Abstract
Background
Existing literature demonstrating the negative impact of delayed hip fracture surgery on mortality consists largely of observational studies prone to selection bias and may overestimate the negative effects of delay. We conducted an intervention study to assess initiatives aimed at meeting a 48-hour benchmark for hip fracture surgery to determine if the intervention achieved a reduction in time to surgery, and if a general reduction in time to surgery improved mortality and length of stay.
Methods
We compared time to surgery, length of stay and mortality between pre- and postintervention patients with a hip fracture using the Kaplan–Meier estimator and Cox proportional hazards model adjusting for age, sex, comorbidities, type of surgery and year.
Results
We included 3525 pre- and 3007 postintervention patients aged 50 years or older. The proportion of patients receiving surgery within the benchmark increased from 66.8% to 84.6%, median length of stay decreased from 13.5 to 9.7 days, and crude in-hospital mortality decreased from 9.6% to 6.8% (all p < 0.001). Adjusted analyses revealed reduced mortality in hospital (hazard ratio [HR] 0.68, 95% confidence interval [CI] 0.57–0.81) and at 1 year (HR 0.87, 95%CI 0.79–0.96). Independent of the intervention period, having surgery within 48 hours demonstrated decreased adjusted risk of death in hospital (HR 0.51, 95%CI 0.41–0.63) and at 1 year postsurgery (HR 0.72, 95% CI 0.64–0.80).
Conclusion
Coordinated, region-wide efforts to improve timeliness of hip fracture surgery can successfully reduce time to surgery and appears to reduce length of stay and adjusted mortality in hospital and at 1 year.
Abstract
Contexte
La littérature actuelle qui démontre l’impact négatif d’un report de la chirurgie pour fracture de la hanche sur la mortalité repose en bonne partie sur des études d’observation sujettes à des biais de sélection et pourrait surestimer cet impact négatif. Nous avons réalisé une étude interventionnelle pour évaluer des mesures visant à faire respecter un délai maximum de 48 heures avant l’intervention pour fracture de la hanche afin de voir si elles avaient effectivement raccourci le délai avant la chirurgie et si l’abrègement général du délai avant la chirurgie avait réduit la mortalité et la durée du séjour hospitalier.
Méthodes
Nous avons comparé le délai avant la chirurgie, la durée du séjour hospitalier et la mortalité des patients victimes d’une fracture de la hanche avant et après l’imposition des mesures, à l’aide d’un estimateur de Kaplan–Meier et d’un modèle de risques proportionnels de Cox, en tenant compte de l’âge, du sexe, des comorbidités, du type de chirurgie et de l’année.
Résultats
Nous avons recruté respectivement 3525 et 3007 patients de 50 ans ou plus, avant et après l’imposition des mesures. La proportion de patients qui ont été opérés à l’intérieur du délai préconisé a augmenté de 66,8 % à 84,6 %, la durée médiane du séjour hospitalier a diminué de 13,5 à 9,7 jours et le taux brut de mortalité perhospitalière a diminué de 9,6 % à 6,8 % (tous, p < 0,001). Les analyses ajustées ont révélé une réduction de la mortalité perhospitalière (risque relatif [RR] 0,68, intervalle de confiance [IC] de 95 % 0,57–0,81) et à 1 an (RR 0,87, IC de 95 % 0,79–0,96). Indépendamment de la période (avant ou après l’imposition des mesures), le fait d’être opéré dans les 48 heures s’est accompagné d’une diminution du risque ajusté de mortalité en cours d’hospitalisation (RR = 0,51, IC de 95 % 0,41–0,63) et dans l’année suivant la chirurgie (RR 0,72, IC de 95 % 0,64–0,80).
Conclusion
Des efforts coordonnés à l’échelle des régions visant à accélérer l’accès à la chirurgie pour fracture de la hanche peuvent réduire avec succès le délai avant la chirurgie et abréger le séjour hospitalier, en plus de diminuer la mortalité ajustée en cours d’hospitalisation et après 1 an.
Every year, nearly 30 000 Canadians older than 50 years are admitted to hospital with an osteoporosis-related hip fracture.1 The incidence of hip fracture begins to rise at age 50 and peaks in the eighth decade of life, with the greatest proportion occurring in women.1,2 Following fracture, mortality ranges from 4% at 1 month3 to 33% at 1 year, with approximately 70% of deaths at 1 year attributed to the hip fracture.4 Thus, in Canada there are an estimated 7000 deaths related to hip fracture every year.
Unless there is decision to palliate, the principal treatment for hip fracture is surgery, using either internal fixation (IF) or total hip arthroplasty (THA) according to fracture pattern.5 The immediate goals of surgery include pain control, early mobilization and avoidance of further complications.6–8 In our health region, these surgical procedures were traditionally done after hours, competing with other acute and emergent surgical cases for operating theatre time, which frequently resulted in patients with hip fractures waiting several days for surgery9 despite longstanding concerns about the potential consequences of delay on postsurgical outcomes, including mortality.10,11
Efforts to reduce the morbidity and mortality associated with hip fracture have focused on 2 main areas: fracture prevention through falls reduction and osteoporosis treatment12 and improved timeliness of surgery.11 Acknowledging the risks associated with delayed hip fracture surgery, the 2004 Canadian First Ministers’ 10-Year Plan to Strengthen Health Care established the path toward evidence-based benchmarks and public reporting of wait times for hip fracture surgery.13 In 2005, this national benchmark was set at 48 hours from the time of patient admission to the time of surgery.14 Two years later, the Canadian Institute for Health Information (CIHI) released its national indicator report showing that only 65% of patients in Canada met the benchmark.9 This report also showed that Manitoba had the lowest percentage of patients receiving surgery within the benchmark (53%).9 Motivated by this report, in 2008 Manitoba Health and the Winnipeg Regional Health Authority (WRHA) undertook a multifaceted year-long initiative to improve the timeliness of surgery within the WRHA, culminating in a mandatory benchmark.
While many clinicians and administrators now accept that unnecessary delays in hip fracture surgery result in poorer outcomes, the current literature actually provides weak evidence for the association between timely surgery and decreased mortality because it comprises almost exclusively nonintervention, retrospective observational studies that compare patients who received timely surgery to those who did not.15,16 The findings are therefore susceptible to selection bias, as one would expect medically complicated patients to have their surgery delayed while they undergo preoperative investigations or treatments,17,18 thus tending to overestimate the risk of death associated with delayed surgery. Published prospective intervention studies are small and therefore underpowered to detect differences in mortality.19,20
The purpose of the present study was to determine if our improvement intervention achieved the intended reduction in time to surgery and if a reduction in time to surgery improved mortality and length of stay (LOS). We believe that this work is unique in that it is, to our knowledge, the first adequately powered intervention study that examines the association between timely hip fracture surgery and mortality.
Methods
Study design
We used a pre-/postintervention design using administrative data to compare time to surgery, length of stay and mortality in all patients admitted to our health region with a hip fracture between January 2004 and March 2012.
Patient population
Our preintervention group consisted of all patients aged 50 years or older who were admitted to hospitals in the WRHA with a hip fracture during the 48 months between Jan. 1, 2004, and Dec. 31, 2007, inclusive. Our postintervention group consisted of all hip fracture patients aged 50 years or older who were admitted during the 39 months between Jan. 1, 2009, and Mar. 31, 2012, inclusive. Patients admitted during the year the improvement initiative was being implemented (Jan. 1–Dec. 31, 2008) were excluded. We obtained clinical, demographic and administrative data from WRHA’s discharge abstract database (DAD) and mortality data from the provincial client registry database. Hip fracture diagnoses included were femoral neck, intertrochanteric and subtrochanteric fractures (ICD-10-CA codes: S72.010, S72.080, S72.081, S72.090, S72.091, S72.100, S72.101, S72.190, S72.200, & S72.900). To avoid possible bias from excluding patients who may have died while waiting for surgery, we included all patients with these fractures, not just those who underwent surgery.
Setting
The WRHA is Manitoba’s largest health authority, serving a large portion of the province’s population of 1.2 million people.21 It includes 2 tertiary hospitals, 4 community hospitals, 5 community health centres, personal care homes, community-based health facilities and a number of clinical and community programs. Canadian provinces each have a single-payer health care system that provides all necessary hospital, medical and surgical services; this characteristic allows for a population-based study of all hip fracture patients.
Intervention
In late 2007, our year-long improvement intervention began with a prospective audit of several hundred hip fracture patients by the WRHA surgical leadership and Orthopaedic Standards & Quality Committee. The audit revealed multiple sources of delay along the often convoluted care trajectory of these frail patients en route to surgery. Seven potential contributors to delay in delivery of surgical care were identified, against which actions were taken during the latter half of 2008 (Table 1).
Table 1.
Seven potential sources of delay to surgical repair of hip fracture identified during a WRHA audit in 2008 along with the actions taken to address sources of delay
| Potential sources of delay | Actions taken to address sources of delay |
|---|---|
| i) Time required to transfer patients from rural hospitals without surgical facilities to WRHA hospitals with surgical facilities | i) Development of an orthopedic surgery coverage algorithm that matched WRHA hospitals with rural hospitals and required WRHA hospitals to accept rural patients regardless of bed availability |
| ii) Routing rural patients through the receiving hospital’s emergency department rather than going directly to the surgical ward | ii) Direct transfer of patients from rural hospitals’ emergency departments to the surgical ward at the accepting hospital |
| iii) Availability of operating room time | iii) Creation of additional daytime orthopedic trauma slates to accommodate patients during regular working hours and clarification of prioritization rules so that hip fracture patients who are “bumped” from surgery one day receive high priority the next day |
| iv) Lack of uniform understanding among all care providers of the association between delayed time to surgery and outcome | iv) Education in the form of combined orthopedics, anesthesia and internal medicine rounds on the importance of timeliness of surgery and common reasons for delay |
| v) Lack of consensus between surgeons and anesthesiologists about the timing of surgery in patients on clopidogrel | v) A collaborative determination by the WRHA anesthesia and orthopedic standards committees that clopidogrel in and of itself need not delay surgery |
| vi) Mandatory internal medicine consultations in order to be cleared for surgery | vi) The use of internal medicine consultations only when a correctable serious medical condition was identified preoperatively (e.g., an uncontrolled arrhythmia or congestive heart failure) |
| vii) Difficulties repatriating patients to home hospitals after surgery, resulting in a functional bed shortage for new patients | vii) WRHA surgery program collaborated with rural health regions to improve repatriation of patients once fit for transfer following surgery |
WRHA = Winnipeg Regional Health Authority.
Study outcomes
We compared the pre- and postintervention groups based on the outcomes of time to surgery, LOS, in-hospital mortality and 1-year mortality. Time to surgery was defined as the interval between the time of hospital admission and time of surgery. Prior to 2008, 2 of the 6 hospital sites did not consistently capture the exact time of surgery, resulting in 1766 cases (50% of the preintervention group) with a date but not an exact time of surgery. For these cases, we used nonmissing surgery time data, stratified by weekday and weekend, to estimate the site’s missing data. We defined LOS as the time from hospital admission to discharge for the hip fracture stay, in-hospital mortality as a death associated with the hip fracture that occurred during the hospital stay, and 1-year mortality as death within 12 months of the index admission. We calculated the Charlson Comorbidity Index22,23 using the coding algorithm reported by Quan and colleagues24 based on comorbidities present at the time of admission. The Charlson Index was then dichotomized into presence/absence of comorbidities. Patients were also categorized according to type of surgical procedure: internal fixation (IF) or total hip arthroplasty (THA).
Statistical analysis
We compared patient demographics, time to surgery, mortality (in-hospital and 1-yr) and LOS between the pre- and postintervention groups. We used the Student t test to compare means, the Wilcoxon rank-sum test to compare medians and the χ2 test to compare proportions. In-hospital and 1-year survival were assessed using the Kaplan–Meier estimator; the log rank statistic was used to test for differences between the groups. The Cox proportional hazards multiple regression model was used to estimate risk of death with and without adjustment for the covariates of age, sex, type of surgery and presence of co-morbidities.10,15 To control for possible pre-existing or underlying changes in time to surgery and mortality, we created a centred year of surgery variable that was also included in the Cox model. Similar to the existing literature, we also stratified patients into those who received surgery within 48 hours and those who did not. We compared the in-hospital and 1-year mortality between these 2 groups using the same Cox multiple regression model. The assumption of proportionality of the hazards function for the Cox models was assessed graphically using the Kaplan–Meier survival functions, functional forms for continuous variables and cumulative Martindale residuals for categorical and dichotomous variables. We assessed Schoenfeld residuals for any variables appearing to violate proportional hazards assumptions, and Supremum tests of functional form and the proportional hazards assumption were also used. Hazard ratios (HRs) are reported along with 95% confidence intervals (CIs). We carried out all statistical analyses using SAS version 9.2 (SAS Institute).
The University of Manitoba Health Research Ethics Board approved our study protocol.
Results
We included 6542 patients in the study: 3535 in the preintervention group and 3007 in the postintervention group. The mean age of patients was 81.4 ± 10.1 years, 71% were women and 37.2% had 1 or more comorbidities at the time of admission. The postintervention group had a higher rate of comorbidities and a higher proportion of patients who underwent THA than the preintervention group (Table 2).
Table 2.
Demographic characteristics of pre- and postintervention groups
| Characteristic | Group; mean ± SD* | p value | |
|---|---|---|---|
| Preintervention, n = 3535 | Postintervention, n = 3007 | ||
| Sex, % female | 72.1 | 70.6 | 0.18 |
| Age, yr | 81.5 ± 9.9 | 81.4 ± 10.4 | 0.75 |
| Men | 78.6 ± 10.9 | 79.0 ± 10.8 | 0.49 |
| Women | 82.6 ± 9.2 | 82.4 ± 10.1 | 0.53 |
| Femoral neck fracture, % | 50.6 | 51.8 | 0.28 |
| Arthroplasty, % | 35.5 | 38.1 | 0.035 |
| Patients with ≥ 1 preadmission comorbidities, % | 34.9 | 39.8 | < 0.001 |
SD = standard deviation.
Unless otherwise indicated.
Comparison between the pre- and postintervention groups demonstrated improvements in the proportion of cases meeting the 48-hour benchmark, reduced LOS and improved in-hospital crude mortality; however, the trend toward improved 1-year crude mortality did not reach statistical significance (Table 3). Older age, male sex, presence of comorbidities and internal fixation of fracture (as opposed to THA) were all associated with increased risk of death in hospital and at 1 year (Table 4 and Table 5).
Table 3.
Benchmark, time to surgery and crude mortality rate comparisons
| Variable | Group; %* | p value | |
|---|---|---|---|
| Preintervention | Postintervention | ||
| % Meeting 48-h benchmark | 66.8% | 84.6% | < 0.001 |
| Median time to surgery, d | 1.5 | 1.0 | < 0.001 |
| Median length of stay, d | 13.5 | 9.7 | < 0.001 |
| In-hospital mortality (all patients) | 9.6% | 6.8% | < 0.001 |
| In-hospital mortality (only those undergoing surgery) | 6.2% | 4.6% | 0.006 |
| 1-yr mortality (all patients) | 25.7% | 24.0% | 0.12 |
Unless otherise indicated.
Table 4.
Hazard ratios for in-hospital mortality by intervention period
| Variable | HR (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| Period (post v. pre) | 0.73 (0.62–0.87) | 0.68 (0.57–0.81) |
| Age, yr | — | 1.04 (1.03–1.05) |
| Sex (male v. female) | — | 2.05 (1.73–2.44) |
| Presence of comorbidities (≥ 1 v. 0) | — | 4.02 (3.34–4.84) |
| Procedure type (internal fixation v. arthroplasty) | — | 1.66 (1.37–2.01) |
| Centred year of surgery (last v. first) | — | 0.91 (0.83–1.01) |
CI = confidence interval; HR = hazard ratio.
Table 5.
Cox analysis of hazard ratios for 1 year mortality risk by intervention period
| Variable | HR (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| Period (post v. pre) | 0.935 (0.85–1.03) | 0.87 (0.79–0.96) |
| Age | — | 1.05 (1.04–1.05) |
| Sex (male v. female) | — | 1.87 (1.69–2.07) |
| Presence of comorbidities (≥ 1 v. 0) | — | 2.57 (2.33–2.84) |
| Procedure type (internal fixation v. arthroplasty) | — | 1.20 (1.08–1.33) |
| Centred yr of surgery (last v. first) | — | 0.98 (0.94–1.03) |
CI = confidence interval; HR = hazard ratio.
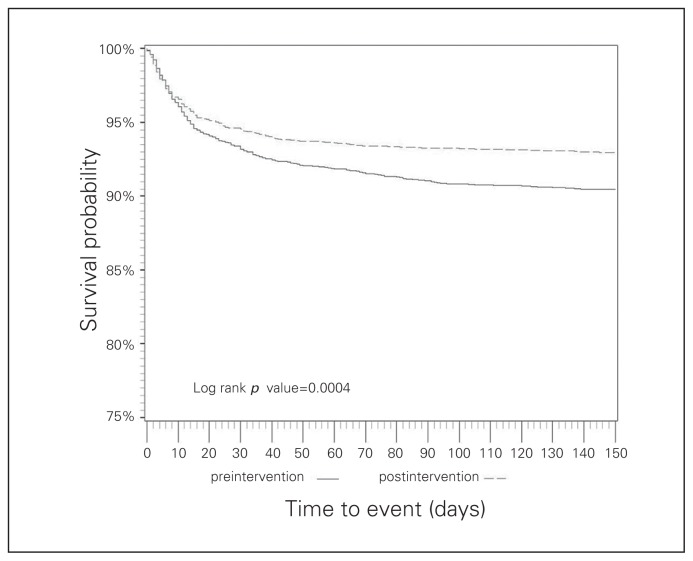
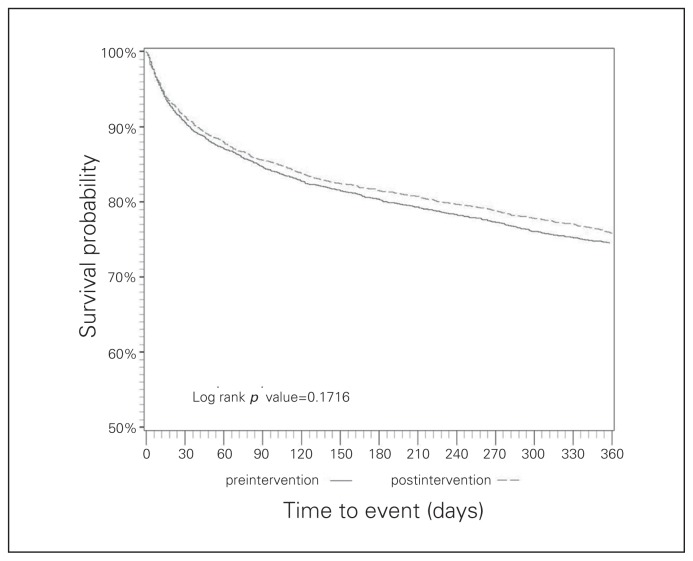
The observed reduction of crude in-hospital mortality was confirmed using Kaplan–Meier survival curves (log rank statistic p < 0.001; Fig. 1); the trend toward improved crude mortality at 1 year still did not reach statistical significance (log rank statistic p = 0.17; Fig. 2). However, once adjusted for confounding variables, a significant reduction in risk of death in the postintervention group was observed both in-hospital (HR 0.68, 95% CI 0.57–0.81) and at 1 year (HR 0.87, 95% CI 0.79–0.96; Table 4 and Table 5).
Fig. 1.
Kaplan–Meier survival curves for in-hospital mortality comparing survival rates before and after the initiative.
Fig. 2.
Kaplan–Meier survival curves for 1-year mortality comparing survival rates before and after the initiative.
Regardless of membership in the pre- or postintervention groups, once adjusted for the same confounders, patients who received surgery within 48 hours had decreased risk of death both in hospital (HR 0.51, 95% CI 0.41–0.63) and at 1 year (HR 0.72, 95% CI 0.64–0.80).
Discussion
Coordinated, multifaceted region-wide efforts to improve the timeliness of hip fracture care can successfully reduce the time to surgery. This reduction in time to surgery appears to reduce both LOS and adjusted mortality in-hospital and at 1 year.
We are aware of 3 other studies that incorporated a control group to study the effectiveness of similar interventions.19,20,25 These studies were limited by small sample sizes and did not detect an effect on mortality. There are 2 important considerations when interpreting the results of meta-analyses15,16 evaluating the effects of surgery within 48 hours. First, they mainly analyzed studies that included only patients who underwent surgery, excluding surgical candidates who died while awaiting surgery. Effects of delayed surgery on risk of death would likely be underestimated as a result. Second, they rely overwhelmingly on observational studies that simply stratify patients into those who received timely surgery and those who did not, thus overlooking the impact of delays in medically complicated patients undergoing preoperative investigations. This would tend to overestimate the risk of death associated with delaying surgery. Our findings actually support this overestimation: the adjusted HR for 1-year mortality when we simply compared patients who received surgery within 48 hours to those who did not (in essence an observational study) was 0.51; when we reduced this selection bias by comparing patients in the postintervention group to the preintervention group, the adjusted HR for 1-year mortality rose to 0.72. This is likely a more accurate assessment of the effect of timely surgery on mortality. Other limitations of the existing literature include the lack of a uniform definition of surgical delay (24, 48 or 72 h) and variability in duration of follow-up when determining mortality.
Our findings are generally consistent with those found by Holt and colleagues26 in their investigations from the Scottish Hip Fracture Audit database. In their examination of the association between patient and management variables and risk of death in 18 817 patients, they found that older age, male sex and preoperative comorbidities (assessed with American Society of Anesthesiologists score) were all strongly associated with greater risk of death. However, they found that management variables, such as time to surgery and seniority of surgeon and anesthesiologist, played a much smaller role, with only the interval from fracture to surgery (and not the interval between admission and surgery) and seniority of anesthesiologist having a significant effect on 30-day and 120-day mortality, respectively. Their 2010 investigation18 involving 4284 patients and studying the association between delays for medical reasons and mortality found that patients with major clinical abnormalities were more likely to have surgery delayed and had higher 30-day mortality. If the abnormalities were corrected during the delay, there was a trend toward increased 30-day survival (odds ratio [OR] 1.69, p = 0.10); if they were not corrected, delay further decreased 30-day survival (OR 0.44, p = 0.008). After controlling for patient case mix factors, they were unable to find a negative association between delay to surgery and mortality. However, only 22.1% of their patients had any sort of delay, and 96% of their patients went to theatre within 2 days of being deemed fit for surgery, thus making it likely that the study was underpowered to detect the negative effect of delay. It is very likely that the improvements we saw in the proportion of patients meeting benchmark (from 66.8% to 84.6%) was largely a result of reducing unnecessary delays in medically fit patients.
We feel that our interventional study design incorporating a control group and a large sample size, using a consistent 48-hour Canadian benchmark, including patients who died before surgery and adjusting analysis for both in-hospital and 1-year risk of death addresses many of the deficiencies that exist in the current literature.
Limitations
Although our study adds to the existing literature by being interventional and not observational in nature, we acknowledge some limitations. The use of administrative data did not allow us to exclude nonsurgical patients from our analysis. However, since the majority of hip fracture patients are treated surgically, with nonoperative treatment typically reserved for the small proportion who are critically ill with very short life expectancy,6–8 the latter group of patients would represent only a small proportion and be unlikely to alter our findings. Furthermore, the postintervention group had a higher rate of comorbidities than the preintervention group (39.8% v. 34.9%), potentially increasing the proportion of patients who were palliative and therefore strengthening our findings of improved crude mortality with improved timeliness of surgery. Although it is possible that changes in coding practice over such a long timeframe studied could have resulted in the comorbidity differences, the ICD-10 was fully implemented in Manitoba by 2004,27 and we therefore feel this is unlikely. The other difference between the 2 groups was the higher rate of THA in the postintervention group. However, this difference was not unexpected, given the slightly higher proportion of femoral neck fractures in this group, combined with recent trends toward increased use of arthroplasty for displaced femoral neck fracture.5,28,29 It is important to note that the possible confounding effects of these differences between the groups were controlled with the use of the Cox model.
We acknowledge that our decision not to compare complications between the groups could be a critique. Others have reported reductions in postoperative complications with timely surgery,16 and the effects of complication rates should ultimately be reflected in our measures of mortality and LOS.
A possible shortcoming was the need for us to estimate the exact time of surgery at 2 of the 6 hospital sites before 2008. This arose because only the date, and not the exact time, of surgery was recorded in the DAD. As a face validity check of the estimated times, we were reassured to find that weekend cases typically occurred around noon, and weekday cases typically occurred around 4 pm. These estimations seem reasonable. The times were comparable to sites with nonmissing data; on the weekend hip fractures would be delayed until midday by the more urgent cases that came in during the preceding night, and on weekdays they would start at the end of the elective slate. As a further check, we performed a sensitivity analysis by setting all the missing time data to 12 am — the best possible scenario, although highly unlikely as hip fracture cases are not typically started after midnight. In this best case scenario, our overall findings did not change.
Finally, it is not possible for us to say with certainty which of our intervention initiatives ultimately led to the observed improvements, or to measure the effect of other unrecognized changes on the improvements. It is possible that at least part of the observed reduction in LOS is attributable to improved repatriation of patients to their home hospitals after surgery. Nonetheless, our findings of reduced adjusted risk of death in those patients undergoing surgery within 48 hours, regardless of time period, underscore the role of timely surgery in reducing mortality.
Generalizability
Although the demographics of patients with a fragility fracture of the hip are similar around the world,2 it is difficult to make direct comparisons of our patient demographics, LOS and crude mortality rates owing to variations in methodology and reporting among existing Canadian studies. Other reports have excluded patients who died while awaiting surgery, included younger patients17,30 and relied on data for LOS and comorbidity status that are collected and categorized in a manner unique to their setting.18,26,31 Comparison of crude rates to non-Canadian data presents similar challenges and underscores the importance of comparing adjusted analyses. Our findings of improved adjusted risk of death both in-hospital (HR 0.68) and at 1 year (HR 0.87) are similar in magnitude to those found in meta-analyses using data derived largely from studies without a control group. Moja and colleagues15 reported an OR of 0.74, while Simunovic and colleagues16 reported a relative risk of 0.81 with shorter times to surgery. Despite the difficulties in making direct comparisons, we feel that our findings have direct relevance to jurisdictions with universal health care coverage.
Conclusion
Region-wide changes directed at meeting a 48-hour benchmark for hip fracture surgery can result in shorter time to surgery, decreased LOS and improved in-hospital and 1-year mortality. This has direct health implications for patients and resource implications for the health systems and further highlights the need to overcome administrative delays for hip fracture surgery.15 Adequately powered prospective studies that examine the role of emergent versus urgent surgery are warranted to provide further clarity around the exact timing of surgery and its effect on complications and health system costs.
Footnotes
Competing interests: None declared.
Contributors: E. Bohm, L. Loucks and L. Lix designed the study. E. Bohm and L. Loucks acquired the data, which all authors analyzed. E. Bohm and L. Loucks wrote the article, which all authors reviewed and approved for publication.
References
- 1.Tarride JE, Hopkins RB, Leslie WD, et al. The burden of illness of osteoporosis in Canada. Osteoporosis Int. 2012;23:2591–600. doi: 10.1007/s00198-012-1931-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporosis Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence VA, Hilsenbeck SG, Noveck H, et al. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162:2053–7. doi: 10.1001/archinte.162.18.2053. [DOI] [PubMed] [Google Scholar]
- 4.Richmond J, Aharonoff GB, Zuckerman JD, et al. Mortality risk after hip fracture. J Orthop Trauma. 2003;17:53–6. doi: 10.1097/00005131-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Heetveld MJ, Rogmark C, Frihagen F, et al. Internal fixation versus arthroplasty for displaced femoral neck fractures: What is the evidence? J Orthop Trauma. 2009;23:395–402. doi: 10.1097/BOT.0b013e318176147d. [DOI] [PubMed] [Google Scholar]
- 6.Handoll HH, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst Rev. 2008;(3):CD000337. doi: 10.1002/14651858.CD000337.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Mak JC, Cameron ID, March LM, et al. Evidence-based guidelines for the management of hip fractures in older persons: an update. Med J Aust. 2010;192:37–41. doi: 10.5694/j.1326-5377.2010.tb03400.x. [DOI] [PubMed] [Google Scholar]
- 8.Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003;27:11–7. doi: 10.1007/s00264-002-0404-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canadian Institute for Health Information. Health Indicators 2007. Ottawa: 2007. [accessed 2015 June 28]. Available: https://secure.cihi.ca/free_products/hi07_health_indicators_2007_e.pdf. [Google Scholar]
- 10.Roos LL, Walld RK, Romano PS, et al. Short-term mortality after repair of hip fracture. Do Manitoba elderly do worse? Med Care. 1996;34:310–26. doi: 10.1097/00005650-199604000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Zuckerman JD, Skovron ML, Koval KJ, et al. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77:1551–6. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Papaioannou A, Morin S, Cheung AM, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–73. doi: 10.1503/cmaj.100771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canada H. First Minister’s Meeting on the Future of Health Care 2004: A 10-year plan to strengthen health care. 2004. [accessed 2013 Nov. 29]. Available: www.hc-sc.gc.ca/hcs-sss/delivery-prestation/fptcollab/2004-fmm-rpm/index-eng.php.
- 14.Ontario Ministry of Health and Long Term Care. First ever common benchmarks will allow Canadians to measure progress in reducing wait times. 2005. [accessed 2015 June 28]. Available: http://news.ontario.ca/archive/en/2005/12/12/First-ever-common-benchmarks-will-allow-Canadians-to-measure-progress-in-reducin.html.
- 15.Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS ONE. 2012;7:e46175. doi: 10.1371/journal.pone.0046175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182:1609–16. doi: 10.1503/cmaj.092220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergeron E, Lavoie A, Moore L, et al. Is the delay to surgery for isolated hip fracture predictive of outcome in efficient systems? J Trauma. 2006;60:753–7. doi: 10.1097/01.ta.0000214649.53190.2a. [DOI] [PubMed] [Google Scholar]
- 18.Holt G, Smith R, Duncan K, et al. Does delay to theatre for medical reasons affect the peri-operative mortality in patients with a fracture of the hip? J Bone Joint Surg Br. 2010;92:835–41. doi: 10.1302/0301-620X.92B6.24463. [DOI] [PubMed] [Google Scholar]
- 19.Roberts HC, Pickering RM, Onslow E, et al. The effectiveness of implementing a care pathway for femoral neck fracture in older people: a prospective controlled before and after study. Age Ageing. 2004;33:178–84. doi: 10.1093/ageing/afh063. [DOI] [PubMed] [Google Scholar]
- 20.Swanson CE, Day GA, Yelland CE, et al. The management of elderly patients with femoral fractures. A randomised controlled trial of early intervention versus standard care. Med J Aust. 1998;169:515–8. [PubMed] [Google Scholar]
- 21.Winnipeg Regional Health Authority. About Us 2013. [accessed 2013 Nov. 29]. Available: www.wrha.mb.ca/about/aboutus.php.
- 22.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 24.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 25.Beringer TR, Crawford VL, Brown JG. Audit of surgical delay in relationship to outcome after proximal femoral fracture. Ulster Med J. 1996;65:32–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Holt G, Smith R, Duncan K, et al. Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the Scottish hip fracture audit. J Bone Joint Surg Br. 2008;90:1357–63. doi: 10.1302/0301-620X.90B10.21328. [DOI] [PubMed] [Google Scholar]
- 27.Walker RL, Hennessy DA, Johansen H, et al. Implementation of ICD-10 in Canada: How has it impacted coded hospital discharge data? BMC Health Serv Res. 2012;12:149. doi: 10.1186/1472-6963-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Clinical Guideline Centre Hip fracture. The management of hip fracture in adults. London (UK): National Institute for Health and Clinical Excellence (NICE); 2011. Jun. [accessed 2015 June 16]. p. (Clinical guideline; no. 124). Available: www.guideline.gov/content.aspx?id=34827. [Google Scholar]
- 29.Callaghan JJ, Liu SS, Haidukewych GJ. Subcapital fractures: a changing paradigm. J Bone Joint Surg Br. 2012;94(Suppl A):19–21. doi: 10.1302/0301-620X.94B11.30617. [DOI] [PubMed] [Google Scholar]
- 30.Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332:947–51. doi: 10.1136/bmj.38790.468519.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weller I, Wai EK, Jaglal S, et al. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87:361–6. doi: 10.1302/0301-620x.87b3.15300. [DOI] [PubMed] [Google Scholar]