Abstract
Background:
Craniometric studies have shown that both Chiari malformation (CM) and basilar invagination (BI) belong to a spectrum of malformations. A more precise method to differentiate between these types of CVJM is desirable. The Chamberlain's line violation (CLV) is the most common method to identify BI. The authors sought to clarify the real importance of CLV in the spectrum of craniovertebral junction malformations (CVJM) and to identify possible pathophysiological relationships.
Methods:
We evaluated the CLV in a sample of CVJM, BI, CM patients and a control group of normal subjects and correlated their data with craniocervical angular craniometry.
Results:
A total of 97 subjects were studied: 32 normal subjects, 41 CM patients, 9 basilar invagination type 1 (BI1) patients, and 15 basilar invagination type 2 (BI2) patients. The mean CLV violation in the groups were: The control group, 0.16 ± 0.45 cm; the CM group, 0.32 ± 0.48 cm; the BI1 group, 1.35 ± 0.5 cm; and the BI2 group, 1.98 ± 0.18 cm. There was strong correlation between CLV and Boogard's angle (R = 0.82, P = 0.000) and the clivus canal angle (R = 0.7, P = 0.000).
Conclusions:
CM's CLV is discrete and similar to the normal subjects. BI1 and BI2 presented with at least of 0.95 cm CLV and these violations were strongly correlated with a primary cranial angulation (clivus horizontalization) and an acute clivus canal angle (a secondary craniocervical angle).
Keywords: Arnold–Chiari malformation, basilar impression, cephalometry, platybasia
INTRODUCTION
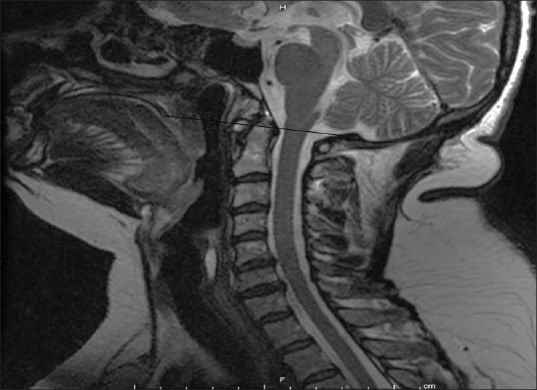
The most common adult craniocervical junction malformations (CVJM) are Chiari malformation (CM) [Figure 1] and basilar invagination (BI).[18]
Figure 1.
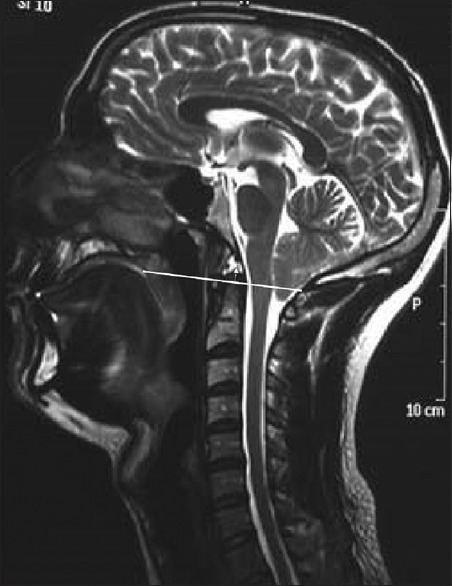
Chiari malformation patient. Solid line is the Chamberlain's line. Dotted arrow above CL represent Chamberlain's line violation
Craniometric studies have shown that both of these malformations belong to a spectrum of malformations whose common characteristic is the underdevelopment of the occipital bone and consequent neural and cerebrospinal fluid (CSF) flow compression at the craniocervical junction. BI is the more substantial malformation and differs from CM by the displacement of the cervical spine toward the foramen magnum and ventral brainstem compression.[18]
Increasing evidence has identified two subgroups of BI: One is associated with craniovertebral instability in which the tip of the odontoid process projects inside the foramen magnum,[7,8,10,11,17,19,21,24] and the other is not associated with instability, but with greater cranial deformity [Figures 2 and 3]. Angular craniometric studies have identified differences between the types of adult CVJM.[1]
Figure 2.
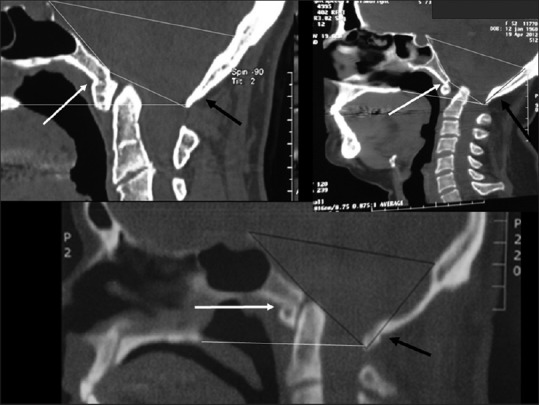
Basilar Invagination type 1. Note that in all cases the odontoid process is inside foramen magnum. The white arrows point to the anterior atlas assimilation and black arrow point to the posterior atlas assimilation. D: Dorsum sellae; B: Basium; O: Opistium
Figure 3.
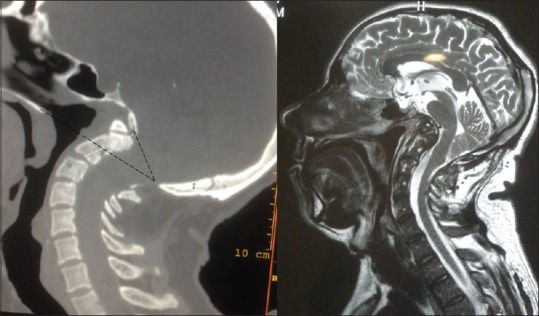
Type 2 Basilar Invagination. At left, CT scan. Lower black line represents Chamberlain's Line (CL). Upper line represents foramen magnum line. Black arrow is inserted in the C2 axis. The Odontoid above CL is the amount of odontoid CL violation
Classically, the Chamberlain's baseline violation (CLV) has been used to diagnose BI, but in the literature, this criterion has varied between extreme values of 1 and 6.6 mm above the CLV.[6,22] A precise definition of CLV for diagnosing BI is lacking.[22]
In order to reveal the relationship between CLV in BI, CM patients and normal subjects, we correlated their data with craniocervical angular craniometry to identify possible pathophysiological relationships.
MATERIALS AND METHODS
This study was approved by the Research Ethics Committee (Instituto de Assistencia Médica ao Servidor Público Estadual - sp-caae07284212000005463).
To study the degree of odontoid process invagination, we evaluated magnetic resonance imaging (MRI) scans of the craniocervical junction in T1 and T2 midline sagittal scan acquisitions from a CVJM patient sample consecutively treated by the authors between 1996 and 2012. Computed tomography (CT) scans were used only in specific cases, when necessary, to clarify details of bone anatomy.
The measurements were performed by an observer who was unaware of other study data.
Patients with CVJM were divided into three groups: CM patients, basilar invagination type 1 (BI1) patients and basilar invagination type 2 (BI2) patients.[1,6]
Patients with CM had symptomatic cerebellar tonsil herniation and/or posterior fossa structure and cisterna magna compressions [Figure 1].
Patients with BI were divided into two groups: Those with axis dens invagination into the foramen magnum were referred to as type I (BI1) [Figure 2].
Patients with invagination of the dens toward the base of the skull but not toward the inside of the foramen magnum were classified as BI2 [Figure 3].[1,6]
The studied sample was based on primary craniovertebral junction malformations without any immediate evident inflammatory, bone, or connective tissue disease.
To compare these findings with the odontoid process invagination in normal subjects (control group), images from 32 consecutive normal subjects were evaluated [Figure 4].
Figure 4.
Control group image. Note the odontoid tip at the Chamberlain's line and the vertical clivus
Patients who had normal MRI scans that were performed by the Radiology Department of the Hospital do Mandaqui to clarify cervical spine or head symptoms and who were matched by age and sex to the CCJM group made up the control group. Patients with tumors, trauma, and any diagnostic pathology were excluded from this study.
The amount of Chamberlain's basal line violation (CLV) was measured as follows [Figure 5]:
Figure 5.
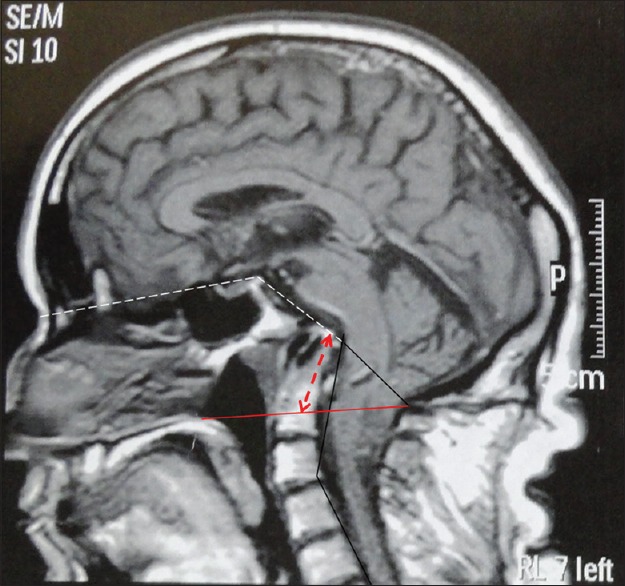
Type 2 Basilar invagination. The red line is the Chamberlain's Line (CL). The dotted red arrow represents CLV. Dotted white lines above represents Welcher's angle. The angle formed by the inferior dotted white line and solid black line is the Boogard's angle. The vertical lines along with C2 and C7 axis forms the cervical spine lordosis angle
Images from the midline craniocervical MRI (or CT) were digitalized, and the CLV was traced from the hard palate to the opistion. The distance above or below the CLV was measured using the Meazure 3.2 software and the image ruler. The distance above the CLV was considered positive measurements, and the distance below the CLV was considered negative measurements. The 95% confidence interval was set as the limits for BI diagnosis.
One study evaluating craniovertebral angulations among CCJM and normal subjects revealed significant differences between the groups.[1] To analyze the possible physiopathological association between the degree of CL violation and the angular craniometric variables, the following angles divided into two groups were studied in the craniocaudal direction in a previous study:[1]
Primary cranial angles: Basal (Welcher's angle) and Boogard's angle (BOO)
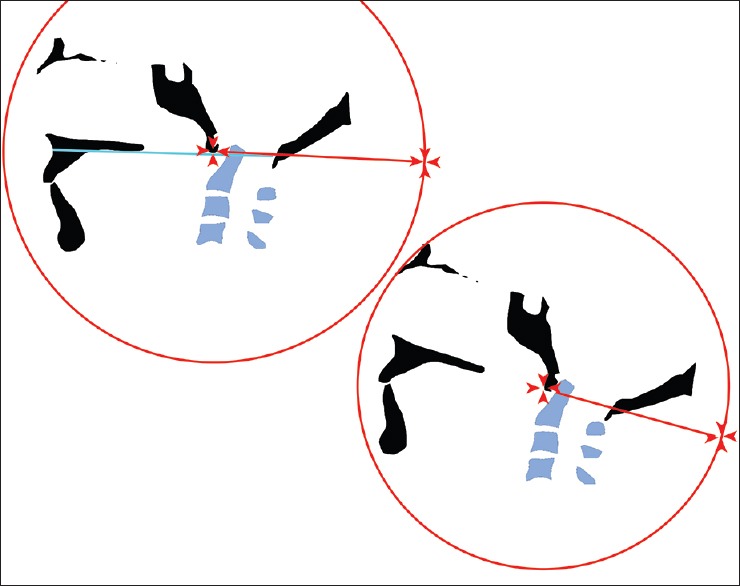
Secondary craniocervical angles: Clivus canal angle (CC) and cervical spine lordosis angle (CL) are illustrated in Figures 5 and 6.
Figure 6.
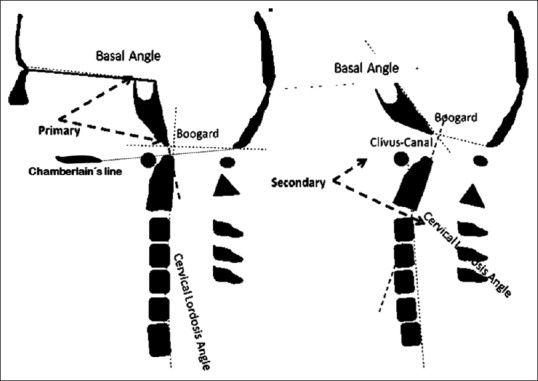
At left are represented the primary angles: Basal angle (Welcher) and Boogard's angle. The Chamberlain's line is represented from the hard palate to the opistion. At right are represented secondary craniocervical angles: Clivus canal angle and cervical lordosis
Basal angle (BA): Defined as the angle measured from the nasion, top of the dorsum sellae, and the basion.[1,12,23]
CC: The angle between the line extending from the top of the dorsum sellae to the basion and the line between the inferodorsal portions of C2 to the most superodorsal part of the dens.
BOO: The angle between the top of the dorsum sellae, basion, and opisthion.[1,12,23]
CL: The angle between a line drawn from the most inferodorsal to the most superodorsal part of C2 (dens of the axis) and another line drawn between the supero- and inferodorsal regions of the C7 posterior vertebral body.[1] The larger CL resulted in a more straightened spine, and the shorter CL resulted in a more lordotic spine.
The degree of CLV was correlated to the primary cranial angles and secondary craniovertebral angles.
Statistics: Demographic data and descriptive statistics are expressed as the media, standard deviation and 95% confidence intervals. The Kolmogorov–Smirnov test was used to evaluate the normality of the numeric variable distribution. The Levine test was used to verify the variance homogeneity. Gender distributions were compared with the Chi-squared test. The ANOVA Kruskal–Wallis test was used to compare the media of the four groups, and Bonferroni's (correction) test was used as a post hoc test. The correlations between CLV and the cranial and craniovertebral angles were tested with the Spearman correlation test. The correlation strength was classified as follows: 0: Absence of correlation; 0.1–0.3: Weak correlation; 0.4–0.6: Moderate correlation; >0.6–0.9: Strong correlation; and 1: Perfect correlation.
RESULTS
A total of 97 subjects were studied: 32 normal subjects in the control group, 41 CM patients, 9 BI1 patients and 15 BI2 patients.
The mean age of the control group was 44.8 ± 12 years, and the mean age in the craniovertebral junction malformation groups was 46.9 ± 11 years (t test: P = 0.40).
Among the 32 normal subjects, 17 were male, and among the 65 malformation patients, 30 were male (Chi-square, P = 0.51).
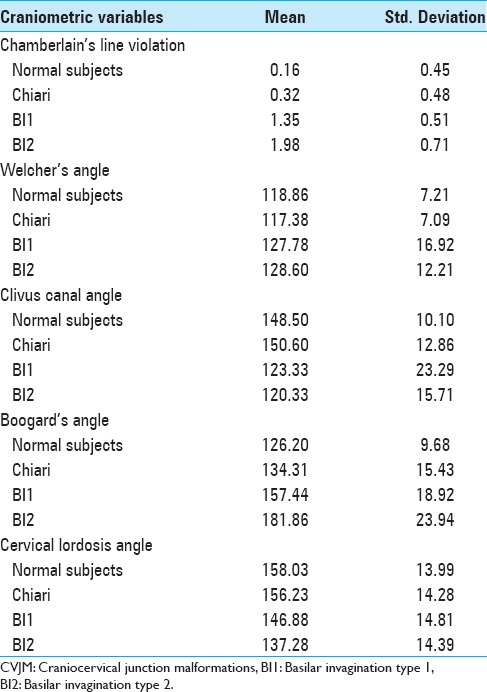
Descriptive data for CLV, Welcher angle, CC, BOO, and CL for all groups are described in Table 1.
Table 1.
Chamberlain's line violation and craniometric values of CVJM and normal subjects
Chamberlain's line violation
The mean and 95% confidence intervals of CLV in the three groups are illustrated in Figure 7.
Figure 7.
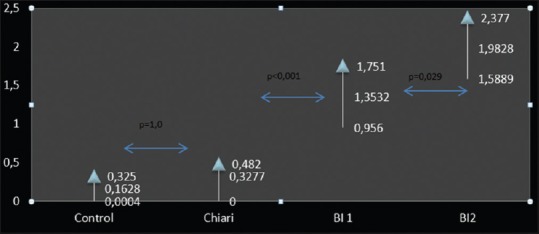
The Chamberlain's line violation by odontoid process in Control group, Chiari malformation, Basilar type1 (BI1) and Type 2 groups (BI2). Upper and lower values are the 95% confidence limit values and the median value is the media of sample values
The mean CLV values were as follows: The control group (CTRL), 0.16 ± 0.45 cm; the CM group, 0.32 ± 0.48 cm; the BI1 group, 1.35 ± 0.5 cm; and the BI2 group, 1.98 ± 0.18 cm.
The CLV differed among the four groups (ANOVA–Kruskal–Wallis, P < 0.001).
The post hoc (Bonferroni) test revealed that the CLV between the CTRL and CM groups did not differ (P = 1.0). Both groups differed from the BI1 and BI2 groups (Bonferroni; P < 0.001). The IB2 group exhibited significantly greater CLV than the BI1 group (1.98 × 1.35, Bonferroni, P = 0.029).
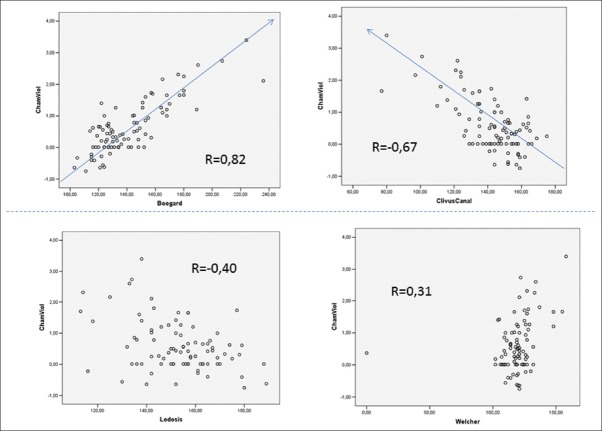
Correlation among CLV and the craniometric Welcher, Clivus canal, Boogard, and cervical lordosis angle
To evaluate the physiopathological association with the cranial or craniocervical angles, a Spearman correlation among these variables was tested [Figures 8 and 9]. There was a strong correlation between CLV and BOO (R = 0.81, P = 0.000) and between CLV and the CC (R = -0.688, P = 0.000) and a moderate correlation between CLV and CL (R = -0.39, P = 0.000) and between CLV and Welcher's angle (R = 0.32, P = 0.002). The scatter dot plot does not illustrate a significant correlation between CLV and Welcher's angle.
Figure 8.
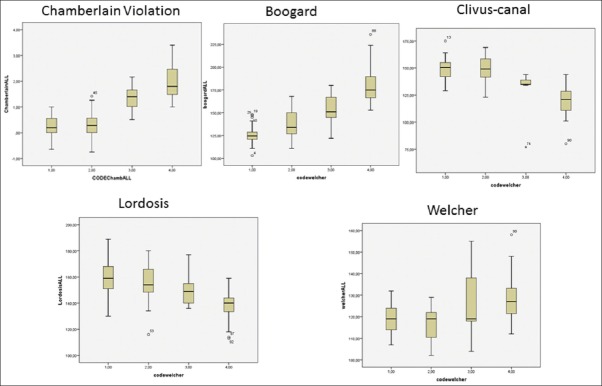
Illustration of descriptive statistcs for Chamberlain's line violation, Boogard's angle, Clivus canal angle, cervical lordosis angles (Lordosis) and Welcher's angle (Welcher). In the x-axis, 1, 2, 3, and 4 is referred to control group, Chiari malformation, Basilar Invagination type 1 and Basilar invagination type 2 groups, respectively. Note that as the as the CLV increases, Boogard's values increase and Clivus canal and Cervical lordosis angle decrease
Figure 9.
Scatter dot plot. Upper part: At left, data from CLV are plotted against Boogard's angle. The “R” numbers are referred to the amount of correlation between data. At right, data from CLV and Clivus canal angle are plotted. Lower left: Relation between cervical lordosis angle and CLV. At right, relation between Welcher angle and CLV
DISCUSSION
BI was originally described by Ackermann in cretins from the Alps.[20,23]
In 1939, Chamberlain described four cases of basilar impression, and his method for diagnosing this condition was the “base line.”[3] Since then, the most cited way of precisely diagnose BI was measuring the amount of base line violation or CLV. However, the cited CLV criterion varies widely (between 1 and 6.6 mm of CLV).[1,6,22]
Craniocervical junction patient's identification has significantly improved in the last three decades. MRI has increased the diagnosis of tonsillar herniation through the foramen magnum and has facilitated the identification of BI patients with and without craniovertebral instability but a more precise definition of the malformation types is lacking.[15,16] With the use of MRI, the precise diagnosis of BI type and the nature of neural compression facilitate the selection of the best surgical approach for each CCJM case.[13,25]
BI may be “primary” (resulting from a congenital or developmental anomaly) or “secondary” (basilar impression), resulting from bony softening and molding.[17] We only investigated primary cases in this study.
The term CM, as currently defined, have included heterogeneous group of disorders with different pathogenetic origins.[15] Due to the great variability in CLV described in the literature, many BI cases may have been described under the common term, Chiari malformation.
Two relatively new treatment modalities have been used for treating BI: The anterior transnasal endoscopic approach and the posterior reduction and stabilization approach.[2,4,9,14,18,19,21,22,23,24] Some authors have performed both anterior and posterior approaches in unstable BI1 cases.[13] It is likely that isolated posterior approaches could be indicated in these instability cases.
A careful observation of a series of publications on adult BI cases revealed that BI invaginations associated with instability are a homogeneous group with common characteristics: Anterior atlas assimilation and ventral brainstem compression by the odontoid process invagination through the foramen magnum.[1,10,14,21] These cases have been reduced promptly under only head extension or skull traction [Figure 10].
Figure 10.

Upper part: T1 (left) and T2 acquisitions showing BI1. Note the ventral cord and brainstem compression by odontoid process. Lower part: CT scan sagittal reconstruction. At left, the odontoid process in inside foramen magnum (Dotted line passing below anterior assimilated C1 arc)
BI without instability is associated with greater cranial deformity, greater clivus horizontalization, an acute CC, and associated platybasia [Figures 3 and 5].[1,6,23] The anterior approach and endscopic transnasal approach play an important role in these complications. Recent experience has revealed that the most difficult cases for the transoral approach, in which the odontoid process was located very high, has been the most appropriate cases for the transnasal approach.[5]
CLV analysis suggests fundamental differences among the CCJM groups. In the CM group, the upper confidence limit is set to below 5 mm. The amount of CLV in this group is small and was not significantly different from the control group. Other angular craniometric CM values did not differ from those in normal subjects.[1] CLV is more significant in BI than in CM. The CLV lower confidence interval limit was set at 9.56 mm in the BI1 group. This 95% lower confidence interval value is suggested to be the lower limit of CLV for BI diagnosis. For the BI2 group, the 95% lower limit of the confidence interval was set at 1.6 cm.
The strongest correlation with CLV was shown by the clivus horizontalization measured by BOO, and the second strongest correlation with CLV was shown by the CC. The association of CLV with one primary cranial angle suggests that the skull shape has is a direct determinant of the physiopathology of CLV and ventral brainstem compression. Published data shows that clivus horizontalization is associated with craniovertebral angulation and craniocervical kyphosis.[1] Craniocervical kyphosis is associated with ventral brainstem compression. These associations have practical and clinical importance: Although BOO is an unchangeable characteristic, the CC may be modified by head extension or traction.[2,4,8,9,10,11,14,17,19,21,24] Clivus canal reduction may decrease the CLV and ventral neural compression [Figures 10 and 11].[2] The hyperlordosis associated with these cases may decrease secondary to the more physiologic values if the fixation system does not stop below C2.[1,2] These findings have potential clinical implications in a better selection of CVJ type and amplification of those patients who would be candidates for single posterior alignment and correction rather than ventral approaches or circumferential surgeries.
Figure 11.
The importance of head in reducing BI1. Note the reduction of ventral brainstem compression and CLV with extension of head and caniocervical junction kyphosis normalization
CONCLUSIONS
CM patients presented with discrete CLV similar to normal subjects. BI1 presented a CLV of at least of 0.96 cm and BI2 patients had at least 1.5 cm of CLV. There is strong correlation with CLV and clivus horizontalization, suggesting pathopysiologic relationship with the primary cranial angle and, with and CC, a secondary craniocervical angle.
Footnotes
Contributor Information
Jânio A. Ferreira, Email: janio_21@yahoo.com.br.
Ricardo V. Botelho, Email: bitbot@uol.com.br.
REFERENCES
- 1.Botelho RV, Ferreira ED. Angular craniometry in craniocervical junction malformation. Neurosurg Rev. 2013;36:603–10. doi: 10.1007/s10143-013-0471-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Botelho RV, Beco Neto E, Patriota GC, Daniel JW, Dumont PAS, Rotta JM. Basilar invagination: Craniocervical instability treated with cervical traction and occipitocervical fixation. J Neurosurg Spine. 2007;7:444–9. doi: 10.3171/SPI-07/10/444. [DOI] [PubMed] [Google Scholar]
- 3.Chamberlain WE. Basilar Impression (Platybasia): A Bizarre Developmental Anomaly of the Occipital Bone and Upper Cervical Spine with Striking and Misleading Neurologic Manifestations. Yale J Biol Med. 1939;11:487–96. [PMC free article] [PubMed] [Google Scholar]
- 4.Dahdaleh NS, Dlouhy BJ, Menezes AH. Application of neuromuscular blockade and intraoperative 3D imaging in the reduction of basilar invagination. Technical note. J Neurosurg Pediatrics. 2012;9:119–24. doi: 10.3171/2011.11.PEDS11332. [DOI] [PubMed] [Google Scholar]
- 5.El-Sayed IH, Wu J, Dhillon N, Ames CP, Mummaneni P. The Importance of Platybasia and the Palatine Line in Patient Selection for Endonasal Surgery of the Craniocervical Junction: A Radiographic Study of 12 Patients. World Neurosurg. 2011;76:183–8. doi: 10.1016/j.wneu.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goel A, Bhatjiwalem M, Desai K. Basilar invagination: A study based on 190 surgically treated Patients. J Neurosurg. 1998;88:962–8. doi: 10.3171/jns.1998.88.6.0962. [DOI] [PubMed] [Google Scholar]
- 7.Goel A, Shah A. Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine. 2009;10:220–7. doi: 10.3171/2008.12.SPINE08499. [DOI] [PubMed] [Google Scholar]
- 8.Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1:281–6. doi: 10.3171/spi.2004.1.3.0281. [DOI] [PubMed] [Google Scholar]
- 9.Hsu W, Zaidi HA, Suk I, Gokaslan ZL, Wolinsky JP. A new technique for intraoperative reduction of occipitocervical instability. Neurosurgery. 2010;66(6 Suppl Operative):S319. doi: 10.1227/01.NEU.0000369925.81522.60. [DOI] [PubMed] [Google Scholar]
- 10.Joseph V, Rajshekhar V. Resolution of syringomyelia and basilar invagination after traction. Case illustration. J Neurosurg. 2003;98(3 Suppl):S298. doi: 10.3171/spi.2003.98.3.0298. [DOI] [PubMed] [Google Scholar]
- 11.Kim IS, Hong JT, Sung JH, Byun JH. Vertical reduction using atlantoaxial facet spacer in basilar invagination with atlantoaxial instability. J Korean Neurosurg Soc. 2011;50:528–31. doi: 10.3340/jkns.2011.50.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Konigsberg RA, Vakil N, Hong TA, Htaik T, Faerber E, Maiorano T, et al. Evaluation of platybasia with MR imaging. AJNR Am J Neuroradiol. 2005;26:89–92. [PMC free article] [PubMed] [Google Scholar]
- 13.Kwong Y, Rao N, Latief K. Craniometric measurements in the assessment of craniovertebral settling: Are they still relevant in the age of cross-sectional imaging? AJR Am J Roentgenol. 2011;196:W421–5. doi: 10.2214/AJR.10.5339. [DOI] [PubMed] [Google Scholar]
- 14.Mcgirt MJ, Attenello FJ, Sciubba DM, Gokaslan ZL, Wolinsky J. Endoscopic transcervical odontoidectomy for pediatric basilar invagination and cranial settling. J Neurosurg Pediatrics. 2008;1:337–42. doi: 10.3171/PED/2008/1/4/337. [DOI] [PubMed] [Google Scholar]
- 15.Milhorat TH, Bolognese PA, Nishikawa M, McDonnell NB, Francomano CA. Syndrome of occipitoatlantoaxial hypermobility, cranial settling, and Chiari malformation type I in patients with hereditary disorders of connective tissue. J Neurosurg Spine. 2007;7:601–9. doi: 10.3171/SPI-07/12/601. [DOI] [PubMed] [Google Scholar]
- 16.Milhorat TH, Nishikawa M, Kula RW, Dlugacz YD. Mechanisms of cerebellar tonsil herniation in patients with Chiari malformations as guide to clinical management. Acta Neurochir. 2010;152:1117–27. doi: 10.1007/s00701-010-0636-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishikawa M, Ohata K, Baba M, Terakawa Y, Hara M. Chiari I malformation associated with ventral compression and instability: One-stage posterior decompression and fusion with a new instrumentation technique. Neurosurgery. 2004;54:1430–4. doi: 10.1227/01.neu.0000125326.15525.b8. [DOI] [PubMed] [Google Scholar]
- 18.Nishikawa M, Sakamoo H, Hakuba A, Nakanishi N, Inoue Y. Pathogenesis of Chiari malformation: A morphometric study of the posterior cranial fossa. J Neurosurg. 1997;86:40–7. doi: 10.3171/jns.1997.86.1.0040. [DOI] [PubMed] [Google Scholar]
- 19.Peng X, Chen L, Wan Y, Zou X. Treatment of primary basilar invagination by cervical traction and posterior instrumented reduction together with occipitocervical fusion. Spine. 2011;36:1528–31. doi: 10.1097/BRS.0b013e3181f804ff. [DOI] [PubMed] [Google Scholar]
- 20.Silva JAG da, Santos AA do, Jr, Melo LRS, de Araújo AFA, Regueira GP. Posterior fossa decompression with tonsillectomy in 104 cases of basilar impression, Chiari malformation and/or syringomyelia. Arq Neuropsiquiatr. 2011;69:817–23. doi: 10.1590/s0004-282x2011000600018. [DOI] [PubMed] [Google Scholar]
- 21.Simsek S, Yigitkanli K, Belen D, Bavbek M. Halo traction in basilar invagination: technical case report. Surg Neurol. 2006;66:311–4. doi: 10.1016/j.surneu.2005.12.029. [DOI] [PubMed] [Google Scholar]
- 22.Smoker WR. Craniovertebral junction: Normal anatomy, craniometry, and congenital anomalies. Radiographics. 1994;14:255–77. doi: 10.1148/radiographics.14.2.8190952. [DOI] [PubMed] [Google Scholar]
- 23.Vet AD. Basilar impression of the skull. J Neurol Psychiatry. 1940;3:241–50. doi: 10.1136/jnnp.3.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Young RM, Sherman JH, Wind JJ, Litvack Z, O’Brien J. Treatment of craniocervical instability using a posterior-only approach. J Neurosurg Spine. 2014;21:239–48. doi: 10.3171/2014.3.SPINE13684. [DOI] [PubMed] [Google Scholar]
- 25.Yu Y, Wang X, Zhang X, Hu F, Gu Y, Xie T, et al. Endoscopic transnasal odontoidectomy to treat basilar invagination with congenital osseous malformations. Eur Spine J. 2013;22:1127–36. doi: 10.1007/s00586-012-2605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]