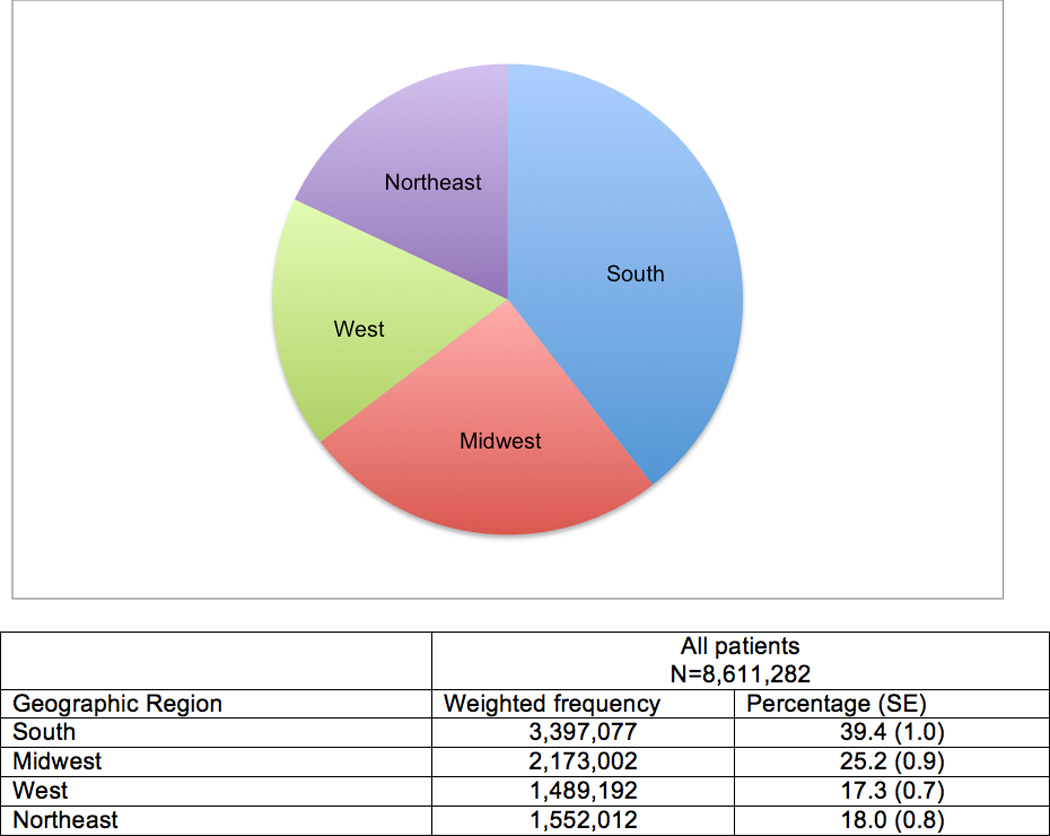
National weighted estimates for incidence of primary otologic visits to hospital-based EDs by census-defined regions of the United States (2009–2011).
Admission to the Hospital
Of otologic diagnoses resulting in admission, the most common diagnoses included benign paroxysmal vertigo (33.3%), labyrinthitis (12.1%), otitis media NOS (11.5%), and vestibular neuronitis (8.1%). (Table 2) Bivariable comparisons for patient demographics and visit characteristics for patients that were admitted versus patients who were treated and released are presented in Table 1. Of note, older patients (>65 years old, 46.9%) were more likely to be admitted. Patients in a larger metropolitan area and those with Medicare were also more likely to be admitted. Several predictors of inpatient admission were identified in multivariable logistic regression modeling. A notable demographic predictor of admission included patient's residence in a large central metropolitan area (OR 1.35, CI=1.04–1.76). Patients less likely to be admitted included lower median household income (<$39,000, OR 0.78, CI 0.65–0.92). Specific diagnoses that predicted admission included mastoiditis and related conditions (OR 81.50, CI 81.50–144.56) and vertiginous symptoms (OR 16.07, CI 12.14 – 21.27). (Table 3)
Table 3.
Multivariable analysis of demographics predicting patient disposition outcomes for patients with primary otologic injuries.
| Admission | |||
|---|---|---|---|
| Variable | OR | 95% CI* | P-value |
| Male gender | 1.04 | 1.01–1.08 | 0.0137 |
| Age (per 1 additional year) | 1.03 | 1.02–1.03 | <0.0001 |
| Age Category | |||
| 0–17 | REF | ||
| 18–44 | 0.43 | 0.36–0.51 | <0.0001 |
| 45–64 | 0.58 | 0.48–0.69 | <0.0001 |
| >65 | 0.57 | 0.46–0.71 | <0.0001 |
| Patient’s residence | |||
| Large central, metropolitan | 1.35 | 1.04–1.76 | 0.0265 |
| Large fringe, metropolitan | 1.08 | 0.85–1.34 | 0.5474 |
| Medium, metropolitan | 0.70 | 0.57–0.86 | 0.0006 |
| Small, metropolitan | 1.07 | 0.70–1.63 | 0.7660 |
| Micropolitan | 1.16 | 0.96–1.40 | 0.1313 |
| Other | REF | ||
| Insurance: | |||
| Private insurance | 0.67 | 0.61–0.74 | <0.0001 |
| Medicaid | 0.62 | 0.52–0.73 | <0.0001 |
| Medicare | REF | ||
| Self-pay | 0.34 | 0.30–0.39 | <0.0001 |
| Other | 0.78 | 0.59–1.04 | 0.4116 |
| No charge | 0.84 | 0.56–1.27 | 0.0904 |
| Median household income: | |||
| $1–$38,999 | 0.78 | 0.65–0.92 | 0.0359 |
| $39,000–$47,999 | 0.85 | 0.73–1.00 | 0.6313 |
| $48,000–$63,999 | 0.89 | 0.81–1.00 | 0.5728 |
| $64,000 or more | REF | ||
| Weekend | 1.05 | 1.01–1.09 | 0.0067 |
| Admission month | NA | NA | 0.0075 |
| Geographic region | |||
| Northeast | 1.88 | 1.51–2.34 | 0.0004 |
| Midwest | 1.81 | 1.28–2.57 | 0.0873 |
| South | 1.45 | 1.18–1.78 | 0.6488 |
| West | REF | ||
| Hospital Teaching Status | |||
| Non-teaching, metropolitan | 2.34 | 1.71–3.20 | 0.003 |
| Teaching, metropolitan | 2.38 | 1.81–3.13 | <0.0001 |
| Non-metropolitan | REF | ||
| Trauma I or II (vs. III/NT) | 1.07 | 0.86–1.34 | |
| Non-injury related visit (vs. injury related visit) | 0.42 | 0.38–0.47 | <0.0001 |
| Diagnosis | OR | 95% CI* | P-value |
| Disorders of the external ear | 2.00 | 1.63–2.45 | <0.0001 |
| Hearing loss | 1.60 | 0.96–2.68 | 0.0731 |
| Mastoiditis and related conditions | 108.55 | 81.50–144.56 | <0.0001 |
| Non-suppurative otitis media and Eustachian tube disorders | 1.61 | 1.34–1.94 | <0.0001 |
| Other disorders of the ear | 0.97 | 0.86–1.09 | 0.5861 |
| Other disorders of the middle ear and mastoid | 8.25 | 5.52–12.34 | <0.0001 |
| Other disorders of the tympanic membrane | 0.89 | 0.60–1.31 | 0.5431 |
| Otosclerosis | 5.56 | 1.09–28.28 | 0.0386 |
| Vertiginous symptoms and other disorders of the vestibular system | 16.07 | 12.14–21.27 | <0.0001 |
CI = confidence interval,
REF=Reference, NT=Non-trauma, ED=emergency department,
N/A = not applicable
Charge Data for Otologic Diagnoses
The mean charge for diagnosis and treatment of an otologic complaint in the ED was $793.35 (SE 11.77). Common diagnoses included otitis media NOS (ICD-9CM 382.9) at $622.29 (SE=9.41) and infected otitis externa NOS (ICD-9CM 380.10) at $648.23 (SE=8.83). The most expensive diagnoses included inactive Meniere’s disease (ICD-9CM 386.04) at $5343.84 (SE=146.66) and bilateral sensorineural hearing loss (ICD9-CM 389.18) at $5343.84 (SE=146.66). (Table 5)
Discussion
Few studies have investigated the burden of otologic complaints at a national level beyond individual diagnoses, especially in the ED setting. We provide a contemporary overview of otologic complaints that are a commonly treated, but often-overlooked diagnostic category in public health research and policy. In addition to emergency department providers, the wide array of other health care providers (e.g., internists, pediatricians, neurologists, otolaryngologists, radiologists, and audiologists) that treat otologic complaints adds to the fractured nature of such epidemiological research. Two themes permeate investigation of otologic visits in the ED: 1) the significant number of otologic-related visits in the pediatric and adult population and 2) the high proportion of non-urgent otologic diagnoses evaluated in EDs.
From 2009–2011, primary otologic complaints encompass over 8 million ED visits in the United States. Strikingly, in the pediatric patient population, 6.79% of all ED visits were due to otologic diagnoses. NEDS data demonstrate that the majority of patients (62.7%) presenting with otologic complaints are patients under the age of 18, and relatively few patients over the age of 65 (4.7%) present with otologic complaints. Further, the most common diagnoses differ between adults and pediatric patients. Whereas adults typically present with a more evenly distribution of otologic diagnoses, including otitis media (32.4%) and vertiginous syndromes (19.1%), pediatric patients predominantly present with otitis media (82.1%). The charges of these visits range from several hundred to several thousand dollars and do not include charges associated with inpatient status.
Data from NEDS and HCUP further illustrate the significant number of non-urgent otologic diagnoses in EDs. The majority (98.17%) of patients that are evaluated in the ED for an otologic complaint are discharged home. Not surprisingly, older patients were more frequently admitted. Patients with Medicaid and self-pay were less likely to be admitted. Interestingly, among the most frequently admitted patients included patients with vertiginous diagnoses, such as benign paroxysmal vertigo (BPV), which is not an otologic emergency and traditionally does not require inpatient status.8,13,14,20,21 The significant number of admitted patients identified in the database with a diagnosis of BPV may reflect several concurrent issues, such as the final diagnosis after an inpatient evaluation to exclude other potentially serious causes of vertigo or unfamiliarity with vertiginous disorders. Indeed, the significant number of patients admitted with a diagnosis of BPV is an ideal patient population to examine for potential cost savings, as BPV can be readily diagnosed and managed in an outpatient, non-ED setting. The diagnosis of BPV is based on history and physical exam findings, does not require imaging, and is not a diagnosis of exclusion. Improved understanding of BPV, among other otologic diagnoses, in the ED setting could potentially decrease the number of patients requiring admission for new onset vertigo. In contrast, there are clearly diagnoses that require inpatient status; these diagnoses are reflected in multivariable regression and include mastoiditis. (Table 3) Thus, there are patients being admitted that are both expected and unexpected. Improved understanding of emergent otologic symptoms at the time of presentation may enable cost savings by reserving admission for true otologic emergencies.18
Beyond the sheer volume of diagnoses, the obvious question from these data is why patients, especially pediatric patients with otitis media, are being evaluated in the ED. From a cost standpoint, primary care and outpatient settings may offer similar or higher quality care at a reduced price to the health care system, although this concept is currently debated.22–25 While this study was not geared to directly answer the question of access, patient presentation to the ED may to be related to patient education or difficulty obtaining immediate access to primary care providers and significant research has addressed patient decision making for visiting the ED versus outpatient setting for other diagnoses.26–28 Prior studies evaluating dedicated otolaryngology and ophthalmology EDs have also demonstrated that the majority of problems evaluated in an “emergency” setting are actually not true emergencies and these patients may place additional strain on the health care safety net.29–34 Moreover, as many otologic diagnoses are potentially due to an infectious etiology, there may be overuse (or incorrect use) of antibiotics.35,36
The abundance of otologic-related visits raises important issues regarding training, staffing, and hospital-based resource allocation. EDs should remain prepared for a spectrum of otologic complaints. Increased otologic-specific training at both the provider and nursing level may be necessary. A wide range of evidence-based guidelines for common otologic complaints, currently applied to patient treatment in the outpatient setting, may be incorporated into ED-based care.37–40 High admission rates for workup of potentially non-emergent complaints, such as BPV, raises concerns about diagnosis and treatment.
In addition, there is a possibility that some otologic conditions are being under recognized and potentially undertreated. One emergent complaint, sudden hearing loss, (ICD9-CM 388.2) that can be treated with oral or intratympanic steroids if recognized early, was only diagnosed 730 times over a three-year period in our study. (Data not shown.) Estimates of sudden hearing loss are typically much higher (incidence of approximately 1:10,000 per year), suggesting that emergency providers may be missing opportunities to intervene in true otologic emergencies.41
Moreover, new triage mechanisms may be utilized to best manage patients. For example, the Institute of Medicine Committee on the Future of Emergency Care recommends the development of a regionalized system of emergency care to increase access to specialty care.42 In a regionalized system, hospitals, emergency care providers and administrators coordinate specialist expertise to allocate resources. The regionalized system of ED care is currently in development, and examples of this new model include treatment of cardiac arrest and stroke, as well as management of pediatric patients.42 While most otologic complaints do not require rapid evaluation and treatment, the concept of a regionalized system for triage of particular complaints may also be applied to more common diagnoses and provide an additional mechanism to decrease non-urgent complaints in EDs. Previous reports have demonstrated the potential for urgent care or retail clinics43, or even subspecialty EDs29 adjacent to standard EDs that may be able to provide rapid access to specialists.
There are several limitations to this study. First, we attempted to look only at primary otologic complaints; thus, this study may underestimate otologic diagnoses that are associated with other presentations that may contain a different primary diagnostic code. Second, as with all large, retrospective database studies, this study is limited in its ability to account for unknown confounders. Finally, discharge abstracts are interpreted and coded by independent reviewers and are subject to their individual biases.
Taken together, a significant number of patients visit EDs with a primary otologic complaint. The majority of these patients, however, do not need emergent care and could be managed appropriately in an outpatient setting. Although beyond the scope of this report, access to urgent care clinics or specialists may decrease the need for ED visits. Urgent clinics, subspecialized emergency rooms or “fast tracks” may provide rapid access to specialty care that could be staffed with providers with additional otologic training.
Conclusion
We provide a contemporary epidemiological evaluation of otologic complaints in EDs in the United States. Our study demonstrates significant number of visits related to otologic complaints, especially in the pediatric population, that are non-emergent in nature. This study has implications for otologic patient triage, risk stratification, as well as resource allocation from the perspectives of providers and hospitals.
Table 4.
Frequency of primary otologic diagnosis categories by age group.
| Diagnostic Category | Pediatric N=5,484,720 Percentage (SE) |
Adult N=3,126,562 Percentage (SE) |
P-value |
|---|---|---|---|
| Suppurative and unspecified otitis media | 82.1% (0.3) | 32.4% (0.3) | <0.0001 |
| Disorders of the external ear | 9.0% (0.1) | 28.8% (0.3) | |
| Other disorders of the ear | 5.5% (0.1) | 12.3% (0.2) | |
| Vertiginous syndromes and other disorders of the vestibular system | 0.2% (0.001) | 19.1% (0.3) | |
| Non-suppurative otitis media and Eustachian tube disorders | 2.5% (0.1) | 4.3% (0.1) | |
| Other disorders of the tympanic membrane | 0.6% (0.01) | 1.5% (0.03) | |
| Mastoiditis and related conditions | 0.1% (0.01) | 0.6% (0.01) | |
| Hearing loss | 0.04% (0.002) | 0.7% (0.1) | |
| Other disorders of the middle ear and mastoid | 0.05% (0.01) | 0.1% (0.01) | |
| Otosclerosis | 0.002% (0.0004) | 0.006% (0.002) |
Acknowledgements
We would like to thank Louise Collins of The LeRoy A. Schall Library of Otolaryngology for her support in preparation of this manuscript.
Footnotes
Conflict of Interest: None
Financial Disclosures: None
References
- 1.Institute of Medicine. At the breaking point. Washtington, DC: National Academies Press; 2006. Hospital-based emergency care. [Google Scholar]
- 2.Johnson K, Winkelman C. The Effect of Emergency Department Crowding on Patient Outcomes. Advanced Emergency Nursing Journal. 2011;33:39–54. doi: 10.1097/TME.0b013e318207e86a. [DOI] [PubMed] [Google Scholar]
- 3.Richardson D. Increase in patient mortality at 10 days associated with emergency department overcrowding. MJA. 2006;184:213–216. doi: 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 4.Pines JM, Iyer S, Disbot M, Hollander JE, Shofer FS, Datner EM. The Effect of Emergency Department Crowding on Patient Satisfaction for Admitted Patients. Academic Emergency Medicine. 2008;15:825–831. doi: 10.1111/j.1553-2712.2008.00200.x. [DOI] [PubMed] [Google Scholar]
- 5.Pines JM, Pollack CV, Jr, Diercks DB, Chang AM, Shofer FS, Hollander JE. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2009;16:617–625. doi: 10.1111/j.1553-2712.2009.00456.x. [DOI] [PubMed] [Google Scholar]
- 6.Kalson NS, Dunn KW. Contribution to national acute injury and intensive care audit databases in England and Wales. Emergency medicine journal : EMJ. 2011;28:538. doi: 10.1136/emj.2010.109363. [DOI] [PubMed] [Google Scholar]
- 7.Ahsan SF, Syamal MN, Yaremchuk K, Peterson E, Seidman M. The costs and utility of imaging in evaluating dizzy patients in the emergency room. The Laryngoscope. 2013;123:2250–2253. doi: 10.1002/lary.23798. [DOI] [PubMed] [Google Scholar]
- 8.Bashir K, Alessai GS, Salem WA, Irfan FB, Cameron PA. Physical maneuvers: effective but underutilized treatment of benign paroxysmal positional vertigo in the ED. The American journal of emergency medicine. 2014;32:95–96. doi: 10.1016/j.ajem.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Burmeister D, Sacco R, Rupp V. Management of Benign Paroxysmal Positional Vertigo With the Canalith Repositioning Maneuver in the Emergency Department Setting. JAOA. 2010;110:602–604. [PubMed] [Google Scholar]
- 10.Kerber KA, Morgenstern LB, Meurer WJ, et al. Nystagmus assessments documented by emergency physicians in acute dizziness presentations: a target for decision support? Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18:619–626. doi: 10.1111/j.1553-2712.2011.01093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozono Y, Kitahara T, Fukushima M, et al. Differential diagnosis of vertigo and dizziness in the emergency department. Acta oto-laryngologica. 2014;134:140–145. doi: 10.3109/00016489.2013.832377. [DOI] [PubMed] [Google Scholar]
- 12.Saber Tehrani AS, Coughlan D, Hsieh YH, et al. Rising annual costs of dizziness presentations to U.S. emergency departments. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2013;20:689–696. doi: 10.1111/acem.12168. [DOI] [PubMed] [Google Scholar]
- 13.Chase M, Joyce NR, Carney E, et al. ED patients with vertigo: can we identify clinical factors associated with acute stroke? The American journal of emergency medicine. 2012;30:587–591. doi: 10.1016/j.ajem.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Kerber KA. Vertigo and dizziness in the emergency department. Emergency medicine clinics of North America. 2009;27:39–50. viii. doi: 10.1016/j.emc.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawhn-Heath C, Buckle C, Christoforidis G, Straus C. Utility of head CT in the evaluation of vertigo/dizziness in the emergency department. Emergency radiology. 2013;20:45–49. doi: 10.1007/s10140-012-1071-y. [DOI] [PubMed] [Google Scholar]
- 16.Lo AX, Harada CN. Geriatric dizziness: evolving diagnostic and therapeutic approaches for the emergency department. Clinics in geriatric medicine. 2013;29:181–204. doi: 10.1016/j.cger.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Conover K. Earache. Emergency medicine clinics of North America. 2013;31:413–442. doi: 10.1016/j.emc.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 18.McWilliams B, Jacobson R, Van Houten H, Naessens J, Ytterberg K. A Program of Anticipatory Guidance for the Prevention of Emergency Department Visits for Ear Pain. Arch Pediatr Adoles. 2008;162:151–156. doi: 10.1001/archpediatrics.2007.30. [DOI] [PubMed] [Google Scholar]
- 19.Reger C, Kennedy DW. Changing practice models in otolaryngology-head and neck surgery: the role for collaborative practice. Otolaryngol Head Neck Surg. 2009;141:670–673. doi: 10.1016/j.otohns.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Kentala E, Rauch SD. A practical assessment algorithm for diagnosis of dizziness. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2003;128:54–59. doi: 10.1067/mhn.2003.47. [DOI] [PubMed] [Google Scholar]
- 21.Chang AK, Schoeman G, Hill M. A randomized clinical trial to assess the efficacy of the Epley maneuver in the treatment of acute benign positional vertigo. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2004;11:918–924. doi: 10.1197/j.aem.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Soni A. Statistical Brief: #228. Ear Infections (Otitis Media) in Children (0–17): Use and Expenditures, 2006. Medical Expenditure Panel Survey. 2008:1–5. [Google Scholar]
- 23.Baker LC, Baker LS. Excess cost of emergency department visits for nonurgent care. Health affairs. 1994;13:162–171. doi: 10.1377/hlthaff.13.5.162. [DOI] [PubMed] [Google Scholar]
- 24.Thygeson M, Van Vorst KA, Maciosek MV, Solberg L. Use and costs of care in retail clinics versus traditional care sites. Health affairs. 2008;27:1283–1292. doi: 10.1377/hlthaff.27.5.1283. [DOI] [PubMed] [Google Scholar]
- 25.Mehrotra A, Liu H, Adams J, et al. Comparing Costs and Quality of Care at Retail Clinics With That of Other Medical Settings for 3 Common Illnesses. Ann of Internal Medicine. 2009;151:322–329. doi: 10.7326/0003-4819-151-5-200909010-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency Department Visits for Nonurgent Conditions: Systematic Literature Review. American Journal of Managed Care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 27.Young G, Wagner M, Kellermann A, Ellis J, Bouley D. Ambulatory Vists to Hospital Emergency Departments. Jama. 1996;276:460–465. doi: 10.1001/jama.276.6.460. [DOI] [PubMed] [Google Scholar]
- 28.Berry A, Brousseau D, Brotanek J, Tomany-Korman S, Glores G. Why Do Parents Bring Children to the Emergency Department for Nonurgent Conditions? A Qualitative Study. Ambulatory Pediatrics. 2008;8:360–367. doi: 10.1016/j.ambp.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Sethi R, Kozin E, Remenschneider A, et al. Subspecialty Emergency Room as Alternative Model for Otolaryngologic Care: Implications for Emergency Health Care Delivery. American Journal of Otolaryngology. 2014 doi: 10.1016/j.amjoto.2014.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andrade JS, Albuquerque AM, Matos RC, Godofredo VR, Penido Nde O. Profile of otorhinolaryngology emergency unit care in a high complexity public hospital. Brazilian journal of otorhinolaryngology. 2013;79:312–316. doi: 10.5935/1808-8694.20130056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saha S, Chandra S, Mondal PK, et al. Emergency Otorhinolaryngolocal cases in Medical College, Kolkata-A statistical analysis. Indian J Otolaryngol Head Neck Surg. 2005;57:219–225. doi: 10.1007/BF03008018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Timsit CA, Bouchene K, Olfatpour B, Herman P, Tran Ba Huy P. Epidemiology and clinical findings in 20,563 patients attending the Lariboisiere Hospital ENT Adult Emergency Clinic. Ann Otolaryngol Chir Cervicofac. 2001;118:215–224. [PubMed] [Google Scholar]
- 33.Vasileiou I, Giannopoulos A, Klonaris C, et al. The potential role of primary care in the management of common ear, nose or throat disorders presenting to the emergency department in Greece. Quality in primary care. 2009;17:145–148. [PubMed] [Google Scholar]
- 34.Schull MJ, Kiss A, Szalai JP. The effect of low-complexity patients on emergency department waiting times. Annals of emergency medicine. 2007;49:257–264. 264–e251. doi: 10.1016/j.annemergmed.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 35.Collier SA, Hlavsa MC, Piercefield EW, Beach MJ. Antimicrobial and analgesic prescribing patterns for acute otitis externa, 2004–2010. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2013;148:128–134. doi: 10.1177/0194599812467000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fischer T, Singer AJ, Lee C, Thode HC., Jr National trends in emergency department antibiotic prescribing for children with acute otitis media, 1996 2005. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007;14:1172–1175. doi: 10.1197/j.aem.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 37.Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131:e964–e999. doi: 10.1542/peds.2012-3488. [DOI] [PubMed] [Google Scholar]
- 38.Roland PS, Smith TL, Schwartz SR, et al. Clinical practice guideline: cerumen impaction. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2008;139:S1–S21. doi: 10.1016/j.otohns.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 39.Bhattacharyya N, Baugh RF, Orvidas L, et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2008;139:S47–S81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 40.Rosenfeld RM, Schwartz SR, Cannon CR, et al. Clinical practice guideline: acute otitis externa. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2014;150:S1–S24. doi: 10.1177/0194599813517083. [DOI] [PubMed] [Google Scholar]
- 41.Rauch S, Halpin C, Antonelli P, et al. Oral vs Intratympanic Corticosteroid Therapy for Idiopathic Sudden Sensorineural Hearing Loss A Randomized Trial. Jama. 2071;305:2071–2079. doi: 10.1001/jama.2011.679. [DOI] [PubMed] [Google Scholar]
- 42.Kellermann AL, Hsia RY, Yeh C, Morganti KG. Emergency care: then, now, and next. Health Aff (Millwood) 2013;32:2069–2074. doi: 10.1377/hlthaff.2013.0683. [DOI] [PubMed] [Google Scholar]
- 43.Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health affairs. 2010;29:1630–1636. doi: 10.1377/hlthaff.2009.0748. [DOI] [PMC free article] [PubMed] [Google Scholar]


