Abstract
Background:
This study aimed to determine how age groups effect on the phenotype of metabolic syndrome (MetS) among Iranian population.
Materials and Methods:
This cross-sectional study was conducted as part of Isfahan Healthy Heart Program. Height, weight, waist circumference, and blood pressure were measured by trained health-care professionals. MetS was defined as having three or more of the National Cholesterol Education Program III criteria. The relation between different age groups and different phenotypes of MetS was examined using the multinomial logistic regression.
Results:
We found low high-density lipoprotein-cholesterol (HDL-c) was the most common feature, followed by hypertriglyceridemia (HTG), abdominal obesity (ABO), hypertension (HTN), and high fasting blood glucose in decreasing order of prevalence. The most prevalent combination of MetS components was hypertrigeceridemia, low HDL-c and ABO (50.7%) in all subjects and especially in younger age group (63.2%). In elder age group, the most prevalent three components combination was HTG, Low HDL-c and HTN (43.9%). Logistic regression analysis demonstrated that elder subjects were at approximately 12 times higher risk of having the combination HTG, ABO, low HDL-c, and HTN (P < 0.001) compared to the middle age subjects who had a lower risk for the same combination; (2 [1.49-3.49]) (P < 0.001).
Conclusion:
This study provides a nationally representative estimate of the prevalence of different phenotypes of MetS across different age groups. Regarding different phenotypes of MetS in various age groups need to have important implications in the clinical management of these patients and the implementation of public health.
Keywords: Age groups, Iran, metabolic cardiovascular syndrome, phenotype
INTRODUCTION
The metabolic syndrome (MetS) is a clinical syndrome characterized by clustering cardiovascular risk factors. MetS increase the risk of cardiovascular events, diabetes mellitus, and the related mortality.[1,2,3] Previous studies demonstrated a high prevalence of MetS among both adolescents and adults in Iran as well as other countries.[4,5,6,7,8,9,10,11] In Iran, the high prevalence of specific components of MetS such as diabetes, hypertriglyceridemia (HTG), hypertension (HTN), and abdominal obesity (ABO), shown to be increasing during recent years.[12] Previous studies that were locally conducted in Iran, had reported the prevalence of MetS and its components in different age groups and in different population.[13] However, it is unclear how age effects on phonotype of MetS among Iranian population. We believe finding a correlation between age distribution, different MetS components and their phenotypes may give policy and health-care decision makers some indications for better planning. Moreover, these findings will create a new view points for clinicians. The aim of this study is to demonstrate the effect of age on the phenotype of MetS in Iranian population.
MATERIALS AND METHODS
This cross-sectional study conducted as a part of Isfahan Healthy Heart Program (IHHP). The IHHP was a 6 year comprehensive integrated community base program for cardiovascular disease (CVD) prevention and control through reducing CVD risk factors and improving life- style to encourage healthy behaviors.[14,15] Participants in this secondary analysis were 4644 individuals aged over 19 years in resident Isfahan, which participate in the final phase of IHHP in 2007. Finally, 982 subjects with MetS based on National Cholesterol Education Program (NCEP) were studied. All participants signed an informed written consent and the study was approved by Research Council of Isfahan Cardiovascular Research Institute. Height, weight, waist circumference, and the blood pressure were measured by trained health-care professionals. We measured waist circumference at the part of the trunk located midway between the lower costal margin (bottom of the lower rib) and the iliac crest (top of the pelvic bone) while the person was standing with feet about 25-30 cm apart.
After 15 min rest, blood pressure was measured twice on the right arm and in the sitting position. The mean of the two recordings was reported as patient's blood pressure. Subjects who had three or more of the criteria defined by NCEP was diagnosed with MetS. The criteria of NCEP include: (1) central obesity as the waist circumference > 102 cm in men and > 88 cm in women; (2) fasting plasma triglycerides ≥ 150 mg/dl; (3) low high-density lipoprotein-cholesterol (HDL-c) <40 mg/dl in men and < 50 mg/dl in women; (4) systolic blood pressure ≥ 130 mm Hg and/or diastolic blood pressure 85 mm Hg and/or antihypertensive agents (5) hyperglycemia with fasting plasma glucose ≥ 100 mg/dl and/or hypoglycemic medications.[16]
Statistical analysis
Age-specific data were analyzed with descriptive statistics to determine the general and clinical characteristics of the study participants. The Chi-square test and the ANOVA test were used to examine significant differences according to age groups. To identify the relation between age groups and different components of MetS were examined using the multinomial logistic regression with adjustments for general characteristics of the study participants such as smoking; nutritional habit and the physical activity were performed by presenting odds ratios (ORs) and their 95% confidence intervals. Since, the prevalence of low HDL-c + HTN + high fasting blood sugar (FBS) and HTN + ABO + high FBS was very low among younger and middle age subject so OR of elder subjects compared with younger plus middle age. All statistical analyses were conducted using the SPSS 16.0.
RESULTS
The prevalence of the MetS among the adults was 21.1%. The prevalence of MetS increased with age from 8.3% in young adults (aged 18-34 years) 30.8% in middle age (35-64) and 48.6% in elderly adults (65 years and older) (results not shown in table). The prevalence of the components of MetS varied in our study. Low HDL was the most common feature, followed by HTG, ABO, HTN and high fasting blood glucose (FBG) in decreasing order of prevalence. The prevalence of each specific component of MetS differed between younger and older adults. Compared to older adults, young adults had a higher prevalence of low HDL-c and a lower prevalence of high FBG. In the middle age subjects the same pattern for a single component was observed regardless of age. Low HDL-c plus obesity (67.3%) and HTG plus ABO (59.9%) were more prevalent combinations among our subjects. Low HDL-c was very prevalent in all subjects with MetS [Table 1]. 76% of young individuals with MetS had both ABO and low HDL-c levels compared to 68.5% of middle age and 54.1% of elder adults with MetS (P = 0.001).
Table 1.
MetS components in patients with MetS
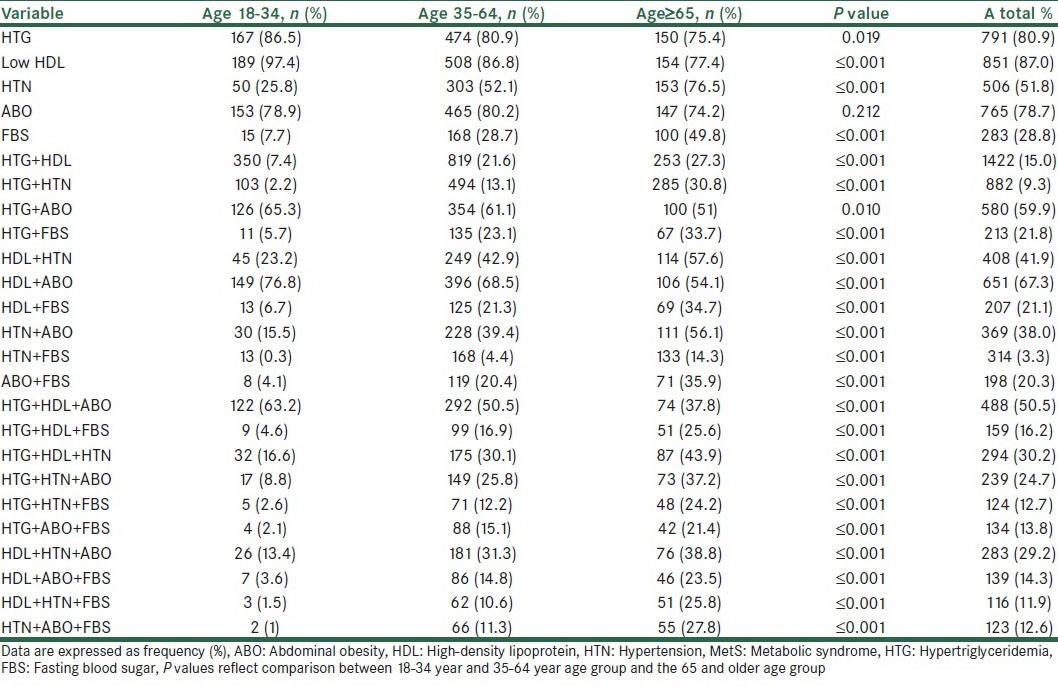
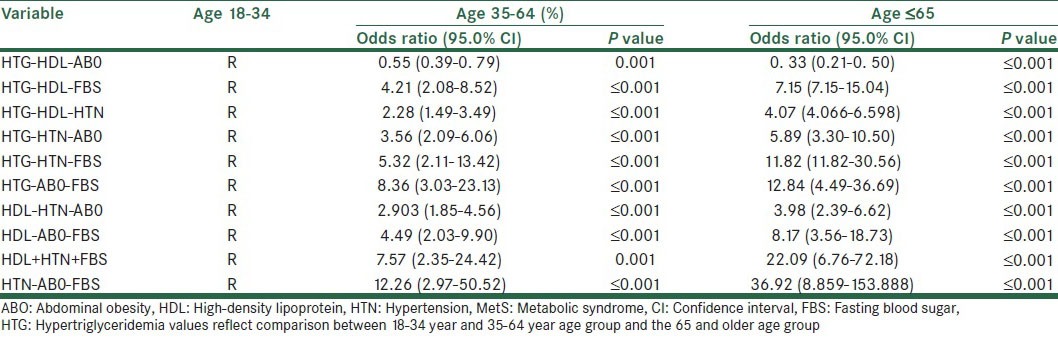
In subjects with MetS, we observed HTN and ABO in 56.1% of older individuals compared to only15.5% of younger adults (P = 0.001) [Table 1]. When we looked into a combination of three components namely HTG, low HDL-c and ABO, we found the highest prevalence (50.7%) in all subjects and especially in younger age group (63.2%). Middle age and elder groups followed the younger age group with prevalence of 50.5% and 37.8%, respectively. The most prevalent three components combination among elder subjects was HTG plus low HDL-c and HTN (43.9%) [Table 1]. In elder subjects the risk of having the combination of high FBS, ABO and Hypertrigeliceridemia was approximately 13 times more compared to younger and middle age groups (12.84 [4.49-36.69]).
Our results revealed a significant correlation between age and the risk of having major risk factors (P > 0.01) [Table 2].
Table 2.
Adjusted odds ratio for age groups according to the various MetS phenotype
DISCUSSION
Our findings showed phenotype of MetS is significantly different among different age groups. Previous evaluations of the IHHP data revealed relatively high prevalence of the MetS, which correlated with increasing prevalence of its individual components.[17] Large body of published studies reported an increasing in management of individual components of MetS such as HTN, diabetes, and dyslipidemia.[18] However, generally, MetS prevalence increased over the past decades in Iranian population as other ethnics.[19,20]
Previously, age related presence of MetS described in US population.[21] In a previous study, Sarrafzadegan et al. showed the prevalence of MetS in subjects aged over 60 years was significantly higher than those under 60.[19] However, our study adds to previous findings the age-related phenotypes of MetS in a relatively larger population. In addition, to the best of our knowledge this is the first time that the relationship between age groups and different phenotypes of MetS has discussed. Similar to other studies, our results showed a higher prevalence of the MetS in elder subjects and a larger number of the components of the syndrome clustering in elderly patients compared with younger patients. The prevalence of MetS was almost 4 times higher in individuals of 65 years and older compared with younger participants. Furthermore, the number of MetS components and their cluster was found higher in those aged 65 and older. This could be justified by hormonal changes over time especially in women.[22] Another study reported that with time secretary function of pancreatic β cells vary this could affect the development of insulin resistance and increase prevalence of MetS.[23]
In the present study, we found that the number of MetS components in subjects over 65 years is significantly higher than younger participants. Other study reported similar findings in participants over 50 years.
A recent study, which carried out in US showed the most frequent feature in young adults with MetS was ABO and low HDL-c in contrast to the oldest age group, in whom the triad of ABO, HTN, and HTG was most frequent.[24] They claimed that ABO was a predominant factor in all age groups in the western population and did not demonstrate any significant changes in prevalence across the age groups evaluated. However, our findings illustrated low HDL-c is dominant risk factor in all age-groups and followed by HTG in younger and middle age subjects and HTN in elder persons. Although in younger and middle age groups of Iranian low HDL-c, HTG and ABO are the more prevalent (63.2% and 50.7% respectively). The highest prevalent of three components combination among elder subjects was HTG plus low HDL-c and HTN (43.9%). Although Sumner et al. showed that HTG, HTN, and hyperglycemia significantly increased in prevalence with increasing age. Similar to Seo et al. study,[25] we found lower prevalence of ABO among elderly. It is well-documented that body weight and height decrease and fat mass increase, trunk, and visceral adipose tissue redistribute across higher age.[26,27]
Two other studies argued that risk factor clustering depends on the interaction between environmental and genetic factors. The penetrance of a particular common genetic factor involved in the simultaneous expression of several risk factors should permit clearer observation of risk factor clustering in younger subjects. A longer exposure to environmental factors that may lead to the development of particular individual risk factors in older subjects (principally HTN, which increased with age more than any other risk factor) may modify the risk factor clustering observed in this group. On the other hand, risk factor treatment also more prevalent in the 55-74 group.[28,29] Ramos et al. claimed that in younger subjects blood pressure was related to lipids, obesity, and glycaemia.[30] In addition, Poulter found that obesity, smoking, glucose intolerance, physical inactivity, and dyslipidemia often co-exist with HTN in both older and younger age groups in Italian population.[31] Whereas, Pasini et al. studied the clustering of different combinations of CVD risk factors including systolic and diastolic HTN, total cholesterol, and obesity among aged 40-59 years Italian population.[32]
Limitations
First of all, we made a cross-sectional evaluation and our results are subjective; therefore, to survival bias. Some of combinations of traits were present in a very low number so that the OR could not be calculated or resulted no significant. Secondly, It was important to evaluate for sex limitation effects, but we did not investigate the effect of sex on the phenotype of MetS, because we did not access to some biological factors as hormonal levels as we as sex-specific behavior and life-style factors.
CONCLUSION
This study provides a nationally representative estimate of the prevalence of MetS and its different phenotypes among different age groups. Low HDL-c is the most prevalent component among all study groups. ABO is more prevalent in young adults with the Mets while HTN and HTG are more prevalent in older adults. Therefore, regarding different phenotypes of MetS in various age groups, need to have important implications in the clinical management of these patients and the implementation of public health.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Qiao Q, DECODE Study Group Comparison of different definitions of the metabolic syndrome in relation to cardiovascular mortality in European men and women. Diabetologia. 2006;49:2837–46. doi: 10.1007/s00125-006-0438-6. [DOI] [PubMed] [Google Scholar]
- 2.Thomas GN, Schooling CM, McGhee SM, Ho SY, Cheung BM, Wat NM, et al. Metabolic syndrome increases all-cause and vascular mortality: The Hong Kong cardiovascular risk factor study. Clin Endocrinol (Oxf) 2007;66:666–71. doi: 10.1111/j.1365-2265.2007.02798.x. [DOI] [PubMed] [Google Scholar]
- 3.Wassink AM, van der Graaf Y, Olijhoek JK, Visseren FL, SMART Study Group Metabolic syndrome and the risk of new vascular events and all-cause mortality in patients with coronary artery disease, cerebrovascular disease, peripheral arterial disease or abdominal aortic aneurysm. Eur Heart J. 2008;29:213–23. doi: 10.1093/eurheartj/ehm582. [DOI] [PubMed] [Google Scholar]
- 4.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein Sadri G, Malekafzali H, Mohammadifard N, et al .Metabolic syndrome: An emerging public health problem in Iranian women: Isfahan healthy heart program. Int J Cardiol. 2008;131:90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 5.Gharipour M, Kelishadi R, Toghianifar N, Tavassoli AA, Khosravi AR, Sajadi F, et al. Socioeconomic disparities and smoking habits in metabolic syndrome: Evidence from Isfahan healthy heart program. Iran Red Crescent Med J. 2011;13:537–43. [PMC free article] [PubMed] [Google Scholar]
- 6.Gharipour M, Kelishadi R, Baghaie M, Rabiei K. Metabolic syndrome in an Iranian adult population. Eur Heart J. 2006;27 Suppl 1:250–251. [Google Scholar]
- 7.Haas GM, Bertsch T, Schwandt P. Trends of components of the metabolic syndrome in German first graders throughout 10 years: The PEP family heart study. Cholesterol 2012. 2012:231962. doi: 10.1155/2012/231962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dajani R, Khader YS, Hakooz N, Fatahalla R, Quadan F. Metabolic syndrome between two ethnic minority groups (Circassians and Chechens) and the original inhabitants of Jordan. Endocrine. 2013;43:112–9. doi: 10.1007/s12020-012-9723-y. [DOI] [PubMed] [Google Scholar]
- 9.Stefanov TS, Temelkova-Kurktschiev TS. The metabolic syndrome in Bulgaria. Folia Med (Plovdiv) 2011;53:5–14. doi: 10.2478/v10153-011-0061-2. [DOI] [PubMed] [Google Scholar]
- 10.Xu H, Song Y, You NC, Zhang ZF, Greenland S, Ford ES, et al. Prevalence and clustering of metabolic risk factors for type 2 diabetes among Chinese adults in Shanghai, China. BMC Public Health. 2010;10:683. doi: 10.1186/1471-2458-10-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford ES, Li C, Zhao G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes. 2010;2:180–93. doi: 10.1111/j.1753-0407.2010.00078.x. [DOI] [PubMed] [Google Scholar]
- 12.Hosseini-Esfahani F, Mousavi Nasl Khameneh A, Mirmiran P, Ghanbarian A, Azizi F. Trends in risk factors for cardiovascular disease among Iranian adolescents: The Tehran lipid and glucose study, 1999-2008. J Epidemiol. 2011;21:319–28. doi: 10.2188/jea.JE20100162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelishadi R, Gharipour M, Sadri GH, Tavasoli AA, Amani A. Cardiovascular disease risk factors, metabolic syndrome and obesity in an Iranian population. East Mediterr Health J. 2008;14:1070–9. [PubMed] [Google Scholar]
- 14.Sarraf-Zadegan N, Sadri G, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan healthy heart programme: A comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58:309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 15.Sarraf-Zadegan N, Baghaei M, Sadri G, Kelishadi R, Malek AH, Boshtam M, et al. Isfahan healthy heart program: Evaluation of comprehensive, community-based interventions for non-communicable disease prevention. Prev Contr. 2006;2:73–84. [Google Scholar]
- 16.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 17.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among US Adults. Diabetes Care. 2004;27:2444–9. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 18.Gharipour M, Sarrafzadegan N, Sadeghi M, Andalib E, Talaie M, Shafie D, Aghababaie E. Predictors of Metabolic Syndrome in the Iranian Population: Waist Circumference, Body Mass Index, or Waist to Hip Ratio? Cholesterol 2013. 2013:198384. doi: 10.1155/2013/198384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarrafzadegan N, Gharipour M, Sadeghi M, Khosravi AR, Tavassoli AA. Metabolic syndrome in Iranian elderly. ARYA Atheroscler. 2012;7:157–61. [PMC free article] [PubMed] [Google Scholar]
- 20.Tavassoli AA, Gharipour M, Khosravi A, Kelishadi R, Siadat ZD, Bahonar A, et al. Gender differences in obesogenic behaviour, socioeconomic and metabolic factors in a population-based sample of Iranians: The IHHP study. J Health Popul Nutr. 2010;28:602–9. doi: 10.3329/jhpn.v28i6.6609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sniderman AD, Holme I, Aastveit A, Furberg C, Walldius G, Jungner I. Relation of age, the apolipoprotein B/apolipoprotein A-I ratio, and the risk of fatal myocardial infarction and implications for the primary prevention of cardiovascular disease. Am J Cardiol. 2007;100:217–21. doi: 10.1016/j.amjcard.2007.02.086. [DOI] [PubMed] [Google Scholar]
- 22.Kraja AT, Borecki IB, North K, Tang W, Myers RH, Hopkins PN, et al. Longitudinal and age trends of metabolic syndrome and its risk factors: The family heart study. Nutr Metab (Lond) 2006;3:41. doi: 10.1186/1743-7075-3-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Razzouk L, Muntner P. Ethnic, gender, and age-related differences in patients with the metabolic syndrome. Curr Hypertens Rep. 2009;11:127–32. doi: 10.1007/s11906-009-0023-8. [DOI] [PubMed] [Google Scholar]
- 24.Sumner AD, Sardi GL, Reed JF., 3rd Components of the metabolic syndrome differ between young and old adults in the US population. J Clin Hypertens (Greenwich) 2012;14:502–6. doi: 10.1111/j.1751-7176.2012.00647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seo JA, Kim BG, Cho H, Kim HS, Park J, Baik SH, et al. The cutoff values of visceral fat area and waist circumference for identifying subjects at risk for metabolic syndrome in elderly Korean: Ansan Geriatric (AGE) cohort study. BMC Public Health. 2009;9:443. doi: 10.1186/1471-2458-9-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moon HK, Kim EG. Comparing validity of body mass index, waist to hip ratio, and waist circumference to cardiovascular disease risk factors in Korean elderly. Korean J Nutr. 2005;38:445–54. [Google Scholar]
- 27.Perissinotto E, Pisent C, Sergi G, Grigoletto F, ILSA Working Group (Italian Longitudinal Study on Ageing) Anthropometric measurements in the elderly: Age and gender differences. Br J Nutr. 2002;87:177–86. doi: 10.1079/bjn2001487. [DOI] [PubMed] [Google Scholar]
- 28.Liese AD, Mayer-Davis EJ, Haffner SM. Development of the multiple metabolic syndrome: An epidemiologic perspective. Epidemiol Rev. 1998;20:157–72. doi: 10.1093/oxfordjournals.epirev.a017978. [DOI] [PubMed] [Google Scholar]
- 29.Edwards KL, Newman B, Mayer E, Selby JV, Krauss RM, Austin MA. Heritability of factors of the insulin resistance syndrome in women twins. Genet Epidemiol. 1997;14:241–53. doi: 10.1002/(SICI)1098-2272(1997)14:3<241::AID-GEPI3>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 30.Ramos R, Marrugat J, Basagaña X, Sala J, Masiá R, Elosua R, et al. The role of age in cardiovascular risk factor clustering in non-diabetic population free of coronary heart disease. Eur J Epidemiol. 2004;19:299–304. doi: 10.1023/b:ejep.0000024697.55346.c2. [DOI] [PubMed] [Google Scholar]
- 31.Poulter NR. Risk factors for cardiovascular disease: ‘Clustering’ in the older hypertensive man. Br J Clin Pract Suppl. 1994;74:4–7. [PubMed] [Google Scholar]
- 32.Pasini GF, Donato F, Buizza MA, Fantoni C, Gelatti U, Tani M, et al. Prevalence of risk factors for coronary heart disease in a mountain community in northern Italy. G Ital Cardiol. 1999;29:891–7. [PubMed] [Google Scholar]


